Abstract
Introduction
Nowadays, liposuction is the most frequently performed aesthetic surgery procedure in Western Countries. This technique has had rapid development since the 1970s, when it was experimented for the first time by A. and G. Fischer. It is currently widely used in clinical practice for many different situations in aesthetic, reconstructive and functional fields.
Materials and methods
This review aims to describe the historical evolution of liposuction by analyzing the transformation of the method in function of the introduction of innovative ideas or instruments. We have also focused on reporting the major clinical applications of this surgical technique, applicable to almost the entire body surface. We finally analyzed the complications, both major and minor, associated with this surgical technique.
Results
Liposuction is mainly used to correct deep and superficial fat accumulations and remodel the body contour. It has become an essential complementary technique to enhance the aesthetic result of many other aesthetic procedures such as reduction mammoplasty, abdominoplasty, brachioplasty, thigh lift and post bariatric body contouring. However, it can be largely used for the treatment of innumerable pathologies in reconstructive surgery such as lipomas, lipedema, lipodystrophies, pneudogynecomastia and gynecomastia, macromastia e gigantomastia, lymphedema and many others. The complication rate is very low, especially when compared with conventional excisional surgery and the major, complications are generally associated with improper performance of the technique and poor patient management before and after surgery.
Conclusion
Liposuction is a safe, simple and effective method of body contouring. It has enormous potential for its application in ablative and reconstructive surgery, far from the most common aesthetic processes with a very low complication rate.
Keywords: Liposuction, Suction assisted lipectomy, Liposuction outcome, History of liposuction
Highlights
-
•
Liposuction techniques are noteworthy evolved during the last two decades.
-
•
This review deals with major indications and clinical application of liposuction.
-
•
Minor and major complications of this operative technique are also described and analyzed.
1. History
Liposuction is a very common cosmetic procedure: a safe, simple and effective method of body contouring. The first attempt to remodel the body silhouette dates back to 1921, when Dr. Charles Dujarrier wanted to improve the shape of the ankles and knees to a dancer patient. He removed a large part of skin and soft tissue, with a broad subcutaneous dissection and long skin incision. The result was tragic because of an excessive removal of tissue and suture too tight and live. This caused necrosis and amputation [1], [2].
After that, many other attempts are followed with less tragic results, with en bloc resection of both fat and skin to recontour outer thigh adiposity. Several complications such as hematoma, long-term seroma, necrosis, infections, and many post-operative body deformities burdened this technique [3], [4].
In 1972, the German physician Schrudde published a new less invasive technique to remove subcutaneous fat, using a uterine curette in a “sharp” technique of subcutaneous surgery. Several other surgeons used this technique through the mid 1970's: Kesserling and Meyer [5], in 1976, used a large, double blade cutting curette connected to a low-power aspirator to suck the fat, previously separated from the deep plane by scissors. This “sharp” technique restricts its use only to poorly vascular regions to limit the complications, which are already high [6], [7].
In 1975, Arpad and Giorgio Fischer [8], father and son cosmetic surgeons, developed the modern technique of liposuction. They was the first to introduce blunt hollow cannula attached to a suction source and the criss-cross suctioning technique from multiple incision sites. This “blunt” method allowed obtaining better and more predictable aesthetic results with much less complications. The Fischer applied their method only to outer thigh adiposity [9].
Illouz and Fournier, two Parisian surgeons, modified and popularized the Fischer's technique. In 1977, Illouz [10] developed modified equipment for performing liposuction and extended technique to the whole body. He introduced blunt cannulas of smaller diameter to reduce the section of nerves, lymphatic vessels and blood vessels. He used three different size of blunt-tipped cannulas depending on the area to be aspirated: the larger (10 mm) for the flanks, hips and buttocks, the middle one for knees, ankles, abdomen and the smaller for the face.
To make the technique less traumatic and reduce hemorrhagic risk, he gradually developed the “wet technique”, based on the injection of saline solution and hyaluronidase into the fat performing a hydrodissection before the liposuction procedure.
The hydrotomy allowed preserving the neurovascular bundles, the enlargement of the deep adipose layer that needs to be aspirated. This make easer for the surgeon preserving the superficial flap and removing only the deep layer [11].
Fournier, who also worked in Paris, was initially a supporter of the “dry technique”, in which no fluid was injected before the procedure, considering it more precise and accurate. However, experience has led it to abandon this approach in favor of local lidocaine infiltration and eventually the tumescent technique, recognizing the bleeding advantages.
He has also strongly supported the need for taped compression to support and shape the suctioned tissue, during the post-operative period.
However, the greatest merit of Fournier was to travel the world teaching others this technique and inspiring those [12].
Lawrence Field, a Californian based dermatological surgeon, visited and studied this evolving technique in 1977. He was probably the first American to visit France and learn the new technique of liposuction from the Italian and French pioneers [13], [14].
After that, in the early 1980s, many other surgeons traveled to France to study this procedure. The blunt cannula technique came to be the accepted liposurgical method in this country and around the world, and in 1982, the American Society of Lipo-Suction was formed to bring surgeons from both the United States and foreign countries into one group to establish a teaching program [15], [16].
Furthermore, by 1984, liposuction training was available in some dermatology and plastic surgery residency program [17], [18].
Throughout this period, liposuction surgery was mostly performed under general anesthesia.
Dermatologists were very interested in performing the process in local anesthesia. Therefore, they started to combine a slight preoperative sedation with local lidocaine infiltration. However, the possible applications were limited by the maximum recommended local anesthetic dosage to few cases with small areas to be treated.
In 1987 Jeffrey Klein, a Californian dermatologist, first reported on the use of large volumes of very dilute anesthesia which allowed liposuction to be performed in larger volumes completely under local anesthesia without the need of sedation or general anesthesia. Klein invented a recipe consisting of 0.05% lidocaine, 1:1,000,000 epinephrine, and 10 mL sodium bicarbonate per liter of saline, which could be infused into tissue prior to liposuction [19].Klein also demonstrated that the same dosage of lidocaine diluted in a large volume of fluid allowed obtaining a good degree of anesthesia even on large areas, without evidence of systemic toxicity.
Moreover, the presence of epinephrine produced an important vasoconstriction which greatly reduces bleeding during the procedure, which was a major liposuction problem prior to Klein's development [20], [21].
Lillis demonstrated that the Klein's tumescent technique offered significant reduction in blood loss, even in suction case of over 3L. He verified, also, that Klein's work demonstrating minimal plasma absorption of lidocaine when low concentration solutions were infused [22], [23].
Furthermore, performing liposuction without general anesthesia offered other different advantages like reduction of hospitalization, costs and risks of anesthesia.
The main disadvantage of this method is that infiltration of the anesthetic takes a significant length of time. In addition, the cannulas used to extract the fat need to be somewhat finer in diameter to be tolerated by the patient and hence the time to remove a given volume of fat is lengthened compared with general anesthesia [24].
Liposuction was born as a suction technique by means a vacuum pump [25]. However, the Brazilian Luiz Toledo, in 1988 [26], experienced the use of disposable syringes of different gauges and size for aspiration of adipose tissue. The main advantage was a wider freedom of movement for the operator during the procedure, making surgery simpler and easier. In addition, the syringes allow you to know precisely the amount of local anesthetic that has been infiltrated before the procedure and the exact amount of fat removed from each area, all data which are just approximate with the use of the lipoaspirator. Toledo also proposed creating a patient's body map to ensure symmetry as much as possible. A nurse marked exactly the amount of injected local anesthetic and fat tissue removed from each body area to improve as much as possible the aesthetic result and symmetry [27].
