Abstract
Objective
This study aimed to explore the perspectives of caregivers regarding the information and support they received following diagnosis of their child’s hearing loss.
Design
A mixed methods explanatory sequential design was conducted.
Study Sample
A total of 445 caregivers of children completed a written survey, and five parents participated in qualitative in-depth interviews.
Results
The most common sources of information for caregivers were discussion with an audiologist, written information, and discussion with a medical professional. Approximately 85% of caregivers reported they were satisfied with the personal/emotional support and information received from service providers. Additional comments from 91 caregivers indicated that 11% experienced a breakdown in information transfer with health professionals. Interviews conducted with 5 parents from 3 families revealed two themes which described the diagnostic period as a difficult and emotional experience for parents: (1) support and information provided during diagnosis: what happens first?; and (2) accessing early intervention services following a diagnosis of hearing loss: navigating the maze.
Conclusions
The findings of this study give insight into the perspectives of caregivers who have a child diagnosed with hearing loss. The importance of providing timely information and personal/emotional support to caregivers cannot be underestimated.
Keywords: pediatric, psycho-social/Emotional, cochlear implant, hearing aids
In Australia, children with a condition that may lead to a developmental disability or delay are offered early intervention services from birth to school entry, with the majority of children entering school between the ages of 5 and 6 years. All children and young adults who are identified with a permanent or long-term hearing loss are referred to Australian Hearing, the national service provider, for assessment, diagnosis, the provision amplification devices and ongoing follow-up (Australian Hearing, 2014). This process of assessment and diagnosis of hearing loss in a young child can be a very difficult and overwhelming time for parents (e.g., Kurtzer-White & Luterman, 2003; Rice & Lenihan, 2005; Russ et al., 2004). A number of studies have explored parent reactions and emotions associated with a diagnosis of hearing loss (Fitzpatrick et al, 2008; Gilliver et al, 2013; Kampfe, 1989). Throughout the diagnostic process, parents of children with hearing loss typically move through a cycle of grief, including shock, recognition, denial, acknowledgement, and action (Kampfe, 1989; Kurtzer-White & Luterman, 2003). During this emotional time, parents are expected to make significant decisions regarding their child’s early intervention, often very quickly following the diagnosis (Decker, Vallotton, & Johnson, 2012; Matthijs et al., 2012). One of the first decisions that must be made concerns the use of hearing technology, including hearing aids and cochlear implants (Matthijs, et al., 2012). Parents also need to make decisions regarding their child’s mode of communication (e.g., Crowe et al., 2014a, 2014b; Gravel & O’Gara, 2003).
A number of studies have explored parent perceptions of the process of diagnosis of hearing loss and the information and support they received. A recent Australian study conducted in South Australia explore the perceptions of parents of children with cochlear implants regarding the support and services they had received following their child’s diagnosis with hearing loss (Roberts et al., 2015). Qualitative interviews with parents from 14 families indicated that while the majority of parents were satisfied with the services they received, some parents were dissatisfied with non-specialised teaching staff and the amount of technical support they received for device management.
In another Australian study conducted before universal newborn hearing screening was implemented in Victoria, 82 parents completed an open-ended questionnaire regarding their experiences during the diagnostic and early intervention period (Russ et al, 2004). Following the risk-based screening process, parents in this study described lengthy delays before an actual diagnosis was confirmed, leaving them feeling frustrated, anxious, and helpless. Furthermore, parents felt that they received unclear explanations about the hearing loss, and perceived the advice they received to be misleading or incorrect.
More recently, Gilliver et al. (2013) explored the recollections and experiences of 40 parents of children who were diagnosed with hearing loss before three years of age in Australia. Parents completed a written questionnaire consisting of open-ended questions relating to the timing of diagnosis and their reactions to this news. Parents were also asked to reflect on their experiences regarding amplification and intervention options, and how this affected their family. Substantial grief-related reactions to diagnosis were reported, with parents utilizing a wide range of support and information during this period, including the Internet, family, friends, and contact with audiologists. Parent perceptions of the level of support provided by audiologists was mixed. While many parents reported that they did not receive enough information, others reported positive support from audiologists. Although some parents of earlier diagnosed children expressed that they wished they had more time to enjoy their newborn before having to deal with the identification of hearing loss, most parents felt earlier diagnosis was beneficial in order to access earlier intervention.
In addition to the challenges faced by caregivers regarding the provision of information at diagnosis, caregivers have also reported feeling overwhelmed by the decision they must make following this information regarding their child’s educational intervention and questioned whether they had enough information to select an appropriate communication mode for their child (Eleweke & Rodda, 2000). In relation to this, a body of research has highlighted that many parents are strongly influenced by the information they receive from professionals (Crowe et al, 2014a; Eleweke & Rodda, 2000; Li et al, 2003; Roberts et al, 2015; Steinberg et al, 2003), especially in the period immediately after the diagnosis of their child’s hearing loss (Eleweke & Rodda, 2000). Thus, it is clearly important to consider the potential influences of information provided to parents at diagnosis regarding communication mode and early intervention options.
Decker and colleagues (2012) conducted an online survey with 36 parents of children with hearing loss in the US regarding the information they received at diagnosis and how they felt this information influenced their decisions. Findings revealed that parents who chose an oral communication method received information from sources that were more likely to align with a medical model of hearing, such as speech pathologists and audiologists. In contrast, parents who chose to incorporate sign language were more likely to receive information from a wide range of other sources such as friends, family members, and commercial agencies. Despite parents reporting that the main source of influence was their own judgement and the other parent’s opinion, Decker and colleagues questioned whether parents may have internalised the views of professionals and hence, believed that they were influenced by their own decisions rather than outside sources.
Research to date has clearly highlighted the important role that professionals play in providing information and support to parents following a diagnosis of hearing loss. However, despite the important contribution these studies have made to the literature, the majority of these studies have used a single survey methodology to collect data, potentially limiting the scope of information that could be gathered from parents. Further research with a larger number of participants, including qualitative data, is required to explore parents’ perspectives of the diagnosis and intervention decision process, and importantly, a population-based study that includes children with hearing loss who had access to early diagnosis and early intervention. Such research is especially vital now that universal newborn hearing screening has been implemented widely across the world, including Australia (Ching et al, 2013). In order to obtain findings relevant to Australian families exposed to early management of hearing loss, this study aimed to explore the perspectives of caregivers across Australia on the information and support received during the diagnostic period, and their satisfaction with these services.
Method
Research Approach
This study utilised a mixed methods sequential explanatory design, consisting of quantitative and qualitative phases. Mixed methods research is beneficial because it allows research questions to be explored that could not be answered by quantitative or qualitative methods alone (Creswell & Plano Clark, 2011). A sequential explanatory design was chosen for this study as it provides the opportunity to further explore the quantitative data collected in Phase 1, with the use of a qualitative method in Phase 2 (Creswell & Plano Clark, 2011; DiCicco-Bloom & Crabtree, 2006).
