Abstract
Background
Most hospitalized patients with asthma or chronic obstructive pulmonary disease (COPD) misuse respiratory inhalers. An in-person educational strategy, teach-to-goal (TTG), improves inpatients’ inhaler technique.
Objective
To develop an effective, portable education intervention that remains accessible to hospitalized patients post-discharge for reinforcement of proper inhaler technique.
Methods
A mixed methods approach at an urban academic hospital was used to iteratively develop, modify and test a virtual teach-to-goal™ (V-TTG™) educational intervention using patient end-user feedback. A survey examined access and willingness to use technology for self-management education. Focus groups evaluated patients’ feedback on V-TTG™’s access, functionality, and quality.
Results
Forty-eight participants completed the survey with most reporting having internet access; 77% used the internet at home and 82% used the internet at least once every few weeks. Over 80% reported they were somewhat or very likely to use V-TTG™ to gain skills to improve their health. Most participants reported smart phone access (73%); half owned laptop computers (52%). Participants with asthma versus COPD were more likely to own a smartphone, have a data plan, and have daily internet use (p<0.05). Nine focus groups (n=25) identified themes for each domain: access--platform and delivery, internet access, and technological literacy; functionality--usefulness, content, and teaching strategy; and quality-- clarity, ease of use, length, and likability.
Conclusion
V-TTG™ is a promising educational tool for improving patients’ inhaler technique, iteratively developed and refined with patient input. Patients in our urban, academic hospital overwhelmingly reported access to platforms and willingness to use V-TTG™ for health education.
Primary Funding
National Heart Lung and Blood Institute (NIH K23HL118151).
Keywords: Self Care, Patient Education, Asthma, Pulmonary Disease, Chronic Obstructive
Introduction
In the United States, asthma and chronic obstructive pulmonary disease (COPD) affect almost 30 million adults.1–2 Medications delivered by inhalers provide the mainstay of treatment in controlling and preventing symptoms for both diseases.3–8 However, respiratory inhaler misuse is exceedingly common,9–10 with 86% of observed inpatients with asthma or COPD displaying incorrect technique.3,11 Improper inhaler use, especially certain critical errors like inspiratory effort, leads to ineffective medication delivery and correlates closely with suboptimal symptom control, lower quality of life (QOL), and increased emergency room visits and hospitalizations.12, 13 This ineffective inhaler technique is often not considered prior to escalating treatment, therefore doses of medications or even additional medications may be unnecessarily added to patients’ regimens.10 The economic cost of wasted medications alone is estimated to be 5–7 billion dollars annually, and the burden on the health care system due to uncontrolled chronic symptoms is tremendous.12,14–18 Proper inhaler technique education is therefore crucial for effective self-management of asthma and COPD.13,19
Our previous work has shown that Teach-To-Goal (TTG), an in-person educational method of cycles of demonstration and assessment,11,20–21 is effective for teaching inhaler technique to hospitalized patients with asthma or COPD.11,21–22 However, we have also shown that the improved inhaler technique initially obtained through TTG wanes within 30 days post-discharge.22 Since providing in-person inhaler teaching post-discharge is often impractical, but reinforced teaching is necessary, a need exists for an effective, portable education strategy that remains accessible to patients both in-hospital and post-discharge.
With increasing internet access among the American public,24 employing a virtual teach-to-goal™ (V-TTG™) education module for inhaler training may be a viable and efficient alternative.25 Previous studies have shown technology-based interventions to be effective at improving self-management for other chronic conditions.26–32 However, access and willingness to use technology for home-based self-management education among inpatients with asthma or COPD is unknown, particularly among an underserved patient population. Further, the use of adaptive learning technology for self-management education for this topic and population has not been widely studied. Therefore, when developing the V-TTG™ learning module it was necessary to iteratively modify and test each module component, which included demonstration and narration videos, pre- and post-demonstration self-assessment questions, and overall video module design and delivery, to ensure that we optimized V-TTG™ for patient use.
The overall goal was to develop V-TTG™ into an effective and acceptable interactive learning module that would be easily accessed post-discharge on patients’ home devices. After developing the inhaler technique demonstration videos produced by Click To Play Media (Berkeley, CA), we partnered with the Smart Sparrow (Sydney, NSW, Australia) for their adaptive learning technology platform. Our aim was to optimize the V-TTG™ through mixed methods, including surveys and focus groups, to offer two different perspectives across three key domains of the module design and delivery: access, functionality, and quality. Using mixed-methods, we aimed to 1) understand patient access to technology, including which platforms would be both favorable and available to our patient population using quantitative survey data, and 2) obtain in depth feedback on the usability and quality of the module assessment questions and the overall learning module itself using qualitative patient focus group data.
Methods
Design and Setting
We conducted a prospective mixed methods study33 at the University of Chicago Medicine (UCM), an urban, predominantly underserved adult patient population. Iterative testing of V-TTG™ and its components was completed with surveys on patients’ use and ownership of technology and with patient focus groups, collecting quantitative and qualitative data, respectively. This use of mixed methods was selected for the insight it could offer into two different aspects of V-TTG™: 1) the proportion of inpatients who have used specific devices or have accessed the internet and 2) the subjective experience of interacting with and learning from the module.33 The former could be best examined using quantitative methods, while the latter by qualitative.
Participants
Technology survey
Survey participants were recruited from the general medicine service from January-September 2014. Patients who provided written informed consent to take part in the Hospitalist Project, an ongoing study on cost and quality of care,34 and who met inclusion criteria for the technology survey study were approached during the same hospitalization by trained research assistants. For this report, we only used survey data from inpatients with a diagnosis of asthma and/or COPD. Patients with asthma only were included in the asthma cohort, while patients with COPD or COPD and asthma were included in the COPD cohort. Additional inclusion criteria included being over 18 years and English-speaking. Exclusion criteria included inability to provide consent. All participation was voluntary. The study was approved by the UCM Institutional Review Board (IRB16-0763).