The main advantage of syringe liposuction is, therefore, the precision and accuracy in measurement of adipose harvested volumes, in addition to the possibility of injecting fat. The vacuum-pump assisted liposuction makes the surgical procedure more comfortable and less tiring for the surgeon, especially in case of large amounts of fat to be removed. Therefore, the vacuum pump assisted liposuction was usually chosen for major lipoplasty procedures, in which quantity of fat to be removed is a priority over the topographic, symmetric, precise distribution of fat harvest [28].
Ultrasonic liposuction was introduced by Zocchi, in Italy, in 1992 [29] as an alternative to conventional blunt cannula suction. Zocchi credits Scuderi for the original concept of lipo-exeresis [30].
This technique is based on the application of ultrasounds to the fatty tissue to be aspirated, resulting in both thermal effects and mechanical effects to the surrounding adipocytes. These mechanical oscillations pass through the cannula that emits the waves from its tip. The thermal effects play a role in fat dissolution and must be dissipated by tissue infiltration [31], [32].
In this way, Zucchi tried to make aspiration easier and to preserve the neurovascular structures, which can be destroyed by the cannulas.
Zocchi detailed what he believed were the advantages of Ultrasonic technique over traditional liposuction: a more selective destruction of the undesired tissue while preserving surrounding higher-density structures; elimination of the “fluid part” of the adipose tissue (fatty acids), leaving the adipocyte wall and intercellular substance to create a smooth skin surface; skin contraction secondary to stimulation of the dermis by ultrasonic energy; correction of cellulite; once the fat is dissolved with ultrasound, the procedure requires less physical exertion on the part of the surgeon [29], [33].
Ultrasonic liposuction was embraced initially in South American and Europe and then largely rejected after experience with skin sloughs, burns, and seromas [34].
Laser-lipolysis began to spread after the publication of the studies about the interaction between laser and adipose tissue, conducted by Apfelberg [35] and Apfelberg et al. [36], [37] in 1992.
Laser-assisted liposuction represents a relatively recent advancement in the treatment of lipodystrophies and irregularities of adipose tissue. The laser beam is directly propagated to adipose tissue with which it keeps a direct contact. The action of the laser causes the rupture of the adipocyte membrane and consequent release of oily content into the extracellular fluid. Complications and results of laser-assisted liposuction are similar to those obtained with the majority of liposuction techniques. In addition to the cytolitic effects on adipocytes, the laser can cause neoformations and remodeling of the collagen and reorganization of the reticular dermis. It is particularly indicated for localized areas of lipodystrophy in the body or face [2], [38].
2. Indications
Liposuction is the most performed aesthetic surgery in the world. It is mainly used to correct deep and superficial fat accumulations and remodel the body contour. It has become an essential complementary technique to enhance the aesthetic result of many other aesthetic procedures such as cervicoplasty, reduction or augmentation mammoplasty, abdominoplasty, brachioplasty thigh lift and postbariatric body contouring.
It now seems to have enormous potential for its application in ablative and reconstructive surgery, far from the most common aesthetic processes [39] (Table 1).
Table 1.
Summary of the main functional and therapeutic indications.
| Main indications of liposuction procedure | |
|---|---|
| Lipoma and Multiple lipomatosis | Muscocutaneous or fasciocutaneous flaps management |
| Lipedema and Lipodystrophy syndromes | Scar revision |
| Insulin-induced lipodystrophy | Genital area and Sexual dysfunction |
| Hiv-associated cervicodorsal lipodystrophy | Tracheostomy, Colostomy, and Urostomy management |
| Gynecomastia, Macromastia and Gigantomastia | Axillary hyperhidrosis |
| Postbariatric body contouring | Aesthetic body contouring |
One of the first non-cosmetic clinical applications of liposuction was the aspiration of a large lipoma without leaving a visible scar [10].
Lipomas are the most common benign tumor of soft tissues and have very variable dimensions. Simple surgical excision remains the main and most effective treatment, however, removal of large or multiple lesions may be problematic and result in significant objectionable scars [40].
However, the removal of bulky lipomas or multiple lipomas through liposuction has been described in the literature [40], [41], [42]. The disadvantage of this technique lies in the frequent incomplete resection and at a high recurrence rate associated with it [41].
The small liposuction incision can also be located in a less visible area than the area affected by the lipoma, so you can choose the less visible region where to position the scar. Furthermore, in the case of multiple lipomatosis, it is possible to remove more injuries with a single incision, the healing of the small incision is rapid, and there is a minimal postoperative discomfort [43].
Liposuction can also be a useful solution for the treatment of the multiple-lipoma syndromes and familiar multiple lipomatosis associated with some genetic pathology [44], [45].
Lipedema is characterized by bilateral symmetrical and localized subcutaneous fat deposits of the buttocks and lower limbs. It causes significant physical disability, fatigability, pain, difficulty in wearing shoes and boots [46].
Diet and exercise, even if performed correctly, are not enough to reduce the disproportion between the upper and lower body. Indeed, sometimes, they make the anesthetic dispensation more noticeable, as the patient slides only in the upper body of the body [47], [48]. Skin and subcutaneous excision significantly improve the size and shape of the limbs; however, it may be associated with severe complications. Suction-assisted lipectomy may be a good surgical option given the diffuse nature of lipedema adipose hypertrophy and it may be combined with limited skin and subcutaneous tissue excision in cases of persistent redundant skin [48], [9].
In these patients, liposuction provides good aesthetic results, improving the proportion between the upper and lower body and, also, it reduces painful symptoms, especially at the lower limb articulations, ensuring better mobility [50].
Lipodystrophies represent a group of rare diseases characterized by selective body fat loss with altered body fat amount and/or repartition that can be either generalized or partial. Lipodystrophies are usually associated with insulin resistance, type 2 diabetes, dyslipidemia, liver steatosis, polycystic ovaries, acanthosis nigricans, and cardiovascular complications [46], [50].
Treatment of lipodystrophies is difficult. Lifestyle is generally very helpful in controlling the disease but not enough. Aesthetic surgery is essential to improve the body contouring, especially in areas where there has been loss of adipose tissue [51]. The only therapeutic options for controlling the metabolic disorder are insulin sensitizers, insulin, and lipid-lowering drugs. Autologous adipose tissue transplantation or implantation of dermal fillers can improve facial appearance and excess adipose tissue from the chin, buffalo hump, and vulvar region can be surgically excised or removed by liposuction [46], [52].
In addition, hypertrophic insulin lipodystrophy may benefit from suction-associated lipectomy. It occurs frequently in the sites of multiple insulin injections in diabetic patients causing functional and aesthetic disorders including pain, reduction of treatment efficiency, hematoma and edema [53], [54].
Cervicodorsal lipodystrophy is another secondary lipodystrophy in which liposuction is needed to achieve satisfactory results. It is a side effect of some drugs including the corticosteroids (Cushing's syndrome) and human immunodeficiency virus (HIV) medications [55], [56].
Liposuction subcutaneous mastectomy is the initial surgical approach of choice for pneudogynecomastia and gynecomastia. In pseudogynecomastia, there is an increased development of the fatty component in the male breast region. In true gynecomastia, however, there is an increase in volume of the male breast gland with a dense fibrous and vascular stroma, which makes suction more difficult. The gynecomastia liposuction treatment is usually associated to a resection under direct vision of the glandular tissue through a periareolar or transareolar incision. After that, compression dressing and limited activity are necessary for several days to minimize bruising and hematoma formation allowing the skin to adhere to the chest in a favorable position [57], [58], [59].
