Abstract
Purpose
Preoperative preparation for adrenalectomy for pheochromocytomas and paragangliomas (PPGL) is universally recognized as necessary, while the optimal strategy remains controversial. Our aims were to increase intraoperative hemodynamic stability, expedite postoperative recovery, decrease side effects and reduce costs for patients with PPGL undergoing adrenalectomy.
Methods
We identified 526 patients undergoing open adrenalectomy for PPGL in the West China Hospital of Sichuan University between May, 2007 and December, 2016. 149 patients received preoperative selective α-blockade with phenoxybenzamine, and 377 patients received non-selective α-blockade with prazosin, doxazosin or terazosin. There were no statistical differences between groups regarding preoperative patient and tumor characteristics. Operations were planned once hypertensive patients were well-controlled with blood pressure ≤130/85 mmHg. Intraoperatively, all patients received arterial blood pressure monitoring, and indwelling urinary catheters to record urine output. We recorded intraoperative hemodynamics, status in the postanesthesia or intensive care unit, postoperative recovery and complications.
Results
Patients in the non-selective group showed a more significant decline in postoperative systolic blood pressure than the selective group (P = 0.041). Also, patients in the non-selective group appeared to receive a long-term anti-hypertensive effect, especially for diastolic blood pressure (P = 0.037), which was a novel finding, based on the current literature.
Conclusions
Our results confirmed that non-selective α-blockade produced a more significant anti-hypertensive effect than selective α-blockade. However, we found no significant difference in intraoperative hemodynamic instability, postoperative recovery and postoperative complications between groups.
Keywords: PPGL, pheochromocytoma, adrenalectomy, preoperative preparation, selective α-blockade
Introduction
Pheochromocytomas and paragangliomas (PPGL) are rare catecholamine-secreting tumors with a low incidence of 0.8 per 100,000 individuals/year in the general population (1). However, the incidence among the hypertensive population is estimated to be 0.1%–0.6% (2). Based on the origin, PPGL can be categorized as pheochromocytomas arising from the adrenal medulla (85%) and paragangliomas arising from sympathetic or parasympathetic ganglia (15%) (3).
Because the release of catecholamine by PPGL is unpredictable and differs from person to person, the clinical presentation ranges from asymptomatic to life-threatening hypertensive crisis (4). Classic symptoms include episodic tachycardia, sweating, headache and signs of paroxysmal hypertension (5). Surgical resection, the only curative therapy, still carries a high intraoperative risk of causing massive catecholamine release into the circulation (6). This leads to a complex series of intraoperative hemodynamic instability issues during adrenalectomy for pheochromocytomas, including rapid and severe blood pressure fluctuations that greatly increase the risk of major morbidity (7). Anesthetic induction, intraoperative tumor handling and accidental squeezing of the tumor can instantly increase catecholamine release, resulting in severe intraoperative hypertensive crisis and potentially stroke, myocardial infarction and other severe complications (8).
Using α-blockade for preoperative medical preparation for adrenalectomy for PPGL has been universally recognized and advocated to decrease intraoperative hypertension by preventing binding of catecholamines with α1 receptors (9). Clinically, two types of α-blockade are widely used: selective and non-selective. The effects of non-selective α-blockade are irreversible, inhibiting both α1 and α2 receptors (10). Because new receptors are constantly being made, the effects of non-selective α-blockade do not last its half-life (24 h); therefore, patients must take the medication every 8–12 h (11). Also, non-selective α-blockade may cause side effects such as orthostatic hypotension, reflex tachycardia and nasal congestion because of the inhibition of α2 receptors (12).
Selective α-blockade competitively inhibits only α1 receptors, causing fewer side effects because most side effects are driven by the inhibition of α2 receptors (3). However, competitive inhibition can be overcome by high levels of catecholamines, especially when handling pheochromocytomas intraoperatively (13); therefore, the anti-hypertensive effect of selective α-blockade may not be as potent (1).
Several studies have evaluated the different effects of selective and non-selective α-blockade on intraoperative and postoperative hemodynamics (14); however, most studies have several limitations (15). Many studies have inadequate sample sizes of only dozens of patients in each group, while a more objective and comprehensive conclusion should be based on data from large sample sizes (16). Some studies are highly specialized and discuss laparoscopic adrenalectomy to provide a technique-specific conclusion (17, 18). However, open adrenalectomy, which is more widely used and recognized in China and many other countries, has not been specifically researched (19). Also, some unspecialized studies have considered only general patient and tumor conditions and produced only partial statistical results leading to biased conclusions (20).
