Abstract
Recent studies have delineated cancer type-specific roles of histone 3 lysine 27 (H3K27) demethylase KDM6B/JMJD3 depending on its H3K27 demethylase activity. Here we show that KDM6B is expressed in multiple myeloma (MM); and that shRNA-mediated knockdown and CRISPR-mediated knockout of KDM6B abrogate MM cell growth and survival. TNFα or bone marrow stromal cell culture supernatants induce KDM6B, which is blocked by IKKβ inhibitor MLN120B, suggesting KDM6B is regulated by NF-κB signaling in MM cells. RNA-sequencing and subsequent ChIP-qPCR analyses reveal that KDM6B is recruited to the loci of genes encoding components of MAPK signaling pathway including ELK1 and FOS, and upregulates these genes expression without affecting H3K27 methylation level. Overexpression of catalytically-inactive KDM6B activates expression of MAPK pathway-related genes, confirming its function independent of demethylase activity. We further demonstrate that downstream targets of KDM6B, ELK1 and FOS, confer MM cell growth. Our study therefore delineates KDM6B function that links NF-κB and MAPK signaling pathway mediating MM cell growth and survival, and validates KDM6B as a novel therapeutic target in MM.
INTRODUCTION
Multiple myeloma (MM) is a plasma cell malignancy that proliferates in the bone marrow.1, 2 Although novel agents including proteasome inhibitors and immunomodulatory drugs (IMiDs) have remarkably improved MM patient survival, MM remains incurable. Hence, there is a need to decipher the pathogenesis of MM to identify novel therapeutic targets for MM. Recent studies using whole-genome and whole-exome sequencing have identified driver mutations in MM, and revealed relevant pathways in myelomagenesis.3 For example, MAPK pathway genes including KRAS, NRAS, BRAF are mutated in about 40% of patients.4–6 NF-κB pathway molecules such as TRAF3, CYLD, LTB are also mutated in about 20% of patients.4–6 These results highlight the roles of these two signaling pathways in MM. These pathways are also known to be activated by extrinsic factors in the bone marrow microenvironment.1, 2 For example, bone marrow stromal cells (BMSCs) produce extrinsic ligands including IL6, IGF1, TNFα, APRIL and BAFF, further activating MAPK and NF-κB pathways. Thus, MM cells are largely dependent on these two major pathways.
Lysine demethylase 6B (KDM6B, also known as JMJD3) is a Jumonji C-domain-containing histone demethylase which removes histone 3 lysine 27 (H3K27) di- and tri-methylation (me2/me3) through iron and α-ketoglutarate-dependent oxidative reactions.7–9 KDM6B is upregulated via NF-κB binding to its promoter region by inflammatory stimuli in macrophages.7 KDM6B contributes not only to inflammatory response, but also to various biological processes including stress-induced senescence, development and differentiation.7–13 Importantly, recent studies have also shown that KDM6B is implicated in the pathogenesis of several cancers in a context-dependent fashion;14–19 however, to date the biological function of KDM6B in MM remains to be determined.
Here we investigate the biological impact of KDM6B in MM. We show that KDM6B is highly expressed in MM. Depletion of KDM6B leads to MM cell death. KDM6B is activated by NF-κB signaling in MM cells, consistent with previous reports in other cell types.7, 14 Importantly, we demonstrate that KDM6B, in a demethylase-independent fashion, upregulates MAPK signaling molecules mediating MM cell growth and survival. Our data therefore delineate the biologic sequelae of KDM6B, and validate KDM6B as a novel therapeutic target in MM.
MATERIALS AND METHODS
Reagents and antibodies
Reagents used in this study are described in Supplementary Materials and Methods. Antibodies used in this study are listed in Supplementary Table 1.
Cell lines
Human MM cell lines MM.1S, RPMI 8226, KMM-1, NCI-H929, KMS-11 and KMS-27 were stocked in our laboratory, and the identity of these cell lines was confirmed before use by STR profiling (GenePrint®10 System, Promega, Madison, WI, USA). Human MM cell lines MOLP-8 and KMS-20 were recently obtained from DSMZ (Braunschweig, Germany) and JCRB Cell Bank (Osaka, Japan), respectively. Human embryonic kidney cell line 293T was obtained from ATCC (Manassas, VA, USA). Cell lines were regularly tested to rule out mycoplasma contamination.
Primary MM cell, BMSC, and peripheral blood mononuclear cell (PBMNC) samples
Bone marrow or peripheral blood samples were obtained from MM patients or healthy volunteers with informed consent and approval of the Institutional Review Board of the Dana-Farber Cancer Institute. After separating mononuclear cells from patients’ bone marrow by Ficoll-Paque PLUS (GE Healthcare, Little Chalfont, UK), MM cells were purified by CD138-positive selection using anti-CD138 magnetic activated cell separation microbeads (Miltenyi Biotec, Bergisch Gladbach, Germany). Long-term MM patient BMSCs were established and maintained by culturing CD138-negative bone marrow mononuclear cells in DMEM containing 100U/m1 penicillin and 100μg/ml streptomycin, supplemented with 15% (v/v) fetal bovine serum (FBS). PBMNCs were isolated from normal donors’ peripheral blood using Ficoll-Paque centrifugation.
RNA-sequencing (RNA-seq) analysis
Detailed method is found in Supplementary Materials and Methods. RNA-seq data are deposited at https://www.ncbi.nlm.nih.gov/geo/ under accession number GSE93395.
Statistical analysis
No statistical method was used to predetermine sample size. Data are presented as mean ± s.d. as indicated in each figure legend. Comparison between two groups assuming normal distribution was made with two-tailed Student’s t-test, and Welch’s correction was applied when variances were unequal, which was determined by F-test. A value of P < 0.05 was considered significant.
Additional methods are described in Supplementary Materials and Methods.
