Abstract
Background:
Previous meta-analyses have compared bone–patellar tendon–bone (BPTB) with hamstring tendon (HT) autografts for primary anterior cruciate ligament reconstruction (ACLR).
Purpose:
To conduct a systematic review of overlapping meta-analyses comparing BPTB with HT autografts for ACLR to determine which meta-analyses provide the best available evidence.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic review was performed by searching the PubMed and Cochrane Library databases. Search words included “anterior cruciate ligament” AND “patellar tendon” AND “hamstring tendon” AND “meta-analysis.” Results were reviewed to determine study eligibility. Patient outcomes and postoperative complications were extracted from the included meta-analyses. Meta-analysis quality was assessed using the Oxman-Guyatt and Quality of Reporting of Meta-analyses (QUOROM) scores. The Jadad decision algorithm was then utilized to determine which meta-analyses provided the best level of evidence.
Results:
Sixteen meta-analyses containing an average of 1396 patients met the eligibility criteria. Most studies found BPTB autografts to provide superior stability but more postoperative complications, such as anterior knee pain and kneeling pain. Studies by Gabler et al (2016), Mohtadi et al (2011), and Xie et al (2015) received the highest Oxman-Guyatt and QUOROM scores, and therefore, these meta-analyses proved to provide the highest level of evidence. Additionally, Xie et al was selected as the highest-quality study in this systematic review based on the Jadad decision algorithm.
Conclusion:
The current best evidence suggests that ACLR with BPTB autografts provides superior static knee stability and that there are fewer postoperative complications in ACLR with HT autografts.
Keywords: knee, anterior cruciate ligament reconstruction, bone–patellar tendon–bone autograft, hamstring tendon autograft, meta-analysis
There are several options when considering anterior cruciate ligament reconstruction (ACLR), including graft choice. A recent review of meta-analyses concluded that the current best evidence suggests no difference in rerupture rates or clinical outcomes between autografts or allografts.20 However, this review did not specify patient demographics.20 This same study found that lower evidence level suggest lower rerupture rates and better clinical outcomes with autografts.20 Regarding autografts, the decision between using a bone–patellar tendon–bone (BPTB) or hamstring tendon (HT) autograft remains controversial. Potential drawbacks of a BPTB autograft include the risk of patellar fractures, patellar tendon ruptures, quadriceps weakness, and donor site morbidity,12,13,21 while disadvantages of an HT autograft include decreased hamstring strength, increased joint laxity, and delayed graft-tunnel healing.4,21 In addition to graft choice, the surgeon must also decide which surgical technique to use. Anteromedial and transtibial techniques are the most commonly used, with most orthopaedic surgeons using the anteromedial technique, as it allows for unconstrained anatomic placement of the femoral tunnel.14 Regardless of the technique, surgeons must be careful to avoid a vertical or low femoral tunnel because of increased anterior translation and less rotational resistance compared with more anatomically oriented grafts.14
There are currently multiple meta-analyses evaluating BPTB versus HT autografts. A recent review of these meta-analyses15 evaluated their methodological rigor and credibility. However, no conclusion was made as to which type of autograft was superior according to the best available evidence. In addition, a systematic review of overlapping meta-analyses from 2007 compared BPTB versus HT autografts for primary ACLR and concluded that HT autografts are superior for preventing anterior knee pain and that there is limited evidence supporting the claim that BPTB autografts provide better stability.26 However, this study is now 10 years old, and several new meta-analyses have been published since.
The purpose of this study was to perform an updated systematic review of overlapping meta-analyses comparing primary ACLR with BPTB versus HT autografts to determine which meta-analyses provide the best available evidence. We hypothesized that ACLR with a BPTB autograft would demonstrate superior results when accounting for knee stability but that ACLR with an HT autograft would lead to fewer postoperative complications.
Methods
The methods of this study were similar to those of previous systematic reviews of overlapping meta-analyses.9,20 Two independent reviewers searched the PubMed and Cochrane Library databases up to December 19, 2016. The following search words were used: “anterior cruciate ligament” AND “patellar tendon” AND “hamstring tendon” AND “meta-analysis.” Inclusion criteria consisted of meta-analyses that were written in English and that compared BPTB versus HT autografts for primary ACLR. Exclusion criteria included (1) meta-analyses not including both autografts, (2) systematic reviews that did not perform a meta-analysis, and (3) cadaveric, animal, or other laboratory studies. The full articles of all studies that satisfied the inclusion and exclusion criteria were then collected. A thorough review of the articles was performed to ensure that all relevant studies were included in this systematic review.
After selecting studies to be included in this review, the following data were collected from each study: primary author, year of publication, levels of evidence included, number and publication dates of primary studies included, inclusion and exclusion criteria, performance of heterogeneity analytics, patient sample size, patient-reported outcomes, objective outcomes, surgical technique, and postoperative complications. The following outcome scores were identified as being reported or not reported by each meta-analysis: Lysholm score,18 Tegner score,31 Cincinnati score,24 subjective International Knee Documentation Committee (IKDC) score,10 objective IKDC score,8 Knee injury and Osteoarthritis Outcome Score (KOOS),29 range of motion, strength testing, radiographic evaluation, patient satisfaction, instrumental laxity, Lachman test, pivot-shift test, and single-legged hop test.
