Supplemental Digital Content is available in the text.
Abstract
Background:
Breast augmentation continues to be one of the most common surgical procedures performed by plastic surgeons. As implant options expand, controlling the numerous variables required for a successful result will prove increasingly challenging. The purpose of this study was to outline specific steps that can be taken during the patient consultation and during surgery to decrease complications and improve overall patient satisfaction and patient outcomes.
Methods:
A retrospective review of 494 consecutive patients who underwent primary augmentation mammaplasty performed by a single surgeon was undertaken. Surgical outcomes were recorded and compared with previously published results. Patient satisfaction was measured using the BREAST-Q Augmentation Module.
Results:
Patients were followed for an average of 6 months (range, 0–45 months). Of the 494 patients, 1.3% developed capsular contracture. Other complications included 0.6% asymmetry, 0.4% malposition, 0.2% hematoma, and 0.2% rippling. The median BREAST Q score for the patient's overall satisfaction with outcome was 86%. The median BREAST Q score for patient's satisfaction with the plastic surgeon, medical team, and office staff was 100% in each case. The median score for psychological well-being, physical well-being, and sexual well-being was 100%, 90%, and 88%, respectively.
Conclusions:
The system outlined in this study showed very low rates of complications and high scores for patient satisfaction. Following a system like this will become increasingly important as breast augmentation continues to become more popular, implant options continue to expand, and social media continues to be used by patients to share surgical experiences.
INTRODUCTION
Breast augmentation continues to be one of the most common procedures performed by plastic surgeons. According to the American Society of Plastic Surgeons, over 290,000 breast augmentation procedures were performed in 2016.1 It has increased almost 40% since 2000 and the trend predicts it will increase in the future.
As the procedure continues to become more popular, it is imperative that plastic surgeons continue to strive to improve patient outcomes. It is now easy, and commonplace, for results to be scrutinized in the public eye due to the popularity of social media and review sites. These platforms have become a source of medical information and the combination of them, with surgeon reviews, drive up patient expectations. As implant options expand, patient expectations rise, and surgical experiences are shared online, controlling the numerous variables required for a successful result will prove increasingly challenging.
Multiple investigators have looked at improving surgical outcomes.2,3 Other investigators have looked at patient satisfaction after breast augmentation.4 Several authors have focused on patient education during the consultation to achieve improved patient outcomes.5–8
In contrast, there are very few studies to date that provide a comprehensive review of consultation practices and surgical steps that can be taken to improve both surgical outcomes and patient satisfaction after breast augmentation. This is an important issue since it is well known that patients may not be satisfied with their outcome, even when there are no surgical complications. Furthermore, there are no published studies that correlate patient satisfaction, as measured by the BREAST-Q questionnaire, with specific consultation practices.
The purpose of this study was to outline specific steps that can be taken during the patient consultation and during surgery to decrease complications and improve overall patient satisfaction and patient outcomes. Surgical outcomes were recorded and compared with previously published results for comparison. Patient satisfaction was then measured using the BREAST-Q augmentation module.
PATIENTS AND METHODS
This retrospective study includes 494 consecutive patients who underwent primary augmentation mammaplasty within a single surgeon’s practice from 2012 to 2015. Only data from patients who underwent a cosmetic primary breast augmentation and had at least 1 year minimum follow-up were included for analysis. Those who had concomitant mastopexy or secondary breast augmentation surgery were excluded. All 494 patients received implants manufactured by Allergan, Inc., (Irvine, Calif.).
All charts were reviewed for demographic data, incision location, pocket selection, implant type, length of follow-up, postoperative complications, total reoperation and implant-specific reoperation rates. Implant-specific reoperations included Baker grade III/IV capsular contracture, rippling, and implant rupture. Total reoperation rates include implant-specific causes in addition to hematoma, infection, asymmetry, ptosis, scarring, elective size change, and elective style change.
BREAST-Q questionnaires were used to evaluate patient satisfaction after breast augmentation. Development and validation of the BREAST-Q has been reported previously.9–12 Questionnaires were sent to patients operated on between January 12, 2012, and May 21, 2014. Patients operated on after May 21, 2014, were excluded to ensure that all questionnaire results would represent patients who had a minimum of 1 year follow-up before analysis. A total of 404 questionnaires were sent.
During the initial consultation, all implant options for surface texture, fill, and style/profile were reviewed, and the advantages and disadvantages of each were discussed in detail with the patient.
Once an implant style was selected, biodimensional planning was accomplished using a modified version of the High Five Decision Support Process as described by Tebbetts and Adams.13 From January 23, 2013, to December 20, 2014, all consecutive patients who underwent primary breast augmentation also underwent imaging with Vectra (Canfield Scientific Inc., Fairfield, N.J.) imaging system. The author captured all Vectra images to ensure consistency. 3D simulations for each volume option were created. The final volume of the implant was then chosen by the patient based on this overall analysis (Fig. 1).
Fig. 1.

Typical simulation created by 3D imaging. Patients can view simulations of proposed implant results from all angles. Images courtesy of Canfield Scientific Inc., N.J.
The 3D images were then reviewed with the patient to discuss potential implications of asymmetries in breast size, nipple position, inframammary fold (IMF) position and ribcage contour on the final result. The amount of preoperative and predicted postoperative breast gap was also specifically addressed.
The advantages and disadvantages of all implant placement and incision location options were then discussed. All patients were advised to undergo a partial subpectoral implant placement through an inframammary incision.
A detailed description of the operative day and recovery process was then reviewed with the patient.
All procedures were performed by the author. General anesthesia was used in all cases. A dose of prophylactic antibiotics was given before surgery.
Optimal IMF location is determined using a physical maneuver. Downward pressure is applied to the breast mound, and this accurately predicts the neo-IMF. This technique has been previously described by Hammond14 (see video, Supplemental Digital Content 1, which demonstrates the design of the IMF incision and the initial dissection. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A562).
Video 1.
See video, Supplemental Digital Content 1, which demonstrates the design of the IMF incision and the initial dissection. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A562.
An IMF or periareolar incision was used in all cases. The lateral border of the pectoralis muscle was identified and elevated. The submuscular dissection is initiated by entering the space between the pectoralis muscle and the serratus anterior muscle (Fig. 2; see video, Supplemental Digital Content 2, which demonstrates dissection with preservation of IMF fibers. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A563; see video, Supplemental Digital Content 3, which demonstrates exposure of lateral border of pectoralis muscle. Creation of submuscular plane. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A564).
