Abstract
Background
Comminuted tibial end bony avulsion of posterior cruciate ligament (PCL) is a challenging problem in terms of accurate reduction, fixation and union to provide a stable knee. Arthroscopic reduction or a screw fixation is good option for a large fragment but comminuted fragment reduction remains a challenge. Suture bridge technique using two anchors can provide an accurate reduction and stable fixation.
Method
10 patients of isolated comminuted PCL avulsion with a mean age of 30 years were fixed by standard posterior approach using suture bridge technique.
Results
Mean follow up was 12 months. All patients showed radiological union at 12 weeks with a mean Lysholm score of 92. Seven out of ten achieved IKDC grade A and remaining three had grade B. No complication of the procedure were noted.
Conclusion
Suture bridge technique is an excellent option to fix a comminuted PCL avulsion fracture where arthroscopic reduction or open single screw fixation is not a viable due option due to comminution.
Keywords: Posterior cruciate ligament, Avulsion, Comminuted, Suture bridge, Fixation
1. Introduction
Injuries of the posterior cruciate ligament (PCL) represents about 20% of the knee ligament injuries.1,2 The damage to PCL varies from bony avulsion to intrasubstance tear, for which the treatment differs. Even though the global incidence of avulsion fracture of the PCL from the tibial insertion is rare, the occurrence is high in Asian countries due to higher two wheeler related injuries.3 The restoration of normal anatomy and biomechanics of the PCL is crucial for the return of the function and stability of the knee while avoiding the late arthritis of the knee.4 The fixation techniques for PCL avulsion fracture varies from arthroscopic techniques5 to open reduction and internal fixation (ORIF) with cannulated cancellous screws, Kirschner wires, and sutures anchors.6, 7, 8 Although the management of single, large, non-comminuted bony avulsion injury have shown universally good results after open or arthroscopic repair, the treatment of comminuted PCL avulsion injury remains controversial regarding the most optimal method.1,6, 7, 8, 9 Arthroscopic reduction of the comminuted fragment remains a challenge. Recently, few authors have described ORIF using suture anchors for comminuted PCL avulsion.10,11 Lee et al. used suture bridge technique to fix comminuted bony avulsion of PCL using ‘four’ anchors.
We described a suture bridge technique by using only two suture anchors to fix the comminuted avulsed PCL fragment and its results in ten patients.
2. Method
From May 2013 to April 2016, a total of 10 patients were operated for comminuted displaced bony avulsion of PCL from the tibial end by a standard posterior approach using suture anchors ‘suture bridge technique’. Nine were males and one female with mean age of 30 years (range, 21–42 years). The indication for surgery included; 1) isolated closed injury to the PCL and 2) displaced comminuted avulsion fracture of less than 2 cm. Periarticular and intraarticular knee injuries along with other collateral or anterior cruciate ligament injuries were excluded from the study. Three patients had additional fractures of shaft Femur, shaft Tibia and Femur and one had medial malleolus fracture. The diagnosis was confirmed by plain radiographs of the knee, computed tomography (CT) and Magnetic resonance imaging (MRI) [Fig. 1A, B]. The latter was done to exclude any additional soft tissue injury in and around the knee joint.
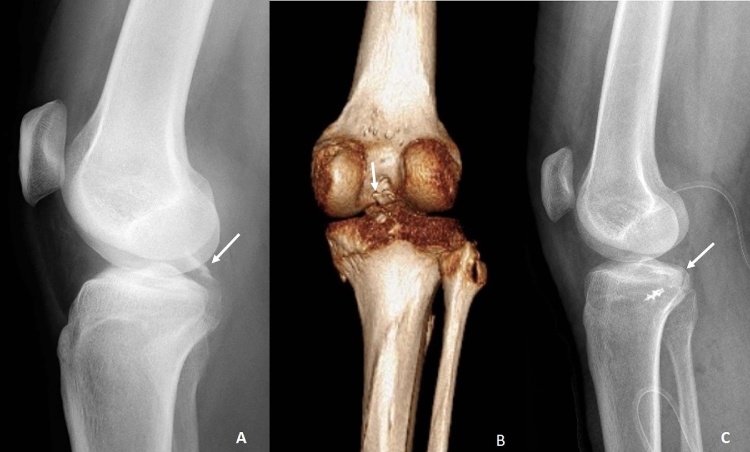
Fig. 1.