Focus groups
Participants were recruited from the UCM Department of Internal Medicine and Asthma and COPD Center between December 2013 and April 2014. Inclusion criteria included being over 18 years and English-speaking, physician diagnosis of asthma or COPD, and prescribed use of a metered dose inhaler. Exclusion criteria included current hospitalization and inability to provide consent. Potential participants were contacted using a phone script and, if interested, were mailed or emailed a letter regarding their participation. All participation was voluntary and written informed consent was obtained. This study was approved by the University of Chicago Institutional Review Board (IRB13–1139).
Data Collection
Technology survey
The survey was developed to obtain a comprehensive understanding of our patient population’s use, ownership, and access to technology, and their willingness to utilize technology for health-related information. Survey items were benchmarked against similar items from the existing literature including the national Pew survey35 and questions from a local research study,36 in addition to V-TTG™ specific questions for more detailed information on patients’ willingness and ability to use V-TTG™.
For this study, we focused our analysis on a subset of survey items that pertained to internet access, device ownership and preference, and willingness to use V-TTG™. Surveys were completed on paper-based forms and managed using REDCap37 (Research Electronic Data Capture) electronic data capture tools hosted at the University of Chicago.
Focus group interviews
The qualitative approach taken in this study was that of phenomenology, which examines a particular phenomenon, in this case V-TTG™, through the perceptions of users interacting with the module.33 This approach, allows for the collection of detailed data regarding how participants personally relate to and interpret V-TTG™ as a tool for self-management education.
Focus groups were selected as the specific means of data collection for their ability to capture participant reactions to the perspectives shared by others, allowing the collective conversation to clarify or build upon the breadth of participant insight. Therefore, focus group data not only captures similar and conflicting viewpoints, but also provides a deeper understanding of why and how these viewpoints may inform the development of V-TTG™.
All focus groups were conducted using a semi-structured interview format in which moderators asked open-ended questions to elicit participant feedback on the three predetermined themes of interest: access (e.g., “What device would you prefer to use to watch this module?”), functionality (e.g., “How useful is this module?”), and quality (e.g., “How interesting did you find the module?”) based on prepared scripts. Further probing questions were improvised by the moderators during the focus group sessions to draw out additional participant comments. All focus group activity was video-recorded and transcribed to ensure accuracy of qualitative data, with identifying markers removed.
Three rounds of focus groups were held, with each round building upon the findings of the previous, in a snowball fashion. Focus group scripts were prepared for each round based on the results from the previous round and introducing the next phase of the focus group testing, as appropriate. The first round of focus groups discussed the videos and a list of assessment questions provided on paper. The second round focused on the videos and electronic assessment questions. The third round viewed and discussed the entirety of V-TTG™, with full adaptive learning functionality enabled. After the focus groups had been completed and V-TTG™ finalized, a member check meeting was held, in which all participants of previous focus groups were invited back to view and comment on the final V-TTG™. Participants rated their satisfaction with the incorporation of their feedback on a Likert scale from 1 to 10.
Data analysis
Technology survey
Descriptive statistics (means, medians, and proportions) were computed using Stata 14 software (College Station, TX) and used to summarize respondent demographics and technology characteristics. Chi-square and Fisher’s Exact tests were used for categorical differences; t-tests were used for continuous variables. Survey data regarding technology ownership and use were considered in determining the optimal platform for V-TTG™ (i.e., web-based vs. application-based). Statistical significance was defined as p<0.05.
Focus groups
Qualitative content analysis was completed from professionally transcribed recordings using a deductive approach with subsequent sub-themes developed. Participant comments were grouped under three pre-determined domains of interest: access, functionality, and quality. Access referred to participants’ ability to use the V-TTG™ in terms of possessing and knowing how to use necessary internet devices. Functionality was judged according to how effective participants perceived the V-TTG™ to be in teaching patients about inhaler technique. Quality was defined as the degree to which participants had a positive experience while using the V-TTG™. Transcript sections were then inductively coded using the constant comparative method to generate new themes within each domain. Three members of the research team coded the interview transcripts. One principal investigator (VP) and one research assistant (NW) independently coded 10% of the same interview transcripts to establish a coding scheme.38–39 Two research assistants (NW and MW) then independently coded all of the transcripts using that coding scheme, with VP coding a further 20%.40–42 Discrepancies between investigators were resolved via consensus. Coding continued until theme saturation was reached. Transcripts and codes were not returned to focus group participants. However, the general results were reported to the member check focus group participants.
All qualitative analysis of the data, including retrieving, coding, and sorting the data, was completed using Atlas.ti 7.5 (Berlin).
Results
Technology Survey
A total of 48 participants with asthma (67%, 32/48) or COPD (33%, 16/48) completed the technology survey. The majority were African American (77%) and female (60%), with a mean age of 48 years (Table 1). No demographic differences were found by diagnosis except that patients with asthma (vs. COPD) had a median younger age (38 years vs. 56 years, p <0.001).
Table 1.