The number of “possible” previous meta-analyses cited relative to the number “actually” cited was recorded for each meta-analysis as well as the databases used in each literature search. The primary studies included in each meta-analysis were recorded in addition to study type (randomized controlled trials, prospective comparative studies, retrospective comparative studies, noncomparative prospective and retrospective studies). We then recorded which studies included the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). The quality of each meta-analysis was scored using the Quality of Reporting of Meta-analyses (QUOROM) system22 and the Oxman-Guyatt quality-appraisal tool.25 The QUOROM system evaluates meta-analyses based on the quality of their methodology and reporting in 18 different categories. A perfect score of 18 is obtained if each category is met. The Oxman-Guyatt quality-appraisal tool scores meta-analyses on a scale of 1 to 7 based on 9 different questions.
Because of the discordance among meta-analyses, the Jadad decision algorithm was used to guide appropriate interpretation. According to Jadad et al,11 discordance among meta-analyses is caused by the following 6 factors: clinical question, study selection and inclusion, data extraction, assessment of study quality, assessment of the ability to combine studies, and statistical methods for data synthesis. Two authors (H.B.S., D.A.H.) independently applied the Jadad decision algorithm to determine which meta-analyses provided the current best evidence. When discrepancies were present, the 2 reviewers discussed the results and came to an agreement.
Results
The initial search strategy resulted in a total of 37 results. After a review, 16 meta-analyses§ were found to meet inclusion and exclusion criteria. These studies were published between 200134 and 2016.6 The number of primary studies included in these meta-analyses ranged from 425 to 64.28 The number of patients analyzed ranged from 36130 to 3402,28 with an average of 1396 patients per study. Twelve of the studies|| reported the sample size of patients undergoing ACLR with a BPTB autograft, with an average of 677 patients, as well as the sample size of patients with an HT autograft, with an average of 738 patients.
Assessment of Previous Meta-analysis Literature
Fourteen of the meta-analyses cited some of the previously published meta-analyses,¶ while at the time of their publication, 2 meta-analyses5,34 had no other published meta-analyses to cite (Table 1). Only 2 studies7,23 cited all meta-analyses possible at the time of their last literature search. Three studies1,27,28 did not report the date of their last literature search; therefore, no conclusions could be made regarding the number of possible meta-analyses available for citation.
TABLE 1.
Number of Systematic Reviews or Meta-analyses Actually Cited Compared With Maximum Number That Could Possibly Have Been Citeda
| Author | Date of Publication | Date of Last Literature Search | No. of Systematic Reviews or Meta-analyses Possible to Cite | No. of Systematic Reviews or Meta-analyses Cited |
|---|---|---|---|---|
| Yunes et al34 | Mar 2001 | May 1997 | 0 | 0 |
| Freedman et al5 | Jan 2003 | May 2000 | 0 | 0 |
| Goldblatt et al7 | Jul 2005 | Apr 2003 | 2 | 2 |
| Prodromos et al28 | Oct 2005 | NR | NR | 2 |
| Biau et al3 | Apr 2006 | Mar 2005 | 3 | 1 |
| Biau et al2 | May 2007 | Apr 2006 | 5 | 4 |
| Poolman et al27 | Jun 2007 | NR | NR | 2 |
| Biau et al1 | Dec 2009 | NR | NR | 5 |
| Magnussen et al19 | Mar 2011 | May 2009 | 7 | 6 |
| Mohtadi et al23 | Sep 2011 | Apr 2008 | 7 | 7 |
| Li et al17 | Oct 2011 | Sep 2008 | 7 | 3 |
| Shi and Yao30 | Dec 2011 | Aug 2011 | 9 | 4 |
| Li et al16 | Sep 2012 | Dec 2011 | 11 | 7 |
| Xie et al33 | Jan 2015 | Sep 2013 | 13 | 4 |
| Xie et al32 | Mar 2015 | Dec 2012 | 13 | 4 |
| Gabler et al6 | Apr 2016 | Mar 2014 | 13 | 6 |
aNR, not reported.
Outcome Measures
Table 2 shows the wide variety of clinical outcomes assessed by each of the meta-analyses. The Lachman test was the most commonly analyzed outcome and was reported by 12 of the 16 studies. Other commonly analyzed outcomes included instrumental laxity, graft failure, and the pivot-shift test.
TABLE 2.