1A shows lateral radiograph of knee showing comminuted PCL avulsion fracture (white arrow). 1 B depicts the 3-D CT scan of the knee with comminuted PCL avulsion (white arrow). 1C shows an accurately reduced PCL avulsion fracture into the crater (white arrow).
2.1. Surgical technique
The surgery was carried out under spinal or general anesthesia under tourniquet control. The patient was positioned in a prone position with knee flexion of 20–300 achieved with the help of bolster pillow. After standard part preparation and draping, a lazy S-shaped incision was placed over the popliteal fossa with the superior limb proximal medial and inferior limb distal between two heads of Gastrocnemius (Fig. 2A). Deep fascia was incised in the line of the incision to reveal the medial cutaneous sural nerve lateral to the small saphenous vein in the distal aspect of the incision. The raphe between the medial and lateral head of gastrocnemius was identified and bluntly separated. The neurovascular bundle, with the popliteal artery being the deepest is identified and retracted laterally along with the lateral head of Gastrocnemius. Then the posterior capsule of the knee joint is identified and a vertical capsulotomy was performed to expose the avulsed PCL fragment. The fracture bed was debrided and washed to remove any free fragments and debris. A no.2 Ethibond suture (Johnson and Johnson, Ethicon, USA) was passed from the osseotendinous junction to hold and pull the fragment downwards (Fig. 2B). Then, a double loaded 5 mm titanium suture anchor with needles (Fastin RC 5 mm Orthocord w/Needles; DePuy Mitek Inc, Raynham, USA) was inserted into the bed of the fracture (Fig. 2C). The sutures were taken through the osseotendinous junction of the avulsed PCL fragment in a mattress fashion and tied while keeping the fracture reduced with the help of a dental hook and by the pull on the two limbs of ethibond suture. All four of the tied suture limbs or sometimes two of the tied suture limb and two limbs of Ethibond suture were then passed through the hole at the end of the another footprint suture anchor (Versalok anchor; DePuy Mitek Inc, Raynham USA or 4.5 mm Swivel lock, Arthrex, FL, Naples, USA) [Fig. 2D]. The pilot hole for the footprint anchor was made about 1 cm inferior to the distal edge of the fracture bed, and the anchor was inserted along with four sutures into the hole keeping the sutures manually tight, thereby giving the adequate compressive force of the fragment across the fracture bed (Fig. 2E). A ray diagram summarizes the key steps (Fig. 3). The posterior capsule was closed, and the wound was sutured in layers over a drain following which a compression dressing was applied.
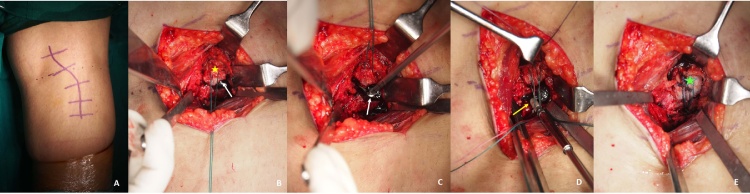
Fig. 2.