RESULTS
KDM6B confers MM cell growth and survival
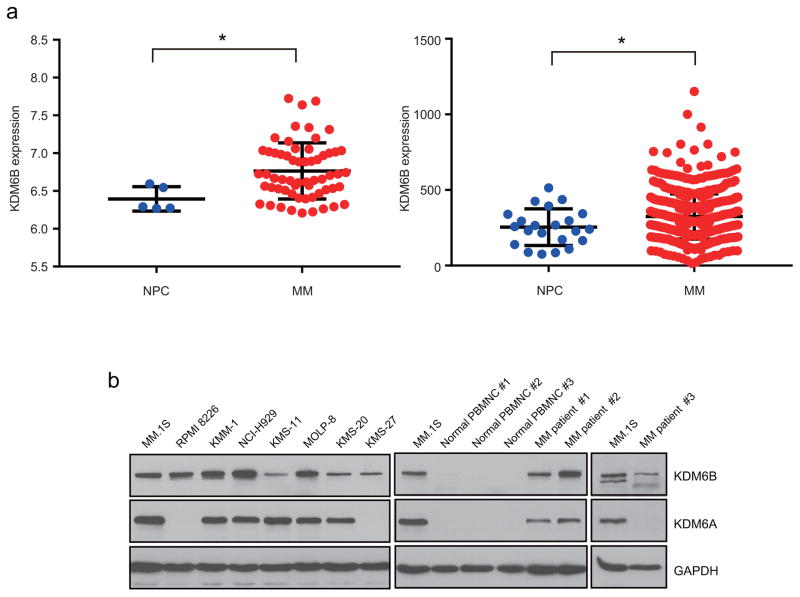
We first assessed KDM6B expression in MM patient samples using publicly available data sets. Expression of KDM6B was significantly elevated in MM patient samples compared with healthy donor plasma cells (Figure 1a), suggesting the role of KDM6B in the pathogenesis of MM. KDM6B protein expression was also verified by immunoblotting in 8 MM cell lines and 3 primary MM samples, while KDM6B protein was not detected in 3 healthy volunteer derived-PBMNCs (Figure 1b). We therefore explored the biologic role of KDM6B in MM cells.
Figure 1.
KDM6B expression in MM
(a) KDM6B expression was analyzed in normal plasma cells (NPC) and MM patient samples (MM) using publicly available data sets (GSE16558, left panel; combining data from University of Arkansas for Medical Sciences (GSE5900 and GSE2658), right panel). *P <0.05.
(b) Whole cell lysates were extracted from MM cell lines, MM patient samples, and normal peripheral blood mononuclear cells (PBMNC), and subjected to immunoblot analysis with the indicated antibodies.
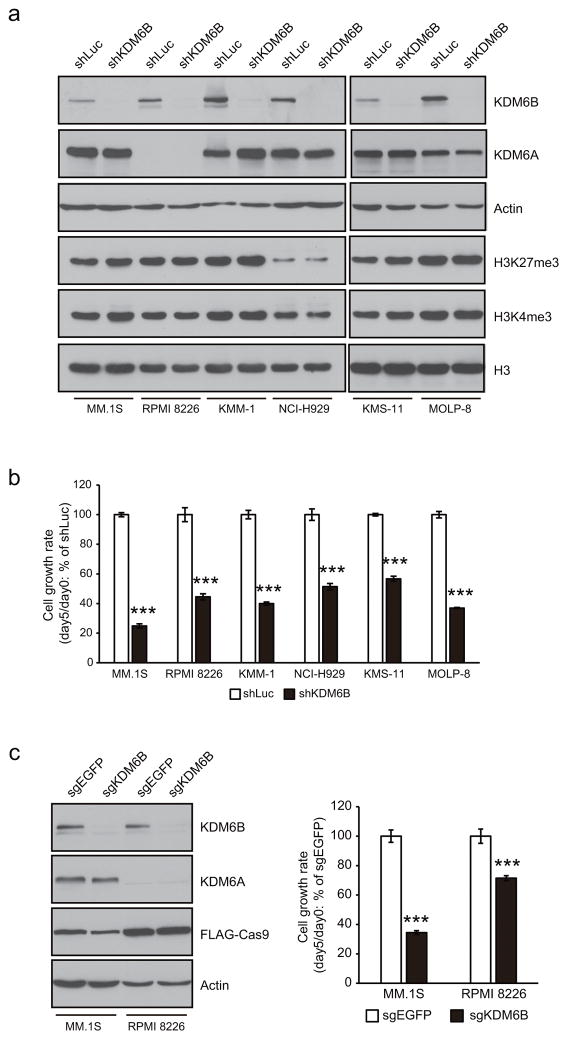
We transduced short hairpin (sh) RNA against KDM6B (shKDM6B) or control shRNA against luciferase (shLuc) into MM cell lines. Depletion of KDM6B protein was confirmed in shKDM6B-transduced cells (Figure 2a). In contrast, transduction of shKDM6B had little effect on closely related KDM6A expression, suggesting specific knockdown of KDM6B by the hairpin (Figure 2a). Although KDM6B is an H3K27 demethylase,7–9 we observed that global H3K27me3 level was minimally affected after KDM6B knockdown (Figure 2a). Of note, knockdown of KDM6B reduced growth of 6 MM cell lines tested (Figure 2b). Cell growth was inhibited even in the presence of MM patient-derived BMSC conditioned medium (BMSC CM) after knockdown of KDM6B (Supplementary Figure 1). To confirm the result of shRNA knockdown experiments, we introduced single guide (sg) RNA targeting KDM6B into MM.1S and RPMI 8226 cell lines stably expressing Cas9. The reduction of KDM6B protein level was validated by immunoblot (Figure 2c, left panel). Consistent with shRNA results, CRISPR-mediated KDM6B knockout inhibited growth of MM.1S and RPMI 8226 cells (Figure 2c, right panel). Conversely, overexpression of KDM6B significantly increased growth of MM.1S cells (Supplementary Figure 2), further confirming the role of KDM6B in MM cell growth.
Figure 2.
Silencing of KDM6B reduces MM cell growth.
(a,b) MM cell lines were transduced with shRNA targeting KDM6B (shKDM6B) or control shRNA targeting luciferase (shLuc). Three days post infection (two days post puromycin selection) is designated as day 0. (a) On day 0, whole cell lysates were extracted and subjected to immunoblot analysis with the indicated antibodies. (b) Cell viability was determined by MTT assay on days 0 and 5. The cell growth rate (day 5/day 0) relative to shLuc is shown.
(c) MM.1S and RPMI 8226 cells expressing Cas9 were transduced with sgRNA against KDM6B (sgKDM6B) or control sgRNA against EGFP (sgEGFP). Three days post infection is designated as day 0. On day 0, whole cell lysates were extracted and subjected to immunoblot analysis with the indicated antibodies (left panel). FLAG-tagged Cas9 was detected by anti-FLAG. Cell growth rate (day 5/day 0) relative to sgEGFP is shown (right panel).