In female macromastia and gigantomastia, there is an important increase in breast fat component. Bulky and heavy breasts often cause significant symptoms such as neck and back pain, dermatitis and skin irritations. Liposuction combined with traditional resection mammoplasty allows volume reduction before excision and refining the results after the reconstruction with an easier surgical procedure and better aesthetic results [60], [61], [62].
Lymphedema is a condition with a wide range of etiologies; the most common cause is the removal of one or more lymph nodes stations for neoplastic disease. Consists in the accumulation of lymphatic fluid in the dermis and subcutaneous tissues, due to a blockage of the lymphatic flow. Chronically accumulated lymphatic fluid causes cutaneous dermal thickening, hypercellularity, and progressive fibrosis. Secondary to restricted lipid transport from limited lymph flow, lipids accumulate in adipocytes and macrophages, resulting in increased adipose tissue [49], [63], [64], [65].
In chronic lymphedema, the increase in volume of the area is mainly due to the accumulation of adipose tissue and not fluid. For this reason, conservative therapies and lymphatic flow regeneration are not effective at this stage. Before it is necessary to surgically remove the bulky subcutaneous tissues. Traditional surgical excision, however, causes unacceptable complications and scar and often the result is unsatisfactory, liposuction provides good aesthetic and functional long-term results with a minimum complications rate [66], [67], [68].
It is important to emphasize that liposuction alone cannot eliminate the tendency to accumulate fluids and fat tissue, therefore it must always be associated with conservative therapies and lymphatic flow regeneration [64], [66], [67], [68].
Muscocutaneous or fasciocutaneous flaps are widely used successfully for the reconstruction of a wide variety of defects. In many cases, the flaps are set up to a greater extent than necessary, in the sense of having enough tissue for the recoating, resulting in unsatisfactory aesthetic results.
Surgical review in a second time is needed to remodel the flap, especially at certain body areas such as the ankles, knees, feet and breast, to obtain a better aesthetic result and to improve the functionality of that area. Liposuction allows thinning the subcutaneous tissue usually without the risk of flap necrosis and reduces the number of revision procedures required to achieve optimal aesthetic and functional result [69], [70].
Other less common clinical applications include axillary hyperhidrosis [71], [72], [73], revision of surgical scars [74], [75], [76], sexual dysfunctions and genital area (e.g. the “buried” penis in fatty men) [77], [78].
Liposuction is also used to facilitate tracheostomy, colostomy and urostomy in great obese patients, in which the stoma could be occluded by excessive fatty tissue surrounding [79], [80], [81].
3. Surgical technique
Before the surgery it is important preparing for surgery by marking. Areas to be suctioned are typically marked with a circle in a topographic pattern. Zones of adherence and areas to avoid are marked with hash marks [82].
Areas that can be suctioned effectively include the face, chin, neck, anterior and posterior axillary areas, arms, breasts, abdomen, waist, hips, buttocks, thighs, knees and ankles.
The current options for anesthesia are dry, wet, superwet, and tumescent. The essential differences between these techniques focus on the amount of infiltrating solution injected into the tissues and the resultant blood loss as a percentage of aspirated fluid. The dry technique involves no infused fluid and results in approximately 25–40 percent blood loss of the volume removed. Blood loss has been estimated to represent approximately 1 percent of the liposuction aspirate volume for both tumescent and superwet techniques [83], [84].
Klein's tumescent technique has been gradually embraced by all medical specialties [4], because of the advantages including especially bleeding reduction [20], [21].
With awake tumescent liposuction, the patient is able to drink normally the night before and the day of surgery, eliminating the need to replace deficits after important bleeding, avoiding the risks of postoperative overhydration or underhydration [85].
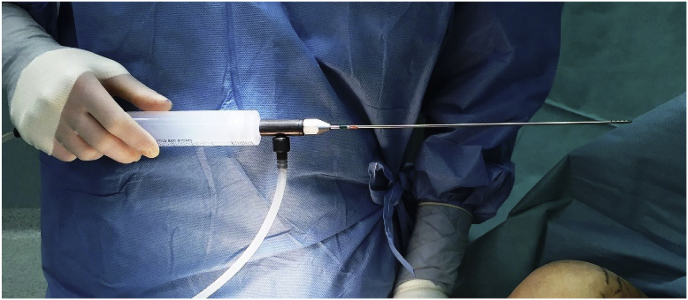
The Klein's solution, consisting of 0.05% lidocaine, 1:1.000.000 epinephrine, and 10 mL sodium bicarbonate per liter of saline, is infused into tissue prior to liposuction [19] by blunt multi-hole cannulas (Fig. 1, Fig. 2). This helps avoid damage to the surrounding tissues, and this means less postoperative edema and ecchymoses [39]. Tissue blanching and moderate tension are considered clinical endpoints of infiltrate [84].
Fig. 1.
Suction cannula collected to vacuum pomp.
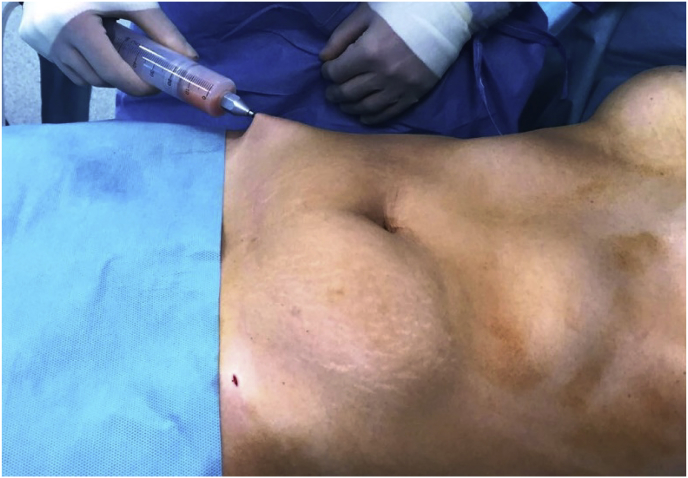
Fig. 2.
Klein's solution infiltration.
Small incisions are performed in different places depending on the area to be treated, but always designed to hide the small surgical scar [16].
For example, the chin and neck can be approached through a small incision placed in the submental crease, posterior lobular crease, or in the nasal vestibule. These incisions are limited to 5–10 mm and are made within relaxed skin tension lines. They are well hidden and allow excellent access to the cervicofacial region [39].
An abdominal procedure could be approached through three or four incisions. Two incisions are suprapubic, at the lower abdominal fold and another incision is placed over the umbilicus. Other incisions can be placed under the breast or through an existing scar. Of course, different situations require different incisions [16], [39].
The cannula is inserted with the opening away from the skin, and the adipose tissue is broken loose from the fibrous stroma with multiple crisscross movements. These movements create tunnels in the subcutaneous flap of the area [16] (Fig. 3, Fig. 4).
Fig. 3.
Harvesting abdominal fat.
Fig. 4.
Harvesting fat collected in the syringe. This allows to precisely knowing the exact quantity of adipose tissue aspirated. In this picture is possible to note the different between the right abdomen, in which the liposuction has already been performed, and the left abdomen.
The deep and/or intermediate fat layer should be suctioned primarily [86], but in rare cases, superficial or subdermal liposuction may be appropriate [85], [86], [87].
Anatomical “zones of adherence,” present in both men and women, are important to identify preoperatively. These are areas with relatively dense fibrous attachments running to the underlying deep fascia where they help define the natural shape and curve of the body. These areas are not to be suctioned because of the high potential for contour deformities [85], [86], [87], [88].
For the body 2–4.6-mm cannulas with lengths from 15 to 45 cm are used according to the areas to be treated. For the face and other delicate work 10-ml syringes and cannula gauges between 1 and 3 mm are preferred [39].