The data for Phase 1 of this study were collected through the Longitudinal Outcomes of Children with Hearing Impairment (LOCHI) study (Ching et al., 2013), with data for Phase 2 collected subsequently as an extension of the LOCHI study. The LOCHI study is a population-based cohort study of Australian children with permanent hearing loss designed to examine the speech, language, academic, psychosocial, and functional outcomes of these children in a prospective manner. Families residing in the Australian states of New South Wales (NSW), Victoria (VIC), and Southern Queensland (QLD) were invited to participate in the LOCHI study if their child with hearing loss: (1) was born between 2002 and 2007; and (2) accessed services at an Australian Hearing centre before their third birthday. The three states each commenced universal newborn hearing screening (UNHS) programs within a three-year period between 2002 and 2005. In NSW, the UNHS program achieved >95% coverage in 2003. On the other hand, the roll-out of the program was a staged process in QLD and VIC, with different regions of each state commencing screening progressively over periods of 2 and 6 years respectively (Ching et al. 2013). Australian Hearing is the national service provider for children, adolescents, and young adults with hearing loss. Once enrolled in the study, children were evaluated at 6 and 12 months after initial fitting of hearing aids or cochlear implantation, and subsequently at chronological ages of 3, 5 and 9 years of age. Ethical approval for this study was obtained from the Behavioural and Social Sciences Ethical Review Committee of The University of Queensland and the Australian Hearing Human Research Ethics Committee.
Phase 1
Participants
The caregivers of all children participating in the LOCHI study were asked to complete a questionnaire as part of the assessment battery. The questionnaire consisted of a range of open and closed response questions, related to demographic information and recollections of the services and information they received at the time of diagnosis of their child’s hearing loss. Caregivers received the questionnaires by post, and were asked to return the completed forms either by post or in person to the researcher who performed direct assessments of the children. Of the 457 families who were sent the questionnaires, valid responses were received from 445 caregivers. Participant demographics are presented in Table 1. Respondents had children who were, on average, 27.9 months of age at the time of data collection (range = 5.3 – 79.8 months; SD = 17.7 months). The mean duration between age at diagnosis and data collection was 21.7 months (range = 5 – 76 months; SD = 15.03 months). For two families, either the teacher or interpreter, assisted in completing the questionnaire in the form of an interview with the caregiver, and are therefore in both these cases, the teacher and interpreter are reported as the participant in Phase 1.
Table 1.
Participant Demographics: Phase 1
| Characteristic | N = 445 | % |
|---|---|---|
| Survey Respondents | ||
| Mother | 411 | 92.4 |
| Father | 23 | 5.2 |
| Foster mother | 4 | 0.9 |
| Grandmother | 4 | 0.9 |
| Mother-father dyad | 1 | 0.22 |
| Teacher | 1 | 0.22 |
| Interpreter | 1 | 0.22 |
| Location | ||
| New South Wales (NSW) | 228 | 51.24 |
| Victoria (VIC) | 122 | 27.42 |
| Queensland (QLD) | 91 | 20.45 |
| Australian Capital Territory (ACT) | 4 | 0.1 |
| Child participants | ||
| Gender: male | 242 | 54.4 |
| Maternal Education | ||
| University qualification | 169 | 37.98 |
| Diploma/Certificate education | 114 | 25.62 |
| 7–12 years formal | 143 | 32.13 |
| 1– 6 years formal education | 7 | 1.57 |
| Undisclosed | 12 | 2.70 |
| Paternal Education | ||
| University qualification | 142 | 31.91 |
| Diploma/Certificate | 140 | 31.46 |
| 7–12 years formal education | 109 | 24.49 |
| 1 – 6 years formal education | 2 | 0.45 |
| Undisclosed | 52 | 11.69 |
| Hearing Device | ||
| Bilateral hearing aids | 248 | 55.73 |
| Bilateral cochlear implant | 80 | 17.98 |
| One cochlear implant & one hearing aid | 47 | 10.56 |
| Unaided | 36 | 8.09 |
| Unilateral hearing aid | 21 | 4.72 |
| Unilateral cochlear implant | 13 | 2.92 |
| Hearing screening status | ||
| Screened | 327 | 73.48 |
| Passed | (23) | (5.17) |
| Referred | (286) | (64.27) |
| unknown | (18) | (4.04) |
| Not screened | 81 | 18.20 |
| Unknown | 37 | 8.31 |
| Ethnic background | ||
| English-speaking background | 316 | 71.01 |
| Non-English-speaking background | 119 | 26.74 |
| Unknown | 10 | 2.25 |
Procedure
Responses to two questions relevant to the aims of the present study were analysed in this paper. The first question aimed to find out what information and/or support was received by the caregivers at the time of diagnosis of their child’s hearing loss. The allowable responses included a list of options as well as an open invitation for comments and specifications. Specifically, the first question asked: “What information and/or support were you given to help you at the time you learned your child had a hearing loss?” Caregivers indicated what information and/or support they received from a list of seven responses including: (1) written information; (2) discussion with audiologist; (3) discussion with general practitioner; (4) discussion with medical specialist (e.g., pediatrician, ENT specialist); (5) discussion with teacher/habilitationist; (6) professional support/counselling; and (7) support from another parent/parent support group. Caregivers were instructed to select all responses that applied, and if they wish, to provide some comments in the space provided. The second question aimed to determine the level of satisfaction of the caregivers with the information and/or support provided. Therefore, a rating scale was provided, together with an invitation for comments. Specifically, the second question asked: “How satisfied were you with: (a) the personal/emotional support; and (b) the information you were given at the time you learned your child had a hearing loss?” Caregivers were asked to rate their satisfaction with regards to the personal and emotional support and the information they received on a scale from 1 to 5 (1 = not satisfied; 3 = OK; 5 = satisfied). Respondents also had the opportunity to provide further qualitative comments on these questions.
Analysis
Descriptive analysis was conducted on the data to explore what information and support was provided to caregivers at the time of diagnosis, and their satisfaction with these services. Additional qualitative data from the open-ended questions was analysed using summative content analysis. Summative content analysis is a flexible method for analysing text data (Hsieh & Shannon, 2005). It involves firstly identifying and quantifying certain words in the text, and then categorizing these words or phrases, with the occurring frequency listed beside each category. Latent content analysis was then used to interpret the text data, as this method focuses on discovering the underlying meaning of the content (Babbie, 2010). This analysis subsequently informed the design of Phase 2 of the study, including the aims and methodology of Phase 2.
Phase 2
Participants
Five parents, from three families, participated in Phase 2 of this study (see Table 2 for participant demographics). Two of the three families resided in Queensland, with the third family residing in Victoria. These families were recruited as part of a sub-study to the LOCHI project, which had a focus on exploring the nature of parental involvement in the intervention of children with hearing loss (Erbasi et al., in press). Parents were eligible for this sub-study if their child with hearing loss had a nonverbal cognitive ability score of ≥85 (Wechsler Non Verbal Scale of Ability; Wechsler & Naglieri, 2006) and had received educational intervention over the past 3 years. A letter of invitation to participate in this sub-study was sent to 224 eligible families with a reply-paid envelope. A total of 51 families expressed an interest in participation. Due to time and resources, 3 families who provided informed consent were recruited using maximum variation sampling to reflect families of children who were diagnosed at different ages, with different degrees of hearing loss, and where fathers, as well as mothers consented to participate in an interview. Maximum variation sampling is a form of purposive sampling that is used in order to provide diverse perspectives and capture common patterns that are shared among the cases explored (Patton, 2002).
Table 2.