(b,c) Data represent mean ± s.d. of quadruplicate cultures. ***P < 0.001 compared with control.
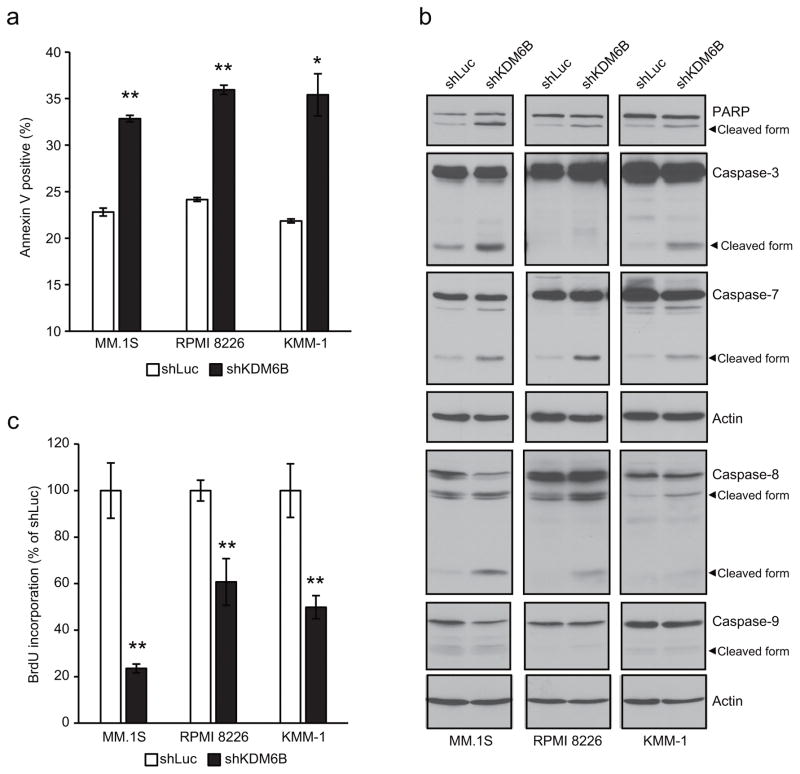
To investigate the underlying mechanism of cell growth inhibition in KDM6B-knockdown cells, we quantified apoptotic cells by flow cytometry using Annexin V staining. As shown in Figure 3a, percentages of apoptotic cells were significantly elevated after KDM6B knockdown in MM cell lines. Furthermore, cleaved forms of caspase-3, caspase-7 and poly (ADP-ribose) polymerase (PARP) (markers of the execution apoptosis pathway) were increased after KDM6B knockdown, except for lack of cleavage of caspase-3 in RPMI 8226 cells, suggesting that KDM6B knockdown-induced apoptosis is dependent on caspase-7 in this cell line (Figure 3b). We further asked whether the intrinsic or extrinsic pathway is involved in the apoptosis induced by KDM6B knockdown. Immunoblot analyses showed increased cleavage of caspase-8 in KDM6B-knockdown cells with little cleavage of caspase-9, indicating involvement of the extrinsic apoptosis pathway (Figure 3b). Consistent with this finding, caspase-8 inhibitor Z-IETD-FMK partially blocked KDM6B knockdown-induced cell growth inhibition in MM.1S cells, whereas caspase-9 inhibitor Z-LEHD-FMK did not; rather it enhanced cell death, similar to the previous observation in B-lineage cells (Supplementary Figure 3).20 We next examined the effect of KDM6B knockdown on cell proliferation. As shown in Figure 3c, BrdU incorporation was significantly decreased after silencing of KDM6B in MM cell lines, while cell cycle profile was minimally altered (Supplementary Figure 4). Taken together, these results indicate that knockdown of KDM6B induces apoptosis and reduces cell proliferation, thereby impairing MM cell growth.
Figure 3.
Knockdown of KDM6B induces apoptosis and reduces cell proliferation in MM cells.
(a-c) MM.1S, RPMI 8226 and KMM-1 cells were transduced with shKDM6B or shLuc. (a) After 3 days (MM.1S) or 5 days (RRPMI 8226 and KMM-1) of infection, cells were analyzed for apoptosis by measuring annexin V-positive cells using the flow cytometer. Data represent mean ± s.d. of duplicate measurements. *P <0.05, **P < 0.01 compared with shLuc. (b) After 3 days (MM.1S) or 5 days (RRPMI 8226 and KMM-1) of infection, whole cell lysates were extracted and subjected to immunoblot analysis with the indicated antibodies. Actin served as the loading control for each membrane. (c) After 3 days of infection, the same number of viable cells were seeded and cultured for another 5 days. BrdU incorporation was then determined by BrdU assay. Data represent mean ± s.d. of triplicate cultures. **P < 0.01 compared with shLuc.