Fig. 2.
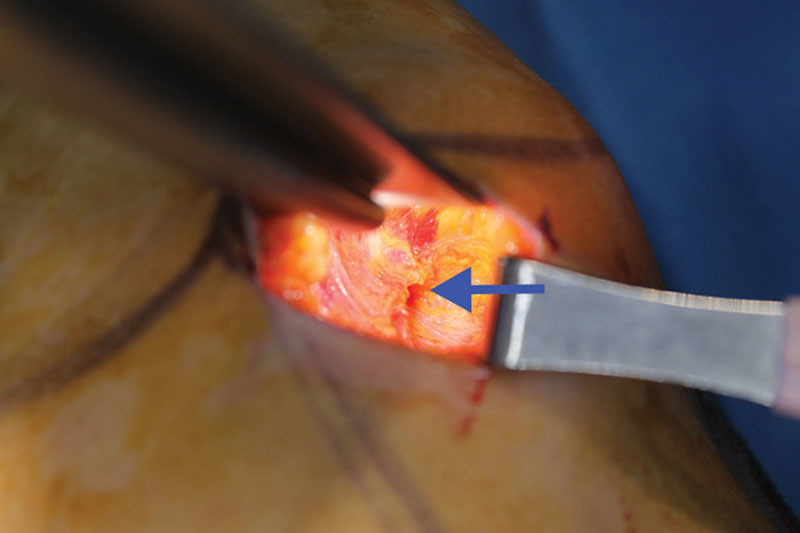
View of left breast, inframammary approach. The arrow points to the lateral border of the pectoralis muscle, which has been elevated. Blunt dissection is used to enter the space and create a pocket.
Video 2.

See video, Supplemental Digital Content 2, which demonstrates dissection with preservation of IMF fibers. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A563.
Video 3.

See video, Supplemental Digital Content 3, which demonstrates exposure of lateral border of pectoralis muscle. Creation of submuscular plane. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A564.
The inferior and inferomedial attachments of the pectoralis muscle were then divided using electrocautery under direct visualization (see video, Supplemental Digital Content 4, which demonstrates division of inferior and inferior medial attachments of the pectoralis muscle. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A565).
Video 4.

See video, Supplemental Digital Content 4, which demonstrates division of inferior and inferior medial attachments of the pectoralis muscle. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A565.
Sizers were used in all cases. The same surgical principles were applied to all implant types, including smooth, round, and textured anatomical implants. Pocket preparation included the use of triple antibiotic solution irrigation and reprepping the breast skin with betadine before implant placement. All implants were placed using a “No Touch” technique. An implant sleeve (Keller Funnel, Keller Medical, Florida) was used in all silicone breast implant augmentations (see video, Supplemental Digital Content 5, which demonstrates insertion of implants. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A566).
Video 5.

See video, Supplemental Digital Content 5, which demonstrates insertion of implants. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A566.
Once the implants have been inserted, the patient is then placed in a sitting position and the breasts are examined. (see video, Supplemental Digital Content 6, which demonstrates examination in the sitting position. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A567). Incision closure was performed in 2 layers using a deep subdermal suture (3-0 Monocryl; Ethicon) and a subcuticular skin closure (3-0 Monocryl; Ethicon).
Video 6.

See video, Supplemental Digital Content 6, which demonstrates examination in sitting position. This video is available in the “Related Videos” section of PRSGlobalOpen.com or at http://links.lww.com/PRSGO/A567.
Postoperatively Steri-StripTM (3M Health Care, St. Paul, Minn.) are maintained for 1 week. After 1 week, Steri-Strips are removed. Patients are placed in a soft bra and are advised to avoid an under-wire bra for 4 weeks. Light aerobic activity can be started at 1 week, nonchest weights at 2 weeks, and chest/sit-ups at 4 weeks.
Multiple postoperative appointments are scheduled at 1 week, 4 weeks, 3 months, 6 months, and 1 year. Patients are given ample time to ask questions and review concerns at each visit. The author saw all patients at all visits.
Patients who underwent breast augmentation between January 12, 2012, and May 21, 2014, were asked to complete the BREAST-Q augmentation module postoperatively. Patients operated on after May 21, 2014, were excluded from the questionnaire to ensure at least 1 year follow-up before analysis. Each patient was sent a questionnaire booklet by mail, with a self-addressed, postage-paid return envelope. Patients who did not respond to the mailed version of the questionnaire were then sent an electronic version of the questionnaire via e-mail. The electronic version of the survey was conducted online using the Survey Monkey Web site.
Patient responses to the BREAST-Q questionnaire were then evaluated. Patient scores were then transformed into quantitative measurements using the Q-Score program and presented on a 0–100 scale, with higher values representing greater satisfaction.
Relevant data were compiled and analyzed by an independent statistician. Descriptive statistics were calculated for continuous variables (i.e., mean, SD, median, interquartile range, minimum, and maximum) and categorical variables (i.e., number and frequency).
Patient characteristics and implant properties of the cohort were summarized. Complication rates and reoperation rates were reported as total reoperation rates and implant-specific reoperation rates. Implant-specific reoperation rates included capsular contracture, rippling, hematoma, infection, implant malposition, asymmetry. Time to complication was defined as time from initial surgery to occurrence of complication. Time to reoperation was defined as time from initial surgery to reoperation. Because of nonnormal distribution of BREAST-Q scores, the median score was used and SD given.
RESULTS
This study includes 494 primary breast augmentation patients who received a total of 988 implants. Patients had their primary operation between January 12, 2012, and December 20, 2014, and were followed for an average of 6 months (range, 0–45 months; Fig. 3).
Fig. 3.
