Abstract
Objective
Despite substantial evidence of the benefits of breastfeeding for both mothers and children, rates of sustained breastfeeding in the United States are quite low. This study examined whether mandated coverage of lactation support services under the Affordable Care Act (ACA) affects breastfeeding behavior.
Data Source
We studied the census of U.S. births included in the National Vital Statistics System from 2009 to 2014.
Study Design
We used regression‐adjusted difference‐in‐differences (DD) to examine changes in breastfeeding rates for privately insured mothers relative to those covered by Medicaid. We adjusted for several health and sociodemographic measures. We also examined the extent to which the effect varied across vulnerable populations—by race/ethnicity, maternal education, WIC status, and mode of delivery.
Principal Findings
Results suggest that the ACA mandate increased the probability of breastfeeding initiation by 2.5 percentage points, which translates into about 47,000 more infants for whom breastfeeding was initiated in 2014. We find larger effects for black, less educated, and unmarried mothers.
Conclusions
The Affordable Care Act–mandated coverage of lactation services increased breastfeeding initiation among privately insured mothers relative to mothers covered by Medicaid. The magnitude of the effect size varied with some evidence of certain groups being more likely to increase breastfeeding rates.
Keywords: Breastfeeding, Affordable Care Act
Breastfeeding offers remarkable disease protection for both mothers and children (Ip et al. 2007; American Academy of Pediatricians 2012). Nearly 72 percent of mothers are breastfeeding their newborns at the time of hospital discharge, but there are significant differences across sociodemographic groups. For example, only 58 percent of low‐income mothers receiving supplemental nutrition assistance through the Women, Infants, and Children (WIC) program, 64 percent of mothers with less than a college degree education, and about 59–60 percent of Hispanic and black mothers attempt to breastfeed their newborns, according to vital statistics records.1
Studies have shown that the use of lactation services, including lactation consultants and breast pumps, can increase both a woman's commitment to and her success with breastfeeding (Bonuck et al. 2005; Olson et al. 2010; Haider et al. 2014). These studies found the use of lactation consultants and peer or role models for counseling increased breastfeeding duration and intensity. Breast pumps, a necessity for mothers who need to be separated from their infants for work or school, can also stimulate milk production to address low milk supply issues (Merewood et al. 2003; Chamberlain et al. 2006; Kent, Prime, and Garbin 2012). Access to breast pumps may be particularly critical for low‐income mothers who may need to return to work soon after delivery (Chamberlain et al. 2006).
The Affordable Care Act (ACA) mandated that all nongrandfathered private health insurance plans must provide coverage for lactation support, counseling, and equipment for breastfeeding starting with the first plan or policy year beginning on or after August 1, 2012 (through the requirement of coverage of preventive services, in Section 2713). Although this mandate did not address existing Medicaid coverage policies, the wider availability and affordability of private health insurance through subsidized Marketplace plans has the potential to greatly expand coverage for low‐income pregnant women who did not qualify for Medicaid because their household income was above the eligibility threshold (about 200 percent of the Federal Poverty Level nationally).2 Little is known, however, about the effect of this expanded coverage on breastfeeding initiation, particularly for vulnerable populations who may have limited access to social supports and resources that would improve breastfeeding success.
Overall estimates suggest that if 80 percent of mothers breastfed for 6 months, the United States could save $10.5 billion in health care costs in the infant's first year of life alone. These cost savings might be greater to the extent that diseases prevented by breastfeeding are more prevalent among certain disadvantaged populations (Bartick and Reinhold 2010). Moreover, savings beyond the first year of life may also be realized to the extent that breastfeeding prevents long‐term chronic conditions, such as obesity (Armstrong and Reilly 2002; Arenz et al. 2004). Thus, the return on investment for mandated coverage of lactation services may be substantially greater if mandated coverage mitigates breastfeeding disparities.
This study provides evidence on the extent to which mandated health insurance coverage of lactation services influences breastfeeding initiation using a regression‐adjusted difference‐in‐differences model and the NCHS NVSS birth data from 2009 to 2014.
Previous Literature
Breastfeeding has been linked to a host of positive child and maternal health outcomes. In particular, breastfeeding has been linked to reduced risks of acute otitis media, gastrointestinal infections, respiratory tract diseases, childhood obesity, and Type 2 diabetes for normal term infants (Ip et al. 2007). For mothers, breastfeeding has been linked to lower postpartum weight retention, incidence of Type 2 diabetes, hyperlipidemia, hypertension, cardiovascular disease, and risk of breast and ovarian cancers (Janney, Zhang, and Sowers 1997; Olson et al. 2003; Stuebe et al. 2005; Schwarz et al. 2009; Østbye et al. 2012). More recent studies have started to question whether previous studies have overestimated the true effects of breastfeeding, particularly on long‐term health outcomes and cognitive development, because women nonrandomly choose to breastfeed (selection bias) (Kramer et al. 2001; Evenhouse and Reilly 2005; Colen and Ramey 2014). The evidence from this newer literature, however, is mixed with some randomized control trials (RCTs) still documenting positive effects of breastfeeding on cognitive ability (Kramer et al. 2001; Kramer 2010), better infant health outcomes, and lower health care costs (Pugh et al. 2002; Anderson et al. 2005). Two sibling studies using within‐mother differences in feeding behaviors have found virtually no positive effects of breastfeeding on long‐term outcomes (Evenhouse and Reilly 2005; Colen and Ramey 2014). Evidence of the benefits of breastfeeding on more immediate child and maternal health outcomes, however, are well established and less controversial (Kramer 2010).
In a Grossman (1972) model of health capital, an infant's stock of health capital depends, largely, on early maternal investments, which are constrained both by the mother's budget and her time (Ruhm 2000). Breastfeeding requires both initial (in some ways “fixed”) costs and ongoing, variable costs. Initially, breastfeeding can be difficult, often requiring help from a lactation consultant, and is very labor intensive with newborns who require feeding every 2–3 hours (American Academy of Pediatricians 2015), on average. Estimates suggest that new breastfeeding mothers spend 75–100 minutes per day nursing or about 5 additional hours per week relative to mothers who choose formula feeding (Cohen et al. 1995; Jegier et al. 2010; Smith and Forrester 2013). As infants get older, the frequency of breastfeeding declines and infants become more efficient at nursing. As nursing mothers return to work, however, time dedicated to breastfeeding may actually increase as separation from the infant requires the mother to express milk while she is away. According to Consumer Reports, a personal‐use electric pump can retail for as much as $400 and hospital‐grade pumps can be rented for about $55 per month (Consumer Reports 2013). Even though this is significantly less than the typical cost of a month's supply of infant formula (at about $170 per month [Consumer Reports 2013]), the time costs of breastfeeding for mothers as they return to work are also likely to increase (Smith and Forrester 2013). Finally, studies suggest that expressing milk with a pump may actually require more time than the mother would have spent nursing and is negatively correlated with milk supply (Zinaman et al. 1992; Meier et al. 2012). Clearly, the economic costs of breastfeeding for mothers are nontrivial.