Demographic, technology ownership, and technology use characteristics of technology survey respondents with asthma and/or COPD (n=48).
| Variables | Asthma or COPD (n=48) |
Asthma (n=32)* |
COPD (n=16)** |
p |
|---|---|---|---|---|
|
| ||||
| Female [n (%)] | 29 (60%) | 22 (69%) | 7 (44%) | 0.07 |
| Age, Median [IQR] | 48 (34–55) | 38 (31–51) | 56 (52–61) | <0.001 |
| Race [n (%)] | 0.7 | |||
| Black | 37 (77%) | 24 (80%) | 13 (81%) | |
| White | 8 (17%) | 5 (17%) | 3 (19%) | |
| Other | 1 (2%) | 1 (3%) | 0 (0%) | |
|
| ||||
| Device ownership | ||||
| Smartphone | 35 (73%) | 28 (88%) | 7 (44%) | 0.004 |
| Laptop | 25 (52%) | 19 (59%) | 6 (38%) | 0.2 |
| Desktop | 20 (42%) | 13 (41%) | 7 (44%) | 0.8 |
| Tablet | 11 (23%) | 9 (28%) | 2 (13%) | 0.3 |
|
| ||||
| Internet Access [n (%)] | ||||
| Uses the internet at home | 37 (77%) | 28 (88%) | 12 (69%) | 0.1 |
| Uses the internet at family’s home | 21 (44%) | 17 (53%)* | 4 (25%)** | 0.1 |
| Uses wifi in public spaces | 27 (56%) | 20 (63%) | 7 (44%) | 0.2 |
| Has phone data plan | 30 (63%) | 24 (75%)* | 6 (38%) | 0.007 |
|
| ||||
| Internet Use Frequency [n (%)]*** | 0.046 | |||
| Several times per day | 29 (60%) | 22 (69%) | 7 (44%) | |
| About once a day | 5 (10%) | 0 (0%) | 1 (6%) | |
| 3–5 days per week | 1 (2%) | 0 (0%) | 1 (6%) | |
| 1–2 day per week | 3 (6%) | 0 (0%) | 3 (19%) | |
| Every few weeks | 2 (4%) | 2 (6%) | ||
| Less often than every few weeks | 4 (8%) | 3 (9%) | 1 (6%) | |
| Never | 3 (6%) | 1 (3%) | 2 (13%) | |
| N/A | 1 (2%) | 0 (0%) | 1 (6%) | |
|
| ||||
| Willing to use V-TTG™ post-discharge [n (%)] | 39 (81%) | 27 (84%) | 12 (75%) | 0.5 |
Data missing for n=2 gender, race; n=9 for internet use at family’s home for asthma; n=1 for data plan
Data missing for n=9 for internet use at family’s home
Internet use frequency dichotomized into “less than” or “at least” daily use for statistical analysis
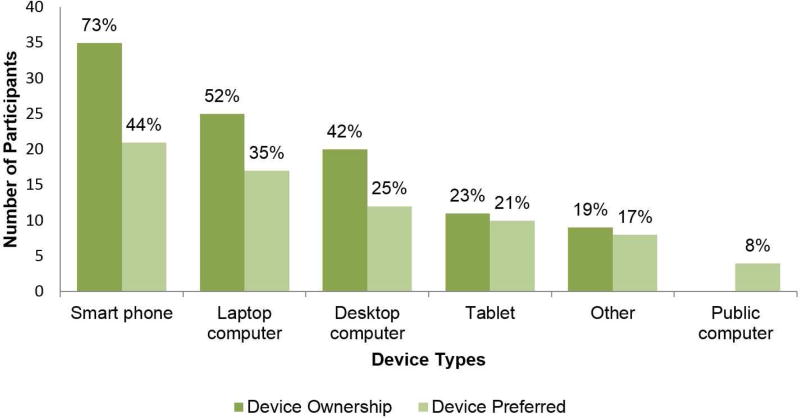
Survey findings regarding technology ownership and use (Table 1) indicated that internet access and use frequency were generally high, with 77% (37/48) of respondents reporting internet use at home, 62% (30/48) reporting phone data plans, and 82% (40/48) reporting frequent internet use. Survey respondents showed high willingness to use V-TTG™ post-discharge, with over 80% (39/48) stating that they would be “somewhat” or “very” likely to use it to learn more about skills to improve their health problems. The majority of survey participants (73%, 35/48) possessed a smart phone, followed by laptop computers (52%, 25/48), desktop computers (42%, 20/48), tablets (23%, 11/48), and other devices (19%, 9/48). Similarly, participants who reported that they would be willing to use V-TTG™ most preferred using smart phones (44%, 21/48), followed by laptop computers (35%, 17/48), desktop computers (25%, 12/48), tablets (21%, 10/48), other devices (17%, 8/48), and finally public computers (8%, 4/48). (Figure 1)
Figure 1. Patients’ device ownership rates and preferred devices for accessing virtual teach-to-goal™ (V-TTG™)*.
*Percent totals exceed 100% because respondents were instructed to select all devices they own or would use. Abbreviations: V-TTG™, Virtual teach-to-Goal™
Participants with asthma compared to COPD were more likely to own a smartphone (88% vs. 44%, p=0.004), have a data plan (77% vs. 38%, p=0.007) and use the internet at least daily (81% vs. 53%, p=0.046). However, there were no significant differences among participants with asthma or COPD with respect to owning laptop, desktop, or tablet computers, use of the internet at their home or their families’, or use of wifi in public (p>0.05). There were also no differences between the groups with respect to willingness to use V-TTG™ at home (p=0.5). (Table 1)
Focus Groups
A total of 9 focus groups with 25 participants took place over the five-month period between December 2013 and April 2014. All participants had diagnoses of asthma and/or COPD. Nine participants returned for the member check meeting.
Themes
Participant comments, grouped under three pre-determined domains of interest: access, functionality, and quality, were then evaluated using inductive analysis to reveal themes within each domain. Themes identified for access were: platform and delivery, internet access, and technological literacy. A representative quote under the access internet theme was: “I do have a friend that she does not have WiFi or – as a matter of fact she don’t have a computer. But, she will go to the library to watch anything and look up anything…” For functionality, themes identified were: usefulness, content, and teaching strategy. A representative quote for the functionality content theme was: “[The module] pertains to my health and it’s helpful because some things I didn’t know and I learned that from that video…” Themes identified for quality were: clarity, ease of use, length, and likeability. A representative quote for the quality likeability theme was: “[T]hat video was fantastic because I could comprehend and I understood everything that she said.”