According to statistical theory, large sample data can considerably reduce systematic error. Therefore, we divided all eligible patients into two groups to precisely compare the effects of selective and non-selective α-blockade from three aspects: intraoperative hemodynamic instability, side effects and continuous postoperative support demands (20). Conclusions based on this analysis could lead to individual preoperative preparation strategies for patients with disparate symptoms to increase intraoperative hemodynamic stability, expedite postoperative recovery, decrease side effects and reduce costs (21).
Material and methods
The study was approved by national clinical trials agencies – Sichuan University of West China Hospital GCP Center.
Consent has been obtained from each patient or subject after full explanation of the purpose and nature of all procedures used.
A previous study about preoperative preparation for laparoscopic adrenalectomy of pheochromocytoma has compared selective with non-selective α-blockade in multiple aspects. This study left us with quite a lot inspiration on research process and result analysis (20, 22). They emphasized that their study just evaluated the patients receiving laparoscopic adrenalectomy; thus, their theory may not be appropriate for patients undergoing open adrenalectomy (18). They also accentuated the significance of conducting the study in a single institution with similar and standardized strategy for preoperative preparation and operation. We carried out this research following the guidelines, making several adjustments to make it more suitable for Chinese patients.
Between May 2007 and December 2016, we received 743 cases of PPGL to be confirmed and operated in West China Hospital of Sichuan University. Aimed at obtaining valid data, we formulate the inclusion and exclusion criteria. The inclusion criteria are diagnosed with PPGL and undergoing adrenalectomy in our hospital; the exclusion criteria are pathological diagnosis negative for PPGL or discharging without surgery. After the filtration, 526 cases are included into the research, all of which underwent open adrenalectomy in West China Hospital.
To ensure the significance of cross-reference, all patient and tumor characteristics were examined in detail, especially intraoperative hemodynamics and postoperative performance between both groups (23). All intraoperative details are gathered from anesthesia record sheets to ensure getting the accurate information.
Almost all patients took preoperative medical preparation. On account of a different α-blockade strategy, patients were partitioned into two groups with similar characteristics. For non-selective α-blockade, we applied phenoxybenzamine as the only choice, which is universally used and generally recognized according to the previous researches. The initial dose was at the discretion of endocrinology doctors or the operating surgeon, always 10–15 mg tid. As for selective α-blockade, we use prazosin, doxazosin or terazosin, the initial dose was usually 5 mg, qd (9).
For a few uncontrollable hypertension patients, we applied drug combination of selective and non-selective α-blockade. Patients with evidence of preoperative tachycardia or arrhythmia were given β-blockade as preoperative preparation (24). Although it is recommended to provide a high-sodium diet and fluid intake to prevent postoperative hypotension according to the guideline for PPGL, we have not increased the salt content in the patients’ daily diet due to the dietary habit of Chinese, which provides an average salt intake of 11.8 ± 4.5 g/day (25).
Operation would be arranged when hypertensive patients has been steadily controlled, SBP/DBP 130/85 mmHg. During operation, all patients are arranged with arterial blood pressure monitoring and indwelling urinary catheter recording the urine output. Anesthesiologists would pay close attention to the blood pressure, heart rate, respiratory rate and oxyhemoglobin saturation, in order to avoid severe intraoperative hypertensive crisis during anesthesia induction.
The application of vasoactive drugs is at the discretion of anesthesiologists. After clamping the main adrenal vein, the application of anti-hypertensive drugs (α-blockade, calcium channel blockade) and β-blockade should be cut off. While using vasoactive drugs during operation, anesthesiologists would estimate patient’s infusion volume of crystalloid and colloid. Assessed via previous large research reports, intraoperative hemodynamic instability (IHD) is defined as the occurrence of hypertensive (intraoperative SBP > 160 mmHg) episodes or hypotensive (mean artery pressure <60 mmHg) episodes. Most of the anesthesia records took down the accurate SBP regularly, but a few recorded the range of SBP in a period, median is set as the representative for the range on this occasion. Other characteristics of patient and tumor were recorded by circulating nurse, including hemorrhage during operation, time of operation, etc.