Posterior view of the popliteal fossa. (A) The lazy S incision over the popliteal fossa. (B) The fragment is held with an Ethibond suture (yellow star) and crater of the avulsed fragment is indicated by a white arrow. (C) Double loaded anchor is placed in the crater (white arrow). (D) After suture passage via osseotendinous junction of PCL- bone fragment and tied, the suture ends are passed via the footprint anchor (yellow arrow) and pushed below the crater. (E) Complete reduction of the fragment into the crater (green star). (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
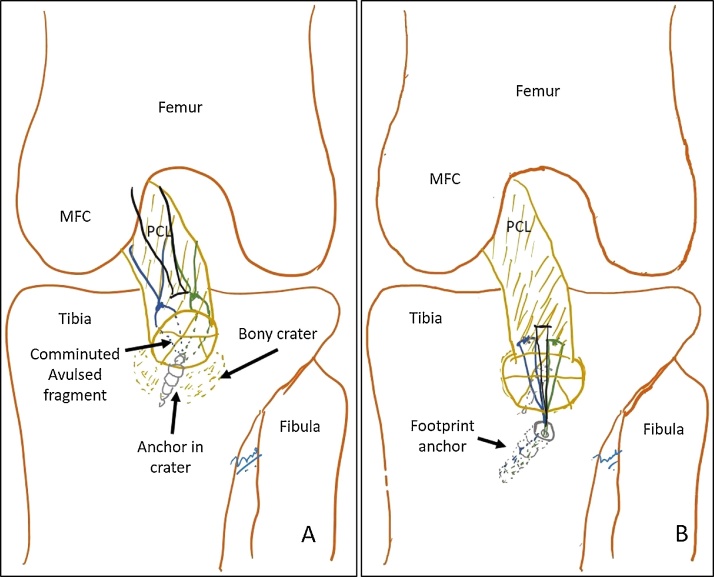
Fig. 3.
A self-explanatory ray diagram for the comminuted fragment fixation. Black suture color is the traction suture. PCL, posterior cruciate ligament; MFC, medial femoral condyle.
3. Post-operative imaging, rehabilitation and follow up
The plain radiograph confirms the accurate fixation in all the cases (Fig. 1C). The knee was immobilized in an extension knee immobilizer with a modification of posterior tibial support to prevent the posterior tibial sag. On the first post-operative day, the patient was taught static quadriceps strengthening exercises and non-weight bearing with bilateral axillary crutches. The drain is removed after 24 h. The knee was immobilized for three weeks. At three weeks, the active knee mobilization was started, but non-weight bearing was continued for another three weeks. Partial weight bearing was started after six weeks and full weight bearing at 10 weeks once fracture united. Patients were allowed to return to full activity at 4–6 months depending on the return of complete strength and movements. Plain radiograph were taken at 6 weeks, 3 months and then yearly. At the final follow up, the Lysholm and international knee documentation committee (IKDC) objective scoring was done to assess clinical performance. The complication of the procedure were noted, if any.
4. Results
The mean follow-up period was 12 months (range, 8–36 months). All patients had shown the radiological union of avulsion fracture at 12 weeks postoperative radiograph. At the final follow-up, all patients have regained full range of motion as compared to the normal knee without any flexion or extension deficit. The mean Lysholm score was 92 (range, 82–100) which was excellent. Seven out of ten (70%) patient showed grade 0 posterior drawer and 3 patients had grade 1 posterior drawer on manual testing. On objective international knee documentation committee (IKDC) score, 70% (n = 7) patient had IKDC grade A and 30% (n = 3) had IKDC grade B. There were no wound or implant related complications or transient neurological deficits.
5. Discussion
This study with suture bridge fixation of comminuted PCL avulsion by the standard open posterior approach in ten patients reports excellent outcome in short term follow up.
Both arthroscopic and open techniques have been used to fix the avulsed PCL fragment depending upon the expertise of the surgeon, but literature is limited suggesting the superiority of one method over the other.12, 13, [14] Arthroscopic PCL fixation is technically challenging, could be time consuming and difficult with a steep learning curve. In addition, arthroscopically it is often difficult to achieve accurate reduction of the widely displaced comminuted fragment.
Albeit the biomechanical properties of open reduction and various arthroscopic techniques are comparable in the case of single large avulsed PCL fragment, literature is limited in a definitive fixation technique for comminuted PCL avulsion fracture.13,14 High chance of further fragmentation of comminuted avulsion fracture occur when drilling, be it open or arthroscopically.15 Hence we decided to avoid this complication by taking a suture in the Osseotendinous junction and employing a suture anchor to achieve adequate compression.
The technique of suture bridge fixation, which was initially described in rotator cuff injuries has been expanded to other orthopedic injuries.16, 17, 18 Zhang et al. used two suture anchors to fix the avulsed PCL fragment11 but the typical suture bridge technique has been utilized by Lee et al. using a posteromedial approach and four suture anchors to achieve compression at the fracture site.10 However, Lee et al. have discussed only two cases with a follow-up of 6 months.10 Our series of ten patients shows excellent outcome in all cases at a mean follow-up of one year. Three patients had IKDC grade B due to residual grade 1 posterior drawer. In these patients, the fracture had united, but perhaps there might remain some posterior capsular laxity contributing to residual posterior laxity.