Outcomes Reported by Each of the Included Studiesa
| Yunes et al34 | Freedman et al5 | Goldblatt et al7 | Prodromos et al28 | Biau et al3 | Biau et al2 | Poolman et al27 | Biau et al1 | Magnussen et al19 | Mohtadi et al23 | Li et al17 | Shi and Yao30 | Li et al16 | Xie et al32 | Xie et al33 | Gabler et al6 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Objective outcomes | ||||||||||||||||
| Tegner | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Objective IKDC | – | – | + | + | – | + | – | – | + | + | – | – | + | + | + | – |
| Instrumental laxity | + | + | + | + | + | – | – | – | + | + | + | + | – | + | + | – |
| Lachman test | + | – | + | + | + | – | + | + | + | + | + | – | + | + | + | – |
| Pivot-shift test | + | + | + | – | + | – | – | + | + | + | + | – | + | + | + | – |
| Single-legged hop test | – | – | – | – | – | – | – | – | – | – | – | + | – | – | – | – |
| Range of motion | + | + | + | – | + | – | – | – | + | + | + | – | + | + | + | – |
| Strength testing | – | – | – | – | – | – | – | – | + | + | – | + | – | – | – | – |
| Radiographic evaluation | – | – | – | – | – | – | – | – | + | – | – | – | – | + | – | – |
| Subjective outcomes | ||||||||||||||||
| Lysholm | – | – | + | – | – | – | – | – | + | – | – | + | – | – | – | – |
| Subjective IKDC | – | – | + | – | – | – | – | – | + | + | – | – | – | – | – | – |
| KOOS | – | – | – | – | – | – | – | – | – | + | – | – | – | – | – | – |
| Cincinnati | – | – | – | – | – | – | – | – | + | + | – | – | – | – | – | – |
| Return to activity/sport | + | + | – | – | – | + | – | – | – | + | – | – | – | + | + | + |
| Satisfaction | – | + | – | – | – | – | – | – | – | + | – | – | – | – | – | – |
| Complications | ||||||||||||||||
| Overall complications | + | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Kneeling pain | – | – | + | – | + | – | – | – | + | + | + | + | + | + | + | – |
| Patellofemoral crepitus | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Anterior knee pain | – | + | + | – | + | – | + | – | + | + | + | – | + | + | + | – |
| Graft failure | + | + | + | – | + | – | – | – | + | + | + | – | + | + | + | + |
| Subsequent meniscectomy or meniscal repair | – | + | + | – | – | – | – | – | – | – | – | – | + | – | – | – |
| Hardware removal | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Manipulation under anesthesia | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Infection | – | + | – | – | – | – | – | – | – | – | – | – | + | – | – | – |
| Swelling | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Giving way | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
a“+” or “–” indicates that an outcome measure was/was not reported, respectively. IKDC, International Knee Documentation Committee; KOOS, Knee Injury and Osteoarthritis Outcome Score.
Search Methodology
Thirteen of the 16 meta-analyses used PubMed/MEDLINE as part of the literature search (Table 3). There was significant variability in the use of other databases, including the Cochrane Library, EMBASE, and other sources.
TABLE 3.
Search Methodology Used by Each of the Included Studiesa
| Author | PubMed/MEDLINE | EMBASE | Cochrane Library | Other | No. of Primary Studies | Primary Studies Including Only RCTs | PRISMA | QUOROM Score | Oxman-Guyatt Score |
|---|---|---|---|---|---|---|---|---|---|
| Yunes et al34 | + | – | – | – | 4 | – | – | 15 | 3 |
| Freedman et al5 | + | – | – | – | 34 | – | – | 16 | 4 |
| Goldblatt et al7 | + | – | – | – | 11 | – | – | 16 | 4 |
| Prodromos et al28 | + | – | – | – | 64 | – | – | 13 | 2 |
| Biau et al3 | + | – | + | + | 18 | +b | – | 17 | 4 |
| Biau et al2 | + | – | + | + | 14 | +b | – | 13 | 6 |
| Poolman et al27 | – | – | – | + | 14 | +b | – | 12 | 1 |
| Biau et al1 | – | – | – | + | 6 | + | – | 16 | 2 |
| Magnussen et al19 | + | + | – | – | 7 | – | – | 15 | 6 |
| Mohtadi et al23 | + | + | + | + | 19 | +b | – | 16 | 7 |
| Li et al17 | + | + | + | – | 19 | +b | + | 16 | 5 |
| Shi and Yao30 | + | + | + | + | 6 | + | – | 16 | 3 |
| Li et al16 | – | – | – | + | 9 | + | – | 17 | 4 |
| Xie et al33 | + | + | + | – | 14 | – | – | 17 | 5 |
| Xie et al32 | + | + | + | – | 22 | + | – | 17 | 6 |
| Gabler et al6 | + | – | – | + | 28 | – | + | 17 | 6 |
a“+” or “–” indicates that a search method was/was not used in the designated meta-analysis, respectively. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses; QUOROM, Quality of Reporting of Meta-analyses; RCT, randomized controlled trial.
bStudy included both RCTs and pseudo-RCTs.
Study Quality and Validity
The QUOROM and Oxman-Guyatt scores for each study are depicted in Table 3. QUOROM scores ranged from 1227 to 17,3,6,16,32,33 with 18 being the maximum possible score.22 The average score was 15.6. Oxman-Guyatt scores ranged from 127 to 7,23 with 7 being the maximum possible score and representing “minimal flaws” in the study methodology.25 The average score was 4.25. Five studies1,27,28,30,34 had Oxman-Guyatt scores of ≤3, which is generally reflective of “major flaws” in the study methodology.25
Among the 16 meta-analyses, a total of 69 prospective comparative studies and 2 retrospective comparative studies were included. Table 4 shows the primary studies used in each meta-analysis.
TABLE 4.