Participants Demographics: Phase 2
| Family 1 | Family 2 | Family 3 | |
|---|---|---|---|
| Respondents | Mother Father |
Mother Father |
Mother |
| Age of Child at time of interview (years) | 9 | 7 | 7 |
| Gender of Child | Male | Male | Female |
| Screening status | Not screened | Screened: Bilateral refer | Not screened |
| Age at Diagnosis of Child’s HL (months) | 24 | 1 | 15 |
| Age at Fitting of Hearing Aids (months) | 25 | 2 | 16 |
| Age at Cochlear Implant (months) | N/A | 10 | 20 |
| Hearing Devices used By the Child | Bilateral Hearing Aids | Bilateral Cochlear Implants | Bilateral Cochlear Implants |
| Unaided Pure Tone Average in Better Ear at 5 years |
Moderate 53.8 dB HL |
Profound (>90dB) |
Profound (>90dB) |
| Parent Education | University | University | University |
| English-speaking background | Yes | Yes | Yes |
Procedure
Following analysis of Phase 1 data, individual semi-structured in-depth interviews were conducted with parents to expand on the results of Phase 1. These interviews were conducted as part of the broader sub-study exploring parent involvement in the early intervention process (Erbasi et al., in press). The interviews were conducted by the second author (EE), an experienced audiologist, unknown to the families. Each participant was interviewed in their own home, with the parents from Family 1 interviewed together, and the parents of Family 2 interviewed on separate occasions. The interview questions for the current study were designed to increase understanding of specific issues raised in Phase 1, including further exploration of parents’ satisfaction and experience with the information and support provided to them after the diagnosis of hearing loss in their children. The current study employed a similar case study design to that used by Eleweke and Rodda (2000), who examined the factors contributing to a parent’s selection of a communication mode for their child with hearing loss. Case study method designs are beneficial because they enable various data to be studied in relation to each other and from different aspects (Gummesson, 1988). In particular, this methodology allows for tailoring the design and data collection procedures to the research question (Meyer, 2001). In-depth interviews are often used in case study method designs (Meyer, 2001), as they allow for documentation of a participant’s perspective on the topic, active engagement from both the interviewer and interviewee to identify and discuss issues, and flexibility and scope for further probing in the discussion of an issue (Simons, 2009). Each interview was audio recorded and transcribed verbatim by a professional transcription service. The duration of interviews ranged from 81 to 124 minutes (M = 95 minutes; SD = 19.92 minutes).
Analysis
Qualitative thematic analysis using the 6-phase approach described by Braun and Clarke (2006) was undertaken in order to identify relevant themes relating to the research aims. Thematic analysis aims to place emphasis on the meaning of data, and the description and experiences of participants (Braun & Clarke, 2006; Simons, 2009).
As described by Braun and Clarke (2006) and implemented by researchers including Eleweke and Rodda (2000) and Russ et al., (2004), codes and quotes from the case study interviews were initially extracted via detailed reading and re-reading of the interview transcripts. A process of inductive coding was used to identify patterns and meanings relevant to the research question throughout the entire dataset. These codes were then collated into potential themes to create both overarching themes and sub-themes that captured the experiences of the parents in this study regarding the information and support they received at diagnosis of their child’s hearing loss. Following identification of these themes and sub-themes, the coded transcripts were reviewed in order to ensure that the identified themes reflected the interview data. Themes were refined and transcripts were subsequently re-coded during this continuous and iterative process (Braun & Clarke, 2006).
Rigour
The authors used a number of techniques in order to ensure the trustworthiness of the data collected and analysed. Firstly, data was triangulated by asking the same questions of both the mothers and fathers who participated in the study. Examination of this data revealed that the data was consistent between the two sources. Secondly, the research team regularly reviewed the findings throughout the data analysis process, with regular research meetings being held with the first, second, and third authors, who reviewed the coding of the data and discussed the emerging findings, reorganising and refining each theme in line with the consensus reached by the team. Finally, following completion of the data analysis, participant checking was conducted, with participants being sent a written summary of the main findings and asked to provide feedback. Responses to this process were received from all 5 parents, who supported the investigators interpretation of their experiences and perceptions of the information and support they received following diagnosis of their child’s hearing loss.
Results
Phase 1
Information and/or support provided to caregivers
Table 3 provides a summary of the responses to Question 1 of the survey, showing that majority of caregivers received information from discussions with an audiologist or written sources. Only about 6% (n = 28) of caregivers reported having received information from another parent or parent support group.
Table 3.
Information and Support Provided to Families at Diagnosis (Question 1) N = 445
| Respondents received information and support from: | n | % |
|---|---|---|
| Discussion with the Audiologist | 387 | 86.97 |
| Written Information | 271 | 60.90 |
| Medical Specialist | 193 | 43.37 |
| Professional Support/Counselling | 94 | 21.12 |
| Teacher/Habilitationist | 51 | 11.46 |
| General Practitioner | 47 | 10.56 |
| Support from Another Parent/Support Group | 28 | 6.29 |
Caregiver satisfaction with personal/emotional support from service providers
The vast majority of caregivers (85.3%; n = 1540) indicated on Question 2 that they were satisfied (i.e., provided a rating of 3, 4 or 5) with the personal/emotional support they received from service providers following diagnosis of their child’s hearing loss. Although consistently high, the level of satisfaction with personal/emotional support varied across service providers with caregivers reporting the highest level of satisfaction with their teacher/habilitationist (94.1%; n = 207), closely followed by the audiologist who provided the hearing aids (92.3%; n = 207), other parents (87.7%;n = 100), counsellor (85.7%; n = 96), medical specialist (82%; n = 278), diagnostic audiologist (79.6%; n = 313), and finally, their general practitioner (78.1%; n = 185). A total of 14.7% (n = 266) of respondents across the sample reported that they were dissatisfied (i.e., provided a rating of 1 or 2 across all the service providers) with the personal/emotional support provided by their services providers, particularly the general practitioner (21.9%; n = 52) and the diagnostic audiologist (20.4%; n = 80). Further details regarding caregiver’s satisfaction with the personal/emotional support given by service providers is outlined in Figure 1.
Figure 1.
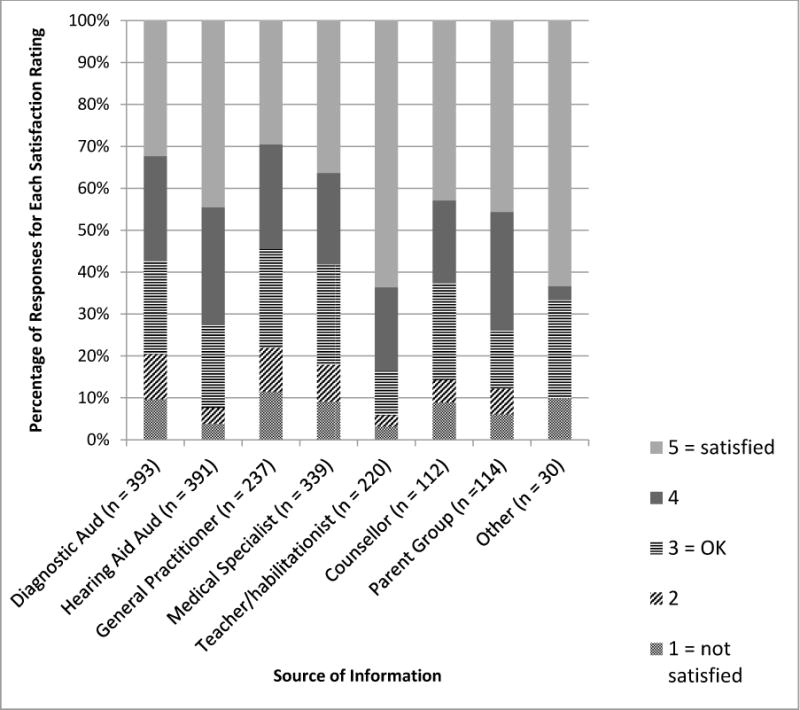
Satisfaction with emotional/personal support provided to caregivers at time of diagnosis by service providers (Question 2a).