When applicable, participant comments were also thematically coded as positive or constructive regarding V-TTG™; examples of positive versus constructive quotes can be found in Table 2.
Table 2.
Domains, themes, and representative positive and constructive quotes
| DOMAIN | THEME | POSITIVE QUOTE | CONSTRUCTIVE QUOTE/SUGGESTION |
|---|---|---|---|
| Access | Platform & Delivery | [MODERATOR: What do you think the best way to deliver this video would be?] I think probably email. | [T]here’s a distinction there about how people want to get the information… you can give people the option of how they’re going to get it. |
| Internet Access | [E]verywhere I go… there’s WiFi… I have five sisters and they have WiFi. I have three daughters and they have WiFi so, the majority of the time everywhere I go I’m using WiFi… | [P]robably more people now have DVD players at home than they have Smartphones for example. Or, maybe even internet access so… then you can use a DVD or CD. | |
| Technological Literacy | I think most people in 2014 are just so literate when it comes to these things and like almost everything is password and using it [for] paying bills, looking at a movie… | I don’t think that serves [this] general population. I think you’re going to have… less tech savvy people. | |
| Functionality | Usefulness | Anyone that has any asthma and COPD or anything like that, I think they would really benefit from watching the movie… | [T]hey’re basically fairly simple steps to take. And, you know, why do I need to watch a video to learn how to do this? |
| Content | [A] lot of people think they know how to use their inhaler but they don’t or… there are little things that they’re not doing correctly… [T]his makes sure that you know exactly what you’re doing… | Does your video go further into detail without… using the spacer? … I mean spacer is a very, very good instrument, but the bottom line most people just don’t use it. | |
| Teaching Strategy | One positive thing I would say is that the demonstration was repeated, and so whatever was there, was reinforced… so I thought that was helpful. | I didn’t like the way they kept you asking you the steps… but then… I guess I need to be aggravated because I got it wrong. | |
| Quality | Clarity | I think it is informative and clear. | But why do they mention step 7 and then they don’t say here’s step 1, here’s step 2, here’s step 3? |
| Ease of Use | [T]he drop-down with the options in it makes it a lot easier. | [I]f I was looking at it a really long time I would probably want a bigger font. | |
| Length | It was short and to the point. | I thought it was a little bit too long. | |
| Likeability | [I]t was just really good… easy to follow, self-explanatory. | I don’t know if I would watch it again. It was a little tiring. |
Iterative development of V-TTG™
Further analysis of the themed feedback was completed in order to identify concrete changes that could be made to the V-TTG™. Positive comments led to retention of that aspect of the V-TTG™ with no changes made. Constructive comments were sorted into “able to change” or “unable to change.” Changes made affected three components: videos, questions, or the module as a whole (Table 2). For instance, it was found that the first round of focus group participants (#1–4), who watched the individual videos and reviewed the pre- and post-video questions on paper, had positive comments regarding the conciseness and content of the videos, but questioned the inclusion of the spacer, found certain aspects of the video narrator and demonstrator distracting, and pointed out segments that needed additional clarification. Constructive comments that were deemed changeable informed the revision of the V-TTG™ prior to the second round of focus groups. (Table 3)
Table 3.
Changes made after focus group feedback and survey data with corresponding domains and themes
| Component | Feedback | Change made | Domain | Theme |
|---|---|---|---|---|
| VIDEO | Narrator comment regarding “step 7” confusing; video had made no reference to other steps | Removed comment | Quality | Clarity |
| Preferred explicit demonstration of “whistle” sound created when breathing from spacer too quickly | Added “whistle” sound effect | Functionality | Content | |
| Youtube™ video ads popped up after instructional videos finished | Extended instructional video length to prevent pop-up ads | Quality | Likeability | |
| Did not like video showing incorrect inhaler technique | No change made - differing opinions | Quality | Likeability | |
| Suggested multiple videos for different inhalers | No change made - videos could not be reshot | Functionality | Content | |
| Issues with appearances of video narrator/demonstrator | No change made - videos could not be reshot | Quality | Likeability | |
| QUESTIONS | Wording | Simplified wording | Quality | Clarity |
| Tested redundant and/or nonessential concepts | Removed question | Functionality | Teaching strategy | |
| Preference for drop-down menu vs. manual input or list format | Changed to drop-down format | Quality | Ease of Use | |
| Pre-test questions did not match post-test questions | Changed from 4 pre-test and 6 post-test questions to 6 matched pre- and post-test questions | Functionality | Teaching strategy | |
| MODULE | Include statistics on rates of inhaler misuse | No change made | Quality | Likeability |
| Brought up unfamiliarity with spacer use in target population | Added introduction to spacers and explanation of their importance | Functionality | Content | |
| Requested inclusion of cleaning instructions for spacer | Added instructions | Functionality | Content | |
| Suggested offering multiple options for accessing V-TTG™ | Made V-TTG™ web-based and delivered via email to optimize multimodal access | Access | Platform & Delivery | |
| Need for clarification on which type of inhaler V-TTG™ is targeted towards | Clarified V-TTG™ instruction targeted towards MDI devices | Quality | Clarity | |
| Disliked having to redo all questions if answered any incorrectly | Changed lesson setup so that patients redo only incorrect questions in subsequent rounds | Functionality | Teaching strategy | |