The dominant hand directs the cannula, with the other hand used as a guide for this blind procedure [16].
Liposuction is generally performed by two methods: the syringe method and the power pump method. Small volume procedures or procedures primarily for harvesting fat can be performed with syringe liposuction. The syringe technique used blunt-tip suction cannulas connected to a syringe. Drawing back the syringe plunger generates the negative pressures needed to remove fat during liposuction and replaces the electric vacuum pump and connecting tubing traditionally used for this procedure [26], [27], [89], [90].
Following extraction, the multiple tunnels created by the cannula form a “honeycomb” inside the suctioned area that allows the skin to adhere to its new profile following surgery. Pressure bandages occlude the tunnels by collapsing the remaining fat into the spaces of the honeycomb [12].
4. Complications
With appropriate patient selection and minimally traumatic techniques, many complications can be avoided.
True complications that are possible include contour defects, permanent skin color changes, infection, emboli, hematomas, or seromas.
The presence of ecchymosis depends on the localization and size of the treated area, the length of the procedure and individual factors. Edema is very common and generally persists for several weeks, in some venous areas such as ankles and calves may persist for six months or a year [2].
Hyperesthesia and dysesthesia are common sequelae of the procedure, which will gradually improve in three to six months after surgery. Hyperpigmentation is relatively infrequent condition and when it shows up it diminishes gradually, and in more serious cases, it responds well to treatment with topical agents [2].
Overly aggressive liposuction can lead to seromas. The collection of serous fluid in a treated area may lead to extensive breaking of the fibrous tissue network, leading to the formation of a single cavity [91].
Infection is extremely uncommon (<1 percent incidence). This may be because of a combination of sterile technique, small incisions, and the antibacterial effects of lidocaine [92].
The most common postoperative complication is contour irregularities, with an incidence of 2.7% [93].
Using small cannulas, not performing superficial liposuction, turning the suction off when exiting incisions, crisscrossing areas, constantly analyzing areas (visual and tactile), and proper positioning can all help reduce the chance of contour irregularities. Autologous fat transfer at the time of surgery or 6 months postoperatively can be used to help correct deformities [85].
Grazer and De Jong [94] reported a fatality rate of 19.1 per 100,000 liposuction procedures. The most frequent potentially lethal complications associated with liposuction are pulmonary embolism, fat embolism, sepsis, necrotizing fasciitis, and perforation of abdominal organs. The most frequent cause of death was deep venous thrombosis (DVT) associated with pulmonary embolism (23.1%). The risk of DVT is associated with blood flow stasis, trauma and possible hypercoagulation status. Intermittent compression devices for legs, early mobilization and the use of low molecular weight heparins can reduce the risk.
Abdominal and bowel perforations are reported as the second commonest lethal event (14.6%). To reduce the risk of perforation, the cannula tip has always to be accompanied by the palm, in particular in obese patients, in whom it is difficult to visualize the cannula, and the position should be hyperextension of the abdomen and severe abdominal pain should always suggest the occurrence of a possible perforation, which may require a laparotomy [2], [93], [94].
In 10% of cases, the death was caused by the use of local anesthesia, sedation and other medications.
Bleeding, formerly the most relevant cause of death due to lipoaspiration, represents just a 4.6% of lethal events [95].
Major risk factors for the development of severe complications are multiple procedures, poor standards of sterility, excessive infiltration and intoxication from lidocaine or adrenaline, excessive removal of adipose tissue with volume depletion in the third space, permissive postoperative discharge, and selection of unfit patients [92].
Furthermore, when tumescent infiltration of large volumes of dilute lidocaine and epinephrine are combined with intravenous fluid replacement and general anesthesia, there are significantly increased risks of fluid overload, pulmonary edema, and drug interaction [96].
5. Conclusions
After more than 40 years of being born, liposuction is currently one of the most accomplished aesthetic interventions around the world.
Surgical technique is simple and has a very low complication rate. However, if you want to get good aesthetic results and want to avoid the greatest possible complications you need a good technical study and a great experience (Fig. 5, Fig. 6).
Fig. 5.
Body remodeling of the left axillary pillar in a 53 years old patient, after oncologic breast reconstruction. Pictures before and after liposuction procedure.
Fig. 6.
Body remodeling of the left axillary pillar in a 53 years old patient, after oncologic breast reconstruction. Pictures before and after liposuction procedure.
Liposuction has many clinical applications both in the field of aesthetic surgery and in functional and reconstructive surgery.
Obesity, initially a clear criterion of exclusion, was no longer considered as such [2].
Liposculture is a great tool for redefining the body's profile in patients who undergo significant weight loss. However, in order to obtain satisfactory aesthetic results, it is always necessary to associate the excision surgery to remove the skin excess. The suction of adipose tissue allows having empty areas, making surgery easier, shorter and reducing possible complications [97], [98], [99], [100].
A recent study reports the use of abdominal lipectomy as an adjunctive procedure to assist with long-term weight loss as part of the overall treatment of bariatric surgery patients [101].
In recent years, liposuction has become more important as a method for harvesting autologous fat and adipose-derived stem cells. Lipofilling is a widely used technique in several different clinical situations such as correction of asymmetry and defects in the body's profile, loss of volume, to improve retrograde or atrophic scars or regenerative medicine for the treatment of chronic wounds [102], [103], [104], [105], [106], [107], [108], [109], [110], [111], [112].
Recently, interest in adipose tissue has increased considerably. In last decades, numerous studies have demonstrated the wide differentiation and regenerative capacity of adipose-derived stem cells [113], [114], [115], [116], [117], [118].
The harvesting technique is currently the traditional liposuction, carried out in small quantities and with the syringes method to limit the traumas on adipocytes. Adipose-derived stem cells have potentially very high clinical applications in various medical and surgical specialties, justifying the present and future significant efforts on new techniques for isolating, collecting and maximizing these stem cells [119], [120], [121], [122].\\\\
Ethical approval
N/A.
Sources of funding
N/A.
Research registration unique identifying number (UIN)
N/A.
Author contribution
Edoardo Raposio: study design and data analysis.
Michele P. Grieco: management of clinical cases.
Elisa Bellini: data collection and writing the manuscript.
Conflicts of interest
None.
Guarantor
Prof. Edoardo Raposio is the Guarantor of the study.