Primary Studies Included in Meta-analysesa
| Yunes et al34 | Freedman et al5 | Goldblatt et al7 | Prodromos et al28 | Biau et al3 | Biau et al2 | Poolman et al27 | Biau et al1 | Magnussen et al19 | Mohtadi et al23 | Li et al17 | Shi and Yao30 | Li et al16 | Xie et al32 | Xie et al33 | Gabler et al6 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prospective comparative studies | ||||||||||||||||
| O’Neill (1996) | + | + | – | – | + | + | + | – | – | + | + | – | – | – | – | – |
| Aglietti (1994) | + | – | + | – | + | + | + | – | – | + | + | – | – | – | – | – |
| Marder (1991) | + | + | + | – | + | + | + | – | – | + | + | – | – | – | – | – |
| Corry (1999) | + | + | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Aune (2001) | – | – | + | – | + | – | + | – | – | + | + | + | – | – | – | – |
| Jansson (2003) | – | – | + | – | + | + | + | – | – | + | + | – | – | – | – | – |
| Ejerhed (2003) | – | – | + | – | + | + | + | + | – | + | + | – | + | – | + | – |
| Eriksson (2001) | – | – | + | – | + | + | + | – | – | + | + | – | – | – | – | – |
| Muneta (1998) | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Barrett (2002) | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Webster (2001) | – | – | + | – | + | + | + | – | – | – | + | – | + | – | + | – |
| Aglietti (2004) | – | – | – | + | – | + | – | – | – | + | + | – | – | – | – | – |
| Aglietti (1997) | – | – | – | – | + | – | + | – | – | – | – | – | – | – | – | – |
| Aglietti (1997) | – | – | – | + | + | + | + | – | – | – | + | – | – | – | – | – |
| Anderson (2001) | – | – | – | + | + | + | + | – | – | + | + | – | + | – | + | – |
| Eriksson (2001) | – | – | – | + | + | + | + | – | – | – | – | – | – | – | – | – |
| Feller (2001) | – | – | – | – | + | + | + | – | – | – | + | + | – | – | – | – |
| Feller (2003) | – | – | – | + | + | + | + | + | – | + | + | – | + | – | + | – |
| Harilainen (2006) | – | – | – | – | – | + | – | + | – | – | + | + | – | + | – | – |
| Ibrahim (2005) | – | – | – | – | + | + | + | – | + | + | + | – | – | + | – | – |
| Laxdal (2005) | – | – | – | – | + | + | + | + | – | + | + | – | + | – | + | + |
| Matsumoto (2006) | – | – | – | – | – | + | – | – | – | + | + | – | – | + | – | – |
| O’Neill (2001) | – | – | – | + | + | + | + | – | + | – | + | – | – | + | – | – |
| Ropke (2001) | – | – | – | – | + | + | + | – | – | + | – | – | – | – | – | – |
| Shaieb (2002) | – | – | + | + | + | + | + | – | – | + | + | – | – | – | – | – |
| Sajovic (2006) | – | – | – | – | – | – | – | + | + | + | + | – | – | – | – | – |
| Zaffagnini (2006) | – | – | – | – | – | – | – | + | + | + | – | – | – | + | – | – |
| Keays (2007) | – | – | – | – | – | – | – | – | + | – | – | – | – | + | – | – |
| Liden (2007) | – | – | – | – | – | – | – | – | + | – | – | – | + | + | + | – |
| Beynnon (2002) | – | – | – | + | + | – | + | – | – | + | + | – | + | – | + | – |
| Maletis (2007) | – | – | – | – | – | – | – | – | – | + | + | – | + | – | + | – |
| Beard (2001) | – | – | – | – | + | – | + | – | – | – | + | – | – | – | – | – |
| Carter (1999) | – | – | – | – | – | – | – | – | – | – | – | + | – | – | – | – |
| Jansson (1999) | – | – | – | – | – | – | – | – | – | – | – | + | – | – | – | – |
| Holm (2010) | – | – | – | – | – | – | – | – | – | – | – | + | – | + | – | – |
| Taylor (2009) | – | – | – | – | – | – | – | – | – | – | – | – | + | – | + | – |
| Drogset (2010) | – | – | – | – | – | – | – | – | – | – | – | – | + | – | + | – |
| Wipfler (2011) | – | – | – | – | – | – | – | – | – | – | – | – | + | + | + | + |
| Pinczewski (2007) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Wagner (2005) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Otero (1993) | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Otsuka (2003) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Felmet (2010) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Gobbi (2003) | – | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – |
| Aglietti (2007) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Aglietti (2010) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Ahldén (2013) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Ferretti (2008) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Gobbi (2012) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Hussein (2012) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Ibrahim (2009) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Jagodzinski (2010) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Jarvela (2008) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Kondo (2008) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Kondo (2012) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Nunez (2012) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Plaweski (2009) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Stener (2010) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Sun (2011) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Suomalainen (2013) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Tohyama (2011) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Yasuda (2006) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Callaway (1997) | – | – | – | – | + | – | + | – | – | – | – | – | – | – | – | – |
| Gifstad (2013) | – | – | – | – | – | – | – | – | – | – | – | – | – | + | – | – |
| Sajovic (2011) | – | – | – | – | – | – | – | – | – | – | – | – | – | + | – | + |
| Zaffagnini (2008) | – | – | – | – | – | – | – | – | – | – | – | – | – | – | – | + |
| Zaffagnini (2011) | – | – | – | – | – | – | – | – | – | – | – | – | – | + | – | – |
| Barenius (2010) | – | – | – | – | – | – | – | – | – | – | – | – | – | + | – | – |
| Leys (2015) | – | – | – | – | – | – | – | – | – | – | – | – | – | + | – | – |
| Retrospective comparative studies | ||||||||||||||||
| Feagin (1997) | – | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – |
| Marumo (2000) | – | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – |
| No. of noncomparative studies | 0 | 26 | 0 | 38 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Prospective | 0 | 13 | 0 | 18 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Retrospective | 0 | 13 | 0 | 20 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
a“+” or “–” indicates that a primary study was/was not used in the designated meta-analysis, respectively.