Before being sent back to the general ward, patients would receive a period of vital signs monitoring in the postanesthesia care unit (PACU). When it occurs to severe hemodynamic instability or other vital signs seriously abnormal, much higher level of monitoring and care would be arranged in ICU. Postoperative data including postoperative BP, complications, postoperative recovering time and length of postoperative stay were collected from daily progress notes. All those data would be evaluated as different grades or be calculated and analyzed directly. Particular specification, postoperative recovering time is defined as the length the patients recovered into a stable situation with their blood pressure in normal range after operation.
Analyzing the data, for nominal variables, descriptive statistics should include frequency and percentage, and for continuous variables, it should include median and standard deviation (s.d.). For comparing nominal variables, chi-squared tests or Fisher exact test would be used to make deep analysis. As for continuous variables, we would adopt Student–Newman–Keuls test or Mann–Whitney U test. Certainly, P < 0.05 is defined as statistical significance according to statistical theory. All statistical analysis was performed using SPSS 23 (IBM).
Results
Among the 526 patients included, all pathological diagnoses are defined as pheochromocytoma or paraganglioma after open adrenalectomy. Their mean age was 47.6 ± 13.2 years, and 273 patients were females (51.9%).
Average tumor size was 4.9 ± 2.3 cm and 409 of the tumors (77.8%) had a size over 3 cm. 450 patients’ (85.7%) tumors were unilateral, no significant difference in left or right. 25.1% of the tumors were adrenal incidentaloma, that means 132 patients discovered their PPGL in physical examination accidentally rather than seeking medical care proactively. 157 patients (29.8%) had non-functioning pheochromocytoma, without any apparent sign of increase in catecholamine secretion, such as hypertension, headache, etc. and their catecholamines or metanephrine levels are within the normal range. 185 patients (35.2%) got pheochromocytoma crisis, with typical symptoms like paroxysmal or persistent hypertension, paroxysmal headache, sweating, palpitation, pale complexion and so forth. More details about patient and tumor characteristics could be found in Table 1.
Table 1.
Preoperative patient and tumor characteristics.
| Selective α-blockade (n = 149) | Non-selective α-blockade (n = 343) | Selective and non-selective α-blockade (n = 11) | No preparation (n = 23) | P value (selective vs non-selective) | |
|---|---|---|---|---|---|
| Sex, male/female | 84/65 | 156/187 | 3/8 | 10/13 | 0.78 |
| Age, year (average(medium)) | 47.8 (49) | 44.4 (45) | 51.3 (53) | 40.8 (43) | 0.81 |
| BMI, kg/m2 (average (s.d.)) | 21.5 (0.7) | 21.8 (2.9) | 21.7 (2.4) | 23.0 (3.6) | 0.86 |
| Ejection fractions (average (s.d.)) | 62.0 (6.1) | 62.2 (5.3) | 76.5 (0.7) | 63.7 (4.3) | 0.89 |
| Tumor side, unilateral/bilateral | 138/11 | 282/61 | 10/1 | 21/2 | 0.62 |
| Tumor size (average (s.d.)) | 4.7 (1.4) | 5.6 (3.0) | 4.7 (1.7) | 4.2 (1.5) | 0.73 |
| Adrenal incidentaloma, % | 47 (31.5%) | 97 (28.3%) | 2 | 2 | 0.72 |
| Non-functioning pheochromocytoma, % | 19 (12.8%) | 130 (37.9%) | 0 | 8 | 0.43 |
| Pheochromocytoma crisis, % | 93 (62.4%) | 166 (48.4%) | 9 | 4 | 0.56 |
| Multiple endocrine neoplasia II, % | 7 (4.7%) | 23 (6.7%) | 1 | 4 | 0.68 |
| Pathological type 1/2/3/4/5* | 129/18/2/0/0 | 279/21/16/12/15 | 11/0/0/0/0 | 21/0/0/1/1 | 0.63 |
1 means pheochromocytoma, 2 means paraganglioma, 3 means invasive pheochromocytoma, 4 means pheochromocytoma with malignant potential, 5 means malignant pheochromocytoma.
337 patients (64.1%) have got obvious symptom of hypertension, and 233 patients (69.1%) among them are persistent. 104 paroxysmal patients (30.9%) underwent quite unstable hypertensive episode, a large fluctuation range and SBP from 110 to 240 mmHg. Mean duration of suffering from hypertension was 4.3 years, and 76 patients (14.4%) suffered over 10 years. Most (95.6%) patients’ hypertension could be controlled by taking single anti-hypertensive medication, 23 patients (4.4%) should take drug combination of selective and non-selective α-blockade.