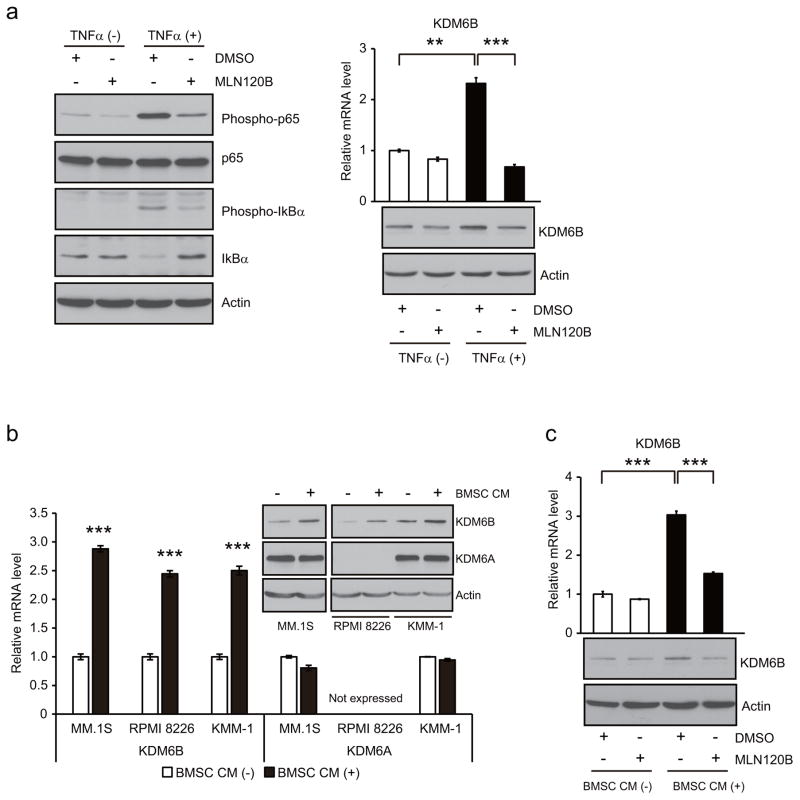
KDM6B is upregulated by NF-κB pathway in MM
NF-κB pathway plays an essential role in the survival of MM.21, 22 Previous studies have shown that NF-κB regulates KDM6B expression in some cell types.7, 14 We therefore hypothesized that KDM6B, as a downstream target of NF-κB, may mediate MM cell growth. To that end, we examined whether KDM6B in MM cells is also regulated by NF-κB. Activation of NF-κB pathway by TNFα, evidenced by increased phospho-IκBα, resulting IκBα protein degradation, as well as increased phospho-p65 (Figure 4a, left panel), induced KDM6B (Figure 4a, right panel and Supplementary Figure 5a), but not KDM6A (Supplementary Figure 5a) expression in MM.1S cells. This KDM6B induction was completely blocked by IκB kinase (IKK) β inhibitor MLN120B (Figure 4a, right panel), indicating that KDM6B expression is induced by NF-κB in MM cells. BMSCs are known to activate NF-κB pathway in MM cells through cytokines such as TNFα, APRIL and BAFF.1, 2 Therefore, we next examined whether BMSCs induce KDM6B expression in MM cells. As shown in Figure 4b, MM patient-derived BMSC CM upregulated KDM6B expression in MM.1S, RPMI 8226 and KMM-1 cells, but did not alter KDM6A expression. We confirmed that KDM6B expression was also induced by additional 4 MM patients’ BMSC CMs in MM.1S cells (Supplementary Figure 5b). Similar to TNFα stimulation, BMSC CM-mediated KDM6B induction was significantly decreased in the presence of MLN120B (Figure 4c), suggesting that KDM6B is induced by BMSCs, at least in part, via NF-κB signaling pathway in MM cells.
Figure 4.
KDM6B is upregulated by NF-κB signaling in MM.
(a) MM.1S cells were incubated with or without 30 ng/ml of TNFα and 20 μM of MLN120B or DMSO. After 5 min of treatment, whole cell lysates were extracted and subjected to immunoblot analysis with the indicated antibodies (left panel). After 2 h of treatment, total RNA and whole cell lysates were extracted and subjected to quantitative real time PCR and immunoblot analysis (right panel).
(b) MM cell lines were treated with conditioned medium from MM patient-derived bone marrow stromal cells (BMSC CM) or control culture medium for 2h.
(c) MM.1S cells were cultured with or without 20 μM of MLN120B in the presence of BMSC CM or control medium for 2h.
(a-c) Data represent the amount of mRNA relative to control. Error bars indicate s.d. of triplicate measurements. **P < 0.01, ***P < 0.001 compared with control.
We next asked whether KDM6B mediates MM cell growth under NF-κB pathway. Endogenous KDM6B expression was significantly reduced after 72 h treatment with MLN120B (Supplementary Figure 6a), associated with growth inhibition in MM.1S cells (Supplementary Figure 6b). The ectopic expression of KDM6B partially rescued MM.1S cells from this growth inhibition (Supplementary Figure 6b), suggesting KDM6B is at least one of the downstream effectors of NF-κB pathway in MM. The limited rescue effect of the ectopic KDM6B expression also implies the existence of other important effectors of NF-κB pathway in MM.
KDM6B regulates expression of MAPK pathway-related genes in MM
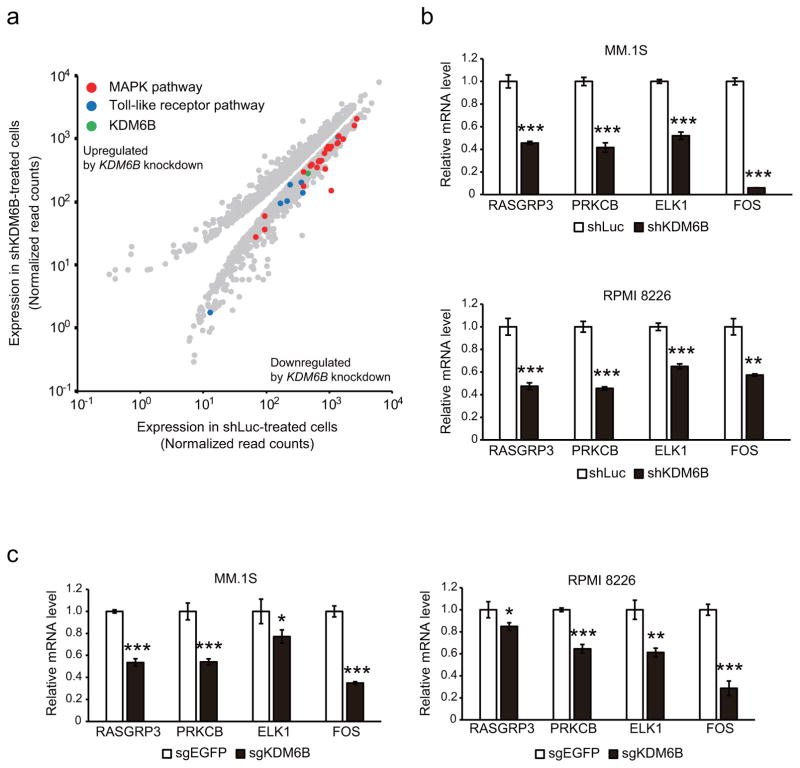
To reveal the downstream targets of KDM6B in MM, we next performed differential gene expression analysis using RNA-seq after knockdown of KDM6B in MM.1S cells (Supplementary Table 5). Pathway analysis using DAVID Bioinformatics Resources23, 24 revealed that Toll-like receptor signaling pathway genes were significantly downregulated after KDM6B knockdown (P = 0.01 at KEGG_PATHWAY, P = 0.0079 at BIOCARTA) (Figure 5a), consistent with a previous observation that KDM6B participates in the inflammatory transcriptional response.25 Interestingly, genes related to MAPK signaling cascade, a major growth and survival pathway in MM, were also significantly downregulated after KDM6B knockdown (P = 0.0029 at KEGG_PATHWAY, P = 0.0013 at BIOCARTA) (Figure 5a). Validation by quantitative real time PCR showed that knockdown of KDM6B significantly reduced expression of MAPK pathway-related genes such as RASGRP3, PRKCB, ELK1 and FOS in 6 MM cell lines (Figure 5b and Supplementary Figure 7a). We also observed reduced protein expression of ELK1 and FOS after KDM6B knockdown in these MM cell lines (Supplementary Figure 7b). CRISPR-mediated KDM6B knockout also demonstrated that depletion of KDM6B decreased expression of RASGRP3, PRKCB, ELK1 and FOS (Figure 5c). Conversely, overexpression of KDM6B increased expression of 3 of these MAPK pathway-related genes, but not ELK1 expression, suggesting that constitutive ELK1 expression is maintained at the maximum level by endogenous level of KDM6B (Supplementary Figure 8).