Findings
Eleven studies3,5–7,16,17,19,23,32–34 reported graft failure outcomes. Only 1 study5 found a statistically significant increase in graft failure for patients with an HT autograft. Eight of the studies3,7,16,17,19,23,32,34 reported higher rates of failure for patients undergoing ACLR with an HT autograft; however, these findings were not significant. Eleven studies# analyzed knee stability via instrumental testing. Five studies3,5,17,23,34 found that those undergoing ACLR with a BPTB autograft had a significantly increased chance of attaining a statically stable knee, while 1 study28 found increased stability with an HT autograft. Five studies7,19,30,32,33 found no significant difference in instrumental stability between BPTB and HT autografts. Eleven studies** evaluated knee stability with the pivot-shift test. Six of these studies1,16,17,23,32,34 found that patients with a BPTB autograft had a significantly lower rate of positive pivot-shift test findings. While 5 studies3,5,7,19,33 found no significant difference between BPTB and HT autografts, all results still favored lower rates of positive pivot-shift test findings with a BPTB autograft.
Anterior knee pain and kneeling pain were the most frequently analyzed patient-reported outcomes. Ten studies†† analyzed anterior knee pain. Nine of these studies‡‡ found a significantly increased rate of anterior knee pain when undergoing ACLR with a BPTB autograft. One study8 found a nonsignificantly higher rate of anterior knee pain with a BPTB autograft. Nine studies§§ analyzed kneeling pain. Eight studies3,7,16,17,19,23,32,33 found a significantly increased rate of kneeling pain with a BPTB autograft, while only 1 study30 found a significantly increased rate of kneeling pain with an HT autograft.
Heterogeneity Assessment
Of the 16 meta-analyses included in this study, 14|||| tested for heterogeneity. All 16 meta-analyses¶¶ performed a subgroup or sensitivity analysis to compare study designs, interventions, and outcomes (Table 5). Other parameters, such as sex, age, surgical procedure, and postoperative protocols, were reviewed without performing a subgroup or sensitivity analysis.
TABLE 5.
Heterogeneity or Subgroup Analyses of Primary Studiesa
| Yunes et al34 | Freedman et al5 | Goldblatt et al7 | Prodromos et al28 | Biau et al3 | Biau et al2 | Poolman et al27 | Biau et al1 | Magnussen et al19 | Mohtadi et al23 | Li et al17 | Shi and Yao30 | Li et al16 | Xie et al32 | Xie et al33 | Gabler et al6 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Statistical heterogeneity analysis | + | + | + | – | + | + | + | 0 | + | + | + | + | + | + | + | + |
| Subgroup or sensitivity analysis | ||||||||||||||||
| Primary study quality | 0 | – | – | – | 0 | 0 | – | – | 0 | 0 | 0 | – | 0 | – | 0 | – |
| Age | 0 | – | – | – | 0 | 0 | – | 0 | 0 | 0 | 0 | – | 0 | 0 | 0 | – |
| Sex | 0 | – | – | – | 0 | 0 | – | 0 | 0 | + | 0 | – | 0 | 0 | 0 | – |
| Surgical procedure | 0 | – | – | – | – | – | + | 0 | 0 | – | – | – | 0 | 0 | 0 | 0 |
| Postoperative protocol | 0 | – | – | – | – | – | – | 0 | – | – | – | – | – | 0 | – | – |
| Return to activity | + | – | – | – | – | + | – | – | – | + | – | – | – | + | + | – |
| Lachman test | + | – | + | – | + | – | – | + | 0 | + | + | – | + | + | + | – |
| Instrumental laxity | + | + | + | + | + | – | – | – | + | + | + | + | – | + | + | – |
| Pivot-shift test | + | + | + | – | + | – | – | + | 0 | + | + | – | + | + | + | – |
| ROM loss of extension | + | + | + | – | + | – | – | – | 0 | + | + | – | + | + | + | – |
| ROM loss of flexion | + | – | + | – | – | – | – | – | – | + | – | – | + | + | + | – |
| Complications | + | – | + | – | – | – | – | – | – | – | – | – | + | – | – | – |
| Graft failure | + | + | + | – | + | – | – | – | + | + | + | – | + | + | + | + |
| Giving way | – | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Subjective IKDC | – | – | + | – | – | + | – | – | 0 | + | – | – | + | – | – | – |
| Objective IKDC | – | – | + | – | – | + | – | – | 0 | + | – | – | + | + | + | – |
| Anterior knee pain | – | + | + | – | + | – | + | – | 0 | + | + | – | + | + | + | – |
| Kneeling pain | – | – | – | – | + | – | – | – | 0 | + | + | + | + | + | + | – |
| Single-legged hop test | – | – | – | – | – | – | – | – | – | + | – | + | – | – | – | – |
| Tegner | – | – | – | – | – | – | – | – | – | + | – | – | – | – | – | – |
| Lysholm | – | – | – | – | – | – | – | – | – | + | – | + | – | – | – | – |
| Cincinnati | – | – | – | – | – | – | – | – | – | + | – | – | – | – | – | – |
| Strength testing | – | – | – | – | – | – | – | – | – | + | – | + | – | – | – | – |
| Infection | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Hardware removal | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Manipulation under anesthesia | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
| Meniscal surgery | – | + | – | – | – | – | – | – | – | – | – | – | – | – | – | – |
a“+” or “–” indicates that formal sensitivity or subgroup analysis was/was not performed, respectively; “0” indicates that descriptive data were performed or discussed but that no analysis was performed. IKDC, International Knee Documentation Committee; ROM, range of motion.
