Abstract
Introduction
The management of pilon fractures is controversial primarily due to the high rate of complications irrespective of the mode of treatment. Limited internal fixation with external fixation is associated with minimal soft tissue handling. This may reduce the chances of wound dehiscence and infection. This study was designed to evaluate the functional and clinical outcomes in patients treated with limited internal fixation combined with external fixation in pilon fractures.
Material and methods
This study was conducted as a prospective clinical study on 56 skeletally mature patients with closed fractures with poor skin condition, and with open grade 1 and grade 2 distal tibial intra-articular fractures. All patients were treated with combined limited internal fixation and ankle spanning external fixation.
Results
All fractures in this series united with an average time period of union of 18.3weeks (ranging from 13 weeks to 30 weeks). There was no non-union in any case. There was malunion in 4 cases, varus malunion (>5 degree) in 2 cases and recurvatum in another 2 cases). Excellent to good functional results were observed in 88% cases based on the modified Ovadia and Beals score. The mean ankle dorsiflexion and planter flexion movements were 10.2±5.3 degrees and 27.4±7.2 degrees respectively. infections occurred in 6 patients which included 4 pin tract infections and 2 superficial wound infection, all 6 healed after removal of pin tract and with oral antibiotics.
Conclusion
The technique of combined external fixation with internal fixation is safe and effective management option for intra-articular distal tibial fractures.
Keywords: Distal tibia fracture, Pilon fracture, Limited internal fixation, External fixation, Open reduction and internal fixation
1. Introduction
Intraarticular distal leg bone fractures involving the weight bearing area of tibia are termed as pilon or tibial plafond fractures and constitute 1% of lower limb fractures and 7% of tibial fractures.[1], [2], [3], [7] These fractures result from high energy trauma in young patients with road traffic accidents or from low velocity trauma in elderly patients. High velocity trauma is often associated with intraarticular comminution, multiple metaphyseal fragments and soft tissue injuries, making their management challenging.7 The management of these fractures is under debate because of the associated high rates of complications irrespective of the mode of treatment chosen. The choice of treatment must take into account not only the stabilization of the fracture but also the management of the soft tissue injury.8 Management options includes manipulative reduction and cast application, open reduction and internal fixation with plates, fibular stabilization alone with plate or intramedullary implant, two staged management, primarily by external fixator followed by definitive internal fixation once skin condition becomes good, or by combined limited internal fixation with external fixation.[3], [4], [5], [6], [9], [14]
Conservative treatment with cast is often associated with joint stiffness, nonunion, malunion, secondary arthritis and reflex sympathetic dystrophy and has limited indications now adays.5 Open reduction and internal fixation is also associated with high rate of complications like wound dehiscence, infection and delayed union.[4], [7] Two staged treatment by initial primary ankle spanning fixator with or without fixation of fibula followed by delayed open reduction and internal fixation has the advantage of better soft tissue management. However, accurate anatomical reduction is technically difficult to achieve after three to four weeks of waiting for the skin condition to improve and often require extensive soft tissue dissection. Moreover, two surgeries lead to an increased cost and time of treatment which may not be applicable in developing countries which have limited resources and operating room facilities.[7], [8]
Limited internal fixation with external fixation associated with minimal soft tissue handling, leaving no large implant subcutaneously may lead to less chance of wound dehiscence and infection. With this approach pilon fractures with poor skin condition can be managed definitively early with good results.[8], [10]
Considering all these facts this study was conceived and designed so as to evaluate overall function and clinical outcomes of patients treated with this procedure and to discuss merits, demerits and cost effectiveness of this procedure.
2. Material and methods
This prospective clinical study was conducted on 56 patients with intra-articular fracture of distal tibia treated with combined limited internal fixation and external fixation by a single senior surgeon (MCB) at a tertiary trauma centre, over a period of four years. After exclusion of 6 patients (which were lost to follow up), a total of 50 patients were included for final outcome analysis with minimum of one year follow up. Ethical clearance was obtained from the institutional review board and patients were included after written informed consent was obtained.