Caregiver satisfaction with information from service providers
Similarly to caregiver satisfaction with the personal/emotional support provided by service providers, the vast majority of caregivers (85.5%; n = 1613) also indicated on question 2 that they were satisfied (i.e., provided a rating of 3 or above) with the information they received from service providers. Although consistently high, the level of satisfaction with information provided by service providers varied, with caregivers reporting the highest level of satisfaction with information from their teacher/habilitationist (95.8%; n = 204), closely followed by the audiologist who provided the hearing aids (92.7%; n = 345), written information (91.1%; n = 163), other parents (89%; n = 89), counsellor (84.5%; n = 87), medical specialist (83.2%; n = 267), diagnostic audiologist (82.8%; n = 345), and finally, their general practitioner (66.1%; n = 146). A total of 15.1% (n = 273) of respondents reported that they were dissatisfied (i.e., provided a rating of 1 or 2) with the information they received from services providers, particularly their general practitioner (33.9%; n = 75), the diagnostic audiologist (17.2%; n = 65), and their medical specialist (16.8%; n = 54). Further details regarding caregiver’s satisfaction with the information provided by service providers is outlined in Figure 2.
Figure 2.
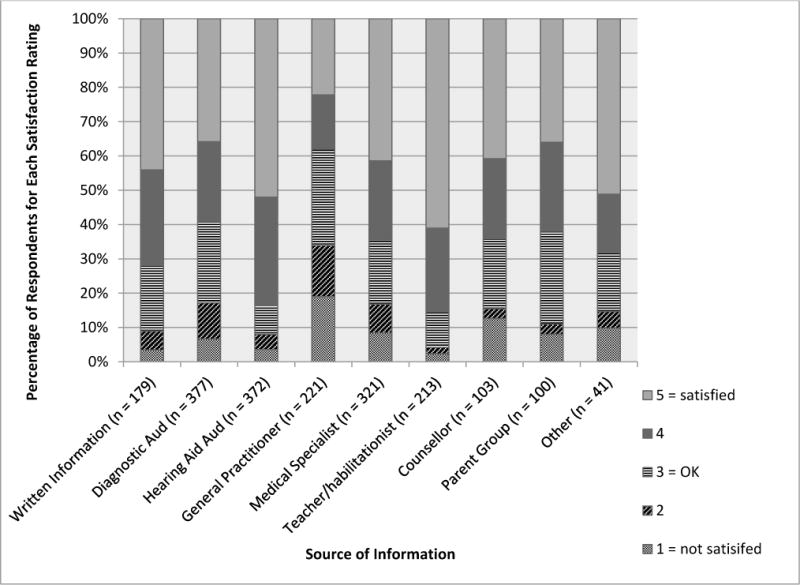
Satisfaction with information content provided to caregivers at time of diagnosis by service providers (Question 2b).
Open ended responses regarding satisfaction with personal/emotional support and information
In addition to the closed response questions, caregivers also had the opportunity to provide additional comments about the personal/emotional support and information they were given at the time of diagnosis of their child’s hearing loss. Analysis of the 91 additional comments provided by caregivers revealed a range of perceptions and experiences from these caregivers, with seven categories and a number of sub-categories identified in the data. Whilst 23 out of the 91 additional comments (25%) made reference to the services and advice received being supportive, a number of comments provided by caregivers indicated that there was limited support provided at initial diagnosis, including a delay in accessing services and confirmation of the results of the hearing test, and a breakdown in information transfer between hearing professionals and caregivers, including misinformation and a perceived lack of professional knowledge. Caregivers also made reference to the diagnosis being an overwhelming shock, with some respondents recommending that a counsellor be present at the time of diagnosis. The list of categories and their corresponding frequencies in the data are displayed in Table 4.
Table 4.
Additional Information Provided by Parents in Questionnaire (n = 91)
| Category | Frequency Identified in Data | Sub-category (if applicable) | Frequency Identified in Data |
|---|---|---|---|
| Limited support and information provided at initial diagnosis | 39 | ||
| The services and the advice received was supportive | 20 | Support improved with access to other services | 3 |
| Diagnosis was an overwhelming shock | 8 | Recommendation of a counsellor to be present at time of diagnosis | 6 |
| Misinformation and perceived lack of knowledge by hearing professionals | 7 | ||
| A delay in accessing services and receiving confirmation of results | 5 | ||
| Lack of understanding of what was communicated by health professionals | 3 |
Frequency identified in data = number of times category or sub-category mentioned by a participant.
Phase 2
Two themes were identified from the Phase 2 interview data, which captured the experiences of five parents regarding their perspectives on the information they received at the time of diagnosis of their child’s hearing loss. The two themes were: (1) support and information provided during diagnosis: what happens first?; and (2) accessing early intervention services following a diagnosis of hearing loss: navigating the maze. Each of these themes and related sub-themes are discussed below with example participant quotes.
Theme 1. Support and information provided during diagnosis: What happens first?
Analysis of the interviews revealed that the process of diagnosis was a difficult and emotional experience for parents. This theme incorporated a number of sub-themes, including: (a) health professionals’ breaking the news; (b) parental emotions at diagnosis; and (c) why the use of hearing aids?
Health professionals’ breaking the news
Each parent described in detail their experiences when they received the news that their child had hearing loss. Parents noted that this was a “disconcerting” time for them, especially given that detailed hearing tests often occurred with little information about the process of testing a child’s hearing. Audiologists and Ear Nose and Throat (ENT) surgeons played an integral role as information providers during the initial stage of diagnosis. With each of the five parents, an audiologist provided the initial diagnosis of hearing loss. Both parents in Family 2 independently reported during their individual interviews that they felt the diagnostic audiologists were secretive, “whispering amongst each other” (Mother, Family 2), and that despite verbal reassurance, the audiologist’s non-verbal communication indicated an impression of worry:
They kept calling more and more audiologists into the room and sort of whispering behind their hands, which was incredibly disconcerting as parents. It’s like ‘Oh, well, we know you’re saying he’s deaf. Come on, just come out and say it,’ and then they eventually did. But their non-verbals, they’re talking behind their hands, they’re worried, worried (Father, Family 2).
When informed of their child’s diagnosis of hearing loss, some parents perceived that this was done with a lack of empathy. One parent shared that,
They [audiologist] said ‘Look, he can’t hear over 100 decibels and we think he’ll be a good candidate for the cochlear implant and here’s a big folder and we’ll book you in to see an ENT.’ It was kind of very short … it was probably like a five minute conversation afterwards of like ‘This is what it could be’. I didn’t know what a good candidate for a cochlear implant meant or anything like that (Mother, Family 2).
Another parent stated that the audiologist broke the news by saying “He’s got permanent hearing loss and you’ll have to go to the doctor for it to be explained” and “I cried obviously and then I was sent out into the full waiting room to pay my bill and leave. It was awful” (Mother, Family 1).
Frustration about having to be referred onto an ENT surgeon for further information following the diagnostic test was echoed by another parent who said: “So we went to the audiologist and she wasn’t allowed to say anything, which was very frustrating. We had to go to the specialist to get the official diagnosis” (Mother, Family 2).
Parental emotions at diagnosis
It was apparent that parents felt a range of emotions when their child was diagnosed with hearing loss. It was described by one parent as “not an easy process” (Father, Family 2). Parents stated that it was an overwhelming and daunting time, with an array of emotions identified, including denial and sadness. One parent stated “I was in shock and I didn’t quite believe it was as bad as that I suppose. … and my brain was kind of going overtime” (Mother, Family 3). Another parent reported that they felt they didn’t know what to expect, thinking their child may “miss out on a whole lot of stuff in life” (Mother, Family 1). One parent also reflected on the grief they felt when they learned of their child’s hearing loss: “…had a bit of grief for a while, vowed not to tell our – well I said that I wasn’t going to tell my family until I knew more, because I didn’t think they would understand really what that meant” (Father, Family 2).