Results of Jadad Decision Algorithm
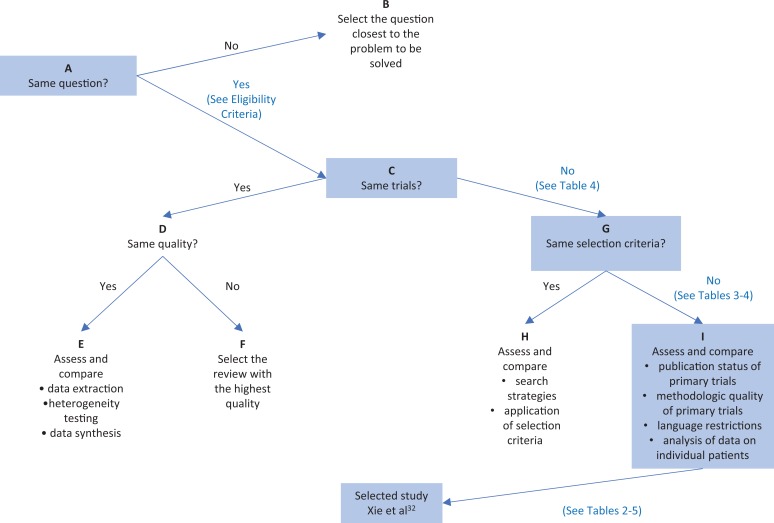
The Jadad decision algorithm11 was used to determine which of the 16 included meta-analyses provided the best available evidence. Figure 1 depicts all outcomes of the included meta-analyses. Because of the variety of selection criteria among included meta-analyses, the Jadad decision algorithm was used to select the highest-quality review based on the publication characteristics of the primary trials, the methodology of the primary trials, language restrictions, and whether an analysis of data on individual patients was included in the study. Xie et al32 provided the best available evidence in accordance with the Jadad decision algorithm for having the largest number of randomized controlled trials included as well as its more thorough methodology assessment of included randomized controlled trials.
Figure 1.
Flow diagram of Jadad decision algorithm.11
Discussion
The purpose of this study was to conduct a systematic review of overlapping meta-analyses comparing the outcomes of BPTB versus HT autografts for primary ACLR and to determine which meta-analyses provide the best available evidence. We hypothesized that ACLR with a BPTB autograft would produce superior results when accounting for knee stability but that ACLR with an HT autograft would lead to fewer postoperative complications. Our hypothesis that ACLR with a BPTB autograft would lead to superior knee stability results was supported.1,3,5,16,17,23,33,34 Also, our hypothesis that ACLR with an HT autograft would result in fewer complications was supported.## While 9 studies3,5,7,16,17,19,23,32,34 found an increase in graft failure after ACLR with an HT autograft, only 1 of these studies6 found a significant difference. Therefore, current evidence is not strong enough to support a significant difference of graft failure between BPTB and HT autografts.
In evaluating the 16 meta-analyses included in this review with the Oxman-Guyatt and QUOROM scores, 3 studies6,23,32 were found to have the highest combination of scores. Two studies6,32 had a QUOROM score of 17 and an Oxman-Guyatt score of 6, while 1 study23 had a QUOROM score of 16 and an Oxman-Guyatt score of 7. According to these 2 evaluation scores, these 3 meta-analyses6,23,32 appear to provide the highest level of evidence. According to the Jadad decision algorithm, Xie et al32 was selected as the highest-quality study in this systematic review. Mohtadi et al23 found significant evidence that ACLR with a BPTB autograft results in a more statically stable knee compared with an HT autograft. They also found a significant increase in postoperative complications after ACLR with a BPTB autograft. These authors concluded that there was insufficient evidence to make a conclusion regarding the long-term functional outcome differences between the 2 graft types. Xie et al32 found no difference between BPTB and HT autografts in terms of instrumental laxity and the Lachman test. However, they did find significant differences in the pivot-shift test in favor of BPTB autografts. They found that the risk ratio for a positive pivot-shift test finding was 0.7 (95% CI, 0.53-0.93; P = .01) in favor of BPTB autografts.32 There was a significant increase in postoperative complications after ACLR with a BPTB autograft. They found that the risk ratio for anterior knee pain was 1.71 (95% CI, 1.35-2.16; P = .01) in favor of HT autografts and that the risk ratio for kneeling pain was 2.05 (95% CI, 1.51-2.77; P < .01) in favor of HT autografts.32 While Xie et al acknowledged the possible benefits of each graft, they were unable to conclude which of the 2 grafts provided a significantly better overall option when undergoing ACLR. Last, Gabler et al6 found no significant difference in graft failure rates or the odds of graft failure between BPTB and HT autografts. Additionally, no significant difference in returning to preinjury activity levels was found. While Gabler et al concluded that both BPTB and HT autografts demonstrated a low risk of graft failure and a moderately high rate of return to preinjury activity levels, no conclusions were made with regard to which graft provided superior results.