Skeletally mature patients with closed fractures and poor skin condition and open grade 1 and grade 2 pilon fractures were included in the study. Patients with metadiaphyseal distal tibial fracture without intra-articular extension, open grade 3 fractures, pathological fractures and patients with multiple musculoskeletal injuries to same or opposite lower limb were excluded. All patients were subjected to a detailed history, clinical and radiological evaluation. Fractures were classified according to Ruedi and Allgover classification.4 Open fractures were classified according to Gustilo and Anderson classification.11 Surgery was undertaken within 2 weeks of being injured, depending on the general medical condition and fitness for anaesthesia.
2.1. Surgical technique and rehabilitation
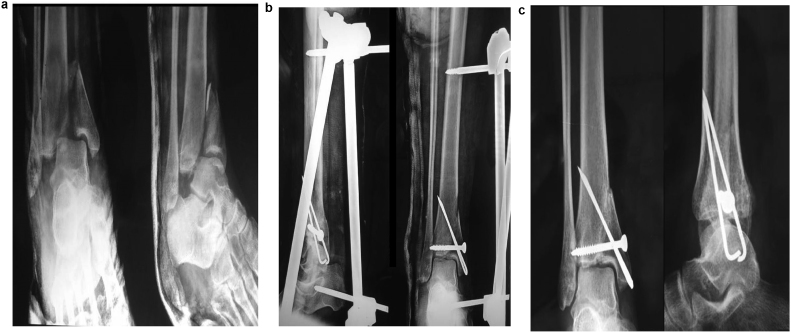
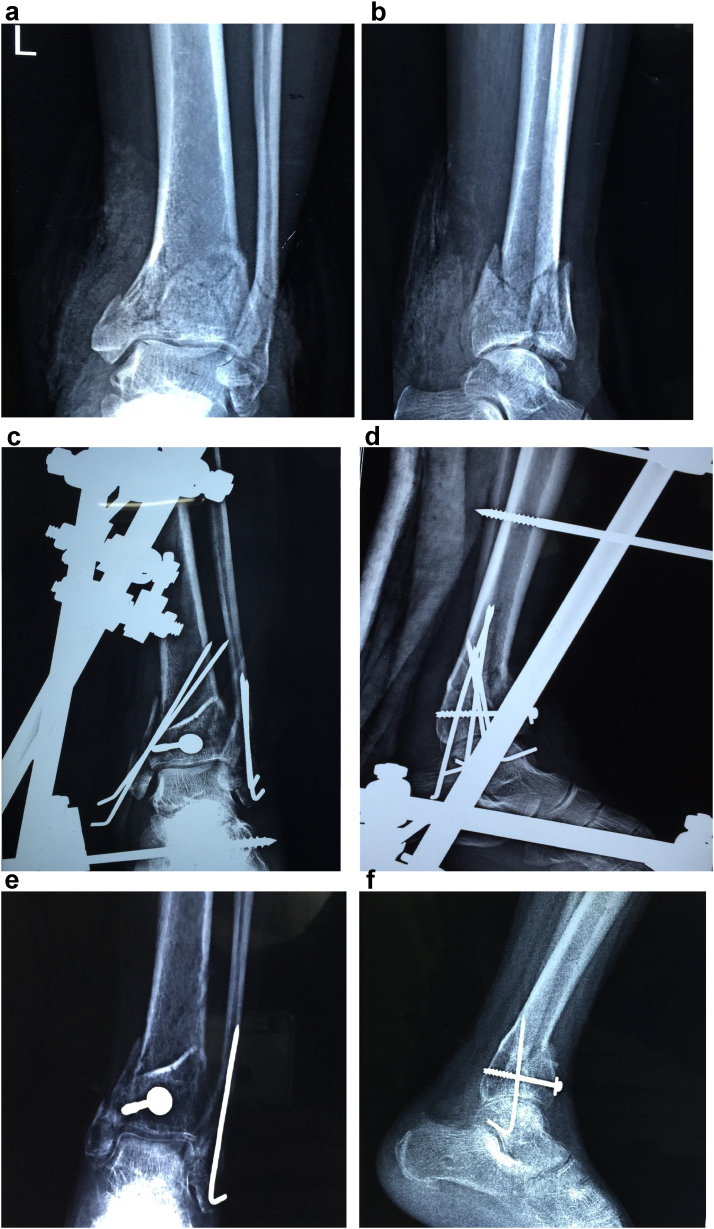
Under all aseptic precautions, patients were operated under spinal or general anaesthesia with patient in supine position on a radiolucent table under tourniquet control. Preoperative intravenous antibiotic (cefuroxime) was administered to all patients. A thorough debridement and wound irrigation was done in patients with open fractures. The fibula was fixed first after open reduction using 1/3 tubular plates in spiral or comminuted fibula fractures and by closed reduction and fixation with Rush pin or Kirschner wire (K-wire) in transverse fractures, to maintain the length and rotation of the limb. The tibial fracture was reduced under image intensifier using traction and manipulation. A 4.5 cm Steinmann pin or Denham’s pin was used inserted into the calcaneus was used for traction. The reduction was maintained by application of reduction clamps, inserted through stab (0.5 cm) skin incisions. Blunt dissection was done down to the bone using a straight hemostat and k wires and/or screws were used to fix each major periarticular fragment. If needed small curved periosteal elevators were inserted through stab incisions to elevate the depressed articular fragments. Two 4.5 mm Schanz screws were inserted in the tibia and connected to each other. The schanz screws were then connected to the calcaneal pin to complete the ankle spanning external fixator. Bone grafting using cancellous bone from the iliac crest of the same side was done as and when deemed necessary to fill up the metaphyseal void formed. Thus, the limited internal fixation was obtained by using K wires and/or screws and the fracture was stabilized using the ankle spanning external fixator (Figs. 1 b and 2c,d).
Fig. 1.
a,b,c Type 2 pilon fracture treated with combined internal and external fixation with good outcome.