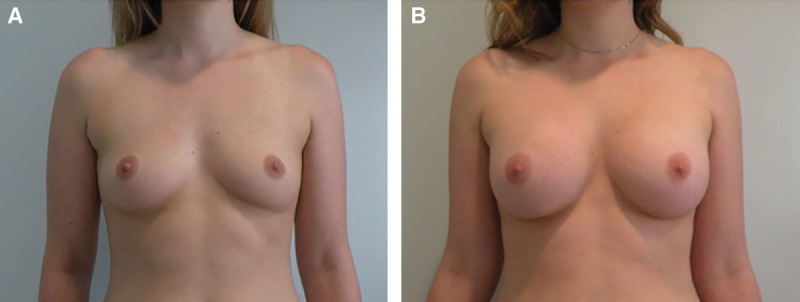
This 26-year-old woman underwent primary breast augmentation. Allergan, Style 15 implants measuring 339 cc in volume were used bilaterally. Implants were inserted through an inframammary approach. Implants were placed in a submuscular plane. Pictures were taken 6 months postoperatively.
The majority of patients had round, silicone implants [n = 277 (56%)]. Two hundred five patients had saline implants (41.5%), and 12 patients had shaped implants (2.5%; Fig. 4). All round implants were smooth. No round textured devices were used.
Fig. 4.
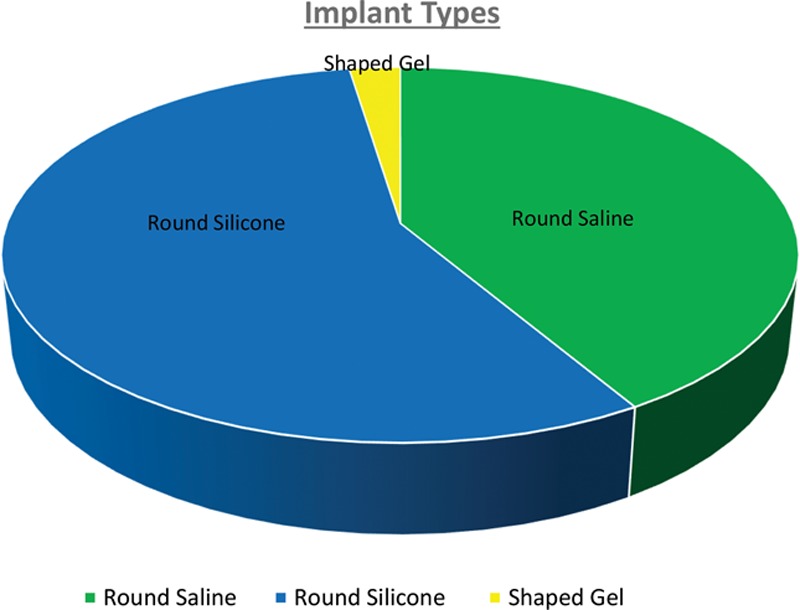
Types of implants used.
The average implant size was 380 cc. (range, 176–700 cm3). Implant volume distribution is illustrated in Figure 5.
Fig. 5.
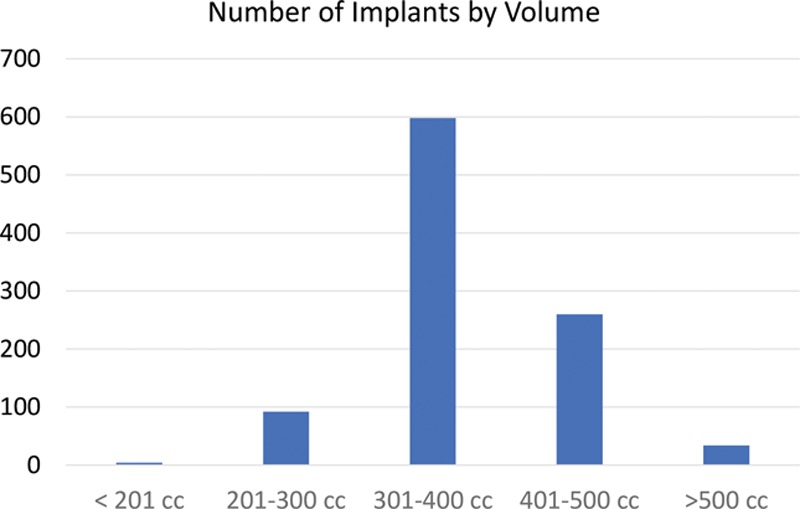
Number of implants by volume.
The majority of patients had their implants placed through an IMF incision [n = 454 (92%)] with the remainder being placed through a periareolar incision [n = 40 (8%)].
Subpectoral pockets were used in all patients. All subpectoral cases refer to dual-plane I as described by Tebbetts15, as this is the author’s standard approach.
A total of 12 patients (2.5%) experienced complications, of which Baker stage III/IV capsular contracture [n = 6 (1.3%)] was the most common. This was followed by asymmetry [n = 3 (0.6%)], implant malposition [n = 2 (0.4%)], and hematoma [n = 1 (0.2%)]. There were no seromas, infections, wound dehiscence, or implant rotation in this patient cohort (Table 1).
Table 1.
Summary of Complications
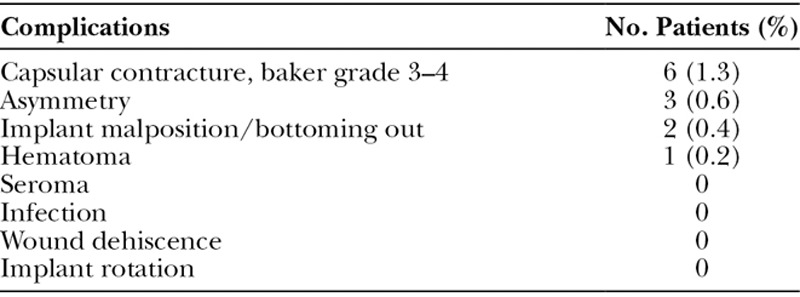
A total of 13 patients (2.7%) underwent reoperation. Of the patients who underwent reoperation, the most common reason for reoperation was capsular contracture (n = 5). The remainder were due to dissatisfaction with size (n = 3), implant malposition/bottoming out (n = 2), asymmetry (n = 2), and hematoma (n = 1). Average length of time from surgery to reoperation was 11 months (range = 1 week to 25 months).
Four hundred two patients were sent BREAST-Q questionnaires. Ninety-two patients were excluded to avoid analysis of patients with less than 1 year of follow-up. One hundred fifty of 402 patients (37%) who received questionnaires completed the postoperative survey.
BREAST-Q scores ranged from 0 to 100, with higher scores indicating a greater quality of life. Due to the nonnormal, left skewed distribution of BREAST-Q scores, the median score was used.