| Wanted feedback for incorrect answers | Feedback given if answer still incorrect after round 3 | Functionality | Teaching strategy | |
| Font size small | Increased module font size | Quality | Ease of Use | |
| Include instructions to rinse mouth with water after use of controller medication | Added instructions | Functionality | Content | |
| Include instructions to call 911 in emergency situation if patient experiences no symptom relief after use of rescue medication | Added instructions | Functionality | Content |
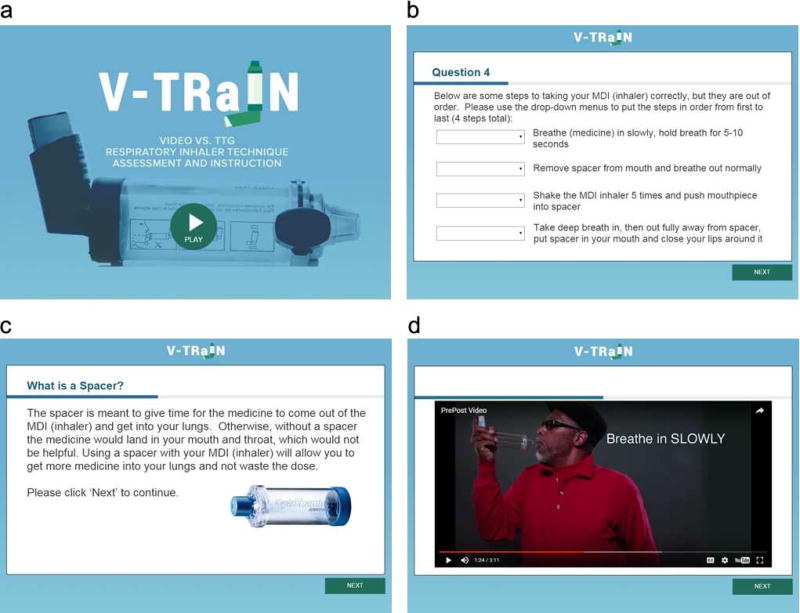
The second round of focus group participants (# 5–6), who watched the videos and separately answered pre- and post-video questions online, gave feedback regarding question wording and areas in which ease of use of the online interface could be improved. Again, constructive comments that were deemed changeable informed the revised V-TTG™ prior to the final round of focus groups. (Table 3) Participants in round three focus groups (#7–9), who completed the full V-TTG™ learning platform, found it highly useful in teaching inhaler technique and noted that the pre- and post-test questions were particularly effective at elucidating aspects of inhaler technique of which they were previously unaware. Any final constructive comments that could be addressed informed the development of the final version of the V-TTG™. (Figure 2)
Figure 2. The finalized virtual teach-to-goal™ (V-TTG™) educational module.
1A: Title screen; 1B: Example question. If answer is incorrect in post-test rounds 1 and 2, prompts to retake the question after reviewing the demonstration; 1C: Additional information on spacer function. 1D: Demonstrator during the video of the correct inhaler technique.
When changes could not be made, it was due to one of four reasons: 1) suggestions went against clinical guidelines, e.g., some participants asked if the demonstration video could show inhaler technique without inclusion of the spacer; 2) participants had differing opinions regarding that aspect of V-TTG™ and did not reach a consensus, in which case the final decision was made according to the research team’s discretion; 3) videos could not be reshot, e.g., some participants commented on aspects of the video narrator and demonstrator that they found distracting, but the videos had been created prior to the focus groups and could not be redone; 4) some suggestions fell out of the scope of the project, e.g., playing the instruction videos in pulmonary clinic waiting rooms.
In order to incorporate all necessary changes, the V-TTG™ went through a total of 7 versions. Member check participants reported a median satisfaction score of 9 (out of 10) with the changes made. The median satisfaction score with the degree to which participants felt their comments had been considered was 10.
Discussion
The findings of the technology survey demonstrated that asthma and/or COPD patients from our hospital population largely have home access to the internet and frequently use it, making baseline access to V-TTG™ a feasible option. However, there were some important differences found between the asthma and COPD cohorts that need to be taken into consideration when implementing V-TTG™ for home use for patients with these different diseases. Feedback from focus group participants praised the ease of use and conciseness of the module, while pinpointing areas of improvement within the user interface. A finalized V-TTG™ module generated high rates of satisfaction among participants in the final member check meeting.
By utilizing a mixed methods strategy that investigated patient technology usage and incorporated end user feedback early in the intervention design process, we were able to refine V-TTG™ for optimal accessibility, acceptability and effectiveness for patient use. The quantitative data from surveys allowed us to broadly determine the appropriateness of V-TTG™ for our population of interest, while qualitative findings from focus groups allowed us to fine-tune V-TTG™ for optimal patient use. Both components of the intervention design process led to the incorporation of end user needs and preferences into the module and better tailored it to our patient population, demonstrating that a V-TTG™ interactive module holds promise as a way to educate hospitalized patients with asthma or COPD about proper inhaler technique.
Focus group feedback was particularly important in improving the functionality and quality of V-TTG™. Constructive comments and suggestions from focus group participants led to several changes that streamlined the user interface experience and increased the clarity of both video demonstrations and wording of assessment questions. Additionally, suggestions that were grounded in participants’ personal experiences with managing asthma or COPD led to the inclusion of content that increased the relevancy of V-TTG™ to our patient population by better addressing their needs and concerns.
Focus group feedback was mixed on the subject of access. Therefore, we supplemented our understanding of any potential access barriers to the internet or to technological devices with data from the technology survey. Preliminary findings from the survey were consistent with prior work done within our local population showing that 65% of the general community uses the internet daily.36 Basic access to V-TTG™ is therefore available to the majority of our patients. From the survey data, it is clear that the majority of patients were open to using technology for health-related information, however, a variety of access types and devices are needed. While the most commonly owned and preferred device was smart phones, no single device was overwhelmingly selected over others. Feedback from our focus group participants that pertained to the theme of access also revealed a similar pattern of heterogeneity in device preference. The final version of our module, therefore, can be used on any device with internet connectivity, maximizing flexibility of access for our patients.