Differences in the economic burden, both in terms of time and out‐of‐pocket expenditures for lactation support, may at least partially explain the well‐documented heterogeneity in breastfeeding initiation and duration among vulnerable populations. Although breastfeeding initiation (measured when the child is 19–36 months old)3 increased from 70.3 percent of mothers in 2000 to 74.6 percent in 2008 (Allen et al. 2013), stark differences remain across subgroups of mothers with 60 percent or less of lower income, less educated, and racial/ethnic minority mothers initiating breastfeeding according to vital statistics records.1 Breastfeeding rates also tend to increase with maternal age and household income (Roe et al. 1999; Centers for Disease Control and Prevention 2012).
Empirical evidence on efforts to reduce the economic burden of breastfeeding has largely been focused on the effects of maternity leave benefits for mothers. Several studies have found that maternity leave increases both breastfeeding initiation and duration (Roe et al. 1999; Dennis 2002; Chatterji and Frick 2005; Baker and Milligan 2008). Returning to work is similarly associated with reduced breastfeeding (Mandal, Roe, and Fein 2010). One study estimating a simultaneous equations model using the Infant Feeding Practices Study data found that mothers working 8 hours outside the home when the infant was 3 months old had 1.5 fewer breastfeedings per day on average relative to mothers not working outside the home (Roe et al. 1999). More generally, increasing evidence suggests that efforts through state laws and employer initiatives to mitigate the costs and burden associated with continuing to breastfeed upon return to work have resulted in improvements in breastfeeding rates (Cohen and Mrtek 1994; Slusser et al. 2004; Hawkins, Stern, and Gillman 2013). The ACA also mandated that employers provide mothers with adequate space and time to pump, but empirical evidence on the effect of this mandate has yet to be established.
Although the ACA specifically addresses lactation support services and equipment, other public programs have been linked to breastfeeding among vulnerable populations. Perhaps most notable is the Special Supplemental Nutrition Program for WIC, which is designed to provide nutritional support and education to lower income pregnant and postpartum WIC. Many researchers have noted lower breastfeeding rates and duration among WIC participants (Ryan and Zhou 2006; Jacknowitz, Novillo, and Tiehen 2007; Martin‐Anderson 2013), but it is unclear how much of this is driven by program design that supplies vouchers for infant formula to mothers who do not exclusively breastfeed, and how much is driven by the individual characteristics of the mothers and infants enrolled in the program. Studies that addressed selection bias in program participation have generated mixed results ranging from positive effects (Joyce, Racine, and Yunzal‐Butler 2008) to suggestive but imprecise negative effects from instrumental variables estimation (Chatterji et al. 2002) to conclusions that differences are driven by differences in maternal characteristics (Jiang, Foster, and Gibson‐Davis 2010). Recent analysis using variation in food prices as an instrument for WIC participation suggests little effect on breastfeeding initiation rates, but large reductions in the amount of time spent breastfeeding exclusively (e.g., not supplementing with formula) (Bullinger and Gurley‐Calvez 2015).
Previous studies have also noted a link between mode of delivery and breastfeeding initiation (Evans et al. 2003). For example, in 2014, only 59 percent of mothers delivering via Cesarean delivery initiated breastfeeding as of discharge compared to 68 percent of mothers delivering vaginally.1 Cesareans result in a painful incision and stress that may hinder breastfeeding by limiting the positions in which a mother can hold her infant for nursing and affect the production of milk supply (Evans et al. 2003; Karlström et al. 2007). Thus, the use of lactation consultants or breast pumps to stimulate milk production may improve rates among Cesarean delivery mothers.
As health service providers and policy makers grapple with the most effective ways to encourage breastfeeding, in this study, we aim to examine the effects of recent policy changes. Specifically, we estimate the effect of the ACA‐mandated coverage of lactation support services, including coverage of lactation consultant visits and breast pumps, on breastfeeding initiation overall, and among vulnerable populations.
Methods
Data
We used publicly available birth certificate data from the NVSS—housed and maintained by the NCHS—to examine the impact of lactation support services on breastfeeding initiation. The NVSS births data are derived from all birth certificates provided by states to NCHS as mandated by federal law. We analyzed data from 2009 to 2014. Aside from containing nearly all births in the United States in a given year, the NVSS data contain information on whether each infant was being breastfed at the time of hospital discharge, details about the infant at birth, and several sociodemographic characteristics of the mother. We restricted our sample to births where our key measures (described below) are not missing, most importantly including payment source of the birth—private health insurance, Medicaid, Indian Health Service, CHAMPUS/TRICARE, other government payer, or self‐pay. Our primary analytic sample contains 17,975,231 births from 2009 to 2014 (8,698,072 covered by Medicaid and 9,287,512 covered by private health insurance).4
Approach
Our primary analytic strategy was to estimate a regression‐adjusted difference‐in‐differences (DD) model using repeated cross‐sectional data. The regression‐adjusted DD model was as follows:
| (1) |
where BF it is a dichotomous variable equal to one if mother i had initiated breastfeeding during the period from birth to hospital discharge in birth year, t, and birth month, m. PrivHI i equals one if the source of payment for the birth was private health insurance and zero otherwise. Although not all mothers with privately insured births would be eligible for the lactation support services and some may have been covered by plans that were already offering such benefits, we compared the change in breastfeeding rates among privately insured mothers with the change in breastfeeding rates among mothers with several other categories of health insurance/source of payment. We examined the plausibility of the common trend assumption in this analysis (see Figure 1 discussed below) and concluded that the Medicaid births are a plausible comparison group,5 but we note how the main results change if we used self‐insured or CHAMPUS/VA births instead. As these comparison groups would not have been affected by the mandated coverage, the DD model should allow us to use these comparison births to difference out any secular trends in breastfeeding that are unrelated to the mandate. Year t is a vector of year dummies (2009 is the omitted year) for each birth year. Using the vector of year indicators instead of a simple “postperiod” indicator allows us to compare changes in breastfeeding rates across multiple years. This is important because although the mandate was effective in 2012, plans technically had until the start of the next plan year (typically January) to provide this coverage. This specification allows us to compare behavior in 2013 or 2014 relative to 2009 (before any ACA changes) or other years after which the ACA was passed but before the mandate (e.g., 2010 or 2011). X is a vector of individual‐level independent control variables, including mother's age at birth, four educational attainment indicators for the mother (less than high school is the omitted category), four racial/ethnic categories of the mother (white is the omitted category), a Hispanic/Latino ethnicity indicator, an indicator for whether the mother was married at the time of birth, whether the mother received WIC during the pregnancy, and parity (number of previous births). X also includes characteristics related to the birth and associated with breastfeeding rates—an indicator for whether the birth occurred in a hospital, an indicator for Cesarean delivery, an indicator for whether the newborn was a boy, indicators for the plurality of the birth (singleton, twins, triplets, quadruplets, or quintuplets or more), the weeks of gestation at the time of birth, and the infant's 5‐minute APGAR score, an indicator of overall infant health (Casey, McIntire, and Leveno 2001), and two indicators for whether the infant had any congenital anomalies6 or abnormal newborn conditions.7 In addition, we included three indicators for maternal risk factors, morbidities, and infections, respectively, to control for differences that might have influenced the difficulty of the labor and delivery in a way that might have influenced breastfeeding proclivity.8 The indicator for maternal risk factor equals one if the mother had any of the following: prepregnancy diabetes, gestational diabetes, prepregnancy hypertension, gestational hypertension, eclampsia, previous preterm birth, previous poor pregnancy outcome, infertility treatment, fertility‐enhancing drugs, assistive reproductive technology, and any previous Cesarean deliveries. The indicator for any maternal morbidity equals one if the mother had any of the following complications with the labor/delivery: transfusion, perineal laceration, ruptured uterus, unplanned hysterectomy, admission to intensive care, or an unplanned operation. The indicator for any maternal infection equals one if the mother had gonorrhea, syphilis, chlamydia, Hepatitis B, or Hepatitis C. Experiencing any of these risk factors, morbidities, or infections may influence the difficulty of the labor/delivery and the likelihood of a Cesarean delivery, which might, therefore, affect the likelihood of attempting breastfeeding. Results without these controls are largely consistent with those presented here. M is a vector of month‐of‐birth fixed effects that absorb any seasonal differences in breastfeeding behaviors (Currie and Schwandt 2013). We estimated equation (1) as a logistic regression but report predicted probabilities with covariates held at their means in tables below. β 3 represents our set of regression‐adjusted DD estimates.