The median BREAST-Q score for psychosocial well-being was 100, with an SD of 16.5. The mean score was 89.1 (Fig. 6). The median BREAST-Q score for physical well-being was 90, with an SD of 13.5. The mean score was 86.7 (Fig. 7). The median BREAST-Q score for sexual well-being was 100, with an SD of 17.8. The mean score was 88 (Fig. 8).
Fig. 6.
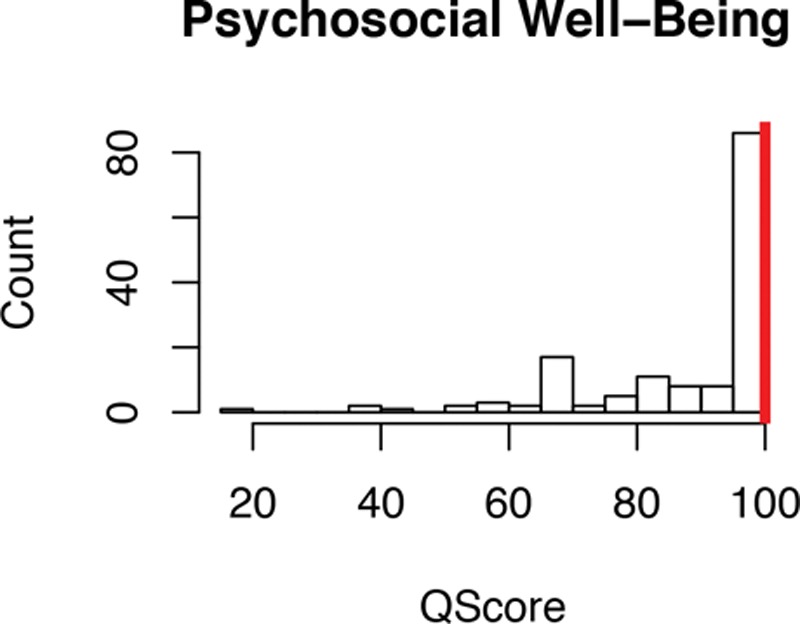
“Psychosocial Well-Being” BREAST-Q score. Median score represented by red bar.
Fig. 7.
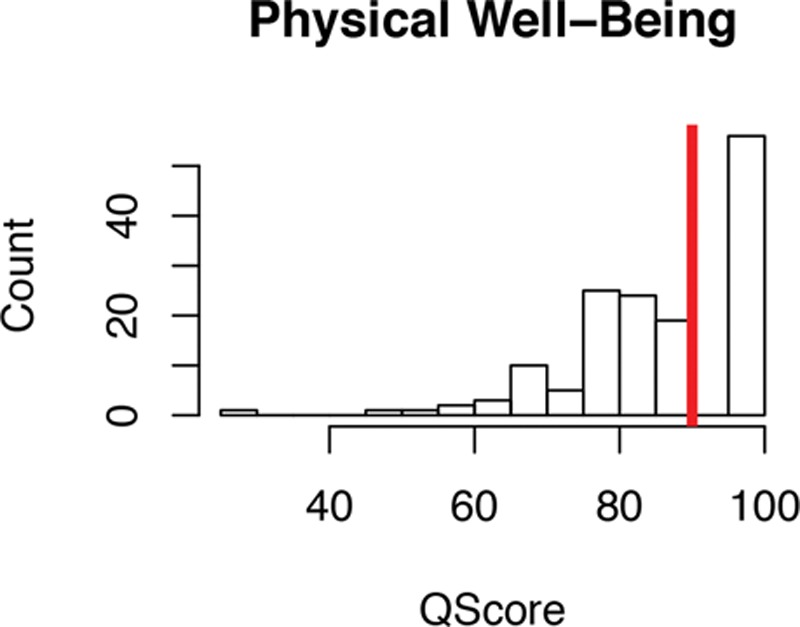
“Physical Well Being” BREAST-Q score. Median score represented by red bar.
Fig. 8.
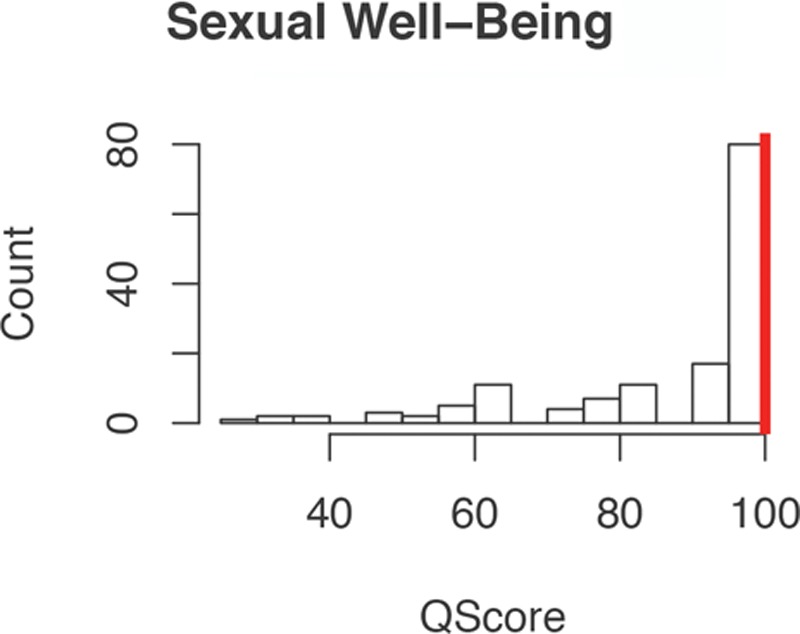
“Sexual Well Being” BREAST-Q Score. Median score represented by red bar.
The median BREAST-Q score for satisfaction with breast was 80, with an SD of 15.1. The mean score was 80.6 (Fig. 9). The median BREAST-Q score for satisfaction with outcome was 86, with an SD of 19.2. The mean score was 83.4 (Fig. 10).
Fig. 9.