Figure 5.
Silencing of KDM6B downregulates MAPK pathway-related genes in MM.
(a) RNA-seq was carried out with MM.1S cells treated with shKDM6B or shLuc. Scatter plot shows differentially expressed transcripts selected based on > 20.3 fold-change with adjusted P < 0.05.
(b,c) Total RNA was isolated from MM.1S and RPMI 8226 cells transduced with shKDM6B or shLuc (b), or sgKDM6B or sgEGFP (c). Expression of 4 MAPK pathway-related genes (RASGRP3, PRKCB, ELK1 and FOS) was then evaluated by quantitative PCR. Expression of each gene relative to control is shown as mean ± s.d. of triplicate measurements. *P <0.05, **P < 0.01, ***P < 0.001 compared with control.
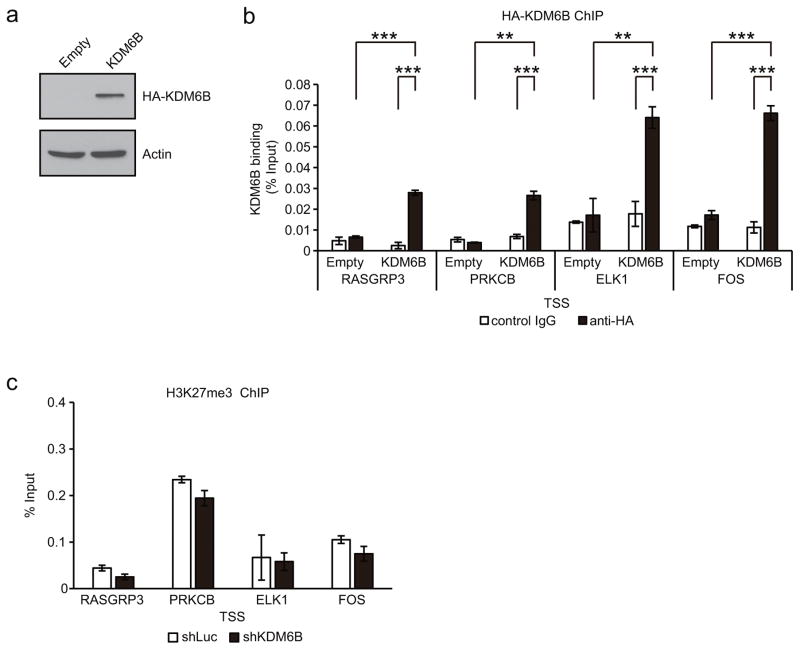
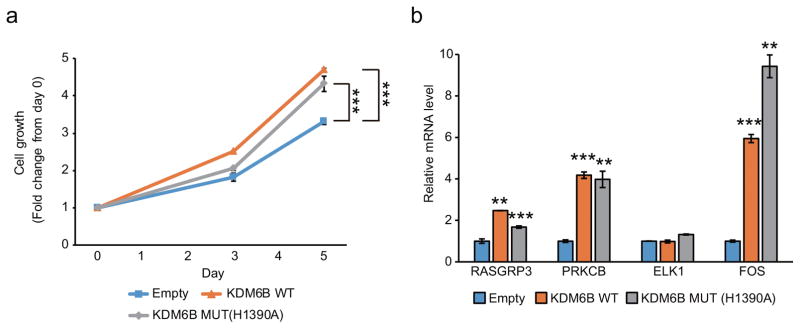
We next tested whether KDM6B is directly recruited to the loci of MAPK pathway-related genes. Since chromatin immunoprecipitation (ChIP)-grade KDM6B antibody is unavailable, we generated HA-tagged KDM6B (HA-KDM6B) stably expressing MM.1S cells for ChIP assays (Figure 6a). Fragments of cross-linked chromatin were immunoprecipitated with anti-HA antibody, followed by quantitative PCR. Empty vector-transduced cells were used as a negative control. As shown in Figure 6b, ChIP signals were enriched at the transcriptional start sites of RASGRP3, PRKCB, ELK1 and FOS genes in HA-KDM6B expressing cells, but not in empty vector-transduced cells, indicating that KDM6B binds to the transcriptional start sites of these genes. We next evaluated H3K27me3 level at these regions after knockdown of KDM6B, since KDM6B is an H3K27 demethylase. Unexpectedly, H3K27me3 level was not increased at these sites in KDM6B-knockdown MM.1S cells compared with control cells (Figure 6c). Previous studies have reported the KDM6B functions that are independent of demethylase activity;25–27 hence, we hypothesized that KDM6B may regulate MAPK pathway genes via an enzymatically-independent function in MM cells. To test this possibility, we expressed demethylase-dead KDM6B (H1390A) cDNA in MM.1S cells. Expression of mutant KDM6B enhanced growth of MM.1S cells (Figure 7a), and induced expression of RASGRP3, PRKCB and FOS similar to wild-type KDM6B (Figure 7b), indicating that KDM6B promotes MM cell growth and regulates MAPK pathway genes independent of its catalytic function. Consistent with these findings, GSK-J4, H3K27 demethylases inhibitor which blocks KDM6B enzymatic activity but induces KDM6B expression (Supplementary Figure 9), upregulates expression of these MAPK pathway molecules (Supplementary Figure 9). Taken together, these results indicate that KDM6B regulates MAPK pathway molecules in a demethylase-independent manner in MM cells.