The average of preoperative mean arterial pressure (MAP) was 127 mmHg (normal range 70–105 mmHg), with no significant difference between selective and non-selective group. The average of preoperative greatest SBP was 178 mmHg, and the average of preoperative greatest DBP was 108 mmHg. The average of preoperative heart rate was 91 bpm, a high level among the normal range. More information about patient preoperative blood pressure could be found in Table 2.
Table 2.
Preoperative blood pressure.
| Selective α-blockade (n = 149) | Non-selective α-blockade (n = 343) | Selective and non-selective α-blockade (n = 11) | No preparation (n = 23) | P value(selective vs non-selective) | |
|---|---|---|---|---|---|
| Hypertension appearance | |||||
| Occurrence, % | 112 (75.1%) | 204 (59.5%) | 11 | 10 | 0.83 |
| Persistent/paroxysmal, % | 83/29 (74.1/25.9) | 138/66 (67.6/32.4) | 8/3 (72.7/17.3) | 4/6 (40/60) | 0.74 |
| Duration, day (average (s.d.)) | 2128 (1272.8) | 949.9 (1305.9) | 4458.8 (5266.0) | 612.8 (1156.3) | 0.42 |
| Preoperative BP (average (s.d.)) | |||||
| Greatest mean BP, mmHg | 121 (16) | 116 (19) | 133 (22) | 110 (17) | 0.87 |
| Greatest systolic BP, mmHg | 175 (37) | 160 (43) | 206 (28) | 152 (46) | 0.76 |
| Greatest diastolic BP, mmHg | 111 (15) | 105 (22) | 120 (17) | 111 (55) | 0.71 |
| HR, bpm | 93 (14) | 90 (14) | 87 (12) | 89 (14) | 0.91 |
All patients were evaluated under preoperative and postoperative catecholamine, and both normetanephrine and metanephrine. As is confirmed in previous study and in our research, normetanephrine and metanephrine in plasma could experience dramatic change in a relatively short period of time, owing to its episodic secretion. Therefore, normetanephrine and metanephrine in 24-h urine reflect more true condition and convey greater reference value.
The average of preoperative normetanephrine in urine was 957 µg/24 h in selective group and 752 µg/24 h in non-selective group, and there is no significant difference (P = 0.69). The average of preoperative metanephrine in urine was 84 µg/24 h in selective group and 152.8 µg/24 h in non-selective group. Here got a intense difference between both groups, but no specific conclusion according to statistical theory (P = 0.42). The average of postoperative normetanephrine in urine was 48 µg/24 h in selective group (5.1% of its preoperative value) and 106 µg/24 h in non-selective group (14.2% of its preoperative value), no significant difference in both relative and absolute value (P = 0.39). The average of postoperative metanephrine in urine was 6.8 µg/24 h in selective group (80.4% of its preoperative value) and 19.0 µg/24 h in non-selective group (12.4% of its preoperative value). Here, there exists a deliberate contrast between the two relative proportions, but this could be partly explained by the preoperative disparity. More details about preoperative and postoperative catecholamine could be found in Table 3.
Table 3.
Preoperative and postoperative catecholamine.
| Selective α-blockade (n = 149) | Non-selective α-blockade (n = 343) | Selective and non-selective α-blockade (n = 11) | No preparation (n = 23) | P value (selective vs non-selective) | |
|---|---|---|---|---|---|
| Preoperative (average (s.d.)) | |||||
| Normetanephrine in plasma, ng/L | 5163 (6894) | 4807 (13663) | 3602 (3224) | 2104 (2697) | 0.78 |
| Metanephrine in plasma, ng/L | 135 (262) | 381 (658) | 388 (734) | 171 (114) | 0.42 |
| Normetanephrine in urine, µg/24 h | 957 (1009) | 752 (1025) | 915 (1321) | 58 (57) | 0.69 |
| Metanephrine in urine, µg/24 h | 84 (34) | 152.8 (321) | 110.1 (243) | 62 (54) | 0.12 |
| Postoperative (average (s.d.)) | |||||
| Normetanephrine in plasma, ng/L | 539 (301) | 1009 (1435) | 475 (345) | 483 | 0.37 |
| Metanephrine in plasma, ng/L | 72 (44.5) | 117 (161) | 100 (29.8) | 128 | 0.41 |
| Normetanephrine in urine, µg/24 h | 48 (48) | 106 (103) | 67 (59) | 63 | 0.39 |
| Metanephrine in urine, µg/24 h | 6.8 (4.4) | 19.0 (30.4) | 20.3 (25.8) | 17.61 | 0.34 |
All patients received their own preoperative medical preparation according to their blood pressure suitable or unsuitable for adrenalectomy. During the preparation, all doses and their duration were at the discretion of endocrinology doctors or the operating surgeon. The average duration of preoperative preparation are quite similar in both groups, 14.8 for selective and 13.5 for non-selective α-blockade group (P = 0.52). Generally speaking, there exists no significant statistical difference in patients between selective and non-selective α-blockade groups in all preoperative aspects (P > 0.05).