Figure 1.
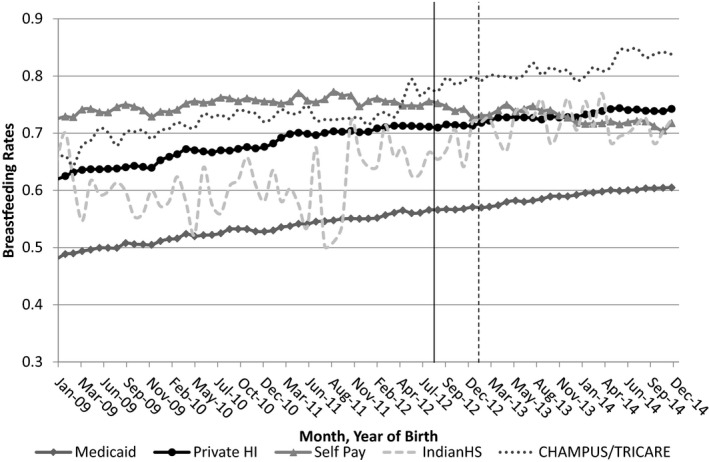
Trends in Breastfeeding Rates, by Source of Payment (for Delivery)
- Notes: 2009–2014 NVSS Births data. Vertical lines represent the legislative implementation (August 2012) and likely effective implementation at the modal plan start month (January 2013) dates. N = 24,005,896 births.
To test whether the mandate mitigated disparities in breastfeeding behaviors, we included interaction terms with variables that define certain vulnerable populations:
| (2) |
where Group equals one for individuals in each vulnerable population and zero otherwise. We defined the following vulnerable population groupings based on the previously documented disparities in breastfeeding along these sociodemographic and health characteristics: race,9 WIC recipient, maternal education, maternal marital status, and Cesarean delivery. The other measures are as described for equation (1). From this model, we are interested in β 7 to determine whether the mandate resulted in changes in breastfeeding behavior differentially for women in the aforementioned subgroups relative to their counterparts.
We note that our measure of “treatment,” in this case, whether the birth's payment source was private health insurance, may suffer from measurement error. In particular, we cannot observe with certainty whether the mother/child was covered by a nongrandfathered health insurance plan at the time of birth or whether the mother's plan covered lactation support services prior to the mandate. In 2014, approximately 26 percent of workers in the United States were covered by a grandfathered plan (i.e., not subject to the ACA mandate) (Claxton et al. 2014). This is down from 56 percent of workers in 2011. Thus, to the extent that our treatment group includes women who were not treated (contamination), our estimated effect will be biased downward. Similarly, although the rates of breastfeeding initiation among Medicaid births appear to have trended similarly in premandate periods, there may actually be some Medicaid births (especially in later years) where the mandate would have applied. That is, the mandate applies to newly eligible Medicaid enrollees, most of whom gained eligibility beginning in 2014 (though eight states expanded Medicaid prior to 2014)10 (Kaiser Family Foundation 2012). This implies that our comparison group may actually contain some “treated” individuals, which will attenuate our estimated treatment effect. Thus, we view our results as a conservative or lower bound of the true treatment effect.
Results
In Figure 1, we present the percent of infants who were breastfed as of hospital discharge over time, stratified by all sources of payment, not just private health insurance and Medicaid (N = 24,005,896). In general, rates of breastfeeding are increasing over time, except for self‐paid births. Notably, for our purposes, although breastfeeding rates are lower among Medicaid births, the trend over time in the preperiod is similar to the trend among private health insurance births.
In Table 1, we present descriptive statistics for our primary analytic sample (Medicaid and private health insurance births). Mothers whose births were paid for by Medicaid are clearly different from mothers covered by private health insurance across several sociodemographic and health characteristics. Overall, about 62 percent of mothers initiated breastfeeding as of discharge.
Table 1.