References
- 1.Flynn T.C., Coleman W.P., 2nd, Field L.M., Klein J.A., Hanke C.W. History of liposuction. Dermatol Surg. 2000;26:515–520. doi: 10.1046/j.1524-4725.2000.00066.x. [DOI] [PubMed] [Google Scholar]
- 2.Sterodimas A., Boriani F., Magarakis E., Nicaretta B., Pereira L.H., Illouz Y.G. Thirtyfour years of liposuction: past, present and future. Eur. Rev. Med. Pharmacol. Sci. 2012;16:393–406. [PubMed] [Google Scholar]
- 3.Pitanguy I. Trochanteric lipodystrophy. Plast. Reconstr. Surg. 1964;34:280–286. doi: 10.1097/00006534-196409000-00010. [DOI] [PubMed] [Google Scholar]
- 4.Coleman W.P., 3rd The history of liposuction and fat transplantation in America. Dermatol Clin. 1999;17:723–727. doi: 10.1016/s0733-8635(05)70121-2. [DOI] [PubMed] [Google Scholar]
- 5.Kesselring L.K., Meyer R. A suction curette for removal of excessive local deposits of subcutaneous fat. Plast. Reconstr. Surg. 1978;62:305. doi: 10.1097/00006534-197808000-00040. [DOI] [PubMed] [Google Scholar]
- 6.Kesselring U. Regional fat aspiration for body contouring. Plast. Reconstr. Surg. 1983;72:610–619. doi: 10.1097/00006534-198311000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Hetter G., editor. Lipoplasty: the Theory and Practice of Blunt Suction Lipectomy. Little, Brown & Co; Boston: 1984. [Google Scholar]
- 8.Fischer A., Fischer G. First surgical treatment for molding body's cellulite with three 5 mm incisions. Bull. Int. Acad. Cosmet. Surg. 1976;3:35. [Google Scholar]
- 9.Fischer G. Liposculpture: the correct history of liposuction: Part I. J. Dermatol Surg. Oncol. 1990;16:1087. doi: 10.1111/j.1524-4725.1990.tb00017.x. [DOI] [PubMed] [Google Scholar]
- 10.Illouz Y. Body contouring by lipolysis: a 5 year experience with over 3000 cases. Plast. Reconstr. Surg. 1983;72:511. doi: 10.1097/00006534-198311000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Illouz Y.G. History and current concepts of lipoplasty. Clin. Plast. Surg. 1996;23:721–730. [PubMed] [Google Scholar]
- 12.Fournier P., Otten F. Lipodissection in body sculpturing: the dry procedure. Plast. Reconstr. Surg. 1983;75:598. doi: 10.1097/00006534-198311000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Hanke C.W., Coleman W.P., Francis L.A. History of dermatologic cosmetic surgery. Am. J. Cosmet. Surg. 1992;9:231–234. [Google Scholar]
- 14.Field L. The dermatologist and liposuction-a history. J. Dermatol Surg. Oncol. 1987;13:1040. [PubMed] [Google Scholar]
- 15.Newman J. Lipo-suction surgery: past-present-future. Am. J. Cosmet. Surg. 1984;1:19–20. [Google Scholar]
- 16.Sumrall A.J. A review of liposuction as a cosmetic surgical procedure. J. Natl. Med. Assoc. 1987;79:1275–1279. [PMC free article] [PubMed] [Google Scholar]
- 17.Coleman W.P. 3rd. The dermatologist as a liposuction surgeon. J. Dermatol Surg. Oncol. 1988;14:1057. doi: 10.1111/j.1524-4725.1988.tb03463.x. [DOI] [PubMed] [Google Scholar]
- 18.Newman J. Training in liposuction for dermatologists. Dermatol Clin. 1990;8:851. [PubMed] [Google Scholar]
- 19.Klein J.A. The tumescent technique for liposuction surgery. Am. J. Cosmet. Surg. 1987;4:263–267. [Google Scholar]
- 20.Klein J.A. Tumescent technique for local anesthesia improves safety in large volume liposuction. Plast. Reconstr. Surg. 1993;92:1085–1098. [PubMed] [Google Scholar]
- 21.Klein J.A. Tumescent technique for regional anesthesia permits lidocaine doses of 35 mg/kg for liposuction. J. Dermatol Surg. Oncol. 1990;16:248–263. doi: 10.1111/j.1524-4725.1990.tb03961.x. [DOI] [PubMed] [Google Scholar]
- 22.Lillis P.J. Liposuction surgery under local anaesthesia: limited blood loss and minimal lidocaine absorption. J. Dermatol Surg. Oncol. 1988;14:1145–1148. doi: 10.1111/j.1524-4725.1988.tb03472.x. [DOI] [PubMed] [Google Scholar]
- 23.Lillis P.J. The tumescent technique for liposuction surgery. Dermatol Clin. 1990;8:439. [PubMed] [Google Scholar]
- 24.Markey A.C. Liposuction in cosmetic dermatology. Clin. Exp. Dermatol. 2001;26:3–5. doi: 10.1046/j.1365-2230.2001.00748.x. [DOI] [PubMed] [Google Scholar]
- 25.Illouz Y.G. Une novelle technique pour les lipodystrophies localisees. Rev. Chir. Esthet. Lang. Franc. 1980;19:3–10. [Google Scholar]
- 26.Toledo L.S. Annals of the International Symposium “Recent Advances in Plastic Surgery”, Sao Paulo, Brazil, Estadao. 1989. Syringe liposculpture for face and body; p. 177. [Google Scholar]
- 27.Toledo L.S. Syringe liposculpture. Clin. Plast. Surg. 1996;23:683–693. [PubMed] [Google Scholar]
- 28.Lewis C.M. Comparison of the syringe and pump aspiration methods of lipoplasty. Aesth. Plast. Surg. 1991;15:203–208. doi: 10.1007/BF02273858. [DOI] [PubMed] [Google Scholar]
- 29.Zocchi M. Ultrasonic liposculpturing. Aesth. Plast. Surg. 1992;16:287–298. doi: 10.1007/BF01570690. [DOI] [PubMed] [Google Scholar]
- 30.Scuderi N., de Vita R., Andrea F. Nuove prospective nella liposuzione: La lipoemulsificazione. Giomale Di Chir. Plast. Ricostr. Ed. Estet. Rheol. Acta. 1987;11:1. [Google Scholar]
- 31.Igra H., Satur N.M. Tumescent liposuction versus internal ultrasonic-assisted tumescent liposuction. A side-to-side comparison. Dermatol Surg. 1997;23:1213–1218. doi: 10.1111/j.1524-4725.1997.tb00477.x. [DOI] [PubMed] [Google Scholar]
- 32.Lawrence N., Cox S.E. The efficacy of external ultrasound-assisted liposuction: a randomized controlled trial. Dermatol Surg. 2000;26:329–332. doi: 10.1046/j.1524-4725.2000.99177.x. [DOI] [PubMed] [Google Scholar]
- 33.Lawrence N., Coleman W.P., 3rd Ultrasonic-assisted liposuction. Internal and external. Dermatol Clin. 1999;17(4):761–771. doi: 10.1016/s0733-8635(05)70125-x. [DOI] [PubMed] [Google Scholar]
- 34.Scheflan M., Tazi H. Ultrasonically assisted body contouring. Aesth. Surg. Q. 1996:16117–16122. [Google Scholar]
- 35.Apfelberg D. laser-assisted liposuction may benefit surgeons and patients. Clin. Laser Mon. 1992;10:259–264. [PubMed] [Google Scholar]
- 36.Apfelberg D., Rosenthal S., Hunstad J. Progress report on multicenter study of laser-assisted liposuction. Aesth. Plast. Surg. 1994;18:259–264. doi: 10.1007/BF00449791. [DOI] [PubMed] [Google Scholar]
- 37.Apfelberg D. Results of multicentric study of laser-assisted liposuction. Clin. Plast. Surg. 1996;23:713–719. [PubMed] [Google Scholar]