Figure 6.
KDM6B is recruited to the transcriptional start sites of MAPK pathway-related genes, but does not affect H3K27me3 level at these sites.
(a) Whole cell lysates from MM.1S cells stably expressing HA-tagged KDM6B were subjected to immunoblot analysis with anti-HA.
(b) ChIP assay using anti-HA antibody was performed with MM.1S cells stably expressing HA-tagged KDM6B.
(c) H3K27me3 level was assessed after knockdown of KDM6B in MM.1S cells.
(b,c) Percent recovery over the input was determined by quantitative PCR. TSS; transcriptional start site. Data represent mean ± s.d. of triplicate measurements. **P < 0.01, ***P < 0.001 compared with control.
Figure 7.
KDM6B regulates MAPK pathway-related genes in a demethylase-independent manner.
(a) MM.1S cells stably expressing wild-type (WT) or catalytically-dead mutant (MUT) KDM6B cDNA, or control cells transduced with empty vector were cultured for indicated intervals, and analyzed for growth by MTT assay. Data represent mean ± s.d. of quadruplicate cultures.
(b) Total RNA was isolated from MM.1S cells stably expressing WT or MUT KDM6B, or control cells. Expression of each gene relative to control is shown as mean ± s.d. of triplicate measurements.
(a,b) **P < 0.01, ***P < 0.001 compared with control.
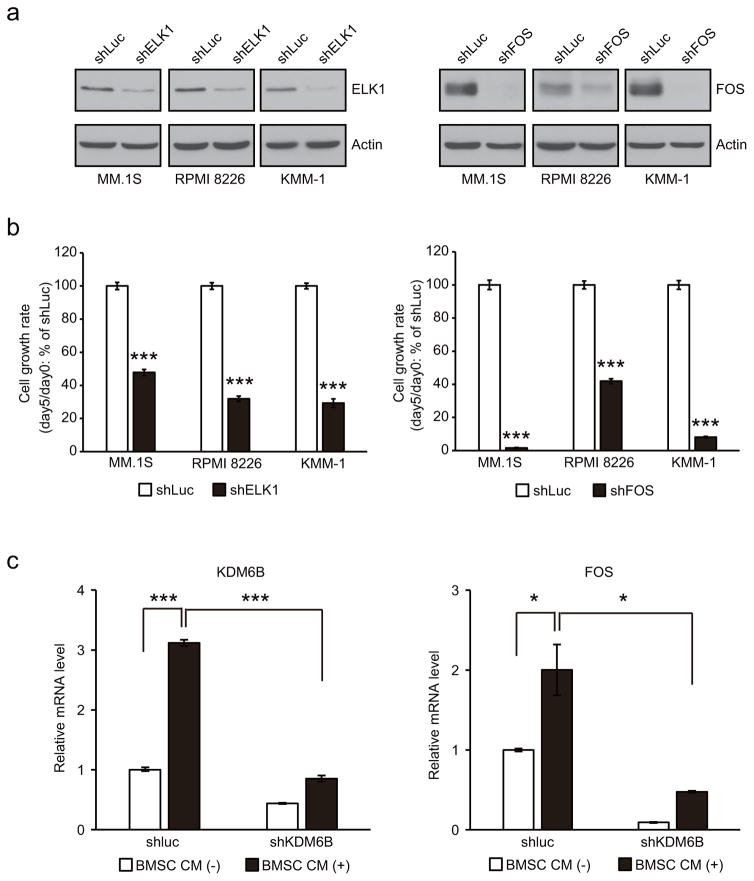
ELK1 and FOS are crucial factors for MM cell growth
We next ascertained whether ELK1 and FOS, the effector transcription factors of MAPK pathway, are required for MM cell growth. shRNA against ELK1 or FOS were transduced into 3 MM cell lines, and immunoblot analyses confirmed reduction of ELK1 or FOS protein after transduction of each shRNA (Figure 8a). Under these condition, cell growth was markedly reduced in MM cell lines (Figure 8b), indicating that these transcription factors mediate MM cell growth.
Figure 8.
ELK1 and FOS are crucial factors for MM cell growth.
(a,b) MM.1S, RPMI 8226 and KMM-1 cells were transduced with shELK1, shFOS or shLuc. Three days post infection is designated as day 0. (a) On day 0, whole cell lysates were extracted and subjected to immunoblot analysis with anti-ELK1 or FOS. (b) The cell growth rate (day 5/day 0) relative to shLuc is shown. Data represent mean ± s.d. of quadruplicate cultures. *** P < 0.001 compared with shLuc.
(c) MM.1S cells transduced with shKDM6B or shLuc were treated with BMSC CM or control culture medium for 2h. Data represent the amount of mRNA relative to shLuc treated with control culture medium. Error bars indicate s.d. of triplicate measurements. *P < 0.05, ***P < 0.001.
Finally, we determined whether BMSCs induce FOS expression, as BMSCs activate NF-κB pathway and induce KDM6B expression in MM cells. As shown in Figure 8c, BMSC CM induced FOS expression in MM.1S cells. This induction was abrogated by KDM6B knockdown (Figure 8c), suggesting that BMSC-induced FOS expression is mediated by KDM6B in MM cells.
DISCUSSION
In this study, we show that KDM6B is induced by activation of NF-κB pathway, and that KDM6B in turn upregulates molecules of MAPK pathway, thereby promoting MM cell growth and survival. Previous reports showed KDM6B dependence in other types of cancers,14–17 but those mechanisms are distinct from our findings in MM. In T cell acute lymphoblastic leukemia, KDM6B regulates genes related to NOTCH pathway,14 whereas silencing of KDM6B has no effect on NOTCH pathway-related genes in MM cells (Supplementary Table 5). Interestingly, Zhang et al. showed subtype-specific KDM6B dependence in diffuse large B cell lymphoma (DLBCL): KDM6B maintains survival of germinal center B cell-like DLBCL through activating BCL2 expression, whereas it promotes activated B cell-like DLBCL survival via upregulating IRF4 expression.17 IRF4 is also known to be an essential survival factor in MM,28, 29 but IRF4 expression is not affected by knockdown of KDM6B in MM cells. A tumor suppressor role of KDM6B has also been reported.10, 11 Oncogenic stress-induced KDM6B upregulates INK4A/ARF, resulting in cellular senescence, but not in MM. These data suggest the cancer type-specific roles of KDM6B.