Descriptive Statistics
| Full Sample | Medicaid | Private HI | |
|---|---|---|---|
| Maternal characteristics | |||
| Age | 27.97 (6.03) | 25.65 (5.82) | 30.14 (5.38) |
| Race = White (%) | 77.04 (42.06) | 71.11 (45.33) | 82.19 (38.26) |
| Race = Black (%) | 15.72 (36.40) | 23.22 (42.23) | 8.69 (28.17) |
| Race = American Indian/Alaska Native (%) | 0.99 (9.89) | 1.54 (12.32) | 0.47 (6.83) |
| Race = Asian/Pacific Islander (%) | 6.47 (24.59) | 4.13 (19.89) | 8.65 (28.12) |
| Hispanic (%) | 33.42 (47.17) | 40.12 (49.01) | 27.14 (44.47) |
| Education <HS (%) | 17.29 (37.82) | 30.60 (46.08) | 4.83 (21.45) |
| Education = HS (%) | 25 (43.30) | 36.27 (48.08) | 14.46 (35.17) |
| Education = Some college (%) | 28.56 (45.17) | 27.45 (44.62) | 29.61 (45.65) |
| Education = College+ (%) | 29.14 (45.44) | 5.69 (23.17) | 51.10 (49.99) |
| Married (%) | 59.1 (49.17) | 34.44 (47.52) | 82.19 (38.26) |
| Had prenatal care (%) | 95.21 (21.36) | 94.14 (23.49) | 96.19 (19.16) |
| Smoked before pregnancy (%) | 10.74 (30.96) | 15.94 (36.61) | 5.86 (23.49) |
| Smoked during pregnancy (%) | 8.04 (27.20) | 12.85 (33.47) | 3.55 (18.5) |
| No. of previous births | 1.52 (1.68) | 1.70 (1.8) | 1.34 (1.55) |
| Had any risk factors* (%) | 27.1 (44.44) | 26.22 (43.98) | 27.93 (44.87) |
| Had any maternal morbidities† (%) | 1.47 (12.02) | 1.19 (10.84) | 1.73 (13.03) |
| Had any infections present‡ (%) | 2.41 (15.33) | 3.96 (19.5) | 0.96 (9.75) |
| Infant/birth characteristics | |||
| Breastfed at discharge (%) | 62.99 (48.28) | 55.47 (49.7) | 70.04 (45.81) |
| Baby boy (%) | 51.17 (49.99) | 51.08 (49.99) | 51.25 (49.98) |
| Hospital birth (%) | 99.42 (0.08) | 99.59 (6.4) | 99.26 (8.55) |
| Singletons (%) | 96.49 (18.41) | 97.31 (16.17) | 95.71 (20.26) |
| Twins (%) | 3.38 (18.08) | 2.63 (15.99) | 4.09 (19.81) |
| Weeks of gestation | 38.61 (3.18) | 38.55 (3.32) | 38.66 (3.06) |
| 5‐minute APGAR (0–10) | 8.79 (0.83) | 8.77 (0.87) | 8.81 (0.78) |
| Cesarean delivery (%) | 33.21 (47.14) | 31.71 (46.54) | 34.57 (47.56) |
| Any abnormal newborn conditions§ (%) | 9.87 (29.82) | 10.38 (30.5) | 9.39 (29.17) |
| Any congenital anomalies¶ (%) | 0.29 (5.35) | 0.29 (5.35) | 0.29 (5.35) |
| N | 17,985,584 | 8,698,072 | 9,287,512 |
| % of all births** | 88.90% | 42.99% | 45.91% |
Means are statistically different across Medicaid and privately insured births on all measures at the 5% level or better, except for the presence of any congenital anomalies. Full sample includes all Medicaid and private health insurance births from 2009 to 2014. Mothers in this sample ranged from 12 to 50 years of age.
*Any risk factors equal one if the mother had any of the following conditions/treatments: prepregnancy diabetes, gestational diabetes, prepregnancy hypertension, gestational hypertension, eclampsia, previous preterm birth, previous poor pregnancy outcome, infertility treatment, fertility enhancing drugs, assistive reproductive technology, and any previous Cesarean deliveries.
†Any maternal morbidity equals one if the mother had any of the following complications with the labor/delivery: transfusion, perineal laceration, ruptured uterus, unplanned hysterectomy, admission to intensive care, or an unplanned operation.
‡Any maternal infections present equals one if the mother had gonorrhea, syphilis, chlamydia, Hepatitis B, or Hepatitis C.
§Any abnormal conditions of the newborn equals one if the infant had assisted ventilation (and whether that is greater than 6 hours), admission to NICU, surfactant, antibiotics, seizures, or birth injury.
¶Any congenital anomalies equals one if the infant had anencephaly, meningomyelocele/spina bifida, cyanotic congenital heart disease, congenital diaphragmatic hernia, omphalocele, gastroschisis, limb reduction defect, cleft lip palate, down syndrome, suspected chromosomal disorder, and hypospadias.
**Total births with non‐missing source of payment and breastfeeding initiation measures.
Next, we estimated the regression‐adjusted probability of breastfeeding at discharge as outlined in equation (1). In the first two rows of Table 2, we present the predicted probabilities obtained after estimation11 (holding all covariates at their means) for our treatment (covered by private health insurance) births and comparison (Medicaid) births for each year. Adjusted breastfeeding rates are similar in 2009 and 2010 for private health insurance and Medicaid mothers, but they start to diverge in 2011. Each year from 2011 onwards, breastfeeding rates among privately insured are 2–3 percentage points higher than among Medicaid births (first differences reported in row 3). In the last three rows of Table 2, we present DD estimates of the effect of the mandate using 2013 or 2014 as the final postperiod and comparing those years to 2009, 2010, and 2011. The increase in breastfeeding rates from 2009 to 2013 among privately insured is 1.5 percentage points greater than the increase among Medicaid births. The effect becomes larger in 2014, with an estimated DD of 2.5 percentage points. Comparing postyears to later “pre” years (e.g., 2010, 2011) yields smaller effect sizes. Using 2013 as the postyear period results in a smaller effect than using 2014 as the postyear, which may reflect a lagged effect. However, because most Medicaid expansions occurred in 2014, we might expect the effect size to be attenuated through contamination of the control group in 2014. Although we present results using three potential “pre” years—2009–2011, our preferred specification is using 2009 as the preyear as this was before other changes implemented as a result of the ACA would have been enacted. In models where we collapse pre‐ and postyears (and exclude 2012), we find about a 2 percentage point increase in breastfeeding due to the ACA mandate.
Table 2.
Adjusted Breastfeeding Rates by Payer, First Differences, DDs
| 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |
|---|---|---|---|---|---|---|
| Source of payment for delivery | ||||||
| Private Health Insurance | 0.58 (0.0004) | 0.60 (0.0004) | 0.63 (0.0004) | 0.65 (0.0004) | 0.66 (0.0004) | 0.70 (0.0004) |
| Medicaid | 0.57 (0.0004) | 0.59 (0.0004) | 0.60 (0.0004) | 0.62 (0.0004) | 0.64 (0.0004) | 0.67 (0.0004) |
| First difference | 0.008 (0.0006) | 0.016 (0.0006) | 0.028 (0.0006) | 0.025 (0.0006) | 0.023 (0.0006) | 0.033 (0.0005) |
| DD—versus 2009 | 0.015 (0.0008) | 0.025 (0.0008) | ||||
| DD—versus 2010 | 0.007 (0.0008) | 0.017 (0.0008) | ||||
| DD—versus 2011 | −0.005 (0.0008) | 0.005 (0.0007) | ||||
N = 17,985,584 births. Predicted probability of breastfeeding adjusted for covariates listed in equation (1). Full set of logistic regression results are in Table S1. All values are statistically significant at p < .01 or better.