During the operation, 26 patients (4.9%) suffered intraoperative BP fluctuate, 5 in selective α-blockade group (3.4%) and 15 in non-selective α-blockade group (4.4%); there is no statistical difference between the groups (P = 0.64).
After operation, we pay more attention to the blood pressure and recovering condition. The average of mean postoperative SBP was 123 mmHg (s.d. = 21) in selective group, and 107 mmHg (s.d. = 23) in non-selective group. Overall, patients in non-selective group had a more obvious decline than in selective group (P = 0.041). The average of greatest postoperative SBP was 132 mmHg (s.d. = 17) in selective group, and 123 mmHg (s.d. = 23) in non-selective group. Here, we can see the trend, but no specific conclusion according to statistical theory (P = 0.113). The average of greatest postoperative DBP was 90 mmHg (s.d. = 6.4) in selective group and 78 mmHg (s.d. = 12) in non-selective group. In this regard, patients in non-selective group may receive a long-term mechanism in anti-hypertensive effect, especially for DBP (P = 0.037). According to the current observation, no exact evidence indicated that this effect will last long after operation. For rigorous conclusion, we should carry on a further research to proceed verification and analysis. The average of postoperative heart rate was 88 bpm in selective group and 90 bpm in non-selective group; there was no significant difference.
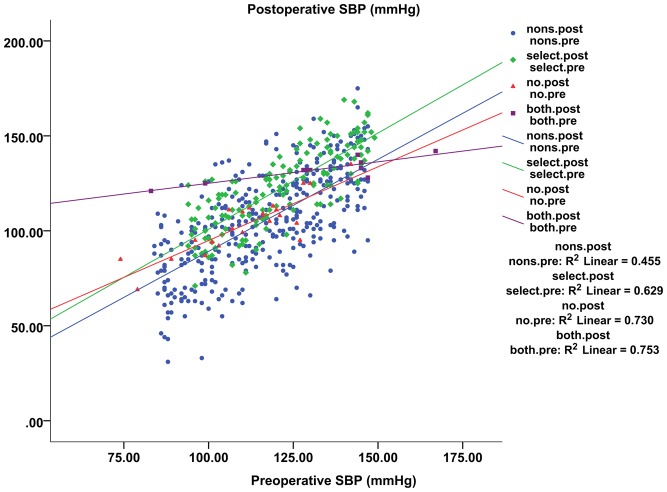
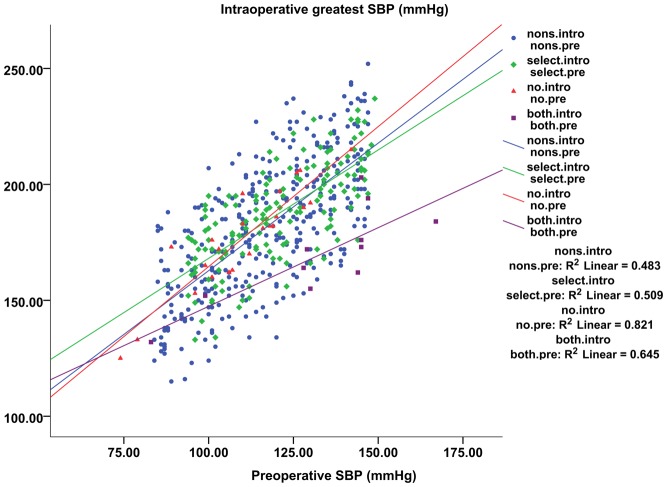
We analyzed the correlation of preoperative, intraoperative and postoperative blood pressure with SPSS 23 (IBM). In bivariate scatter-plot the four groups present quite different tendency of dispersion. The proximity of selective and non-selective α-blocked group in (Fig. 1) confirms the data analysis conclusion: there exists no significant statistical difference in patients between selective and non-selective α-blocked groups in intraoperative hypertensive episodes. However, the two groups differ in (Fig. 2). Combining the tabular data and the scatter-plot, we can strengthen the conclusion that patients in the non-selective group declined more obviously than those in the selective group.