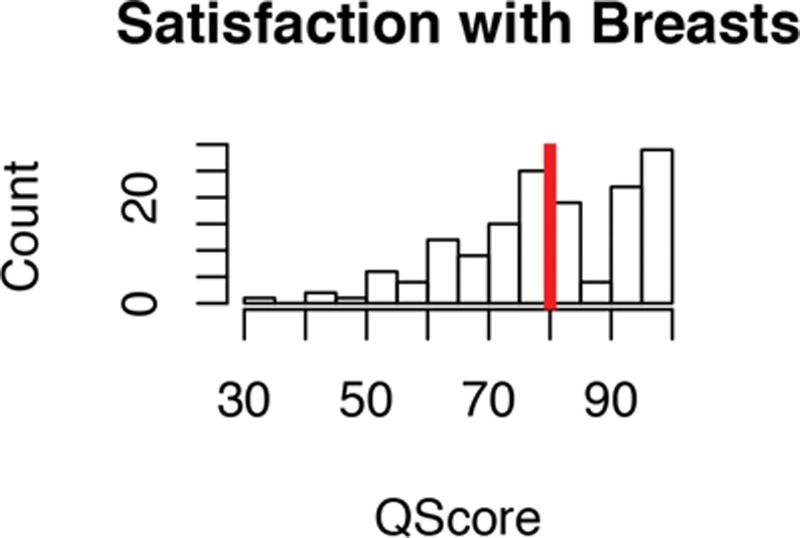
“Satisfaction with Breasts” BREAST-Q Score. Median score represented by red bar.
Fig. 10.
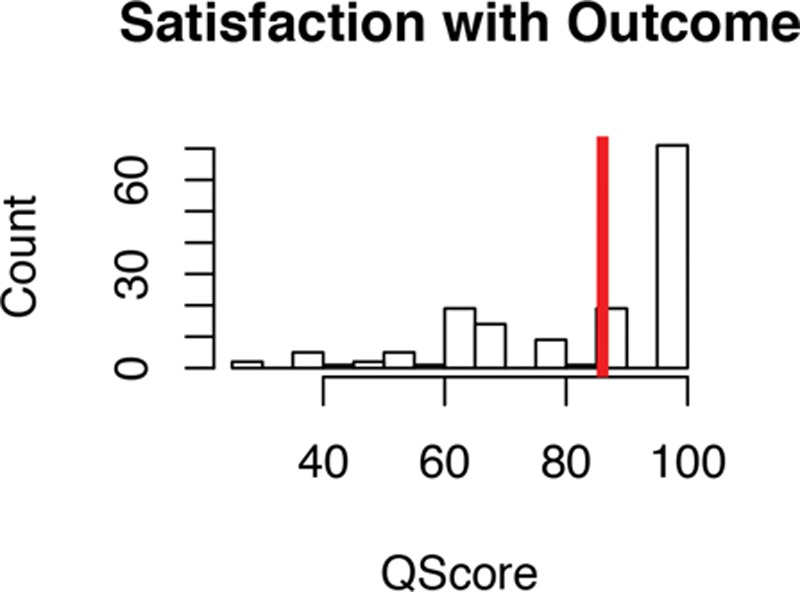
“Satisfaction with Outcome” BREAST-Q Score. Medial score represented by red bar.
Satisfaction with Care is subcategorized into 4 subscales; Satisfaction with Information, Satisfaction with Plastic Surgeon, Satisfaction with Medical Team, and Satisfaction with Office Staff. The median score for Satisfaction with Information was 91, with an SD of 17.7. The mean score was 85.5. The median score for Satisfaction with Plastic Surgeon was 100, with an SD of 13.4. The mean score was 95.2. The median score for Satisfaction with Medical Team was 100, with an SD of 11.7. The mean score was 97. Lastly, the median score for Satisfaction with Office Staff was 100, with an SD of 8.7. The mean score was 98.8 (Figs. 11–14).
Fig. 11.
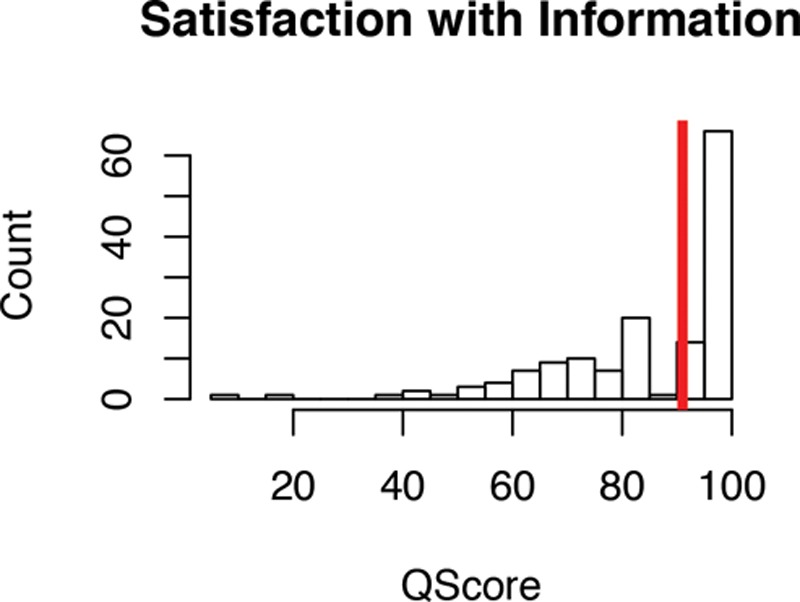
“Satisfaction with Information” BREAST-Q Score. Median score represented by red bar.
Fig. 14.
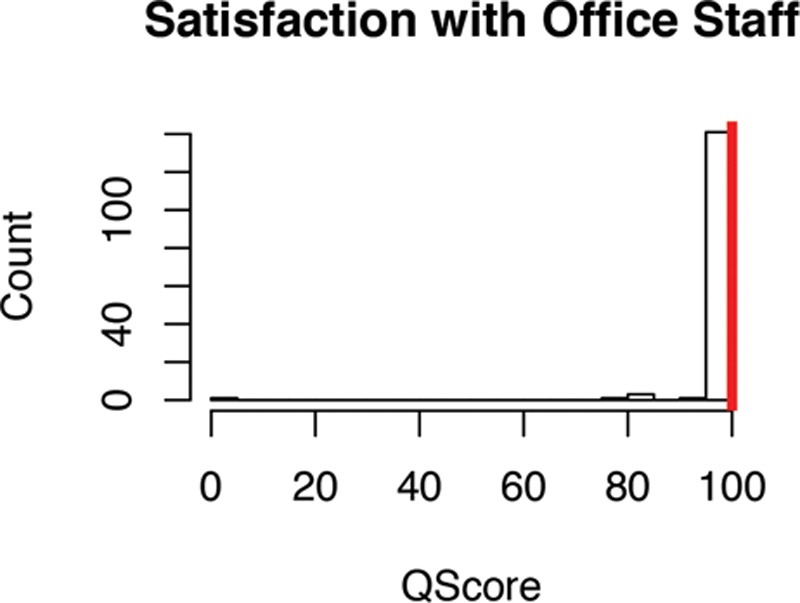
“Satisfaction with Office Staff” BREAST-Q score. Median score represented by red bar.