Fig. 2.
a,b: Type 3 Pilon Fracture preoperative radiographs. c,d: Postoperative Radiographs showing fixation with combined approach. e,f: months follow up radiographs showing malunion and ankle arthritis.
Postoperative intravenous cefuroxime along with amikacin was given for three days. The limb was elevated on two pillows and patients were advised to do active toe movements. Wound was inspected after 48 h of surgery. Suture removal was done after two weeks of surgery. External fixator and k wire removal was done after radiological callus formation and a below knee cast applied subsequently for a period of 4 to 8 weeks depending upon signs of radiological and clinical union. Patients were allowed non weight bearing crutch walking after removal of the sutures and a decrease in the swelling. Partial weight bearing crutch walking was allowed after the below knee cast was applied and full weight bearing mobilization was allowed only after fracture union.
2.2. Follow up and functional outcome measures
All patients were followed up at 2 weeks, 6 weeks, 2–3 months, 6 months and at 1 year post operatively. A modified Ovadia and Beals criteria,12 was used to evaluate outcome at one year follow up. The modified Ovadia and Bealsscore range from two to five, with the final clinical grade categorized as excellent (5/5 points), good (4/5 points) (Fig. 1c), fair (3/5 points), or poor (2/5 points) (Fig. 2e,f) (Table 1). The range of movement of ankle was measured by a goniometer with the patient seated and the knee bent for plantar flexion and dorsiflexion.
Table 1.
Demographic profile of patients.
| Age | 39 years |
| Sex(M:F) | 40:10 |
| Mode of injury(RTA/FFH) | 28:22 |
| Involved side(Rt;Lt) | 28:22 |
| Fracture classification (Allgower and Ruedi) (Type1:2:3) |
12:18:20 |
| Fracture(Closed: open) | 36:14 |
| Associated injuries | 12 |
| Associated fibular fracture | 44 |
RTA: Road traffic accident, FFH: Fall from height.
3. Results
Of the 50 patients studied 40 were males and 10 were females, with age ranging from 19 to 62 years (Table 2). Road traffic accident was most common mode of injury (56%). Open injuries were seen in 28% of our patients. Ruedi-Allgower type 3 was most common fracture pattern (40%). Associated upper limb injuries were present in 4 patients and head injury was there in 8 patients. Associated fibular fracture was present in 88% of patients. Average injury to surgery interval was 3.2 days, most of patients (60%) were operated within 48 h of injury, and main cause of delay was severe soft tissue swelling or lack medical fitness for anaesthesia.