- 38.Valizadeh N., Jalaly N.Y., Zarghampour M., Barikbin B., Haghighatkhah H.R. Evaluation of safety and efficacy of 980-nm diode laser-assisted lipolysis versus traditional liposuction for submental rejuvenation: a randomized clinical trial. J. Cosmet. Laser Ther. 2016;18:41–45. doi: 10.3109/14764172.2015.1039041. [DOI] [PubMed] [Google Scholar]
- 39.Shiffman M.A., Di Giuseppe A. Liposuction Principles and Practice. Springer; Berlin, Germany: 2006. [Google Scholar]
- 40.Stebbins W.G., Hanke C.W., Petersen J. Invasive removal of large lipoma after laser lipolysis with 980 nm diode laser. Dermatol Ther. 2011;24:125–130. doi: 10.1111/j.1529-8019.2010.01385.x. [DOI] [PubMed] [Google Scholar]
- 41.Medina C.R., Schneider S., Mitra A. Giant submental lipoma: case report and review of the literature. Can. J. Plast. Surg. 2007;15:219–222. doi: 10.1177/229255030701500405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Choi C.W., Kim B.J., Moon S.E. Treatment of lipomas assisted with tumescent liposuction. J. Eur. Acad. Dermatol Venereol. 2007;21:243–246. doi: 10.1111/j.1468-3083.2006.02037.x. [DOI] [PubMed] [Google Scholar]
- 43.Field L., Asken S., Caver C. Liposuction surgery: a review. J. Dermatol Surg. Oncol. 1984;10:530–538. doi: 10.1111/j.1524-4725.1984.tb01248.x. [DOI] [PubMed] [Google Scholar]
- 44.Coleman W. Noncosmetic applications of liposuction. Dermatol Surg. Oncol. 1988;14:1085–1090. doi: 10.1111/j.1524-4725.1988.tb03465.x. [DOI] [PubMed] [Google Scholar]
- 45.Ross M., Goodman M. Multiple symmetyric lipomatosis (Launois-Bensaude syndrome) Int. J. Dermatol. 1992;31:80–82. doi: 10.1111/j.1365-4362.1992.tb03240.x. [DOI] [PubMed] [Google Scholar]
- 46.Atiyeh B., Costagliola M., Illouz Y.G., Dibo S., Zgheib E., Rampillon F. Functional and therapeutic indications of liposuction: personal experience and review of the literature. Ann. Plast. Surg. 2015;75:231–245. doi: 10.1097/SAP.0000000000000055. [DOI] [PubMed] [Google Scholar]
- 47.Todd M. Lipoedema: presentation and management. Br. J. Community Nurs. 2010;15:S10–S16. doi: 10.12968/bjcn.2010.15.Sup3.47363. [DOI] [PubMed] [Google Scholar]
- 48.Schmeller W., Hueppe M., Meier-Vollrath I. Tumescent liposuction in lipoedema yields good long-term results. Br. J. Dermatol. 2012;166:161–168. doi: 10.1111/j.1365-2133.2011.10566.x. [DOI] [PubMed] [Google Scholar]
- 49.Peled A.W., Slavin S.A., Brorson H. Long-term outcome after surgical treatment of lipedema. Ann. Plast. Surg. 2012;68:303–307. doi: 10.1097/SAP.0b013e318215791e. [DOI] [PubMed] [Google Scholar]
- 50.Vantyghem M.C., Balavoine A.S., Douillard C. How to diagnose a lipodystrophy syndrome. Ann. Endocrinol. 2012;73:170–189. doi: 10.1016/j.ando.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 51.Capeau J., Magre´ J., Caron-Debarle M. Human lipodystrophies: genetic and acquired diseases of adipose tissue. Endocr. Dev. 2010;19:1–20. doi: 10.1159/000316893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Garg A. Lipodystrophies: genetic and acquired body fat disorders. J. Clin. Endocrinol. Metab. 2011;96:3313–3325. doi: 10.1210/jc.2011-1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brun A., Comparin J.P., Voulliaume D. Insulin-induced lipohypertrophy treated by liposuction. Ann. Chir. Plast. Esthet. 2007;52:218–221. doi: 10.1016/j.anplas.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 54.Field L. Treatment of hypertrophic insulin lipodystrophy by liposuction. J. Am. Acad. Dermatol. 1988;19:570. doi: 10.1016/s0190-9622(88)80325-6. [DOI] [PubMed] [Google Scholar]
- 55.Narins R. Liposuction surgery of a buffalo hump secondary to Cushing's disease. J. Am. Acad. Dermatol. 1991;21:307. doi: 10.1016/s0190-9622(89)70183-3. [DOI] [PubMed] [Google Scholar]
- 56.Gold D.R., Annino D.J., Jr. HIV-associated cervicodorsal lipodystrophy: etiology and management. Laryngoscope. 2005;115:791–795. doi: 10.1097/01.MLG.0000161838.22766.88. [DOI] [PubMed] [Google Scholar]
- 57.Dolsky R., Fetzek J. Gynecomastia: treatment by liposuction. Am. J. Cosmet. Surg. 1987;4:27–34. [Google Scholar]
- 58.Rosenberg G. Gynecomastia: suction lipectomy as a contemporary solution. Plast. Reconstr. Surg. 1987;8(386) 80:379-85, and discussion per Cohen I, 386. [PubMed] [Google Scholar]
- 59.Cigna E., Tarallo M., Fino P. Surgical correction of gynecomastia in thin patients. Aesth. Plast. Surg. 2011;35:439–445. doi: 10.1007/s00266-010-9618-3. [DOI] [PubMed] [Google Scholar]
- 60.Habbema L. Breast reduction using liposuction with tumescent local anesthesia and powered cannulas. Dermatol Surg. 2009;35:41–50. doi: 10.1111/j.1524-4725.2008.34381.x. discussion 50–52. [DOI] [PubMed] [Google Scholar]
- 61.Lejour M. Vertical mammaplasty and liposuction of the breast. Plast. Reconstr. Surg. 1994;94:100–114. doi: 10.1097/00006534-199407000-00010. [DOI] [PubMed] [Google Scholar]
- 62.Aiache A. Lipolysis of the female breast. In: Hetter G., editor. Lipoplasty: the Theory and Practice of Blunt Suction Lipectomy. Little, Brown; Boston: 1984. pp. 227–231. [Google Scholar]
- 63.Brorson H. From lymph to fat: liposuction as a treatment for complete reduction of lymphedema. Int. J. Low. Extrem Wounds. 2012;11:10–19. doi: 10.1177/1534734612438550. [DOI] [PubMed] [Google Scholar]
- 64.Jensen M.R., Simonsen L., Karlsmark T. Lymphoedema of the lower extremities - background, pathophysiology and diagnostic considerations. Clin. Physiol. Funct. Imaging. 2010;30:389–398. doi: 10.1111/j.1475-097X.2010.00969.x. [DOI] [PubMed] [Google Scholar]
- 65.Brorson H. Surgical treatment of postmastectomy lymphedema - liposuction. In: Lee B.B., Bergan J., Rockson S.G., editors. Lymphedema: a Concise Compendium of Theory and Practice. Springer; London, UK: 2011. pp. 409–418. [Google Scholar]
- 66.Brorson H. From lymph to fat: complete reduction of lymphoedema. Phlebology. 2010;25:52–63. doi: 10.1258/phleb.2010.010s08. [DOI] [PubMed] [Google Scholar]
- 67.Brorson H. Liposuction in arm lymphedema treatment. Scand. J. Surg. 2003;92:287–295. doi: 10.1177/145749690309200409. [DOI] [PubMed] [Google Scholar]
- 68.Greene A.K., Slavin S.A., Borud L. Treatment of lower extremity lymphedema with suction-assisted lipectomy. Plast. Reconstr. Surg. 2006;118:118–121. doi: 10.1097/01.prs.0000237020.29209.22. [DOI] [PubMed] [Google Scholar]
- 69.Huang S.H., Wu S.H., Chang K.P. Contour refinements of free flaps for optimal outcome in oral reconstruction: combination of modified liposuction technique and w-plasty in one-stage procedure. J. Craniomaxillofac Surg. 2009;37:201–205. doi: 10.1016/j.jcms.2008.11.008. [DOI] [PubMed] [Google Scholar]