Why the use of hearing aids?
Caregivers in the study who had children with profound hearing loss expressed confusion regarding the necessity for hearing aids when “it didn’t seem like [he] had any hearing” (Mother, Family 2). This mother in particular discussed “this kind of hope and despair cycle” of hearing aid assessments to identify if their child had any access to speech sounds. Another parent felt that the hearing aids process was “stressful” and “very frustrating … and you never felt like you’d achieved anything much of a result with hearing aids” (Father, Family 2). This father did comment however that despite being frustrating, the hearing aids perhaps “got the auditory centre of the brain well and truly stimulated and that probably helped us get into language quicker.”
Theme 2. Accessing early intervention services following a diagnosis of hearing loss: Navigating the maze
The second theme related to parents’ perspectives and experiences when accessing appropriate professionals and early intervention providers following the diagnosis of their child’s hearing loss. Two sub-themes were identified within this theme: (a) understanding the role of service providers at initial diagnosis is a confusing process; and (b) information provided in the early stages: the next step.
Understanding the role of service providers at initial diagnosis is a confusing process
Following the initial diagnosis of hearing loss from the audiologist, parents reported that they were required to navigate a range of service providers and professionals. Parents in the study noted confusion surrounding the role of various professionals with one parent saying “I didn’t understand what her [the ENT] role was. I don’t know what an ENT surgeon does as opposed to [another health professional], I just didn’t know” (Mother, Family 3). Another parent commented, “So the next step that we knew about was the ENT and we also knew that there was [hearing service provider] … but we didn’t know what they offered” (Mother, Family 2). Parents reported that they were confused about the various roles of the service providers. One parent commented extensively on this difficulty stating,
As a parent [it’s] quite confusing, because you’ve got the [hearing service provider] and then you’ve got the early intervention agency and you can’t quite work out – and then you’ve got the ENT person and then you’ve got the audiologist and it takes you a while to work out I think how those different levels work and how they’re helping in different ways. So that was a bit confusing I suppose (Mother, Family 3).
Information provided in the early stages: The next step
Participants in the study received information from a range of sources including medical professionals and written sources. All parents reported receiving information from the ENT surgeon. Overall, parents commented that the information provided by the ENT during the early stages was minimal, with one parent stating, “he drew a little picture about the ear and – no I don’t recall much information. It was very short” (Mother, Family 1). Another parent highlighted that the ENT surgeon only provided her with the names of three early intervention centres on a piece of paper: “I was just given this little piece of paper with three phone numbers and three names that meant nothing to me. I didn’t know what early intervention meant. If you haven’t been part of it you don’t know what those words mean. So those words are being handed to you as though you understand what it means, but you’ve got no idea at all” (Mother, Family 3). Another family commented that the ENT “just sent us to [early intervention provider]” (Mother, Family 1), and no other options were provided at the time.
With regards to written information, one parent responded that she was provided with the written information booklet “Choices”. Choices is a booklet designed to guide parents and families of children newly diagnosed with hearing loss through the first six months. Confusion surrounded the information provided in the booklet, with the participant commenting that “… the Choices booklet I just found bewildering just trying to go through it myself” as the booklet “seemed to be talking about the different early intervention models but we didn’t know which centres were attached to those different models” (Mother, Family 2).
Another parent reported that although she received written information from Australian Hearing, it would have been helpful to receive written information from the ENT as well. She noted that,
It wasn’t well managed in terms of the information. There was no printed flyer that could have had just some very basic straightforward information about what Australian Hearing does, what the cochlear implant clinic does, what early intervention is, their contact numbers, this is the likely process … some broad general information sheet would have been terrific (Mother, Family 3).
After accessing a range of information from various early intervention providers and professionals, parents discussed the need to make decisions quickly regarding their choice of communication mode and early intervention provider for their child. Although one parent reported that service providers encouraged them to take their time to consider all options, parents still felt that they “had to make a really quick choice” (Mother, Family 2) because “we wanted to get things underway and were reading about earlier is better” (Mother, Family 2). Another parent stated that he thought “there’s hardly any time required to make this decision” (Father, Family 2). Thus, the desire to make decisions quickly was important to the families in this study.
Discussion
This study aimed to explore the perspectives of caregivers regarding the information and support received during the diagnosis of their child’s hearing loss and their satisfaction with these services. The study used a two-phase approach to answer these research questions. In the Phase 1 written survey, it became apparent that the most common sources of information for caregivers at the time of diagnosis were through discussions with an audiologist and/or written information. Parents who participated in the Phase 2 in-depth interviews reported receiving the majority of information from specialist medical professionals, including ENTs. This finding is consistent with the study by (Decker, et al., 2012) who also found that most parents (71%) received information from an audiologist and medical professionals.
A positive finding from Phase 1 of this study was that the overwhelming majority of caregivers reported being satisfied with the personal/emotional support and information provided by service providers. This finding is consistent with Robert et al’s (2015) qualitative study, where most parents reported a high level of satisfaction with medical, audiology, and early intervention services, providing further evidence that, for the majority of families, existing support systems appear to be effective in terms of providing information and support. Interestingly, the high level of satisfaction reported by participants in the current study is higher than the overall satisfaction reported by the 82 parents of children with hearing loss in the Russ et al., (2004) study, where only 24% of parents reported being satisfied with the diagnostic period.
It is important to note however that despite the majority of caregivers in the current study being satisfied with the support system, approximately 15% of caregivers reported feeling dissatisfied with the personal/emotional and informational support from some service providers, particularly their general practitioner and the diagnostic audiologist. Interestingly, each of these service providers would most likely align with a medical model of hearing (Senghas & Monaghan, 2002) in their interactions with caregivers. Although the medical approach is an important component of the early diagnostic period, with a justified focus on the medical diagnosis of a hearing loss, and early intervention options from a medical perspective, it is possible that the personal/emotional needs of some caregivers are not necessarily being met by these professional groups. This highlights the importance of ensuring medical professionals and diagnostic audiologists are aware of the support needs of families during this period. In addition, as research indicates that parents who receive initial information from professionals working within a medical model of hearing may be less likely to pursue other sources of information such as friends, families, and other agencies (Decker et al., 2012; Kluwin & Stewart, 2000), it is essential that professionals provide objective, clear, and sufficient information to parents, so that they can source the information they need to make informed decisions for their individual child and family (Graval & O’Gara, 2003).
The fact that the majority of respondents in the current study received written information is a positive finding, as the provision of written health information has been identified as an important consideration for parents of children newly diagnosed with hearing loss (Fitzpatrick et al., 2008). In the Australian context, the provision of written information about childhood hearing loss and choices is part of the audiological protocol of the national hearing service provider, Australian Hearing, for families with children newly diagnosed with hearing loss (Choices, Australian Hearing, https://www.hearing.com.au/wp-content/uploads/2013/09/4712_1173929249618_Choices-national.pdf). The present study did not investigate other sources of written information that the families might have received or accessed.