Importantly, implementation of V-TTG™ into home-based interventions will need to consider unique aspects of the target populations. For instance, patients with COPD, who tend to be older than patients with asthma, are less likely to own a smartphone or have a data plan. Therefore, the accessibility of V-TTG™ on any device makes this a feasible intervention for this population. Further, patients with COPD were found to use the internet less often than patients with asthma, so the schedule of use of V-TTG™ needs to take these data into consideration.
An additional learning point from the study was the strength of applying a mixed methods approach to intervention design. While a mixed methods strategy has been increasingly utilized within the realm of medical education research,43 it has been less frequently applied to the design of interventions for patient care. Combining the advantages of qualitative methods that elicit end user perspectives with quantitative approaches may result in improved usability and likeability of clinical interventions.
This study has limitations that should be noted. Both survey participants and focus group members were recruited from a single academic center with a majority African-American patient population. Levels of interest in V-TTG™ and overall relevance to patients may not be generalizable to patients at other clinical sites. Additionally, participants in both the technology study and focus groups were limited to those who spoke English. It is possible that speakers of other languages may have differential technology access and perceptions of V-TTG™’s usefulness and relevance. The technology survey was also a preliminary study with a small sample size that will require further testing when broader samples are collected.
In summary, V-TTG™ shows promise as a web-based educational tool for improving hospitalized asthma or COPD patients’ inhaler technique. It combines the advantages of in-person Teach-To-Goal training with the portability, flexibility, and decreased resources of an online module that patients can access using their own devices post-discharge for increased learning reinforcement. While some technology use and ownership rates differ among patients with asthma compared to COPD, this V-TTG™ intervention was designed for flexible use among technology device types. The completed development and validation of V-TTG™25 positions us well to move forward with further efficacy and effectiveness studies to determine the full impact and range of use for V-TTG™ to enhance patient self-management skills for asthma or COPD.
Highlights Box.
-
What is already known about this topic?
Self-management education has been shown to improve patient care and health outcomes, however, patients often need repeated educational sessions for long-term retention of learned skills. In addition, clinicians often lack the resources to provide training.
-
What does this article add to our knowledge?
We describe the development of an interactive, adaptive learning module that can be used for repeated educational sessions in multiple settings, allowing for a tailored training session to learn effective inhaler technique skills.
-
How does this study impact current management guidelines?
This study provides important insights into using patient feedback to improve a novel technology-based intervention and obtaining pragmatic information on access and willingness to use the module.
Acknowledgments
The authors thank Click to Play Media (Berkeley, CA) for their partnership in developing the videos and Smart Sparrow (Sydney, NSW, Australia) for their partnership in the development of the adaptive learning module. In addition, the authors thank Nicole Twu, Eddie Kim, John Kim, and Ashley Hull for their support throughout data collection. The REDCap project at the University of Chicago is hosted and managed by the Center for Research Informatics and funded by the Biological Sciences Division and by the Institute for Translational Medicine, CTSA grant number UL1 TR000430 from the National Institutes of Health. REDCap (Research Electronic Data Capture) is a secure, web-based application designed to support data capture for research studies, providing: 1) an intuitive interface for validated data entry; 2) audit trails for tracking data manipulation and export procedures; 3) automated export procedures for seamless data downloads to common statistical packages; and 4) procedures for importing data from external sources.
Funding: Dr. Press received funding from the National Heart Lung and Blood Institute (NIH K23HL118151), American Lung Association Social-Behavioral Award, and the American Thoracic Society. Ms. Wu and Dr. Arora were supported by the National Institute on Aging (NIA Grant #4T35AG029795-09). All other authors have no financial support to report.
Abbreviations
- COPD
chronic obstructive pulmonary disease
- QOL
quality of life
- REDCap
Research Electronic Data Capture
- TTG
Teach-to-goal
- V-TTG™
virtual teach-to-goal™
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions: Dr. Press had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: V Press, V Arora, J Farnan; Acquisition of data: N Woodrick, V Press; Analysis and interpretation of data: M Wu, N Woodrick, J Farnan, V Press; Drafting of the manuscript: M Wu, V Press; Critical revision of the manuscript for important intellectual content: M Wu, N Woodrick, V Arora, J Farnan, V Press; Statistical analysis: M Wu, N Woodrick, V Press; Administrative, technical, and material support: N Woodrick, V Press; Study supervision: V Press.
Prior Presentations: Preliminary versions of this work were presented at the American Lung Association Lung Force Expo in 2015 and the Pritzker School of Medicine Summer Research Program Forum in 2016.
References
- 1. [Accessed April 1, 2017];Summary Health Statistics Tables for U.S. Adults: National Health Interview Survey. 2014 Table A-2b Available at: https://ftp.cdc.gov/pub/health_statistics/NCHS/NHIS/SHS/2014_SHS_Table_A-2.pdf.