In Table 3, we present just the DDs comparing 2013 (column 1) and 2014 (column 2) to 2009 for various subpopulations to estimate whether the mandate differentially affected vulnerable populations. We find a significant difference in the effect of the lactation support services mandate on black/African American births relative to white births: black/African American mothers are 1 to 2 percentage points more likely to initiate breastfeeding than white mothers are after the mandate. American Indian/Alaskan Native mothers are about 1 percentage point more likely to respond to the mandate relative to white mothers. We find little difference between Asian/Pacific Islander and white mothers’ changes in breastfeeding rates from 2009 to 2013, but as of 2014, breastfeeding initiation rates had increased more for white mothers than for Asian/Pacific Islander mothers.
Table 3.
DDs, by Sociodemographic Groups (Robust Standard Errors in Parentheses)
| 2013 versus 2009 | 2014 versus 2009 | |
|---|---|---|
| Maternal race | ||
| White (reference group) | 0.009*** (0.001) | 0.025*** (0.001) |
| Black/African American | 0.032 *** (0.002) | 0.034 *** (0.002) |
| American Indian/Alaska Native | 0.021** (0.01) | 0.039*** (0.01) |
| Asian/Pacific Islander | 0.0002 (0.004) | −0.005 (0.004) |
| Mother received WIC during pregnancy | ||
| No (reference group) | 0.019*** (0.001) | 0.021*** (0.001) |
| Yes | 0.007 *** (0.002) | 0.013 *** (0.002) |
| Maternal education | ||
| <High school degree or equivalent (reference group) | −0.010*** (0.003) | −0.003 (0.003) |
| High school degree or equivalent | 0.021 *** (0.002) | 0.034 *** (0.002) |
| Some college | 0.004 *** (0.002) | 0.012 *** (0.002) |
| College degree or higher | 0.009 *** (0.003) | 0.014 ** (0.003) |
| Mother married | ||
| Yes (reference group) | 0.006** (0.001) | 0.02*** (0.001) |
| No | 0.019 *** (0.002) | 0.030 *** (0.002) |
| Cesarean delivery | ||
| Yes (reference group) | 0.013*** (0.001) | 0.024*** (0.001) |
| No | 0.016*** (0.001) | 0.027 *** (0.001) |
N = 17,985,584 births. Predicted probability of breastfeeding adjusted for covariates listed in equation (1). Bolded DDs are statistically different from reference group DD at p < .05.
***p < .01, **p < .05, *p < .10.
We find some evidence of a small difference in breastfeeding rates by mother's WIC participation by 2014 with WIC mothers being about 0.5 to 1 percentage point less likely to initiate breastfeeding after the mandate. Breastfeeding rates increased the most since 2009 among mothers with a high school degree or equivalent. In contrast, rates among mothers with less than a high school degree actually declined. Comparisons in Table 3 by education compare mothers with no high school degree to other groups, but mothers with just a high school degree were about 2 percentage points more likely initiate breastfeeding after the mandate relative to more highly educated mothers. Unmarried mothers were about 1 percentage point more likely to initiate breastfeeding relative to married mothers after the mandate. Finally, we find no evidence of a differential effect of the mandate on breastfeeding initiation by mode of delivery.
Discussion
Overall, we found that the ACA‐mandated coverage of lactation support services increased breastfeeding initiation by as much as 2.5 percentage points, which represents as many as 47,000 more infants for whom breastfeeding was initiated in a given year in the United States12 This estimate may be a lower bound of the likely true effect as we cannot perfectly identify births that were covered by nongrandfathered plans or those where the mother had lactation support services prior to the mandate. If only 26 percent of covered employees were enrolled in grandfathered plans in 2014 (Claxton et al. 2014), a back‐of‐the‐envelope calculation would suggest true effect might be up to a 3.4 percentage point increase in breastfeeding initiation. It is worth noting that our measure of breastfeeding initiation, however, is as of hospital discharge and, thus, may suffer from measurement error. This could cause a bias if, for example, hospital recording of breastfeeding behavior was somehow systematically different for women over time and by source of payment.
We also find evidence of heterogeneous treatment effects. In particular, black/African American mothers were as much as 2 percentage points more likely to initiate breastfeeding after the mandate relative to white mothers. Mothers with a high school degree were about 2 percentage points more likely to initiate breastfeeding after the mandate relative to college‐educated mothers. Unmarried mothers were about 1 percentage point more likely to initiate breastfeeding after the mandate relative to married mothers. These differential impacts suggest a positive increase in breastfeeding rates among groups that have historically had lower breastfeeding rates. Although it is unknown whether these increases in initiation rates will translate into reducing disparities in sustained breastfeeding rates (e.g., at 6 or 12 months) and ultimately, infant health, these findings are promising. Many of the economic burdens—time and costs—of breastfeeding may be greater for less educated mothers or unmarried mothers, particularly to the extent that education or marital status proxy for income.
Breastfeeding initiation rates increased for both WIC and non‐WIC mothers, but more quickly for non‐WIC mothers. It is unclear why this might have occurred, unless WIC mothers were already getting lactation support services prior to the mandate. Although many state WIC offices offer these services (and pumps), there is variation across states (Forrestal, Briefel, and Mabli 2015). Future work should investigate this finding further.
In addition to the limitations mentioned previously, we note that defining a perfect comparison group is problematic because nearly everyone has been affected in some way by the ACA. Traditionally, Medicaid has not been required to provide lactation support services, but a Kaiser Family Foundation survey of state Medicaid offices found that 15 states covered lactation consultants and 31 covered equipment rentals (though not necessarily without cost‐sharing) (Ranji et al. 2009). As we noted above, newly eligible Medicaid enrollees enrolled as a result of the Medicaid expansions (starting in January 2014) would also have been covered by the preventive services mandate and therefore eligible for lactation support services. Thus, our comparison sample of Medicaid mothers might contain some “treated” women, which would bias our results downward. Using self‐insured births or CHAMPUS/VA covered‐births as two alternative comparison groups yielded much larger effect sizes (16 and 6 percentage point increase in breastfeeding initiation, respectively13), but we note that the preperiod trends for these two sets of mothers are different than for privately insured mothers (see Figure 1), thus potentially invalidating the necessary common trends assumption. We also explored using a propensity‐matched (PSM) sample, whereby we included only Medicaid births that were statistically similar to the births covered by private health insurance. Using one‐to‐one matching of births on year and month of birth, gender, plurality (singletons, twins, etc.), weeks of gestation at delivery, 5‐minute APGAR score, mode of delivery, maternal age, race/ethnicity, education, marital status, any maternal risk factors or morbidities, any infections present, any congenital anomalies, whether the mother received prenatal care, and smoked before/during pregnancy and excluding all observations not on the common support (sample size = 17, 396,144), we found similar effect sizes with a 1.24 (robust standard error = 0.0008) and 2.64 (robust standard error = 0.0008) percentage point increase in breastfeeding rates from 2009 to 2013 and 2014, respectively. We present the propensity score regression results in Table S3 and the PSM‐DD results in Table S4.