Fig. 12.
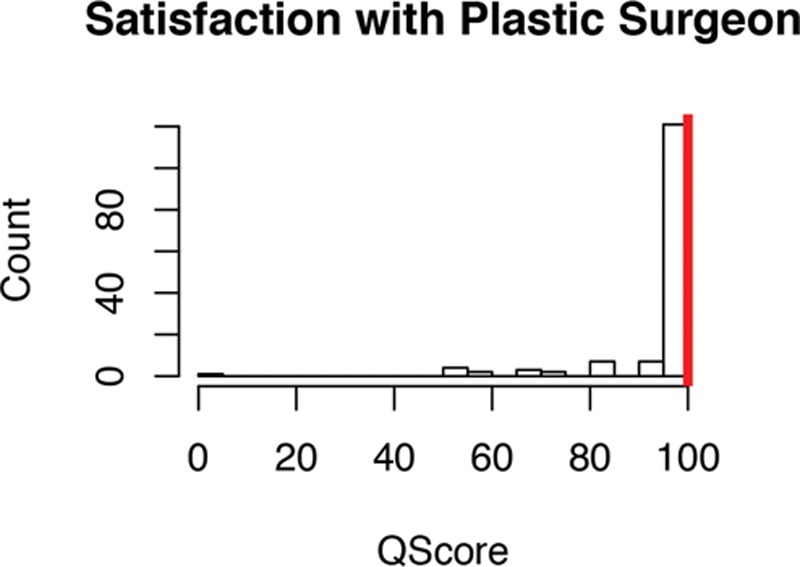
“Satisfaction with Plastic Surgeon” BREAST-Q score. Median score represented by red bar.
Fig. 13.
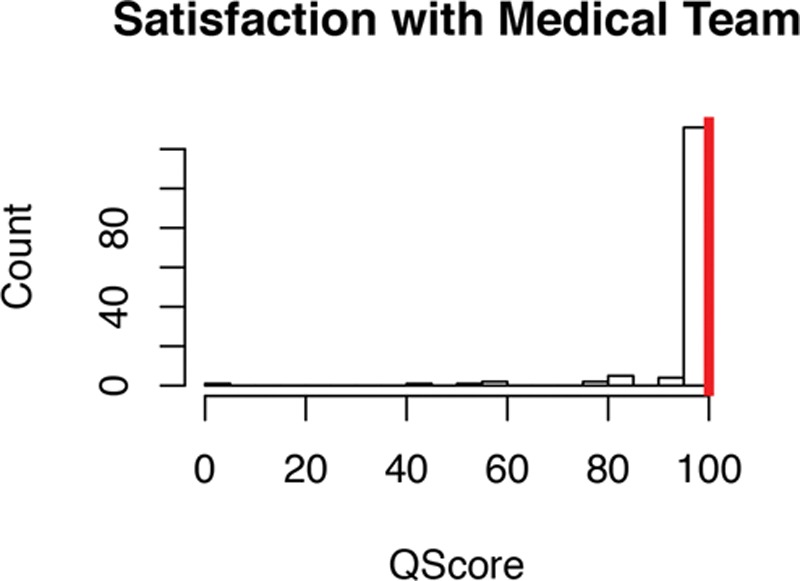
“Satisfaction with Medical Team” BREAST-Q score. Median score represented by red bar.
DISCUSSION
This study outlines a specific system that can be followed to reduce surgical and implant-specific complications and increase patient satisfaction. This developed from an evolution in thinking over the last decade inspired by leaders such as Tebbetts and Adams.13 As a result, the author implemented the following system consistently for the past several years:
Extensive preoperative patient education
Biodimensional planning for implant selection
Preoperative 3D imaging
Use of an inframammary approach
Meticulous pocket dissection
Submuscular placement
Antibiotic irrigation and use of an implant sleeve
Multiple regular postoperative appointments
This system is described in detail in Supplemental Digital Content 7 (see appendix, Supplemental Digital Content 7, which demonstrates the author’s surgical approach to primary breast augmentation, http://links.lww.com/PRSGO/A568).
The most common implant-specific complication in this study was capsular contracture. The incidence in this study was 1.3%. Other studies of primary breast augmentation show rates ranging from 0% to 15%.2,16
Although the exact cause of capsular contracture remains unknown, factors such bacterial contamination, biofilm, tissue trauma, blood, and silicone bleed are thought to contribute to its formation.17–20 Therefore, significant attention has been given to the role that incision location, implant placement, surgical technique, and implant characteristics may play in the development of capsular contracture.
All patients received extensive preoperative education about the risks and benefits of each incision option. The inframmary approach was strongly encouraged in all cases. The periareolar incision was used only if the patient insisted on this location after being informed of all risks, benefits, and alternatives. The inframammary incision was used in 92% of patients. It is believed that the use of the inframammary incision decreased the risk of capsular contracture. This is supported by previous studies.21
All patients had implants placed in the subpectoral plane. The pocket was created initially using blunt dissection to enter the space between the pectoralis muscle and the serratus anterior muscle laterally. Further dissection is performed under direct visualization with special attention on vessel cauterization. It is believed that this approach markedly decreases bleeding and the risk of hematoma.
Antibiotic irrigation was used in all cases. In vitro and clinical studies support the use of antibiotic solution to prevent the growth of common breast implant organisms.22,23 Triple antibiotic breast irrigation is recommended as an adjunctive technique to prevent capsular contracture.