We here demonstrate that KDM6B regulates MAPK pathway-related genes in a catalytically-independent manner. Several studies have highlighted the demethylase activity-independent functions of KDM6B in different contexts.25–27 Using ChIP-sequencing, De Santa et al. showed that KDM6B is preferentially recruited to transcriptional start sites where H3K27 is not methylated in LPS-activated macrophages, suggesting that KDM6B regulates transcription of target genes independently of H3K27 demethylation.25 KDM6B has also been shown to be required for chromatin remodeling in a demethylase-independent fashion by mediating T-bet interaction with a Brg1-containing SWI/SNF complex in Th1 cells.27 Furthermore, KDM6B facilitates ubiquitination of PHF20 by E3 ubiquitin ligase Trim26, thereby triggering PHF20 degradation.26 These studies support the notion that KDM6B mediates various biological functions not only via its H3K27 demethylase activity, but also its non-enzymatic activity.
Our current data suggest that KDM6B represents a potential therapeutic target in MM, and that targeting KDM6B protein itself, but not enzymatic activity, is necessary, given its demethylase-independent function in MM. Inhibition of NF-κB pathway may be one of the promising strategies, since KDM6B expression is, at least in part, regulated by NF-κB. For direct targeting of KDM6B, proteolysis targeting chimeras (PROTACs) technology might be suitable. PROTACs are chimera drugs that recruit specific target protein to E3 ubiquitin ligase, thereby facilitating ubiquitination and resulting degradation of target protein.30 Recent reports in this field showed that target-specific degradation can be achieved at nano molar range within 4 h using two different ubiquitin ligase ligands in cultured cells.31–34 Furthermore, two of these reports demonstrated that their PROTACs reduce the target protein levels even in xenografted tumor cells.32, 34 Thus, PROTACs might be a promising technology for targeting KDM6B protein, even though there is a requirement to identify a KDM6B-specific small molecule ligand for the application of PROTACs.
In conclusion, we identify KDM6B as a key molecule promoting growth and survival of MM cells, independent of its demethylase activity. Our work delineates the role of KDM6B in MM pathogenesis, and validates KDM6B as a promising therapeutic target in MM.
Supplementary Material
Acknowledgments
We thank Dr. John Quackenbush and members of the Center for Cancer Computational Biology, Dana-Farber Cancer Institute for assistance with RNA-seq analysis. This research was supported by NIH grants SPORE P50-CA100707 (KCA), P01-CA078378 (KCA), R01-CA050947 (KCA) and R01-CA178264 (TH and KCA). KCA is an American Cancer Society Clinical Research Professor.
Footnotes
Conflict of interest: The authors declare no conflict of interest.
AUTHOR CONTRIBUTIONS
HO designed and performed experiments, analyzed the data, and wrote the manuscript; T.Harada, MS and SK analyzed the data; Y-TT and PGR provided clinical samples. T.Hideshima and KCA analyzed the data, and edited the manuscript.
References
- 1.Hideshima T, Anderson KC. Molecular mechanisms of novel therapeutic approaches for multiple myeloma. Nature Reviews Cancer. 2002;2:927–937. doi: 10.1038/nrc952. [DOI] [PubMed] [Google Scholar]
- 2.Hideshima T, Mitsiades C, Tonon G, Richardson PG, Anderson KC. Understanding multiple myeloma pathogenesis in the bone marrow to identify new therapeutic targets. Nature Reviews Cancer. 2007;7:585–598. doi: 10.1038/nrc2189. [DOI] [PubMed] [Google Scholar]
- 3.Manier S, Salem KZ, Park J, Landau DA, Getz G, Ghobrial IM. Genomic complexity of multiple myeloma and its clinical implications. Nature Reviews Clinical Oncology. 2016 doi: 10.1038/nrclinonc.2016.122. [DOI] [PubMed] [Google Scholar]
- 4.Lohr JG, Stojanov P, Carter SL, Cruz-Gordillo P, Lawrence MS, Auclair D, et al. Widespread genetic heterogeneity in multiple myeloma: implications for targeted therapy. Cancer Cell. 2014;25:91–101. doi: 10.1016/j.ccr.2013.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bolli N, Avet-Loiseau H, Wedge DC, Van Loo P, Alexandrov LB, Martincorena I, et al. Heterogeneity of genomic evolution and mutational profiles in multiple myeloma. Nature Communications. 2014;5:2997. doi: 10.1038/ncomms3997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Walker BA, Boyle EM, Wardell CP, Murison A, Begum DB, Dahir NM, et al. Mutational Spectrum, Copy Number Changes, and Outcome: Results of a Sequencing Study of Patients With Newly Diagnosed Myeloma. Journal of Clinical Oncology. 2015;33:3911–3920. doi: 10.1200/JCO.2014.59.1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Santa F, Totaro MG, Prosperini E, Notarbartolo S, Testa G, Natoli G. The histone H3 lysine-27 demethylase Jmjd3 links inflammation to inhibition of polycomb-mediated gene silencing. Cell. 2007;130:1083–1094. doi: 10.1016/j.cell.2007.08.019. [DOI] [PubMed] [Google Scholar]
- 8.Agger K, Cloos PA, Christensen J, Pasini D, Rose S, Rappsilber J, et al. UTX and JMJD3 are histone H3K27 demethylases involved in HOX gene regulation and development. Nature. 2007;449:731–734. doi: 10.1038/nature06145. [DOI] [PubMed] [Google Scholar]
- 9.Lan F, Bayliss PE, Rinn JL, Whetstine JR, Wang JK, Chen S, et al. A histone H3 lysine 27 demethylase regulates animal posterior development. Nature. 2007;449:689–694. doi: 10.1038/nature06192. [DOI] [PubMed] [Google Scholar]
- 10.Agger K, Cloos PA, Rudkjaer L, Williams K, Andersen G, Christensen J, et al. The H3K27me3 demethylase JMJD3 contributes to the activation of the INK4A-ARF locus in response to oncogene- and stress-induced senescence. Genes & Development. 2009;23:1171–1176. doi: 10.1101/gad.510809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barradas M, Anderton E, Acosta JC, Li S, Banito A, Rodriguez-Niedenfuhr M, et al. Histone demethylase JMJD3 contributes to epigenetic control of INK4a/ARF by oncogenic RAS. Genes & Development. 2009;23:1177–1182. doi: 10.1101/gad.511109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jepsen K, Solum D, Zhou T, McEvilly RJ, Kim HJ, Glass CK, et al. SMRT-mediated repression of an H3K27 demethylase in progression from neural stem cell to neuron. Nature. 2007;450:415–419. doi: 10.1038/nature06270. [DOI] [PubMed] [Google Scholar]