Figure 2.
Bivariate scatter-plot showing preoperative SBP (X-axis) vs postoperative SBP (Y-axis). Patients in non-selective group got a more obvious decline than those in selective group.
Figure 1.
Bivariate scatter-plot showing preoperative SBP (X-axis) vs intraoperative greatest SBP (Y-axis). Their exists no significant statistical difference patients between selective and non-selective α-blocked groups in intraoperative hypertensive episodes.
According to the statistical results, 42 patients (8.0%) experienced different severities of postoperative complications. 22 of them got intraoperative hemodynamic instability and the occurrence of hypotensive (mean artery pressure <60 mmHg) episodes 3–6 h after operation. By applying vasoactive drugs, all the 22 patients got relieved immediately. On paying close attention, blood pressure of the 22 patients were stable till discharge. The other 20 patients got different severities of tachycardia or arrhythmia, hyperpyrexia and sicchasia for unknown reasons. After symptomatic treatment and longer stay in hospital, all the symptoms got relieved and 20 patients were discharged with a stable condition. Among the 42 patients with postoperative complications, 11 patients (7.4%) were in the selective group and 27 patients (7.9%) were in the non-selective group, with no statistical difference (P = 0.82) between groups.
The average postoperative recovering time was 4.7 day in selective group and 3.9 day in non-selective group, quite similar in both groups. The average length of postoperative stay was 7.9 days in selective group and 7.8 days in non-selective group, and there was no significant difference. More details about postoperative blood pressure and recovering condition could be found in Table 4.
Table 4.
Postoperative blood pressure and recovering condition (average (s.d.)).
| Selective α-blockade (n = 149) | Non-selective α-blockade (n = 343) | Selective and non-selective α-blockade (n = 11) | No preparation (n = 23) | P value (selective vs non-selective) | |
|---|---|---|---|---|---|
| Preoperative medical preparation, day | 14.8 (11.5) | 13.5 (13.6) | 21.9 (14.3) | 0 | 0.52 |
| Intraoperative BP fluctuate, % | 5 (3.4%) | 15 (4.4%) | 0 | 6 | 0.64 |
| Greatest intraoperative SBP, mmHg | 188 (18) | 181 (27) | 170 (20) | 177 (22) | 0.37 |
| Minimal intraoperative SBP, mmHg | 71 (6) | 73 (13) | 92 (11) | 96 (18) | 0.56 |
| Postoperative recovering time, day | 4.7 (2.4) | 3.9 (2.2) | 5.2 (2.5) | 3 (0) | 0.48 |
| Postoperative SBP, mmHg | 123 (21) | 107 (23) | 134 (6) | 100 (11) | 0.04 |
| Greatest postoperative SBP, mmHg | 132 (17) | 123 (23) | 159 (7) | 112 (15) | 0.11 |
| Greatest postoperative DBP, mmHg | 90 (6) | 78 (12) | 91 (7) | 74 (8) | 0.04 |
| Postoperative HR, bpm | 88 (7) | 90 (14) | 85 (13) | 80 (9) | 0.21 |
| Length of postoperative stay, day | 7.9 (4.8) | 7.8 (3.9) | 7.4 (2.3) | 5 (1.9) | 0.43 |
| postoperative complications, % | 11 (7.4%) | 27 (7.9%) | 2 (18.2%) | 2 (8.6%) | 0.82 |
Discussion
In the West China Hospital of Sichuan University, endocrinologists and operating surgeons tend to choose non-selective α-blockade. As stated, non-selective α-blockade provides more obvious preventive effects by irreversible receptor binding, more immediate effects and a significant anti-hypertensive effect (26). Using non-selective α-blockade for preoperative preparation could greatly reduce intraoperative hemodynamic instability and reduce the risk of patient death, intraoperatively (27).
In our study, patients in the non-selective group showed a more significant decline in postoperative systolic blood pressure than patients in the selective group (P = 0.041). Also, patients in the non-selective group appeared to receive a long-term anti-hypertensive effect, especially regarding diastolic blood pressure (P = 0.037). Our results confirmed that non-selective α-blockade produced a more significant anti-hypertensive effect compared with selective α-blockade, for both systolic and diastolic blood pressure. Our results also indicated that this anti-hypertensive effect persists for a limited time, postoperatively, which minimizes any adverse effects to patients. To explore the underlying physiological mechanism, further studies of the cellular pathways are needed (8).