The significant advantage in the use of suture bridge technique is that it allows near anatomic reduction, even if the fragment is comminuted or small as it allows uniform compression. Since there is no drilling performed through the fragment and by taking the suture limb through the osseotendinous junction; there is no fear of further comminution of the fragment. This technique is a growth plate-sparing technique, as there is no drilling or passage of implant through the physis. In addition, the suture bridge technique can also be used to fix an old avulsion fracture where in the non-comminuted fragment may become osteoporotic and passage of a screw can fracture or fragment it further. Unlike cannulated screw, another advantage of this technique is that it does not require implant removal at a later date or does not interfere with any peri- or intraarticular knee reconstruction.
There are not many biomechanical studies to confirm an advantage in using a specific method for fixation of the PCL fragment. Domnick et al. in compared the biomechanical properties of various fixation techniques in vitro and suggested cortical suspension button, retrograde screw fixation, and suture cerclage technique have ‘comparable’ structure properties to the direct screw fixation technique.12
Sawyer et al. compared three techniques of fixation; namely screw fixation, suture fixation, suture bridge technique fixation and reported superior results of suture bridge technique regarding ultimate failure load in porcine models.19 It has been concluded that due to this fact, aggressive rehabilitation protocols and quicker progressive weight bearing is possible with suture bridge technique in the post-operative period.19 However, we continued with traditional slow rehabilitation protocol as a biomechanical study involving suture bridge technique has been reported recently. It may be assumed that in our technique, similar advantage holds true even though in vitro biomechanical and long-term functional outcomes are not available.
There is a disadvantage of suture bridge technique of increased cost incurred for this procedure given multiple suture anchors. However, we have used only two anchors as compared to four used by Zhang et al. which can keep the cost low.11 Nevertheless, it may be negated considering the less operative time, improved chance of healing and union rates with comminuted fracture, quicker rehabilitation and no need of implant removal at a later date.11
Conclusion: We find this technique to be useful and relevant in comminuted PCL avulsion fractures and can be extended to old avulsion fracture where the fragment might be osteoporotic. However, the influence of this technique on the functional and biomechanical outcomes of the knee has to be done in a large cohort of patients while comparing it with currently popular arthroscopic suture technique or open screw fixation.
Funding
None.
Conflict of interest
None.
Acknowledgement
None.
References
- 1.Chen L.B., Wang H., Tie K., Mohammed A., Qi Y.J. Arthroscopic fixation of an avulsion fracture of the tibia involving the posterior cruciate ligament: a modified technique in a series of 22 cases. Bone Joint J. 2015;97-B:1220–1225. doi: 10.1302/0301-620X.97B9.35765. [DOI] [PubMed] [Google Scholar]
- 2.Schulz M.S., Russe K., Weiler A., Eichhorn H.J., Strobel M.J. Epidemiology of posterior cruciate ligament injuries. Arch Orthop Trauma Surg. 2003;123:186–191. doi: 10.1007/s00402-002-0471-y. [DOI] [PubMed] [Google Scholar]
- 3.Bali K., Prabhakar S., Saini U., Dhillon M.S. Open reduction and internal fixation of isolated PCL fossa avulsion fractures. Knee Surg Sports Traumatol Arthrosc. 2012;20:315–321. doi: 10.1007/s00167-011-1618-6. [DOI] [PubMed] [Google Scholar]
- 4.Logan M., Williams A., Lavelle J., Gedroyc W., Freeman M. The effect of posterior cruciate ligament deficiency on knee kinematics. Am J Sports Med. 2004;32:1915–1922. doi: 10.1177/0363546504265005. [DOI] [PubMed] [Google Scholar]