Early qualitative work suggests that despite the mandate, many barriers still exist for new mothers (National Women's Law Center 2015). In particular, there are reports of some health insurance plans imposing time limits to use benefits (e.g., within 48 days of birth), limiting coverage to a certain number of lactation consultant visits, or limiting coverage of equipment until after the baby is born and/or only with a prescription or prior authorization (National Women's Law Center 2015). In addition, there are concerns regarding the insurer network adequacy with reports of women being denied coverage for out‐of‐network providers, which is consistent with studies suggesting shortages of lactation consultants and lack of third‐party reimbursement for International Board Certified Lactation Consultants (Mannel and Mannel 2006).
Although we find evidence of an increase in breastfeeding rates, both overall and among certain vulnerable subpopulations, due to the ACA mandate, more work is needed to determine how these effects translate into long‐term breastfeeding rates (e.g., at 6 and 12 months postpartum) and, ultimately, child and maternal health outcomes.
Supporting information
Appendix SA1: Author Matrix.
Table S1: Regression Coefficients† from DD Estimation (Standard Errors in Parentheses).
Table S2: DD Results Using Alternative Comparison Groups.
Table S3: Regression Coefficients from Propensity Score Estimation: Dependent Variable = Source of Payment Is Private Health Insurance (Standard Errors in Parentheses).
Table S4: Adjusted Breastfeeding Rates by Payer, First Differences, DDs Using PSM Sample.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: This study was supported by grant R40MC28305, MCH Research Program, from the Maternal and Child Health Bureau (Title V, Social Security Act), Health Resources and Services Administration, Department of Health and Human Services.
Disclosures: None.
Disclaimers: None.
Notes
Authors calculations using the National Center for Health Statistics (NCHS) National Vital Statistics System (NVSS) birth data from 2014.
State Health Facts, Henry J. Kaiser Family Foundation. http://kff.org/health-reform/state-indicator/medicaid-and-chip-income-eligibility-limits-for-pregnant-women-as-a-percent-of-the-federal-poverty-level/#. Also note that newly eligible Medicaid enrollees enrolled as a result of the Medicaid expansions (beginning in January 2014) would be covered by the preventive services mandate and 26 states implemented expansions. Some states expanded Medicaid prior to 2014, which implies that some women insured by Medicaid would have been eligible for lactation support services. This would bias our estimates downwards. We discuss this in the conclusion section below.
Allen et al. (2013) use data from the National Immunization Study collected when most children are no longer being breastfed. The NVSS births data used in this study rely on breastfeeding as reported by hospitals as of maternal hospital discharge.
This represents about 75 percent of all births in the NVSS data from 2009 to 2014 (24,005,896 total births).
Note that pretrends in Figure 1 look qualitatively similar using adjusted breastfeeding rates instead of unadjusted rates.
Congenital anomalies noted in the birth certificate date include anencephaly, meningomyelocele/spina bifida, cyanotic congenital heart disease, congenital diaphragmatic hernia, omphalocele, gastroschisis, limb reduction defect, cleft lip palate, Down syndrome, suspected chromosomal disorder, and hypospadias.
Abnormal conditions of the newborn noted in the birth certificate data include assisted ventilation (and whether that is greater than 6 hours), admission to NICU, surfactant, antibiotics, seizures, or birth injury.
Our results presented below are robust to excluding births with more than one fetus, any congenital or fetal abnormalities, any maternal risk factors, morbidities, and infections. Results are not presented here, but they are available upon request.
We do not examine Hispanic origin because the birth certificate form was revised in 2003, but not finalized until 2014; thus, Hispanic ethnicity/origin was collected differently across states at different times until 2015. http://www.cdc.gov/nchs/features/birth_certificate_goes_final.htmI http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_01.pdf
The following states expanded Medicaid in response to the ACA prior to 2014: California, Connecticut, Colorado, District of Columbia, Minnesota, Missouri, New Jersey, and Washington.
The full set of regression coefficients is presented in Table S1.
Based on approximately 1.82 million births covered by private health insurance in 2014.
See Table S2.
References
- Allen, J. A. , Ruowei L., Scanlon K. S., Perrine C. G., Chen J., Odom E., and Black C.. 2013. “Progress in Increasing Breastfeeding and Reducing Racial/Ethnic Differences‐United States, 2000–2008 Births.” Morbidity and Mortality Weekly Report 62 (5): 77. [PMC free article] [PubMed] [Google Scholar]
- American Academy of Pediatricians . 2012. “Breastfeeding and the Use of Human Milk.” Pediatrics 129 (3): e827–41. [DOI] [PubMed] [Google Scholar]
- American Academy of Pediatricians . 2015. “Breastfeeding Frequently Asked Questions” [accessed on September 15, 2015]. Available at https://www2.aap.org/breastfeeding/faqsBreastfeeding.html#70
- Anderson, A. K. , Damio G., Young S., Chapman D. J., and Perez‐Escamilla R.. 2005. “A Randomized Trial Assessing the Efficacy of Peer Counseling on Exclusive Breastfeeding in a Predominantly Latina Low‐Income Community.” Archives of Pediatrics & Adolescent Medicine 159 (9): 836–41. [DOI] [PubMed] [Google Scholar]
- Arenz, S. , Rückerl R., Koletzko B., and von Kries R.. 2004. “Breast‐Feeding and Childhood Obesity—A Systematic Review.” International Journal of Obesity 28 (10): 1247–56. [DOI] [PubMed] [Google Scholar]
- Armstrong, J. , and Reilly J. J.. 2002. “Breastfeeding and Lowering the Risk of Childhood Obesity.” The Lancet 359 (9322): 2003–4. [DOI] [PubMed] [Google Scholar]
- Baker, M. , and Milligan K.. 2008. “Maternal Employment, Breastfeeding, and Health: Evidence from Maternity Leave Mandates.” Journal of Health Economics 27 (4): 871–87. [DOI] [PubMed] [Google Scholar]