When examining implant characteristics, there were no significant differences in complications based on implant fill material, implant fill volume, surface texture, or shape. Of note is that all round saline and gel-filled implants used were smooth surface devices. The lack of a significant difference between these variables is likely due to the overall low number of complications. However, this does suggest that implant surface texture may not play as important a role in preventing capsular contracture or other complications as once thought, especially if a meticulous surgical technique is used.
Using a “No Touch” technique has been shown to decrease the risk of capsular contracture.24 In this study, an implant sleeve was used in all silicone breast augmentation cases. The implant sleeve facilitated the use of a “No Touch” technique. Previous studies suggest that use of a Keller funnel results in a 27-fold decrease in skin contact and makes bacterial contamination less likely.25
Other complications such as asymmetry, implant malposition, and bottoming out were all lower than 1%. There was a 0% incidence of seroma, infection, or implant rotation.
Rippling is a well-known and well-described finding after breast augmentation.7 Animation deformity is also a well-known and well-described complication after augmentation in the submuscular plane.26 These complications were not included in the analysis.
The reoperation rate in this study was 2.7%. Self reported reoperation rates of American Society of Plastic Surgeons members range from 1% to 5%.27 Long-term studies show higher reoperation rates.28 As with most studies, the most common cause of reoperation was capsular contracture. The low overall rate of reoperation is likely due to both the low overall rate of complications and the relatively short average follow-up period in this study.
Dissatisfaction with size and elective size change are major causes of reoperation.28 In one long term study, the rate of reoperation for elective size change was 4%.29 In this study, elective size change occurred in 1% of patients and was the second most common cause of reoperation. It is believed that this low rate is attributable to the extensive preoperative consultation and patient education process. Specifically, the advantages and disadvantages of every option for surface texture, implant fill, and implant shape are discussed during the consultation. Biodimensional planning is used along with patient-specific goals to narrow the options for implant type and volume. 3D imaging is then used to simulate the surgical result. Patients select the final implant choice based on these simulations. Studies have shown that patients are satisfied with the accuracy of 3D simulations and with the size of the implant selected based on these simulations30 (Fig. 15).
Fig. 15.

This is a 22-year-old woman who underwent primary breast augmentation. The left image is the preoperative photograph. The image in the middle is the 3D simulation with Allergan Style 15 silicone implants measuring 339 cm3 placed in the submuscular plane. The image on the right is the postoperative photograph taken at 3 months.
3D imaging is also invaluable when educating patients about potential asymmetries in nipple position, IMF position, breast size, and breast shape. It also allows for clear communication about the breast gap and facilitates discussion. The use of 3D imaging has emerged as an essential tool to educate patients preoperatively about these important issues.
It is believed that all the steps taken during the consultation and during surgery ensure a high level of success regarding patient satisfaction with their breasts and overall result. This was supported by data from the BREAST-Q questionnaire. Patients reported high satisfaction rates with the breasts (80%) and with the outcome (86%). They also reported high satisfaction with psychosocial well-being (100%), sexual well-being (100%), and physical well-being (90%).
Providing extensive preoperative and postoperative patient guidance and education has further benefits. It is widely known that patients may have a satisfactory surgical result, but still be dissatisfied with the care provided by the surgeon, the office and/or his or her staff. It is believed that the quality of the information provided before, during, and after the consultation achieved high patient satisfaction rates in these areas. When asked about their satisfaction with the information provided to them, the median score was 91%. When asked about their satisfaction with the care provided by the plastic surgeon, medical team, and office staff, patients reported scores of 100% in each case. As patients continue to share their surgical experiences on review sites and other social media platforms, implementing systems to ensure high patient satisfaction rates in these areas will continue to grow in importance.
LIMITATIONS
This is a retrospective review of 1 surgeon’s experience. Reviewing a retrospective database may underestimate complication rates due to patients being lost to follow-up. Patients who may have moved or may have presented to other surgeons for revision will not be captured for analysis. Another limitation is that this study measured complication rates using patient-based outcomes rather than implant-based outcomes. Thus, results from this study cannot be compared with results from studies based on implant outcomes. Furthermore, conclusions based on implant surface, fill, and shape characteristics are limited.
Overall, postoperative assessment with the BREAST-Q score showed high patient scores in overall outcomes and quality of life measures. Due to the retrospective study design, preoperative BREAST-Q augmentation modules were not completed before the study. Although the postoperative version also includes all preoperative items, patient completion of the preoperative version before surgery would allow changes in satisfaction to be measured. This could have provided further insights into patient outcomes.
Lastly, this study represents a very narrow group of breast augmentation patients. The vast majority of patients in this study underwent augmentation with round, smooth silicone implants from a single manufacturer using an inframammary approach and submuscular placement. Also, difficult cases such as tuberous breasts, constricted breasts, and short nipple to IMF distances were not included. Therefore, the data used cannot be extrapolated to these patients or patients undergoing other techniques.
CONCLUSIONS
Developing and implementing a detailed system in patient education, implant selection, surgical technique, and postoperative care is paramount for optimizing outcomes with low complication and reoperation rates. It is also critical for achieving higher rates of patient satisfaction. Most studies focus on implant-related complications and/or surgical outcomes. Few studies have looked at patient education and/or patient satisfaction in breast augmentation. Fewer studies look at both. This study outlines a comprehensive system of steps taken during the consultation, during surgery, and during the postoperative period to improve outcomes.
Following a system, like the one described here, will become increasingly important as breast augmentation continues to become more popular, implant options continue to expand and social media continues to be used by patients to share surgical experiences.
ACKNOWLEDGMENTS
The author thanks William J. Rahal, MD, for his support in medical writing and data analysis. The author acknowledges Kayla M. Frisoli, M. Stat., for her help in statistical analysis of the data.
Supplementary Material
Footnotes
Disclosure: The author has no financial interest to declare in relation to the content of this article. The Article Processing Charge was paid for by the author.
Supplemental digital content is available for this article. Clickable URL citations appear in the text.
REFERENCES
- 1.American Society of Plastic Surgeons (ASPS) Statistics. Web. https://www.plasticsurgery.org/documents/News/Statistics/2016/cosmetic-procedure-trends-2016.pdf Accessed September 22, 2017.