In addition to the issues discussed in this study, other factors must be considered when deciding between BPTB and HT autografts for primary ACLR. These include the risk of patellar fractures during harvesting as well as a fixed graft length with a BPTB autograft and graft slippage with an HT autograft.14
One of the strengths of this systematic review included the use of multiple quality-assessment tools11,22,25 to evaluate which meta-analyses provided the best available evidence. The limitations of this systematic review should also be noted. These included variations in the surgical procedure used, or lack of reporting the surgical procedure, and patients lost to follow-up in each of the meta-analyses included. We also believe that the minimum follow-up time of 24 months is a limitation of this study. In addition, variations in subjective outcomes such as anterior knee pain and kneeling pain must be considered. It is also possible that variations in surgical techniques and rehabilitation protocols between studies played a role in the different clinical outcomes observed between these studies. Finally, there exist limitations inherent to a systematic review of overlapping meta-analyses, which include the lack of pooling of data as well as the potential heterogeneity among the 16 included meta-analyses.
While there are multiple meta-analyses evaluating ACLR with BPTB versus HT autografts, further research is necessary to investigate which autograft choice provides superior overall results, specifically within different demographics such as athletes, adults, and adolescents.
Conclusion
This systematic review determined which meta-analyses provide the best available evidence when comparing ACLR with BPTB versus HT autografts. The results of this review suggest that ACLR with a BPTB autograft provides superior static knee stability but an increased postoperative complication rate when compared with an HT autograft. When considering ACLR autograft options, Xie et al,32 Mohtadi et al,23 and Gabler et al6 have provided the highest-quality meta-analyses.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution.
References
- 1. Biau DJ, Katsahian S, Kartus J, et al. Patellar tendon versus hamstring tendon autografts for reconstructing the anterior cruciate ligament: a meta-analysis based on individual patient data. Am J Sports Med. 2009;37(12):2470–2478. [DOI] [PubMed] [Google Scholar]
- 2. Biau DJ, Tournoux C, Katsahian S, Schranz P, Nizard R. ACL reconstruction: a meta-analysis of functional scores. Clin Orthop Relat Res. 2007;458:180–187. [DOI] [PubMed] [Google Scholar]
- 3. Biau DJ, Tournoux C, Katsahian S, Schranz PJ, Nizard RS. Bone-patellar tendon-bone autografts versus hamstring autografts for reconstruction of anterior cruciate ligament: meta-analysis. BMJ. 2006;332(7548):995–1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bizzini M, Gorelick M, Munzinger U, Drobny T. Joint laxity and isokinetic thigh muscle strength characteristics after anterior cruciate ligament reconstruction: bone patellar tendon bone versus quadrupled hamstring autografts. Clin J Sport Med. 2006;16(1):4–9. [DOI] [PubMed] [Google Scholar]
- 5. Freedman KB, D’Amato MJ, Nedeff DD, Kaz A, Bach BR., Jr Arthroscopic anterior cruciate ligament reconstruction: a metaanalysis comparing patellar tendon and hamstring tendon autografts. Am J Sports Med. 2003;31(1):2–11. [DOI] [PubMed] [Google Scholar]
- 6. Gabler CM, Jacobs CA, Howard JS, Mattacola CG, Johnson DL. Comparison of graft failure rate between autografts placed via an anatomical anterior cruciate ligament reconstruction technique: a systematic review, meta-analysis, and meta-regression. Am J Sports Med. 2016;44(4):1069–1079. [DOI] [PubMed] [Google Scholar]
- 7. Goldblatt JP, Fitzsimmons SE, Balk E, Richmond JC. Reconstruction of the anterior cruciate ligament: meta-analysis of patellar tendon versus hamstring tendon autograft. Arthroscopy. 2005;21(7):791–803. [DOI] [PubMed] [Google Scholar]
- 8. Hefti F, Muller W, Jakob R, Staubli H. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1(3-4):226–234. [DOI] [PubMed] [Google Scholar]
- 9. Houck DA, Kraeutler MJ, Schuette HB, McCarty EC, Bravman JT. Early versus delayed motion after rotator cuff repair: a systematic review of overlapping meta-analyses. Am J Sports Med. 2017;45(12):2911–2915. [DOI] [PubMed] [Google Scholar]
- 10. Irrgang J, Anderson A, Boland A, et al. Development and validation of the International Knee Documentation Committee subjective knee form. Am J Sports Med. 2001;29(5):600–613. [DOI] [PubMed] [Google Scholar]
- 11. Jadad AR, Cook DJ, Browman GP. A guide to interpreting discordant systematic reviews. CMAJ. 1997;156(10):1411–1416. [PMC free article] [PubMed] [Google Scholar]
- 12. Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17(9):971–980. [DOI] [PubMed] [Google Scholar]