Table 2.
Modified Ovadia and Beals criteria for outcome analysis of ankle fractures [12].
| Rating | Ankle motion | Tibiotalar alignment | Tibial shortening | Limp | Pain |
|---|---|---|---|---|---|
| Excellent (5/5) | >75% of normal | Normal | Nil | None | None |
| Good(4/5) | 50–75% | Normal | Nil | None | Mild |
| Fair(3/5) | 25–50% | <5% | <1 cm | Occasional | Moderate |
| Poor(2/5) | <25% | >5% | >1 cm | Present | Severe |
minor infection occurred in 6 patients which included 4 pin tract infections and 2 superficial wound infections(Table 3), all 6 healed after removal of pin tract and oral antibiotics. There was no deep infection in any case.
Table 3.
Outcome analysis.
| Outcome variable | No. of patients |
|---|---|
| Duration of hospital stay | 8.4days(3–15days) |
| Time duration for union | 18.3 weeks(13–30weeks) |
| Complications | |
| Infection | 4(pin tract infection), 2(superficial wound infection) |
| Malunion | 2(varus alignment >5 °), 2(recurvatum) |
| Delayed union | 5 |
| Nonunion | Nil |
| Ankle stiffness | 2 |
| Wound dehiscence | Nil |
| Clinical scoring | |
| Excellent | 24(48%) |
| Good | 20(40%) |
| Fair | 4(8%) |
| Poor | 2(4%) |
| Ankle ROM: Dorsiflexion | 10.2 ± 5.3 ° |
| Planter flexion | 27.4 ± 7.2 ° |
Average time period for union was 18.3 weeks (ranging from 13 to 30 weeks). There was no nonunion in any case. There was malunion in 4 cases, varus malunion (>5°) in 2 cases and recurvatum in another 2 cases (Fig. 2e,f) (Table 3).
Excellent to good results were observed in 88% based on the modified Ovadia and Beals score. The mean ankle dorsiflexion and planter flexion movements were 10.2 ± 5.3° and 27.4 ± 7.2° respectively (Table 3).
4. Discussion
Controversy exists over treatment of pilon fractures and wide variations in management have been reported. Traditional treatment methods such as skeletal traction or immobilization in a cast are infrequently used nowadays, because they had unsatisfactory results including insufficient anatomical reduction and joint stiffness.[4], [5], [7]
Ruedi and Allgower in 1969 attempted open reduction and internal fixation in 84 fractures using their principles of Restoration of the correct length of the fibula, Reconstruction of the articular surface of the tibia, Cancellous bone auto-graft to fill the metaphyseal bone defects, and medial support by a buttress plate. While the quality of reduction was better with open reduction and fixation, these procedures were associated with an increased incidence of impaired wound healing and post-traumatic arthrosis.
In order to combine the benefits of ORIF (direct visualization and manipulation of fragments) with the advantages of external fixation (indirect reduction, soft tissue protection), a staged approach was introduced. The results of the two-staged procedure have been promising[16], [17] but there are several disadvantages in the two-staged procedures. Reduction may be difficult after two or three weeks after injury and minimally invasive surgery does not offer adequate visualization of every fragment with the limited exposure. The preliminary results of the two-staged procedure compare favourably with studies using external fixation alone. Both reported limited soft-tissue complications and satisfactory outcomes.[7], [8], [17]
To minimize the risk of postoperative complications, minimally invasive techniques and methods combining external fixation with minimally invasive fixation materials were developed. Various external fixation methods such as circular, unilateral, and hybrid fixators,[10], [13], [14] but it is difficult for an external fixator alone to reduce and maintain the reduction of the tibial articular surface. So we used combination of limited internal fixation with external fixation with minimal soft tissue handling to prevent complications.