- Bartick, M. , and Reinhold A.. 2010. “The Burden of Suboptimal Breastfeeding in the United States: A Pediatric Cost Analysis.” Pediatrics 125 (5): e1048–56. [DOI] [PubMed] [Google Scholar]
- Bonuck, K. A. , Trombley M., Freeman K., and McKee D.. 2005. “Randomized, Controlled Trial of a Prenatal and Postnatal Lactation Consultant Intervention on Duration and Intensity of Breastfeeding Up To 12 Months.” Pediatrics 116 (6): 1413–26. [DOI] [PubMed] [Google Scholar]
- Bullinger, L. R. , and Gurley‐Calvez T.. 2015. “WIC Participation and Maternal Behavior: Breastfeeding and Work Leave.” Contemporary Economic Policy 34 (1): 158–72. [Google Scholar]
- Casey, B. M. , McIntire D. D., and Leveno K. J.. 2001. “The Continuing Value of the Apgar Score for the Assessment of Newborn Infants.” New England Journal of Medicine 344 (7): 467–71. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention . 2012. Rates of Any and Exclusive Breastfeeding by Socio‐Demographics among Children Born in 2012. Washington, DC: Department of Health and Human Services. [Google Scholar]
- Chamberlain, L. B. , McMahon M., Philipp B. L., and Merewood A.. 2006. “Breast Pump Access in the Inner City: A Hospital‐Based Initiative to Provide Breast Pumps for Low‐Income Women.” Journal of Human Lactation 22 (1): 94–8. [DOI] [PubMed] [Google Scholar]
- Chatterji, P. , and Frick K. D.. 2005. “Does Returning to Work after Childbirth Affect Breastfeeding Practices?” Review of Economics of the Household 3 (3): 315–35. [Google Scholar]
- Chatterji, P. , Bonuck K., Dhawan S., and Deb N.. 2002. WIC Participation and the Initiation and Duration of Breastfeeding. Institute for Research on Poverty: University of Wisconsin—Madison. [Google Scholar]
- Claxton, G. , Rae M., Panchal N., Whitmore H., Damico A., and Kenward K.. 2014. “Health Benefits in 2014: Stability in Premiums and Coverage for Employer‐Sponsored Plans.” Health Affairs 33 (10): 1851–60. [DOI] [PubMed] [Google Scholar]
- Cohen, R. , and Mrtek M. B.. 1994. “The Impact of Two Corporate Lactation Programs on the Incidence and Duration of Breast‐Feeding by Employed Mothers.” American Journal of Health Promotion 8 (6): 436–41. [DOI] [PubMed] [Google Scholar]
- Cohen, R. J. , Haddix K., Hurtado E., and Dewey K. G.. 1995. “Maternal Activity Budgets: Feasibility of Exclusive Breastfeeding for Six Months among Urban Women in Honduras.” Social Science & Medicine 41 (4): 527–36. [DOI] [PubMed] [Google Scholar]
- Colen, C. G. , and Ramey D. M.. 2014. “Is Breast Truly Best? Estimating the Effects of Breastfeeding on Long‐Term Child Health and Wellbeing in the United States Using Sibling Comparisons.” Social Science & Medicine 109: 55–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Consumer Reports . 2013. “Breast Pump Buying Guide” [accessed on November 20, 2014]. Available at http://www.consumerreports.org/cro/breast-pumps/buying-guide.htm
- Currie, J. , and Schwandt H.. 2013. “Within‐Mother Analysis of Seasonal Patterns in Health at Birth.” Proceedings of the National Academy of Sciences of the USA 110 (30): 12265–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis, C. L. 2002. “Breastfeeding Initiation and Duration: A 1990‐2000 Literature Review.” Journal of Obstetric, Gynecologic, & Neonatal Nursing 31 (1): 12–32. [DOI] [PubMed] [Google Scholar]
- Evans, K. C. , Evans R. G., Royal R., Esterman A. J., and James S. L.. 2003. “Effect of Caesarean Section on Breast Milk Transfer to the Normal Term Newborn Over the First Week of Life.” Archives of Disease in Childhood—Fetal and Neonatal Edition 88 (5): F380–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evenhouse, E. , and Reilly S.. 2005. “Improved Estimates of the Benefits of Breastfeeding Using Sibling Comparisons to Reduce Selection Bias.” Health Services Research 40 (6 Pt 1): 1781–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forrestal, S. , Briefel R., and Mabli J.. 2015. WIC Breastfeeding Policy Inventory. Washington, DC: Mathematica Policy Research. [Google Scholar]
- Grossman, M. 1972. “On the Concept of Health Capital and the Demand for Health.” The Journal of Political Economy 80 (2): 223–55. [Google Scholar]
- Haider, S. J. , Chang L. V., Bolton T. A., Gold J. G., and Olson B. H.. 2014. “An Evaluation of the Effects of a Breastfeeding Support Program on Health Outcomes.” Health Services Research 49 (6): 2017–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins, S. S. , Stern A. D., and Gillman M. W.. 2013. “Do State Breastfeeding Laws in the USA Promote Breast Feeding?” Journal of Epidemiology and Community Health 67 (3): 250–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ip, S. , Chung M., Raman G., Chew P., Magula N., DeVine D., Trikalinos T., and Lau J.. 2007. “Breastfeeding and Maternal and Infant Health Outcomes in Developed Countries” Evidence Report/Technology Assessment No. 153 (prepared by Tufts‐New England Medical Center Evidence‐based Practice Center, under Contract No. 290‐02‐0022). AHRQ Publication No. 07‐E007. Rockville, MD: Agency for Healthcare Research and Quality. [PMC free article] [PubMed] [Google Scholar]
- Jacknowitz, A. , Novillo D., and Tiehen L.. 2007. “Special Supplemental Nutrition Program for Women, Infants, and Children and Infant Feeding Practices.” Pediatrics 119 (2): 281–9. [DOI] [PubMed] [Google Scholar]
- Janney, C. A. , Zhang D., and Sowers M.. 1997. “Lactation and Weight Retention.” The American Journal of Clinical Nutrition 66 (5): 1116–24. [DOI] [PubMed] [Google Scholar]
- Jegier, B. J. , Meier P., Engstrom J. L., and McBride T.. 2010. “The Initial Maternal Cost of Providing 100 mL of Human Milk for Very Low Birth Weight Infants in the Neonatal Intensive Care Unit.” Breastfeeding Medicine 5 (2): 71–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang, M. , Foster E. M., and Gibson‐Davis C. M.. 2010. “The Effect of WIC on Breastfeeding: A New Look at an Established Relationship.” Children and Youth Services Review 32 (2): 264–73. [Google Scholar]
- Joyce, T. , Racine A., and Yunzal‐Butler C.. 2008. “Reassessing the WIC Effect: Evidence from the Pregnancy Nutrition Surveillance System.” Journal of Policy Analysis and Management 27 (2): 277–303. [DOI] [PubMed] [Google Scholar]