Whilst the vast majority of caregivers were satisfied with the information provided by service providers, additional comments provided by respondents on the written survey revealed that some caregivers felt that the support and information provided at initial diagnosis was limited. These findings were elaborated by parents in Phase 2 of the current study, with some parents reporting that they received information from a range of health professionals, including audiologists and ENTs. However, discussions with these professionals were reported to be short, with minimal written information and support offered at this time. Literature has suggested that information required by parents is not limited simply to information specifically about the hearing loss, but also prognostic information, and information related to educational intervention and other resources in the community, such as parent support groups and home support services (Fitzpatrick, et al., 2008). Another important consideration is that given written information appears to be a major source of information, service providers should be aware of the readability of the written information, especially for families with lower levels of education and for families when English is not the primary language, who may be placed at a disadvantage if they are not able to access written information. Health literacy is quickly growing momentum as a key consideration in providing health information and services to patients and families so that they are able to make appropriate health decisions, navigate the healthcare system, and share information with service providers (Ratzan & Parker, 2000). Given research in the US suggests that approximately one-third of adults have basic or below basic health literacy (Kutner et al., 2006), service providers should also consider the importance of providing information in both written and verbal forms. Importantly, written information should abide by basic health literacy principles such as prioritizing ‘how to’ information for caregivers (Seligman et al., 2007) and emphasizing small practical steps (Centers for Disease Control and Prevention, 2009).
The qualitative nature of the analysis of comments provided by parents in Phase 1 and the interviews conducted with three families in Phase 2 increased understanding about the specific areas of concerns in decision-making that have implications for service providers. When the families had the opportunity to share in-depth information through interviews, they described feeling a need to make fast decisions about their child’s early intervention, and feeling dissatisfied with the information provided by hearing professionals relating to this decision. This is consistent with the findings described by Hyde et al. (2010), who reported that parents have felt pressure to choose an assistive technology (i.e., a cochlear implant) almost immediately after diagnosis, without information provided on the procedure, rehabilitation process or expected outcomes. It is important that the decision-making process is not rushed and parents should be aware that they can take the necessary time to make an informed decision (Duncan, 2009). Further, a small number of parents in this study also indicated that they received misinformation and a perceived lack of information from hearing professionals. Dissatisfaction with regards to service providers was also noted in a previous study by (Russ, et al., 2004) who found that some parents in Victoria, Australia felt that explanations provided by paediatric audiology services, hospitals, and audiologists regarding their child’s hearing loss were unclear, misleading, or incorrect. The information and advice provided by health professionals regarding the use of assistive technologies is an important consideration for parents who have a child newly diagnosed with hearing loss. Parents in the present study also indicated confusion surrounding why their child with profound hearing loss required hearing aids, when it was unlikely this would be sufficient to access speech sounds. This source of parent confusion was also noted in a study by (Archbold et al., 2002) who found that some parents felt conventional hearing aids provided little benefit to their child. Clearly, parents require detailed information and support regarding amplification technology, including the rationale for the use of hearing aids and cochlear implantation (Archbold, et al., 2002), and more effective and coordinated collaboration and communication among professionals to ensure parents receive clear and consistent messages.
Information provided by ENT surgeons appeared to influence parent decisions regarding their child’s early intervention. For instance, in the present qualitative study, one family was referred directly to an early intervention provider, with no other options discussed, while another family was provided with the contact details of three early intervention providers. The reported lack of information and influence towards certain service providers is consistent with previous research in this area. Eleweke and Rodda (2000) found that the contact and information received from medical or educational professionals heavily influenced a parent’s decision regarding their child’s early intervention provider. In the current study, some parents reported only receiving selective information. Given that the Joint Committee on Infant Hearing (2007) states that families should be made aware of all communication options and available hearing technologies, there is the potential that the information provided by health professionals could be perceived as being biased. In addition, Sorkin and Zwolan (2008) identified that parents who received little written information were significantly more likely to rate the information as biased towards one certain approach.
Thus, it is apparent, from both the current study and previous research in this area (Crowe et al., 2014a; Decker, et al., 2012; Eleweke & Rodda, 2000; Roberts et al., 2015), that information provided by health professionals is a key source of influence in the parental decision-making process, with the provision of written health information playing a particularly important role in this process. Interestingly, some parents in the Crowe et al. (2014a) study noted that “professionals presented them with information in a way that allowed them to make their own decision”, however, other parents responded that “their decision was strongly guided by a professional who told them what to do” (p. 8). These findings were also supported in the Roberts et al. (2015) study where some parents reported “feeling pushed by professionals who appeared to have their own biased agenda” (p.947). Given the significant role professional influence plays in this process, it is therefore imperative that audiologists, and other health professionals, provide parents with comprehensive and accuate information regarding all habilitation options (Bekker et al., 1999; Marteau et al., 2001), without any undue bias (Eleweke et al., 2008) thereby allowing parents to make an informed decision regarding their child’s early intervention (Moeller et al., 2013). When making an informed decision, parents must consider two important principles: (1) the decision should be a reflection of the individual’s values; and (2) the decision should be based on relevant and quality information.
As well as the need for adequate and accurate information, parents also need to be provided with appropriate emotional support during the potentially difficult time of diagnosis (Eleweke et al., 2008). Participants in both phases of the present study reported feeling overwhelmed at the time of diagnosis, with a range of emotions expressed that are typical of the feelings experienced by parents as they move through a cycle of grief (Kampfe, 1989; Kurtzer-White & Luterman, 2003). The importance of parent support in these early stages of diagnosis has been well documented (Eleweke, et al., 2008; Gilliver et al., 2013; Kampfe, 1989; Kurtzer-White & Luterman, 2003; Russ, et al., 2004). With this in mind, professionals must be trained in delivering information in an empathetic, open, and respectful manner, and must be prepared to take on a counselling role within their scope of practice (Joint Committee on Infant Hearing, 2013; Luterman & Kurtzer-White, 1999).
Luterman and Kurtzer-White (1999) also identified a need for parents to be able to contact other parents of children with hearing loss. Social networks provide parents with opportunities to share their experiences with other parents, provide support, and develop coping strategies (Eleweke, et al., 2008). Of note is that in the present study, only 6.1% of caregivers recalled receiving information from another parent or parent support group, therefore the importance of providing parents with information about parent to parent support groups is an important consideration. The Joint Committee on Infant Hearing (2013) has also advocated for the importance of family support, with guidelines developed and implemented, which encourage family-centred care. In Phase 1 of the current study, 79.4% of caregivers did not report receiving any information or support from a professional counsellor. This is because professional counselling after diagnosis is not an integral part of state-funded services in two of the three states from which the present cohort was drawn. The present results suggest that caregivers who did receive these services were satisfied with the information and/or support they received, lending support to the valuable role these services play. The addition of professional counselling services to services for families of children with hearing loss, along with structured parent support groups, is recommended as a means to further support parents during this emotional time as they navigate their way through the process of diagnosis and early intervention.
Overall, the provision of information and emotional/personal support for parents of children with hearing loss is consistent with a model of family-centred care (Sass-Lehrer, 2004). Interestingly, research also suggests that patient satisfaction, or “responsiveness” is uniquely predicted by a range of variables within the patient experience, such as autonomy, choice, communication, and prompt attention (Bleich, Özaltin, & Murray, 2009) which are also key determinants of family-centred care (Epley, Summers, & Turnbull, 2010). The acknowledgement of parents as key partners in decision-making, and a focus on strengthening the family’s competence, is vital for positive outcomes for child development (Sass-Lehrer, 2004). Parents of children with hearing loss have the right to access comprehensive information, in an environment that facilitates their acquisition of new information in a meaningful way (Arango, 2011). Importantly, professionals need to mutually discuss with each family the most beneficial method of providing information, strategies or resources at this potentially difficult time (Arango, 2011). Kessels (2003) highlighted that the information communicated by professionals can have profound implications on the client, but approximately 40 to 80% of medical information provided by health practitioners is forgotten immediately. Thus, clinicians must be aware that families are likely to require information to be provided multiple times. Furthermore, the information needs and dynamics of families may evolve over time (Arango, 2011). Clinicians adhering to family-centred care must provide appropriate levels of information and relevant information at these stages of the intervention process in order to meet the needs of the family.