The mean time of union in our series was 4.3 months which was comparable to previously published literature.[7], [10] Tornetta et al. observed 81% good to excellent results in their series using combined limited internal fixation with external fixation. This was better in our series (88%), probably due to exclusion of grade 3 open fractures in our series (Table 4).
Table 4.
Comparison of results with published literature. ORIF stands for open reduction and internal fixation.
| Number of patients |
Treatment Method |
Open fractures |
Infection | Union Time | Malunion | Non-union | Good outcome | |
|---|---|---|---|---|---|---|---|---|
| Mcferran et al 15 |
52 | ORIF | 21% | 17% | Not available | 6% | 4% | Not available |
| Tornetta et al.10 | 26 | Hybrid External fixator, minimal ORIF | Not available | 4% each for pin site and deep infection | 4.2 months | 4% | Not available | 81% |
| Papadokostakis et al. 7 |
179 | Ankle spanning Ext Fixation |
35% | 27% minor infection 2% major infection |
4.3 months |
13% | 7% | Not available |
| Sirkin et al. 16 | 56 | Two stage procedure | 39% | 5% | Not available | 3% | 6% | Not available |
| Present study | 50 | External fixation with minimal ORIF | 28% | 12% minor infection | 4.2 months | 8% | Nil | 88% |
Minor infection occurred in 6(12%) of our patients. The majority of minor infections occurred in relation to the pin tracks. No deep infection was observed in any of our patient. In metaanalysis by Papadokostakis et al. minor and major infection was observed in 11.7% and 3.9% cases respectively, treated with ankle spanning fixator with or without minimally invasive techniques.7 Mcferran et al. 15 observed 17% infection rate in 52 patients treated with ORIF for pilon fractures (Table 4). This technique of combined external fixator with minimal internal fixation associated with decreased deep infection, eliminate wound necrosis and skin slough but associated with higher rate of pin tract infection.
In the present series there were no soft tissue complications. Thus this technique of treating both closed and open pilon fractures may be considered in achieving desired bony alignment with minimal surrounding soft tissue damage. Closure of wound could be done in our cases without any skin tension which we believe was possible because of use of small stab incisions and minimal implants.
Papadokostakis et al. observed malunion in 13% and nonunion in 7% of pilon fractures treated with ankle spanning external fixator. Malunion and nonunion rate in our series were 8% and 0% respectively (Table 4), the probable reason of this decreased malunion was use of primary fibular fixation and minimal tibial fixation at the same time.
Satisfactory range of movement was observed in patients treated with combined external fixation with limited internal fixation in our series. This might be the result of joint distraction and stretching of the ligament during the period of immobilization thereby preventing compression and shortening of the ligaments which in turn may lead to stiffness and restriction of movement.7
Treatment of tibial pilon fractures continues to be challenging with no single treatment modality to be considered as the gold standard. Decisions should be taken not only on the basis of the clinical and radiographic situation but also on the basis of the expertise of the surgeon and this technique of combined external fixation with internal fixation is safe and an effective management option for intraarticular distal tibial fractures, especially associated with severe soft tissue compromise.
There are few important limitations in this study. A pre-operative CT scan of the ankle was not obtained which we retrospectively believe would have helped in proper planning of the surgery. Also, a randomized trial between the described technique and the other treatment modalities would have been more useful.
Conflict of interest
The authors have none to declare.
Source of support/funding
None
Author’s contribution
UKM − conceived the idea and co-wrote the paper. UKM and MCB–analyzed the notes, acquisition, analysis and interpretation of data and contributed to the discussion. RU and GCG–analyse the notes and contributed to the discussion. GCG & UKM − co-wrote the paper and revised it critically before submission.
Contributor Information
Mahesh Chand Bansal, Email: dr.maheshbansal@gmail.com.
Prateek Behera, Email: pbehera15@gmail.com.
Rahul Upadhyay, Email: drrahul.smc@gmail.com.
Gyan Chand Gothwal, Email: gcgothwal15@gmail.com.