- 2.Tebbets JB. Achieving a zero percent reoperation rate at 3 years in a 50-consecutive-case augmentation mammaplasty premarket approval study. Plast Reconstr Surg. 2006;118:1453–1457.. [DOI] [PubMed] [Google Scholar]
- 3.Somogyi RB, Brown MH. Outcomes in primary breast augmentation: a single surgeon’s review of 1539 consecutive cases. Plast Reconstr Surg. 2015;135:87–97.. [DOI] [PubMed] [Google Scholar]
- 4.McCarthy CM, Cano SJ, Klassen AF, et al. The magnitude of effect of cosmetic breast augmentation on patient satisfaction and health-related quality of life. Plast Reconstr Surg. 2012;130:218–223.. [DOI] [PubMed] [Google Scholar]
- 5.Tebbetts JB, Tebbetts TB. An approach that integrates patient education and informed consent in breast augmentation. Plast Reconstr Surg. 2002;110:971–978.; discussion 979. [DOI] [PubMed] [Google Scholar]
- 6.Hedén P, Montemurro P, Adams WP, Jr, et al. Anatomical and round breast implants: how to select and indications for use. Plast Reconstr Surg. 2015;136:263–272.. [DOI] [PubMed] [Google Scholar]
- 7.Adams WP, Jr, Mallucci P. Breast augmentation. Plast Reconstr Surg. 2012;130:597e–611e.. [DOI] [PubMed] [Google Scholar]
- 8.Adams WP., Jr. The process of breast augmentation: four sequential steps for optimizing outcomes for patients. Plast Reconstr Surg. 2008;122:1892–1900.. [DOI] [PubMed] [Google Scholar]
- 9.BREAST-Q. Available at https://webcore.mskcc.org/breastq/.
- 10.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353.. [DOI] [PubMed] [Google Scholar]
- 11.Pusic AL, Lemaine V, Klassen AF, et al. Patient-reported outcome measures in plastic surgery: use and interpretation in evidence-based medicine. Plast Reconstr Surg. 2011;127:1361–1367.. [DOI] [PubMed] [Google Scholar]
- 12.Pusic AL, Reavey PL, Klassen AF, et al. Measuring patient outcomes in breast augmentation: introducing the BREAST-Q augmentation module. Clin Plast Surg. 2009;36:23–32, v.. [DOI] [PubMed] [Google Scholar]
- 13.Tebbetts JB, Adams WP. Five critical decisions in breast augmentation using five measurements in 5 minutes: the high five decision support process. Plast Reconstr Surg. 2005;116:2005–2016.. [PubMed] [Google Scholar]
- 14.Hammond DC. Spear SL. Chapter 92: The Inframammary Approach to Augmentation Mammaplasty. In: Surgery of the Breast. 2006:2nd ed Philadelphia, PA; Lippincott, Williams & Williams; 1297–1303.. [Google Scholar]
- 15.Tebbetts JB. Dual plane breast augmentation: optimizing implant-soft-tissue relationships in a wide range of breast types. Plast Reconstr Surg. 2001;107:1255–1272.. [DOI] [PubMed] [Google Scholar]
- 16.Wan D, Rohrich RJ. Revisiting the management of capsular contracture in breast augmentation: a systematic review. Plast Reconstr Surg. 2016;137:826–841.. [DOI] [PubMed] [Google Scholar]
- 17.Ajdic D, Zoghbi Y, Gerth D, et al. The relationship of bacterial biofilms and capsular contracture in breast implants. Aesthet Surg J. 2016;36:297–309.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jacoby J, Lille ST. The role of pocket dissection in breast implant contracture: a single surgeon’s review. Plast Reconstr Surg. 2011;127:155e–156e.. [DOI] [PubMed] [Google Scholar]
- 19.Hipps CJ, Raju R, Straith RE. Influence of some operative and postoperative factors on capsular contracture around breast prostheses. Plast Reconstr Surg. 1978;61:384–389.. [DOI] [PubMed] [Google Scholar]
- 20.Caffee HH. The influence of silicone bleed on capsule contracture. Ann Plast Surg. 1986;17:284–287.. [DOI] [PubMed] [Google Scholar]
- 21.Wiener TC. Relationship of incision choice to capsular contracture. Aesthetic Plast Surg. 2008;32:303–306.. [DOI] [PubMed] [Google Scholar]
- 22.Adams WP, Jr, Conner WC, Barton FE, Jr, et al. Optimizing breast pocket irrigation: an in vitro study and clinical implications. Plast Reconstr Surg. 2000;105:334–338.; discussion 339. [DOI] [PubMed] [Google Scholar]
- 23.Adams WP, Jr, Rios JL, Smith SJ. Enhancing patient outcomes in aesthetic and reconstructive breast surgery using triple antibiotic breast irrigation: six-year prospective clinical study. Plast Reconstr Surg. 2006;117:30–36.. [PubMed] [Google Scholar]
- 24.Mladick RA. “No-touch” submuscular saline breast augmentation technique. Aesthetic Plast Surg. 1993;17:183–192.. [DOI] [PubMed] [Google Scholar]
- 25.Moyer HR, Ghazi B, Losken A. Sterility in breast implant placement: The Keller Funnel and the “No Touch” Technique. Plast Reconstr Surg. 2011; 128:9. [Google Scholar]
- 26.Spear SL, Schwartz J, Dayan JH, et al. Outcome assessment of breast distortion following submuscular breast augmentation. Aesthetic Plast Surg. 2009;33:44–48.. [DOI] [PubMed] [Google Scholar]
- 27.Choudry U, Kim N. Pre-operative assessment and reoperation rates in breast augmentation—a survey of ASPS members. Plast Reconstr Surg. 2011;128:10–11.. [DOI] [PubMed] [Google Scholar]
- 28.Codner MA, Mejia JD, Locke MB, et al. A 15-year experience with primary breast augmentation. Plast Reconstr Surg. 2011;127:1300–1310.. [DOI] [PubMed] [Google Scholar]
- 29.Becker H. Breast augmentation using the spectrum implant with exteriorized injection domes. Plast Reconstr Surg. 2004;114:1617–1620.; discussion 1621. [DOI] [PubMed] [Google Scholar]
- 30.Donfrancesco A, Montemurro P, Hedén P. Three-dimensional simulated images in breast augmentation surgery: an investigation of patients’ satisfaction and the correlation between prediction and actual outcome. Plast Reconstr Surg. 2013;132:810–822.. [DOI] [PubMed] [Google Scholar]