The strengths of the current study are its population base, and its inclusion of both quantitative and qualitative data. The written survey of families of 445 children (>95% response rate) revealed that caregivers of children with hearing loss received personal/emotional support and information from a wide range of service providers. About 85% of respondents were satisfied with both the personal/emotional support they received, as well as the information provided to them after diagnosis of their child’s hearing loss. This response rate is very high, compared to that of other questionnaire surveys (typically ranging from 7% to 79% in surveys for adults, Shih & Fan, 2008). As the survey in this study was conducted on a population-based cohort, these results are generalizable to Australia. The findings suggest that the public health system met the needs of a large proportion of the population.
Detailed analysis of written and verbal comments from some caregivers, however, revealed that there were instances when families perceived that they received insufficient support at diagnosis, and experienced delays in accessing services. In the qualitative study on 5 parents from 3 families, families specifically discussed the emotional reaction to their child’s diagnosis, and noted that there was limited information and support available to them during this time. Families also discussed the perceived pressure to make decisions quickly regarding their choice of early intervention provider for their child, and reported confusion regarding the role of service providers during the diagnostic period.
Limitations and Future Directions
The qualitative nature of Phase 2 has provided extensive narrative data that increased understanding about the specific experiences of three families. Although the information was provided by only 5 participants who could not have captured the full range of variability likely to be experienced by parents of children with hearing loss in the early diagnostic period, their comments are broadly consistent with reports in the literature. Future explorations of parental experiences and decision-making will require qualitative research with a larger number of families. Further, the data were retrospective in nature, with participants in this study reflecting on their child’s diagnosis up to six years after the event, and therefore, there could have been a recollection bias. However, this study shows how interview data can expand on results from a written survey to increase understanding about parents’ perspectives. Future research including a focus on parents currently on their journey of diagnosis and decision-making in the context of current services would provide a beneficial comparison to this study. Further understanding of parents needs at different phases of their child’s habilitation would also be beneficial, including the stage of initial diagnosis right through to transition to the school environment.
Conclusion
The current study contributes to the growing body of literature highlighting the perspective of parents who have had a child diagnosed with hearing loss. Results highlight the importance of providing parents with accurate and unbiased information in order to allow parents to make an informed decision for their child. At all times, professionals must consider the emotional needs of parents during the potentially overwhelming time after diagnosis of hearing loss in newborns. The role of family-centred care in this setting is essential, so that the individual needs of each family, with regards to information provision and emotional support, are met collaboratively.
Acknowledgments
We gratefully thank all the families who participated in this study. This work was partly supported by the National Institute on Deafness and Other Communication Disorders (Award Number R01DC008080). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute on Deafness and Other Communication Disorders or the National Institutes of Health.
The project was also partly supported by the Commonwealth of Australia through the Office of Hearing Services. We acknowledge the financial support of the HEARing CRC, established and supported under the Cooperative Research Centres Program of the Australian Government. We also thank Vicky Zhang for her assistance in preparing Tables 1 and 2.
Acronyms
- ENT
Ear, Nose, and Throat Surgeon
- FCC
Family-Centred Care
- LOCHI
Longitudinal Outcomes of Children with Hearing Impairment
References
- Arango P. Family-centered care. Acad Pediatr. 2011;11(2):97. doi: 10.1016/j.acap.2010.12.004. [DOI] [PubMed] [Google Scholar]
- Archbold SM, Lutman ME, Gregory S, O’Neill C, Nikolopoulos TP. Parents and their deaf child: Their perceptions three years after cochlear implantation. Deaf Educ Int. 2002;4(1):12–40. doi: 10.1002/dei.114. [DOI] [Google Scholar]
- Australian Hearing. What support does Australian Hearing provide hearing impaired children? 2014 Retrieved from https://www.hearing.com.au/milestone/what-support-does-australian-hearing-provide-hearing-impaired-children/
- Babbie ER. The practice of social research. Belmont, California: Wadsworth Cengage; 2010. [Google Scholar]
- Bekker H, Thornton JG, Airey CM, et al. Informed decision making: An annotated biography and systematic review. Health Technology Assessment. 1999;3(1):39–32. [PubMed] [Google Scholar]
- Bleich SN, Özaltin E, Murray CJL. How does satisfaction with the health-care system relate to patient experience? Bulletin of the World Health Organization. 2009;87(4):271–278. doi: 10.2471/BLT.07.050401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101. doi: 10.1191/1478088706qp063oa. [DOI] [Google Scholar]
- Centers for Disease Control and Prevention. Simply Put: A guide for creating easy-to-understand materials. 2009 Retrieved from www.cdc.gov/healthmarketing/pdf/Simply_Put_082010.pdf.
- Ching TYC, Leigh G, Dillon H. Introduction to the longitudinal outcomes of children with hearing impairment (LOCHI) study: Background, design, sample characteristics. Int J Audiol. 2013;52:54–59. doi: 10.3109/14992027.2013.866342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. Thousand Oaks: SAGE Publications; 2011. [Google Scholar]
- Crowe K, Fordham L, McLeod S, Ching TYC. ‘Part of our world’: Influences on caregiver decisions about communication choices for children with hearing loss. Deaf Educ Int. 2014a;16(2):61–85. doi: 10.1179/1557069x13y.0000000026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe K, McLeod S, McKinnon DH, Ching TYC, Nippold M, Hayes L. Speech, sign, or multilingualism for children with hearing loss: Quantitative insights into caregivers’ decision making. Lang Speech Hear Ser. 2014b;45(3):234–247. doi: 10.1044/2014. [DOI] [PubMed] [Google Scholar]
- Decker KB, Vallotton CD, Johnson HA. Parents’ communication decision for children with hearing loss: Sources of information and influence. Am Ann Deaf. 2012;157(4):326–339. doi: 10.1353/aad.2012.1631. [DOI] [PubMed] [Google Scholar]
- DiCicco-Bloom B, Crabtree BF. The qualitative research interview. Med Educ. 2006;40(4):314–321. doi: 10.1111/j.1365-2929.2006.02418.x. [DOI] [PubMed] [Google Scholar]
- Duncan J. Parental readiness for cochlear implant decision-making. Cochlear Implants International. 2009;10(Suppl 1 (Supplement-1)):38–42. doi: 10.1179/cim.2009.10.Supplement-1.38. [DOI] [PubMed] [Google Scholar]