- 70.Hallock G.G. Defatting of flaps by means of suction-assisted lipectomy. Plast. Reconstr. Surg. 1985;76:948–952. doi: 10.1097/00006534-198512000-00031. [DOI] [PubMed] [Google Scholar]
- 71.Shenaga S., Spira M. Treatment of bilateral axillary hyperhidrosis by suction assisted lipolysis technique. Ann. Plast. Surg. 1987;19:548–551. doi: 10.1097/00000637-198712000-00013. [DOI] [PubMed] [Google Scholar]
- 72.Li Y., Li W., Li X. A refined minimally invasive procedure for radical treatment of axillary osmidrosis: combined tumescent liposuction with subcutaneous pruning through a small incision. J. Plast. Reconstr. Aesthet. Surg. 2012;65:320–321. doi: 10.1016/j.bjps.2012.05.020. [DOI] [PubMed] [Google Scholar]
- 73.Lee D., Cho S.H., Kim Y.C. Tumescent liposuction with dermal curettage for treatment of axillary osmidrosis and hyperhidrosis. Dermatol Surg. 2006;32:505–511. doi: 10.1111/j.1524-4725.2006.32103.x. [DOI] [PubMed] [Google Scholar]
- 74.Atiyeh B.S. Non-surgical management of hypertrophic scars (Hss): evidence-based therapies, standard practices and emerging modalities. Aesth. Plast. Surg. 2007;31:468–492. doi: 10.1007/s00266-006-0253-y. [DOI] [PubMed] [Google Scholar]
- 75.Lei H., Ma G., Chen J. Combination excision and liposuction in a single-stage treatment of various skin disorders. Int. J. Dermatol. 2010;49:311–316. doi: 10.1111/j.1365-4632.2009.04302.x. [DOI] [PubMed] [Google Scholar]
- 76.Ibrahim A.E., Dibo S.A., Shady S.H. Reverse tissue expansion by liposuction deflation for revision of post-surgical thigh scars. Int. Wound J. 2011;8:622–631. doi: 10.1111/j.1742-481X.2011.00842.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Alter G.J. Pubic contouring after massive weight loss in men and women: correction of hidden penis, mons ptosis, and labia majora enlargement. Plast. Reconstr. Surg. 2012;130:936–947. doi: 10.1097/PRS.0b013e318262f57d. [DOI] [PubMed] [Google Scholar]
- 78.Mokhless I.A., Abdeldaeim H.M., Rahman A. Penile advancement and lengthening for the management of post-circumcision traumatic short penis in adolescents. Urology. 2010;76:1483–1487. doi: 10.1016/j.urology.2010.06.018. [DOI] [PubMed] [Google Scholar]
- 79.Fedok F.G., Houck J.R., Manders E.K. Suction assisted lipectomy in the management of obstructive sleep apnea. Arch. Otolaryngol. Head. Neck Surg. 1990;116:968–970. doi: 10.1001/archotol.1990.01870080090023. [DOI] [PubMed] [Google Scholar]
- 80.Samdal F., Amland P.F., Bakka A. Troublesome colostomies and urinary stomas treated with suction-assisted lipectomy. Eur. J. Surg. 1995;161:361–364. [PubMed] [Google Scholar]
- 81.Samdal F., Brevik B., Husby O.S. A troublesome urostomy treated with liposuction. Case report. Scand. J. Plast. Reconstr. Surg. Hand Surg. 1991;25:91–92. doi: 10.3109/02844319109034930. [DOI] [PubMed] [Google Scholar]
- 82.Rohrich R.J., Broughton G., II, Horton B., Lipschitz A., Kenkel J.M., Brown S.A. The key to long-term success in liposuction: a guide for plastic surgeons and patients. Plast. Reconstr. Surg. 2004;114:1945–1952. doi: 10.1097/01.prs.0000143002.01231.3d. discussion 1953. [DOI] [PubMed] [Google Scholar]
- 83.Rohrich R.J., Beran S.J., Fodor P.B. The role of subcutaneous infiltration in suction-assisted lipoplasty: a review. Plast. Reconstr. Surg. 1997;99:514–519. doi: 10.1097/00006534-199702000-00031. discussion 520–526. [DOI] [PubMed] [Google Scholar]
- 84.Matarasso A. Superwet anesthesia redefines large-volume liposuction. Aesthet. Surg. J. 1997;17:358–364. doi: 10.1016/s1090-820x(97)80049-0. [DOI] [PubMed] [Google Scholar]
- 85.Chia C.T., Neinstein R.M., Theodorou S.J. Evidence-based medicine: liposuction. Plast. Reconstr. Surg. 2017;139:267e–274e. doi: 10.1097/PRS.0000000000002859. [DOI] [PubMed] [Google Scholar]
- 86.Stephan P.J., Kenkel J.M. Updates and advances in liposuction. Aesthet. Surg. J. 2010;30:83–97. doi: 10.1177/1090820X10362728. quiz 98. [DOI] [PubMed] [Google Scholar]
- 87.Gasperoni C., Gasperoni P. Subdermal liposuction: longterm experience. Clin. Plast. Surg. 2006;33:63–73. doi: 10.1016/j.cps.2005.08.006. vi. [DOI] [PubMed] [Google Scholar]
- 88.Rohrich R.J., Smith P.D., Marcantonio D.R., Kenkel J.M. The zones of adherence: role in minimizing and preventing contour deformities in liposuction. Plast. Reconstr. Surg. 2001;107:1562–1569. doi: 10.1097/00006534-200105000-00043. [DOI] [PubMed] [Google Scholar]
- 89.Hunstad J.P. Tumescent and syringe liposculpture: a logical partnership. Aesth. Plast. Surg. 1995;19:321–333. doi: 10.1007/BF00451658. [DOI] [PubMed] [Google Scholar]
- 90.Bernstein G. Instrumentation for liposuction. Dermatol Clin. 1999;17:735–749. doi: 10.1016/s0733-8635(05)70123-6. v. [DOI] [PubMed] [Google Scholar]
- 91.Dixit V.V., Wagh M.S. Unfavourable outcomes of liposuction and their management. Indian J. Plast. Surg. 2013;46:377–392. doi: 10.4103/0970-0358.118617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Lehnhardt M., Homann H.H., Daigeler A., Hauser J., Palka P., Steinau H.U. Major and lethal complications of liposuction: a review of 72 cases in Germany between 1998 and 2002. Plast. Reconstr. Surg. 2008;121:396e–403e. doi: 10.1097/PRS.0b013e318170817a. [DOI] [PubMed] [Google Scholar]
- 93.Hughes C.E. 3rd Reduction of lipoplasty risks and mortality: an ASAPS survey. Aesthet. Surg. J. 2001;21:120–127. doi: 10.1067/maj.2001.115166. [DOI] [PubMed] [Google Scholar]
- 94.Grazer F.M., de Jong R.H. Fatal outcomes from liposuction: census survey of cosmetic surgeons. Plast. Reconstr. Surg. 2000;105:436–446. doi: 10.1097/00006534-200001000-00070. discussion 447. [DOI] [PubMed] [Google Scholar]
- 95.Housman T.S., Lawrence N., Mellen B.G. The safety of liposuction: results of a national survey. Dermatol Surg. 2002;28:971–978. doi: 10.1046/j.1524-4725.2002.02081.x. [DOI] [PubMed] [Google Scholar]
- 96.Gilliland M.D., Coctes N. Tumescent liposuction complicated by pulmonary edema. Plast. Reconstr. Surg. 1997;99:215–219. doi: 10.1097/00006534-199701000-00032. [DOI] [PubMed] [Google Scholar]
- 97.Grieco M., Grignaffini E., Simonacci F., Di Mascio D., Raposio E. Post-bariatric body contouring: our experience. Acta Biomed. 2016;87:70–75. [PubMed] [Google Scholar]
- 98.Grignaffini E., Grieco M.P., Bertozzi N., Gandolfi M., Palli D., Cinieri F.G., Gardani M., Raposio E. Post-bariatric abdominoplasty: our experience. Acta Biomed. 2015;86:278–282. [PubMed] [Google Scholar]