Our analysis revealed no statistical difference in intraoperative hemodynamic instability, postoperative recovery and postoperative complications between groups; results were similar for all parameters. This indicated that the different preoperative preparation strategies had essentially no effect on patients’ intraoperative hemodynamics (6). Similarly, we found no significant difference in postoperative recovery and postoperative complications between the groups.
Particularly worth mentioning, patients in the non-selective group did not have a greater probability of suffering from postoperative complications compared with the selective group. In our study, 11 patients (7.4%) in the selective group and 27 patients (7.9%) in the non-selective group experienced postoperative complications with no statistical difference (P = 0.82) between groups. This may have resulted from the accurate and individualized preoperative medical preparation scheme and drug doses determined by endocrinologists or the operating surgeons. This result can also be explained as a metabolic difference between Asian and Caucasian patients (28). We expect further research will provide a reasonable explanation.
Patients experienced intraoperative blood pressure fluctuations, although their preoperative blood pressure was more difficult to control. However, six patients (26.1%) not receiving preoperative preparation suffered intraoperative blood pressure fluctuations. These six patients showed no significant hypertensive symptoms prior to surgery, so they underwent operation the third day after being hospitalized, with no preoperative preparation. We particularly emphasized on preoperative preparation for patients with non-functioning pheochromocytoma because intraoperative stimulation is expected to increase catecholamine release (29), resulting in severe intraoperative hypertensive crisis (24).
As discussed, we adjusted the guidelines to better apply to Chinese patients (13). No patients in our hospital received a high-sodium diet to prevent postoperative hypotension, and 42 patients (8.0%) experienced different severities of postoperative complications. 22 of these 42 patients experienced intraoperative blood pressure fluctuations intraoperatively because of the lack of preoperative preparation or the effects of surgery. The remaining 20 patients (3.8%) experienced postoperative complications for unknown reasons, but all recovered quickly and completely in 3 days. Because of Chinese dietary habits, salt intake is quite adequate in the daily diet. Based on our findings, with an average salt intake of 11.8 ± 4.5 g/day, a high-sodium diet is not necessary for Chinese patients preoperatively (30), as the guidelines recommend (31).
Furthermore, a recently popular type of operation aroused our researching interest. As reported in a systemic review, posterior retroperitoneal adrenalectomy is superior or at least comparable to laparoscopic transperitoneal adrenalectomy in operation time, pain score, blood loss, hospitalization, complications rates and return to normal activity (18). Though we still need further studies to make an objective evaluation, posterior retroperitoneal adrenalectomy has provided us new thought about reducing the burden of preoperative preparation, alleviating patient’s pain and suffering.
During our evaluation of preoperative preparation for adrenalectomy for pheochromocytoma, we also found an issue worthy of further study: 35 patients (6.7%) experienced signs typical of multiple endocrine neoplasia II, with other diseases such as medullary thyroid carcinoma or hyperparathyroidism. Multiple endocrine neoplasia II can be associated with mutation in the RET gene (7). We are following these patients to further research gene sequencing and family heredity.
There are several limitations in our study. First, the preoperative preparation strategy was determined by endocrinologists or operating surgeons based on previous studies and personal experience, probably with strong subjectivity. Second, we have not provided a complete standardized preoperative preparation strategy based on individual patient and tumor characteristics. An individualized strategy suitable for a single patient requires further systematic study. Third, records of intraoperative blood pressure fluctuations were not detailed and included only key data such as maximum value, duration and certain other parameters. Future studies could benefit from recording dynamic changes in intraoperative blood pressure to provide a complete picture. Fitting the dynamic record into mathematical models using MATLAB software, researchers can more accurately analyze patient intraoperative hemodynamic instability data. Finally, because of patients showing poor compliance with postoperative visits, we have inadequate data regarding postoperative one-year- and five-year survival rates. Because of the lack of these data, we could not analyze prognosis or long-term postoperative results.
Conclusion
Our study of selective vs non-selective α-blockade for preoperative preparation of 526 patients undergoing open adrenalectomy for PPGL confirmed that non-selective α-blockade resulted in a more significant anti-hypertensive effect than selective α-blockade. However, we found no significant difference in intraoperative hemodynamic instability, postoperative recovery and postoperative complications between the groups. A complete standardized preoperative preparation strategy based on patient and tumor characteristics is expected and necessary. However, an individual strategy suitable for individual patients requires further systematic research.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This work was supported by National Natural Science Foundation of China (grant numbers 81400665).