- 5.Yoon J.R., Park C.D., Lee D.H. Knee Surg Sports Traumatol Arthrosc. 2016. Arthroscopic suture bridge fixation technique with multiple crossover ties for posterior cruciate ligament tibial avulsion fracture. [DOI] [PubMed] [Google Scholar]
- 6.Kim S.J., Shin S.J., Cho S.K., Kim H.K. Arthroscopic suture fixation for bony avulsion of the posterior cruciate ligament. Arthroscopy. 2001;17:776–780. doi: 10.1053/jars.2001.22392. [DOI] [PubMed] [Google Scholar]
- 7.Littlejohn S.G., Geissler W.B. Arthroscopic repair of a posterior cruciate ligament avulsion. Arthroscopy. 1995;11:235–238. doi: 10.1016/0749-8063(95)90075-6. [DOI] [PubMed] [Google Scholar]
- 8.Martinez-Moreno J.L., Blanco-Blanco E. Avulsion fractures of the posterior cruciate ligament of the knee. An experimental percutaneous rigid fixation technique under arthroscopic control. Clin Orthop Relat Res. 1988:204–208. [PubMed] [Google Scholar]
- 9.Choi N.H., Kim S.J. Arthroscopic reduction and fixation of bony avulsion of the posterior cruciate ligament of the tibia. Arthroscopy. 1997;13:759–762. doi: 10.1016/s0749-8063(97)90015-3. [DOI] [PubMed] [Google Scholar]
- 10.Lee K.W., Yang D.S., Lee G.S., Choy W.S. Suture bridge fixation technique for posterior cruciate ligament avulsion fracture. Clin Orthop Surg. 2015;7:505–508. doi: 10.4055/cios.2015.7.4.505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang X., Cai G., Xu J., Wang K. A minimally invasive postero-medial approach with suture anchors for isolated tibial avulsion fracture of the posterior cruciate ligament. Knee. 2013;20:96–99. doi: 10.1016/j.knee.2012.10.016. [DOI] [PubMed] [Google Scholar]
- 12.Domnick C., Kosters C., Franke F. Biomechanical properties of different fixation techniques for posterior cruciate ligament avulsion fractures. Arthroscopy. 2016;32:1065–1071. doi: 10.1016/j.arthro.2015.10.013. [DOI] [PubMed] [Google Scholar]
- 13.Sabat D., Jain A., Kumar V. Displaced posterior cruciate ligament avulsion fractures: a retrospective comparative study between open posterior approach and arthroscopic single-tunnel suture fixation. Arthroscopy. 2016;32:44–53. doi: 10.1016/j.arthro.2015.06.014. [DOI] [PubMed] [Google Scholar]
- 14.Sasaki S.U., da Mota e Albuquerque R.F., Amatuzzi M.M., Pereira C.A. Open screw fixation versus arthroscopic suture fixation of tibial posterior cruciate ligament avulsion injuries: a mechanical comparison. Arthroscopy. 2007;23:1226–1230. doi: 10.1016/j.arthro.2007.06.012. [DOI] [PubMed] [Google Scholar]
- 15.Gwinner C., Kopf S., Hoburg A., Haas N.P., Jung T.M. Arthroscopic treatment of acute tibial avulsion fracture of the posterior cruciate ligament using the TightRope fixation device. Arthrosc Tech. 2014;3:e377–382. doi: 10.1016/j.eats.2014.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park M.C., ElAttrache N.S., Tibone J.E. Footprint contact characteristics for a transosseous-equivalent rotator cuff repair technique compared with a double-row repair technique. J Shoulder Elbow Surg. 2007;16:461–468. doi: 10.1016/j.jse.2006.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Bowers A.L., Huffman G.R. Suture bridge fixation of a femoral condyle traumatic osteochondral defect. Clin Orthop Relat Res. 2008;466:2276–2281. doi: 10.1007/s11999-008-0357-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim K.C., Rhee K.J., Shin H.D., Kim Y.M. Arthroscopic fixation for displaced greater tuberosity fracture using the suture-bridge technique. Arthroscopy. 2008;24:120 e121–123. doi: 10.1016/j.arthro.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 19.Sawyer G.A., Anderson B.C., Paller D., Schiller J., Eberson C.P., Hulstyn M. Biomechanical analysis of suture bridge fixation for tibial eminence fractures. Arthroscopy. 2012;28:1533–1539. doi: 10.1016/j.arthro.2012.02.020. [DOI] [PubMed] [Google Scholar]