- 99.Grieco M., Grignaffini E., Simonacci F., Raposio E. Analysis of complications in postbariatric abdominoplasty: our experience. Plast. Surg. Int. 2015;2015:209173. doi: 10.1155/2015/209173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Gardani M., Bertozzi N., Grieco M.P., Pesce M., Simonacci F., Santi P.L., Raposio E. Breast reconstruction with anatomical implants: a review of indications and techniques based on current literature. Ann. Med. Surg. 2017;21:96–104. doi: 10.1016/j.amsu.2017.07.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Abbed T.M., Gonzalez-Heredia R., Sanchez-Johnsen L., Elli E.F., Cohen M.N. Impact of body contouring procedures on post-bariatric surgery weight loss. Ann. Plast. Surg. 2017 doi: 10.1097/SAP.0000000000001142. [DOI] [PubMed] [Google Scholar]
- 102.Simonacci F., Bertozzi N., Grieco M.P., Grignaffini E., Raposio E. Autologous fat transplantation for breast reconstruction: a literature review. Ann. Med. Surg. (Lond) 2016;12:94–100. doi: 10.1016/j.amsu.2016.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Raposio E., Bertozzi N. Autologous fat grafting and processing after breast reconstruction. Surg. Chron. 2017;22:66–72. [Google Scholar]
- 104.Caruana G., Bertozzi N., Boschi E., Pio Grieco M., Grignaffini E., Raposio E. Role of adipose-derived stem cells in chronic cutaneous wound healing. Ann. Ital. Chir. 2015;86:1–4. [PubMed] [Google Scholar]
- 105.Fan J., Raposio E., Wang J., Nordström R.E. Development of the inframammary fold and ptosis in breast reconstruction with textured tissue expanders. Aesth. Plast. Surg. 2002;26:219–222. doi: 10.1007/s00266-002-1477-0. [DOI] [PubMed] [Google Scholar]
- 106.Raposio E., Bonomini S., Calderazzi F. Isolation of autologous adipose tissue-derived mesenchymal stem cells for bone repair. Orthop. Traumatol. Surg. Res. 2016;102:909–912. doi: 10.1016/j.otsr.2016.07.006. [DOI] [PubMed] [Google Scholar]
- 107.Raposio E., Bertozzi N., Bonomini S., Bernuzzi G., Formentini A., Grignaffini E., Pio Grieco M. Adipose-derived stem cells added to platelet-rich plasma for chronic skin ulcer therapy. Wounds. 2016;28:126–131. [PubMed] [Google Scholar]
- 108.Raposio E., Calderazzi F. Fat grafting for chronic heel pain following surgery for adult flatfoot deformity: pilot study. Foot (Edinb) 2017;31:56–60. doi: 10.1016/j.foot.2017.02.005. [DOI] [PubMed] [Google Scholar]
- 109.Simonacci F., Bertozzi N., Grieco M.P., Grignaffini E., Raposio E. Procedure, applications, and outcomes of autologous fat grafting. Ann. Med. Surg. 2017;20:49–60. doi: 10.1016/j.amsu.2017.06.059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Porro I., Schenone A., Fato M., Raposio E., Molinari E., Beltrame F. An integrated environment for plastic surgery support: building virtual patients, simulating interventions, and supporting intraoperative decisions. Comput. Med. Imaging Graph. 2005;29:385–394. doi: 10.1016/j.compmedimag.2005.02.005. [DOI] [PubMed] [Google Scholar]
- 111.Bertozzi N., Pesce M., Santi P.L., Raposio E. Oncoplastic breast surgery: comprehensive review. Eur. Rev. Med. Pharmacol. Sci. 2017;21:2572–2585. [PubMed] [Google Scholar]
- 112.Simonacci F., Bertozzi N., Grieco M.P., Grignaffini E., Raposio E. Autologous fat transplantation for breast reconstruction: a literature review. Ann. Med. Surg. (Lond) 2016;12:94–100. doi: 10.1016/j.amsu.2016.11.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bertozzi N., Simonacci F., Grieco M.P., Grignaffini E., Raposio E. The biological and clinical basis for the use of adipose-derived stem cells in the field of wound healing. Ann. Med. Surg. 2017;20:41–48. doi: 10.1016/j.amsu.2017.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Scanarotti C., Bassi A.M., Catalano M., Guida C., Coradeghini R., Falugi C., Aluigi M., Santi P., Raposio E. Neurogenic-committed human pre-adipocytes express CYP1A isoforms. Chem. Biol. Interact. 2010;184:474–483. doi: 10.1016/j.cbi.2010.01.009. [DOI] [PubMed] [Google Scholar]
- 115.Raposio E., Guida C., Baldelli I., Benvenuto F., Curto M., Paleari L., Filippi F., Fiocca R., Robello G., Santi P.L. Characterization and induction of human pre-adipocytes. Toxicol Vitro. 2007;21:330–334. doi: 10.1016/j.tiv.2006.09.022. [DOI] [PubMed] [Google Scholar]
- 116.Coradeghini R., Guida C., Scanarotti C., Sanguineti R., Bassi A.M., Parodi A., Santi P.L., Raposio E. A comparative study of proliferation and hepatic differentiation of human adipose-derived stem cells. Cells Tissues Org. 2010;191:466–477. doi: 10.1159/000273266. [DOI] [PubMed] [Google Scholar]
- 117.Aluigi M.G., Coradeghini R., Guida C., Scanarotti C., Bassi A.M., Falugi C., Santi P., Raposio E. Pre-adipocytes commitment to neurogenesis 1: preliminary localisation of cholinergic molecules. Cell Biol. Int. 2009;33:594–601. doi: 10.1016/j.cellbi.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 118.Raposio E., Guida C., Coradeghini R., Scanarotti C., Parodi A., Baldelli I., Fiocca R., Santi P.L. In vitro polydeoxyribonucleotide effects on human pre-adipocytes. Cell Prolif. 2008;41:739–754. doi: 10.1111/j.1365-2184.2008.00547.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Raposio E., Caruana G., Petrella M., Bonomini S., Grieco M.P. A standardized method of isolating adipose-derived stem cells for clinical applications. Ann. Plast. Surg. 2016;76:124–126. doi: 10.1097/SAP.0000000000000609. [DOI] [PubMed] [Google Scholar]
- 120.Raposio E., Caruana G., Bonomini S., Libondi G. A novel and effective strategy for the isolation of adipose-derived stem cells: minimally manipulated adipose-derived stem cells for more rapid and safe stem cell therapy. Plast. Reconstr. Surg. 2014;133:1406–1409. doi: 10.1097/PRS.0000000000000170. [DOI] [PubMed] [Google Scholar]
- 121.Raposio E., Bertozzi N. Isolation of ready-to-use Adipose-derived Stem Cell (ASC) pellet for clinical applications and a comparative overview of alternate methods for ASC isolation. Curr. Protoc. Stem Cell Biol. 2017;16(41) doi: 10.1002/cpsc.29. 1F.17.1-1F.17. [DOI] [PubMed] [Google Scholar]
- 122.Raposio E., Simonacci F., Perrotta R.E. Adipose-derived stem cells: comparison between two methods of isolation for clinical applications. Ann. Med. Surg. 2017;20:87–91. doi: 10.1016/j.amsu.2017.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]