- 2.NHLBI, National Institutes of Health. Morbidity & mortality: 2012 chart book on cardiovascular, lung, and blood diseases. Bethesda, MD: Author; Feb, 2012. [Accessed March 31, 2016]. Available at: http://www.nhlbi.nih.gov/files/docs/research/2012_ChartBook.pdf. [Google Scholar]
- 3.Wright J, Bracklebank D, Ram F. Inhaler devices for the treatment of asthma and chronic obstructive airways disease (COPD) Qual Saf Health Care. 2002;11:376–382. doi: 10.1136/qhc.11.4.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Global Initiative for Chronic Obstructive Lung Diseases. [Accessed December 9, 2016];Global strategy for diagnosis, management, and prevention of COPD. 2016 Available at: http://www.goldcopd.com/
- 5.NHLBI, National Institutes of Health. Guidelines for the diagnosis and management of asthma (EPR-3) Bethesda, MD: [Accessed January 3, 2017]. Available at: https://www.nhlbi.nih.gov/health-pro/guidelines/current/asthma-guidelines/ [Google Scholar]
- 6.Celli BR, Thomas NE, Anderson JA, Ferguson GT, Jenkins CR, Jones PW, et al. Effect of Pharmacotherapy on Rate of Decline of Lung Function in Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2008;178(4):332–338. doi: 10.1164/rccm.200712-1869OC. [DOI] [PubMed] [Google Scholar]
- 7.Mathison DA, Koziol JA. Utility and Efficacy of Fluticasone Propionate and Salmeterol Inhaled from a Single Inhaler for Persistent Asthma. J Asthma. 2005;42(10):829–831. doi: 10.1080/02770900500369884. [DOI] [PubMed] [Google Scholar]
- 8.Brocklebank D, Wright J, Cates C. Systematic review of clinical effectiveness of pressurised metered dose inhalers versus other hand held inhaler devices for delivering corticosteroids in asthma. BMJ. 2001;323(7318):896. doi: 10.1136/bmj.323.7318.896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McFadden ER., Jr Improper patient techniques with metered dose inhalers: clinical consequences and solutions to misuse. J Allergy Clin Immunol. 1995 Aug;96(2):278–83. doi: 10.1016/s0091-6749(95)70206-7. [DOI] [PubMed] [Google Scholar]
- 10.Braido F, Chrystyn H, Baiardini I, Bosnic-Anticevich S, van der Molen T, Dandurand RJ, et al. “Trying, But Failing” - The Role of Inhaler Technique and Mode of Delivery in Respiratory Medication Adherence. J Allergy Clin Immunol Pract. 2016 Sep-Oct;4(5):823–32. doi: 10.1016/j.jaip.2016.03.002. [DOI] [PubMed] [Google Scholar]
- 11.Press VG, Arora VM, Shah LM, Lewis SL, Ivy K, Charbeneau J, et al. Misuse of respiratory inhalers in hospitalized patients with asthma or COPD. J Gen Intern Med. 2011 Jun;26(6):635–42. doi: 10.1007/s11606-010-1624-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levy ML, Hardwell A, McKnight E, Holmes J. Asthma patients’ inability to use a pressurised metered-dose inhaler (pMDI) correctly correlates with poor asthma control as defined by the Global Initiative for Asthma (GINA) strategy: a retrospective analysis. Primary Care Respiratory Journal. 2013;22(4):406–11. doi: 10.4104/pcrj.2013.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Price DB, Román-Rodríguez M, McQueen RB, Bosnic-Anticevich S, Carter V, Gruffydd-Jones K, et al. Inhaler Errors in the CRITIKAL Study: Type, Frequency, and Association with Asthma Outcomes. J Allergy Clin Immunol Pract. 2017 Mar 9; doi: 10.1016/j.jaip.2017.01.004. pii: S2213-2198(17)30007-7. [DOI] [PubMed] [Google Scholar]
- 14.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, Johnson CA, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS Data Brief. 2012 May;(94):1–8. [PubMed] [Google Scholar]
- 15.Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat 3. 2012 Nov;(35):1–58. [PubMed] [Google Scholar]
- 16.Wier LM, Elixhauser A, Pfuntner A, Au DH. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs [Internet] Rockville (MD): Agency for Health Care Policy and Research (US); 2006–2011. Feb, Overview of Hospitalizations among Patients with COPD, 2008: Statistical Brief #106. [PubMed] [Google Scholar]
- 17.Hasegawa K, Bittner JC, Nonas SA, Stoll SJ, Watase T, Gabriel S, et al. Children and Adults With Frequent Hospitalizations for Asthma Exacerbation, 2012–2013: A Multicenter Observational Study. J Allergy Clin Immunol Pract. 2015 Sep-Oct;3(5):751–8. doi: 10.1016/j.jaip.2015.05.003. [DOI] [PubMed] [Google Scholar]
- 18.Fink JB, Rubin BK. Problems With Inhaler Use: A Call for Improved Clinician and Patient Education. Respir Care. 2005;50(10):1360–75. [PubMed] [Google Scholar]
- 19.Dima AL, de Bruin M, Van Ganse E ASTRO-LAB group. Mapping the Asthma Care Process: Implications for Research and Practice. J Allergy Clin Immunol Pract. 2016 Sep-Oct;4(5):868–76. doi: 10.1016/j.jaip.2016.04.020. [DOI] [PubMed] [Google Scholar]
- 20.Paasche-Orlow MK, Riekert KA, Bilderback A, Chanmugam A, Hill P, Rand CS, et al. Tailored education may reduce health literacy disparities in asthma self-management. Am J Respir Crit Care Med. 2005;172:980–6. doi: 10.1164/rccm.200409-1291OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu HW, Nishimi RY, Page-Loez CM, Kizer KW. Improving patient safety through informed consent for patients with limited health literacy. An implementation report. [Accessed December 15, 2010];National Quality Forum. 2005 Available at: http://www.qualityforum.org/Publications/2005/09/Improving_Patient_Safety_Through_Informed_Consent_for_Patients_with_Limited_Health_Literacy.aspx.