- 13. Kraeutler MJ, Bravman JT, McCarty EC. Bone-patellar tendon-bone autograft versus allograft in outcomes of anterior cruciate ligament reconstruction: a meta-analysis of 5182 patients. Am J Sports Med. 2013;41(10):2439–2448. [DOI] [PubMed] [Google Scholar]
- 14. Kraeutler MJ, Wolsky RM, Vidal AF, Bravman JT. Anatomy and biomechanics of the native and reconstructed anterior cruciate ligament: surgical implications. J Bone Joint Surg Am. 2017;99(5):438–445. [DOI] [PubMed] [Google Scholar]
- 15. Kurz A, Evaniew N, Yeung M, Samuelsson K, Peterson D, Ayeni OR. Credibility and quality of meta-analyses addressing graft choice in anterior cruciate ligament reconstruction: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2017;25(2):538–551. [DOI] [PubMed] [Google Scholar]
- 16. Li S, Chen Y, Lin Z, Cui W, Zhao J, Su W. A systematic review of randomized controlled clinical trials comparing hamstring autografts versus bone-patellar tendon-bone autografts for the reconstruction of the anterior cruciate ligament. Arch Orthop Trauma Surg. 2012;132(9):1287–1297. [DOI] [PubMed] [Google Scholar]
- 17. Li S, Su W, Zhao J, et al. A meta-analysis of hamstring autografts versus bone-patellar tendon-bone autografts for reconstruction of the anterior cruciate ligament. Knee. 2011;18(5):287–293. [DOI] [PubMed] [Google Scholar]
- 18. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10(3):150–154. [DOI] [PubMed] [Google Scholar]
- 19. Magnussen RA, Carey JL, Spindler KP. Does autograft choice determine intermediate-term outcome of ACL reconstruction? Knee Surg Sports Traumatol Arthrosc. 2011;19(3):462–472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mascarenhas R, Erickson BJ, Sayegh ET, et al. Is there a higher failure rate of allografts compared with autografts in anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Arthroscopy. 2015;31(2):364–372. [DOI] [PubMed] [Google Scholar]
- 21. Matsumoto A, Yoshiya S, Muratsu H, et al. A comparison of bone-patellar tendon-bone and bone-hamstring tendon-bone autografts for anterior cruciate ligament reconstruction. Am J Sports Med. 2006;34(2):213–219. [DOI] [PubMed] [Google Scholar]
- 22. Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-analyses. Lancet. 1999;354(9193):1896–1900. [DOI] [PubMed] [Google Scholar]
- 23. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;(9):CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Noyes FR, Barber SD, Mooar LA. A rationale for assessing sports activity levels and limitations in knee disorders. Clin Orthop Relat Res. 1989;(246):238–249. [PubMed] [Google Scholar]
- 25. Oxman AD, Guyatt GH. Validation of an index of the quality of review articles. J Clin Epidemiol. 1991;44(11):1271–1278. [DOI] [PubMed] [Google Scholar]
- 26. Poolman RW, Abouali JA, Conter HJ, Bhandari M. Overlapping systematic reviews of anterior cruciate ligament reconstruction comparing hamstring autograft with bone-patellar tendon-bone autograft: why are they different? J Bone Joint Surg Am. 2007;89(7):1542–1552. [DOI] [PubMed] [Google Scholar]
- 27. Poolman RW, Forrokhyar F, Bhandari M. Hamstring tendon autograft better than bone patellar tendon bone autograft in ACL reconstruction: a cumulative meta-analysis and clinically relevant sensitivity analysis applied to a previously published analysis. Acta Orthop. 2007;78(3):350–354. [DOI] [PubMed] [Google Scholar]
- 28. Prodromos CC, Joyce BT, Shi K, Keller BL. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar tendon graft and fixation type. Arthroscopy. 2005;21(10):1202. [DOI] [PubMed] [Google Scholar]
- 29. Roos EW, Lohmander LS. The Knee injury and Osteoarthritis Outcome Score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes. 2003;1:64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Shi DL, Yao ZJ. Knee function after anterior cruciate ligament reconstruction with patellar or hamstring tendon: a meta-analysis. Chin Med J (Engl). 2011;124(23):4056–4062. [PubMed] [Google Scholar]
- 31. Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;(198):43–49. [PubMed] [Google Scholar]
- 32. Xie X, Liu X, Chen Z, Yu Y, Peng S, Li Q. A meta-analysis of bone-patellar tendon-bone autograft versus four-strand hamstring tendon autograft for anterior cruciate ligament reconstruction. Knee. 2015;22(2):100–110. [DOI] [PubMed] [Google Scholar]
- 33. Xie X, Xiao Z, Li Q, et al. Increased incidence of osteoarthritis of the knee joint after ACL reconstruction with bone-patellar tendon-bone autografts than hamstring autografts: a meta-analysis of 1,443 patients at a minimum of 5 years. Eur J Orthop Surg Traumatol. 2015;25(1):149–159. [DOI] [PubMed] [Google Scholar]
- 34. Yunes M, Richard JC, Engels EA, Pinczewski LA. Patellar versus hamstring tendon in anterior cruciate ligament reconstruction: a meta-analysis. Arthroscopy. 2001;17(3):248–257. [DOI] [PubMed] [Google Scholar]