- 13.Sen GL, Webster DE, Barragan DI, Chang HY, Khavari PA. Control of differentiation in a self-renewing mammalian tissue by the histone demethylase JMJD3. Genes & Development. 2008;22:1865–1870. doi: 10.1101/gad.1673508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ntziachristos P, Tsirigos A, Welstead GG, Trimarchi T, Bakogianni S, Xu L, et al. Contrasting roles of histone 3 lysine 27 demethylases in acute lymphoblastic leukaemia. Nature. 2014;514:513–517. doi: 10.1038/nature13605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hashizume R, Andor N, Ihara Y, Lerner R, Gan H, Chen X, et al. Pharmacologic inhibition of histone demethylation as a therapy for pediatric brainstem glioma. Nature Medicine. 2014;20:1394–1396. doi: 10.1038/nm.3716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park WY, Hong BJ, Lee J, Choi C, Kim MY. H3K27 Demethylase JMJD3 Employs the NF-kappaB and BMP Signaling Pathways to Modulate the Tumor Microenvironment and Promote Melanoma Progression and Metastasis. Cancer Research. 2016;76:161–170. doi: 10.1158/0008-5472.CAN-15-0536. [DOI] [PubMed] [Google Scholar]
- 17.Zhang Y, Shen L, Stupack DG, Bai N, Xun J, Ren G, et al. JMJD3 promotes survival of diffuse large B-cell lymphoma subtypes via distinct mechanisms. Oncotarget. 2016;7:29387–29399. doi: 10.18632/oncotarget.8836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Svotelis A, Bianco S, Madore J, Huppe G, Nordell-Markovits A, Mes-Masson AM, et al. H3K27 demethylation by JMJD3 at a poised enhancer of anti-apoptotic gene BCL2 determines ERalpha ligand dependency. The EMBO Journal. 2011;30:3947–3961. doi: 10.1038/emboj.2011.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wei Y, Chen R, Dimicoli S, Bueso-Ramos C, Neuberg D, Pierce S, et al. Global H3K4me3 genome mapping reveals alterations of innate immunity signaling and overexpression of JMJD3 in human myelodysplastic syndrome CD34+ cells. Leukemia. 2013;27:2177–2186. doi: 10.1038/leu.2013.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shah N, Asch RJ, Lysholm AS, Lebien TW. Enhancement of stress-induced apoptosis in B-lineage cells by caspase-9 inhibitor. Blood. 2004;104:2873–2878. doi: 10.1182/blood-2003-10-3720. [DOI] [PubMed] [Google Scholar]
- 21.Annunziata CM, Davis RE, Demchenko Y, Bellamy W, Gabrea A, Zhan F, et al. Frequent engagement of the classical and alternative NF-kappaB pathways by diverse genetic abnormalities in multiple myeloma. Cancer Cell. 2007;12:115–130. doi: 10.1016/j.ccr.2007.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Keats JJ, Fonseca R, Chesi M, Schop R, Baker A, Chng WJ, et al. Promiscuous mutations activate the noncanonical NF-kappaB pathway in multiple myeloma. Cancer Cell. 2007;12:131–144. doi: 10.1016/j.ccr.2007.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Huang da W, Sherman BT, Lempicki RA. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nature Protocols. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 24.Huang da W, Sherman BT, Lempicki RA. Bioinformatics enrichment tools: paths toward the comprehensive functional analysis of large gene lists. Nucleic Acids Research. 2009;37:1–13. doi: 10.1093/nar/gkn923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.De Santa F, Narang V, Yap ZH, Tusi BK, Burgold T, Austenaa L, et al. Jmjd3 contributes to the control of gene expression in LPS-activated macrophages. The EMBO Journal. 2009;28:3341–3352. doi: 10.1038/emboj.2009.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zhao W, Li Q, Ayers S, Gu Y, Shi Z, Zhu Q, et al. Jmjd3 inhibits reprogramming by upregulating expression of INK4a/Arf and targeting PHF20 for ubiquitination. Cell. 2013;152:1037–1050. doi: 10.1016/j.cell.2013.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller SA, Mohn SE, Weinmann AS. Jmjd3 and UTX play a demethylase-independent role in chromatin remodeling to regulate T-box family member-dependent gene expression. Molecular Cell. 2010;40:594–605. doi: 10.1016/j.molcel.2010.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shaffer AL, Emre NC, Lamy L, Ngo VN, Wright G, Xiao W, et al. IRF4 addiction in multiple myeloma. Nature. 2008;454:226–231. doi: 10.1038/nature07064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ohguchi H, Hideshima T, Bhasin MK, Gorgun GT, Santo L, Cea M, et al. The KDM3A-KLF2-IRF4 axis maintains myeloma cell survival. Nature Communications. 2016;7:10258. doi: 10.1038/ncomms10258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Deshaies RJ. Protein degradation: Prime time for PROTACs. Nature Chemical Biology. 2015;11:634–635. doi: 10.1038/nchembio.1887. [DOI] [PubMed] [Google Scholar]
- 31.Lu J, Qian Y, Altieri M, Dong H, Wang J, Raina K, et al. Hijacking the E3 Ubiquitin Ligase Cereblon to Efficiently Target BRD4. Chemistry & Biology. 2015;22:755–763. doi: 10.1016/j.chembiol.2015.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Winter GE, Buckley DL, Paulk J, Roberts JM, Souza A, Dhe-Paganon S, et al. DRUG DEVELOPMENT. Phthalimide conjugation as a strategy for in vivo target protein degradation. Science. 2015;348:1376–1381. doi: 10.1126/science.aab1433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zengerle M, Chan KH, Ciulli A. Selective Small Molecule Induced Degradation of the BET Bromodomain Protein BRD4. ACS Chemical Biology. 2015;10:1770–1777. doi: 10.1021/acschembio.5b00216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bondeson DP, Mares A, Smith IE, Ko E, Campos S, Miah AH, et al. Catalytic in vivo protein knockdown by small-molecule PROTACs. Nature Chemical Biology. 2015;11:611–617. doi: 10.1038/nchembio.1858. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.