- Eleweke CJ, Gilbert S, Bays D, Austin E. Information about support services for families of young children with hearing loss: A review of some useful outcomes and challenges. Deaf Educ Int. 2008;10(4):190–212. doi: 10.1002/dei.247. [DOI] [Google Scholar]
- Eleweke CJ, Rodda M. Factors contributing to parents’ selection of a communication mode to use with their deaf children. Am Ann Deaf. 2000;145(4):375–383. doi: 10.1353/aad.2012.0087. [DOI] [PubMed] [Google Scholar]
- Epley P, Summers JA, Turnbull A. Characteristics and trends in family-centred conceptualizations. Journal of Family Social Work. 2010;13(3):269–285. [Google Scholar]
- Erbasi E, Scarinci N, Hickson L, Ching TYC. Parental Involvement in the Care and Intervention of Children with Hearing Loss. International Journal of Audiology. doi: 10.1080/14992027.2016.1220679. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzpatrick E, Angus D, Durieux-Smith A, Graham ID, Coyle D. Parents’ needs following identification of childhood hearing loss. Am J Audiol. 2008;17(1):38–49. doi: 10.1044/1059-0889(2008/005). [DOI] [PubMed] [Google Scholar]
- Gilliver M, Ching TYC, Sjahalam-King J. When expectation meets experience: Parents’ recollections of and experiences with a child diagnosed with hearing loss soon after birth. Int J Audiol. 2013;52(S2):S10–S16. doi: 10.3109/14992027.2013.825051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gravel JS, O’Gara J. Communication options for children with hearing loss. Ment Retard Dev D R. 2003;9(4):243–251. doi: 10.1002/mrdd.10087. [DOI] [PubMed] [Google Scholar]
- Gummesson E. Qualitative methods in management research. Lund, Norway: Studentlitteratur, Chartwell-Bratt; 1988. [Google Scholar]
- Hsieh H, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Hyde M, Punch R, Komesaroff L. Coming to a decision about cochlear implantation: Parents making choices for their deaf children. J Deaf Stud Deaf Educ. 2010;15(2):162. doi: 10.1093/deafed/enq004. [DOI] [PubMed] [Google Scholar]
- Joint Committee on Infant Hearing. Year 2007 position statement: Principles and guidelines for early hearing detection and intervention programs. Pediatr. 2007;120(4):898–921. doi: 10.1542/peds.2007-2333. [DOI] [PubMed] [Google Scholar]
- Joint Committee on Infant Hearing. Supplement to the JCIH 2007 position statement: principles and guidelines for early intervention after confirmation that a child is deaf or hard of hearing. Pediatr. 2013;131(4):e1324. doi: 10.1542/peds.2013-0008. [DOI] [PubMed] [Google Scholar]
- Kampfe CM. Parental reaction to a child’s hearing impairment. Am Ann Deaf. 1989;134(4):255–259. doi: 10.1353/aad.2012.0682. [DOI] [PubMed] [Google Scholar]
- Kessels RPC. Patients’ memory for medical information. JRSM. 2003;96(5):219–222. doi: 10.1258/jrsm.96.5.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluwin TN, Stewart DA. Cochlear implants for younger children: A preliminary description of the parental decision process and outcomes. Am Ann Deaf. 2000;145(1):26–32. doi: 10.1353/aad.2012.0247. [DOI] [PubMed] [Google Scholar]
- Kurtzer-White E, Luterman D. Families and children with hearing loss: Grief and coping. Ment Retard Dev D. 2003;9(4):232–235. doi: 10.1002/mrdd.10085. [DOI] [PubMed] [Google Scholar]
- Kutner M, Greenberg E, Jin Y, Paulsen C. The health literacy of America’s adults: Results from the 2003 National Assessment of Adult Literacy. Washington DC: US Department of Education; 2006. (NCES 2006-483). [Google Scholar]
- Li Y, Bain L, Steinberg AG. Parental decision making and the choice of communication modality for the child who is deaf. Arch Pediatr Adolesc Med. 2003;157:162–168. doi: 10.1001/archpedi.157.2.162. [DOI] [PubMed] [Google Scholar]
- Luterman D, Kurtzer-White E. Identifying hearing loss: Parents’ needs. Am J Audiol. 1999;8:13–18. doi: 10.1044/1059-0889(1999/006). [DOI] [PubMed] [Google Scholar]
- Marteau TM, Dormandy E, Michie S. A measure of informed choice. Health Expectations. 2001;4:99–108. doi: 10.1046/j.1369-6513.2001.00140.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matthijs L, Loots G, Mouvet K, Van herreweghe M, Hardonk S, Van hove G, Leigh G. First information parents receive after UNHS detection of their baby’s hearing loss. J Deaf Stud Deaf Educ. 2012;17(4):387–401. doi: 10.1093/deafed/ens020. [DOI] [PubMed] [Google Scholar]
- Meyer C. A case in case study methodology. Field Methods. 2001;13(4):329–352. doi: 10.1177/1525822X0101300402. [DOI] [Google Scholar]
- Moeller MP, Carr G, Seaver L, Stredler-Brown A, Holzinger D. Best practices in family-centered early intervention for children who are deaf or hard of hearing: An international consensus statement. J Deaf Stud Deaf Educ. 2013;18:429–445. doi: 10.1093/deafed/ent034. [DOI] [PubMed] [Google Scholar]
- Patton MQ. Qualitative research and evaluation methods. 3rd. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- Ratzan SC, Parker RM. Introduction. In: Selden CR, Zorn M, Ratzan SC, Parker RM, editors. National Library of Medicine current bibliographies in medicine: Health literacy. Bethesda, MD: National Institutes of Health; 2000. (NLM Pub. No. CBM 2000-1). [Google Scholar]
- Rice GB, Lenihan S. Early intervention in auditory/oral deaf education: Parent and professional perspectives. Volta Rev. 2005;105(1):73–96. [Google Scholar]
- Roberts RM, Sands F, Gannoni G, Marciano T. Perceptions of the support that mothers and fathers of children with cochlear implants receive in South Australia: A qualitative study. International Journal of Audiology. 2015;54(12):942–950. doi: 10.3109/14992027.2015.1060641. [DOI] [PubMed] [Google Scholar]
- Russ SA, Kuo AA, Poulakis Z, Barker M, Rickards F, Saunders K, Oberklaid F. Qualitative analysis of parents’ experience with early detection of hearing loss. Arch Dis Child. 2004;89(4):353–358. doi: 10.1136/adc.2002.024125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sass-Lehrer M. Early detection of hearing loss: Maintaining a family-centered perspective. Semin Hear. 2004;25(04):295–307. doi: 10.1055/s-2004-836132. [DOI] [Google Scholar]
- Seligman HK, Wallace AS, DeWalt DA, Schillinger D, Arnold CL, Shilliday BB, Davis TC. Facilitating behavior change with low-literacy patient education materials. Am J Health Behav. 2007;31(Suppl 1):S69–S78. doi: 10.5555/ajhb.2007.31.supp.S69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Senghas RJ, Monaghan L. Signs of their times: Deaf communities and the culture of language. Annu Rev Anthropol. 2002;31(1):69–97. doi: 10.1146/annurev.anthro.31.020402.101302. [DOI] [Google Scholar]
- Shih TH, Fan X. Comparing response rates from web and mail surveys: A meta-analysis. Field methods. 2008;20(3):249–271. [Google Scholar]
- Simons H. Case study research in practice. London; Los Angeles: SAGE; 2009. [Google Scholar]
- Sorkin D, Zwolan T. Parental perspectives regarding early intervention and its role in cochlear implantation in children. Otol Neurotol. 2008;29:137–142. doi: 10.1097/mao.0b013e3181616c88. [DOI] [PubMed] [Google Scholar]
- Steinberg A, Bain L, Li Y, Delgado G, Ruperto V. Decisions Hispanic Families Make After the Identification of Deafness. J Deaf Stud Deaf Educ. 2003;8(3):291–314. doi: 10.1093/deafed/eng01. [DOI] [PubMed] [Google Scholar]
- Wechsler D, Naglieri JA. Wechsler Nonverbal Scale of Ability: Technical and interpretive manual. San Antonio, TX: The Psychological Corporation; 2006. [Google Scholar]