- Kaiser Family Foundation . 2012. How is the Affordable Care Act Leading to Changes in Medicaid Today? State Adoption of Five New Options. Available at http://kaiserfamilyfoundation.files.wordpress.com/2013/01/8312.pdf [Google Scholar]
- Karlström, A. , Engström‐Olofsson R., Norbergh K.‐G., Sjöling M., and Hildingsson I.. 2007. “Postoperative Pain after Cesarean Birth Affects Breastfeeding and Infant Care.” Journal of Obstetric, Gynecologic, & Neonatal Nursing 36 (5): 430–40. [DOI] [PubMed] [Google Scholar]
- Kent, J. C. , Prime D. K., and Garbin C. P.. 2012. “Principles for Maintaining or Increasing Breast Milk Production.” Journal of Obstetric, Gynecologic, & Neonatal Nursing 41 (1): 114–21. [DOI] [PubMed] [Google Scholar]
- Kramer, M. S. 2010. ““Breast Is Best”: The Evidence.” Early Human Development 86 (11): 729–32. [DOI] [PubMed] [Google Scholar]
- Kramer, M. , Chalmers B., Hodnett E., Sevkovskaya Z., Dzikovich I., Shapiro S., Collet J.P., Vanilovich I., Mezen I., Ducruet T., and Shishko G., Zubovich V., Mknuik D., Gluchanina E., Dombrovskiy V., Ustinovitch A., Kot T., Bogdanovich N., Ovchinikova L., Helsing E. and PROBIT Study Group (Promotion of Breastfeeding Intervention Trial) . 2001. “Promotion of Breastfeeding Intervention Trial (Probit): A Randomized Trial in the Republic of Belarus.” JAMA 285 (4): 413‐20. [DOI] [PubMed] [Google Scholar]
- Mandal, B. , Roe B. E., and Fein S. B.. 2010. “The Differential Effects of Full‐Time and Part‐Time Work Status on Breastfeeding.” Health Policy 97 (1): 79–86. [DOI] [PubMed] [Google Scholar]
- Mannel, R. , and Mannel R. S.. 2006. “Staffing for Hospital Lactation Programs: Recommendations from a Tertiary Care Teaching Hospital.” Journal of Human Lactation 22 (4): 409–17. [DOI] [PubMed] [Google Scholar]
- Martin‐Anderson, S. 2013. “Prenatal Attitudes and Parity Predict Selection Into a US Child Health Program: A Short Report.” Social Science & Medicine 95: 128–32. [DOI] [PubMed] [Google Scholar]
- Meier, P. P. , Engstrom J. L., Janes J. E., Jegier B. J., and Loera F.. 2012. “Breast Pump Suction Patterns That Mimic the Human Infant During Breastfeeding: Greater Milk Output in Less Time Spent Pumping for Breast Pump‐Dependent Mothers with Premature Infants.” Journal of Perinatology 32 (2): 103–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merewood, A. , Philipp B. L., Chawla N., and Cimo S.. 2003. “The Baby‐Friendly Hospital Initiative Increases Breastfeeding Rates in a US Neonatal Intensive Care Unit.” Journal of Human Lactation 19 (2): 166–71. [DOI] [PubMed] [Google Scholar]
- National Women's Law Center . 2015. State of Breastfeeding Coverage: Health Plan Violations of the Affordable Care Act. Washington, DC: National Women's Law Center. [Google Scholar]
- Olson, C. , Strawderman M., Hinton P., and Pearson T.. 2003. “Gestational Weight Gain and Postpartum Behaviors Associated with Weight Change from Early Pregnancy to 1 y Postpartum.” International Journal of Obesity and Related Metabolic Disorders: Journal of the International Association for the Study of Obesity 27 (1): 117–27. [DOI] [PubMed] [Google Scholar]
- Olson, B. H. , Haider S. J., Vangjel L., Bolton T. A., and Gold J. G.. 2010. “A Quasi‐Experimental Evaluation of a Breastfeeding Support Program for Low Income Women in Michigan.” Maternal and Child Health Journal 14 (1): 86–93. [DOI] [PubMed] [Google Scholar]
- Østbye, T. , Peterson B., Krause K., Swamy G., and Lovelady C.. 2012. “Predictors of Postpartum Weight Change among Overweight and Obese Women: Results from the Active Mothers Postpartum study.” Journal of Women's Health 21 (2): 215–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pugh, L. C. , Milligan R. A., Frick K. D., Spatz D., and Bronner Y.. 2002. “Breastfeeding Duration, Costs, and Benefits of a Support Program for Low‐Income Breastfeeding Women.” Birth 29 (2): 95–100. [DOI] [PubMed] [Google Scholar]
- Ranji, U. , Salganicoff A., Stewart A., Cox M., and Doamekpor L.. 2009. State Medicaid Coverage of Perinatal Services: Summary of State Survey Findings. Washington, DC: Kaiser Family Fouundation. [Google Scholar]
- Roe, B. , Whittington L. A., Fein S. B., and Teisl M. F.. 1999. “Is There Competition between Breast‐Feeding and Maternal Employment?” Demography 36 (2): 157–71. [PubMed] [Google Scholar]
- Ruhm, C. J. 2000. “Parental Leave and Child Health.” Journal of Health Economics 19 (6): 931–60. [DOI] [PubMed] [Google Scholar]
- Ryan, A. S. , and Zhou W.. 2006. “Lower Breastfeeding Rates Persist Among the Special Supplemental Nutrition Program for Women, Infants, and Children Participants, 1978‐2003.” Pediatrics 117 (4): 1136–46. [DOI] [PubMed] [Google Scholar]
- Schwarz, E. B. , Ray R. M., Stuebe A. M., Allison M. A., Ness R. B., Freiberg M. S., and Cauley J. A.. 2009. “Duration of Lactation and Risk Factors for Maternal Cardiovascular Disease.” Obstetrics and Gynecology 113 (5): 974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slusser, W. M. , Lange L., Dickson V., Hawkes C., and Cohen R.. 2004. “Breast Milk Expression in the Workplace: A Look at Frequency and Time.” Journal of Human Lactation 20 (2): 164–9. [DOI] [PubMed] [Google Scholar]
- Smith, J. , and Forrester R.. 2013. “Who Pays for the Health Benefits of Exclusive Breastfeeding? An Analysis of Maternal Time Costs.” Journal of Human Lactation 29 (4): 547–55. [DOI] [PubMed] [Google Scholar]
- Stuebe, A. M. , Rich‐Edwards J. W., Willett W. C., Manson J. E., and Michels K. B.. 2005. “Duration of Lactation and Incidence of Type 2 Diabetes.” Journal of American Medical Association 294 (20): 2601–10. [DOI] [PubMed] [Google Scholar]
- Zinaman, M. J. , Queenan J. T., Labbok M. H., Albertson B., and Hughes V.. 1992. “Acute Prolactin and Oxytocin Responses and Milk Yield to Infant Suckling and Artificial Methods of Expression in Lactating Women.” Pediatrics 89 (3): 437–40. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix SA1: Author Matrix.
Table S1: Regression Coefficients† from DD Estimation (Standard Errors in Parentheses).
Table S2: DD Results Using Alternative Comparison Groups.
Table S3: Regression Coefficients from Propensity Score Estimation: Dependent Variable = Source of Payment Is Private Health Insurance (Standard Errors in Parentheses).
Table S4: Adjusted Breastfeeding Rates by Payer, First Differences, DDs Using PSM Sample.