References
- 1.Ries M.D., Meinhard B.P. Medial external fixation withlateral plate internal fixation in metaphyseal tibia fractures: a report of eight cases associated with severe soft-tissueinjury. Clin Orthop Relat Res. 1990;256:215–223. [PubMed] [Google Scholar]
- 2.Bourne R.B. Pylon fractures of the distal tibia. Clin Orthop. 1989;240:42–46. [PubMed] [Google Scholar]
- 3.Calori G.M., Tagliabue L., Mazza E. Tibial pilon fractures: which method of treatment. Injury. 2010;41:1183–1190. doi: 10.1016/j.injury.2010.08.041. [DOI] [PubMed] [Google Scholar]
- 4.Rüedi T.P., Allgöwer M. The operative treatment of intraarticular fractures of thelower end of the tibia. Clin Orthop. 1979;138:105–110. [PubMed] [Google Scholar]
- 5.Ayeni J.P. Pilon fractures of the tibia: a study based on 19 cases. Injury. 1998;19:109–114. doi: 10.1016/0020-1383(88)90085-x. [DOI] [PubMed] [Google Scholar]
- 6.Tarkin I.S., Clare M.P., Marcantonio A., Pape H.C. An update on the management ofhigh-energy pilon fractures. Injury. 2008;39:142–154. doi: 10.1016/j.injury.2007.07.024. [DOI] [PubMed] [Google Scholar]
- 7.Papadokostakis G., Kontakis G., Giannoudis P., Hadjipavlou A. External fixation devices in the treatment offractures of the tibial plafond. A systematic review of the literaturE. J Bone Joint Surg Br. 2008;(90-B):1–6. doi: 10.1302/0301-620X.90B1.19858. [DOI] [PubMed] [Google Scholar]
- 8.Pugh K.J., Wolinsky P.R., McAndrew M.P., Johnson K.D. Tibialpilon fractures: a comparison of treatment methods. J Trauma. 1999;47:937–941. doi: 10.1097/00005373-199911000-00022. [DOI] [PubMed] [Google Scholar]
- 9.Whittle A.P. Fractures of lower extremty. In: Canale S.T., editor. Campbell’s Operative Orthopaedics. 9th ed. St Louis; Mosby: 1998. pp. 2057–2066. [Google Scholar]
- 10.Tornetta P., 3rd, Weiner L., Bergman M. Pilon fractures: treatment with combinedinternal and external fixation. J Orthop Trauma. 1993;7:489–496. doi: 10.1097/00005131-199312000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Gustilo R.B., Mendoza R.M., Williams D.N. Problems in management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma. 1984;24:742–746. doi: 10.1097/00005373-198408000-00009. [DOI] [PubMed] [Google Scholar]
- 12.Ovadia D.N., Beals R.K. Fractures of the tibial plafond. J Bone Joint Surg. 1986;68:543–551. [PubMed] [Google Scholar]
- 13.Bone L., Stegemann P., McNamara K., Seibel R. Externalfixation of severely comminuted and open tibial pilonfractures. Clin Orthop Relat Res. 1993;292:101–107. [PubMed] [Google Scholar]
- 14.Marsh J.L., Bonar S., Nepola J.V., Decoster T.A., Hurwitz S.R. Use of an articulatedexternal fixator for the fractures of the tibial plafond. J Bone Joint Surg Am. 1995;7:7–A. doi: 10.2106/00004623-199510000-00004. [1498-509] [DOI] [PubMed] [Google Scholar]
- 15.McFerran M.A., Smith S.W., Boulas H.J., Schwartz H.S. Complications encounteredin the treatment of pilon fractures. J Orthop Trauma. 1992;6:195–200. doi: 10.1097/00005131-199206000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Sirkin M., Sanders R., DiPasquale T., Herscovici D., Jr. A staged protocol for softtissue management in the treatment of complex pilon fractures. J OrthopTrauma. 2004;18:S32–8. doi: 10.1097/00005131-200409001-00005. [DOI] [PubMed] [Google Scholar]
- 17.Okcu G., Aktuglu K. Intra-articular fractures of the tibial plafond. A comparisonof the results using articulated and ring external fixators. J Bone Joint Surg. 2016;Br2004(86):868–875. doi: 10.1302/0301-620x.86b6.15077. [DOI] [PubMed] [Google Scholar]