- 22.Press VG, Arora VM, Trela KC, Adhikari R, Zadravecz FJ, Liao C, et al. Effectiveness of Interventions to Teach Metered-Dose and Diskus Inhaler Techniques.A Randomized Trial. Ann Am Thorac Soc. 2016;13(6):816–24. doi: 10.1513/AnnalsATS.201509-603OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Press VG, Arora VM, Shah LM, Lewis SL, Charbeneau J, Naureckas ET, et al. Teaching the use of respiratory inhalers to hospitalized patients with asthma or COPD: a randomized trial. J Gen Intern Med. 2012;27(10):1317–25. doi: 10.1007/s11606-012-2090-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Internet Use Over Time. Pew Research Center; Washington, D.C.: Jan, 2014. [Accessed January 3, 2017]. Available at: http://www.pewinternet.org/data-trend/internet-use/internet-use-over-time/ [Google Scholar]
- 25.Press VG, Kelly CA, Kim JJ, White SR, Meltzer DO, Arora VM. Virtual teach-to-goal™ adaptive learning of inhaler technique for inpatients with asthma or COPD. J Allergy Clin Immunol Pract. 2017 Jan 5; doi: 10.1016/j.jaip.2016.11.018. pii: S2213-2198(16)30576-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Boyde M, Song S, Peters R, Turner C, Thompson DR, Stewart S. Pilot testing of a self-care education intervention for patients with heart failure. Eur J Cardiovasc Nurs. 2013;12(1):39–46. doi: 10.1177/1474515111430881. [DOI] [PubMed] [Google Scholar]
- 27.Heapy AA, Higgins DM, Cervone D, Wandner L, Fenton BT, Kerns RD. A Systematic Review of Technology-assisted Self-Management Interventions for Chronic Pain: Looking Across Treatment Modalities. Clin J Pain. 2015;31(6):470–92. doi: 10.1097/AJP.0000000000000185. [DOI] [PubMed] [Google Scholar]
- 28.O’Hara DM, Seagriff-Surtin P, Levitz M, Davies D, Stock S. Using personal digital assistants to improve self-care in oral health. J Telemed Telecare. 2008;14:150–151. doi: 10.1258/jtt.2008.003016. [DOI] [PubMed] [Google Scholar]
- 29.Sobel RM, Paasche-Orlow MK, Waite KR, Rittner SS, Wilson EAH, Wolf MS. Asthma 1-2-3: A low literacy multimedia tool to educate African American adults about asthma. J Community Health. 2009;34:321–327. doi: 10.1007/s10900-009-9153-9. [DOI] [PubMed] [Google Scholar]
- 30.Moore J, Fiddler H, Seymour J, Grant A, Jolley C, Johnson L, et al. Effect of a home exercise video programme in patients with chronic obstructive pulmonary disease. J Rehabil Med. 2009;41:195–200. doi: 10.2340/16501977-0308. [DOI] [PubMed] [Google Scholar]
- 31.Hawkins SY. Improving glycemic control in older adults using a videophone motivational diabetes self-management intervention. Res Theory Nurs Pract. 2010;24(4):217–232. doi: 10.1891/1541-6577.24.4.217. [DOI] [PubMed] [Google Scholar]
- 32.Haines TP, Russell T, Brauer SG, Erwin S, Lane R, Urry S, et al. Effectiveness of a video-based exercise programme to reduce falls and improve health-related quality of life among older adults discharged from hospital: A pilot randomized controlled trial. Clin Rehabil. 2009;23:973–985. doi: 10.1177/0269215509338998. [DOI] [PubMed] [Google Scholar]
- 33.Creswell J. Research Design: Qualitative, Quantitative, and Mixed Methods Approaches. 4. Thousand Oaks, CA: Sage Publications; 2014. [Google Scholar]
- 34.Meltzer D, Manning WG, Morrison J, Shah MN, Jin L, Guth T, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: Results of a trial of hospitalists. Ann Intern Med. 2002;137(11):866–74. doi: 10.7326/0003-4819-137-11-200212030-00007. [DOI] [PubMed] [Google Scholar]
- 35. [Accessed January 3, 2017];Pew Internet and American Life Project: Data Sets. Available at: http://www.pewinternet.org/datasets.
- 36.Schneider J, Makelarski JA, Haitsma MV, Lipton RB, Abramsohn E, Lauderdale DS, et al. Differential access to digital communication technology: Association with health and health survey recruitment within an African-American underserviced urban population. J Urban Health. 2011;88(3):479–492. doi: 10.1007/s11524-010-9533-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Campbell JL, Quincy C, Osserman J, Pedersen OK. Coding In-depth Semistructured Interviews: Problems of Unitization and Intercoder Reliability and Agreement. Sociological Methods & Research. 2013;42(3):294–320. [Google Scholar]
- 39.Hodson R. Analyzing Documentary Accounts. Thousand Oaks, CA: Sage; 1999. [Google Scholar]
- 40.Pincavage AT, Lee WW, Beiting KJ, Arora VM. What do patients think about year-end resident continuity clinic handoffs? A qualitative study. J Gen Intern Med. 2013;28(8):999–1007. doi: 10.1007/s11606-013-2395-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lee WW, Alureishi MA, Ukabiala O, Venable LR, Ngooi SS, Staisiunas DD, et al. Patient Perceptions of Electronic Medical Record Use by Faculty and Resident Physicians: A Mixed Methods Study. J Gen Intern Med. 2016;31(11):1315–1322. doi: 10.1007/s11606-016-3774-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Boeije H. A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Qual Quant. 2002;36:3392–3340. [Google Scholar]
- 43.Lavelle E, Vuk J, Barber C. Twelve tips for getting started using mixed methods in medical education research. Medical Teacher. 2013;35(4):272–276. doi: 10.3109/0142159X.2013.759645. [DOI] [PubMed] [Google Scholar]