References
- 1.Kinney MA, Narr BJ, Warner MA. Perioperative management of pheochromocytoma. Journal of Cardiothoracic and Vascular Anesthesia 2002. 16 359 ( 10.1053/jcan.2002.124150) [DOI] [PubMed] [Google Scholar]
- 2.Isaacs M, Lee P. Preoperative alpha-blockade in phaeochromocytoma and paraganglioma: is it always necessary? Clinical Endocrinology 2016. [DOI] [PubMed] [Google Scholar]
- 3.Kocak S, Aydintug S, Canakci N. Alpha blockade in preoperative preparation of patients with pheochromocytomas. International Surgery 2002. 87 191. [PubMed] [Google Scholar]
- 4.Challis BG, Casey RT, Simpson HL, Gurnell M. Is there an optimal preoperative management strategy for phaeochromocytoma/paraganglioma? Clinical Endocrinology 2017. 86 163 ( 10.1111/cen.13252) [DOI] [PubMed] [Google Scholar]
- 5.Ali AM, Devbhandari M, Sastry A, Ashleigh RJ, Jones MT. Preoperative embolization followed by surgical excision of an intrapericardial pheochromocytoma. Annals of Thoracic Surgery 2007. 83 302–304. ( 10.1016/j.athoracsur.2006.05.100) [DOI] [PubMed] [Google Scholar]
- 6.Almeida CEC, Silva M, Carvalho L, Almeida CMC. Adrenal giant cystic pheochromocytoma treated by posterior retroperitoneoscopic adrenalectomy. International Journal of Surgery Case Reports 2017. 30 201–204. ( 10.1016/j.ijscr.2016.12.018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babic B, Patel D, Aufforth R, Assadipour Y, Sadowski SM, Quezado M, Nilubol N, Prodanov T, Pacak K, Kebebew E. Pediatric patients with pheochromocytoma and paraganglioma should have routine preoperative genetic testing for common susceptibility genes in addition to imaging to detect extra-adrenal and metastatic tumors. Surgery 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brauckhoff M, Gimm O, Dralle H. Preoperative and Surgical Therapy in Sporadic and Familial Pheochromocytoma. Karger Publishers. [DOI] [PubMed] [Google Scholar]
- 9.Erdoğan MA, Uçar M, Özkan AS, Özgul Ü, Durmuş M. Perioperative Management of Severe Hypertension during Laparoscopic Surgery for Pheochromocytoma. Turkish Journal of Anaesthesiology and Reanimation 2016. 44 47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Walther MM, Herring J, Choyke PL, Linehan WM. Laparoscopic partial adrenalectomy in patients with hereditary forms of pheochromocytoma. Journal of Urology 2000. 164 14 ( 10.1016/S0022-5347(05)67438-1) [DOI] [PubMed] [Google Scholar]
- 11.Kiernan CM, Solórzano CC. Pheochromocytoma and paraganglioma: diagnosis, genetics, and treatment. Surgical Oncology Clinics of North America 2016. 25 119–138. ( 10.1016/j.soc.2015.08.006) [DOI] [PubMed] [Google Scholar]
- 12.Gaujoux S, Bonnet S, Lentschener C, Thillois JM, Duboc D, Bertherat J, Samama CM, Dousset B. Preoperative risk factors of hemodynamic instability during laparoscopic adrenalectomy for pheochromocytoma. Surgical Endoscopy 2016. 30 1–10. [DOI] [PubMed] [Google Scholar]
- 13.Miskulin J, Shulkin BL, Doherty GM, Sisson JC, Burney RE, Gauger PG. Is preoperative iodine 123 meta-iodobenzylguanidine scintigraphy routinely necessary before initial adrenalectomy for pheochromocytoma? Surgery 2003. 134 918–922. ( 10.1016/S0039-6060(03)00416-1) [DOI] [PubMed] [Google Scholar]
- 14.Brunt ML, Lairmore TC, Doherty GM, Quasebarth MA, DeBenedetti M, Moley JF. Adrenalectomy for familial pheochromocytoma in the laparoscopic era. Annals of Surgery 2002. 235 713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Naranjo J, Dodd S, Martin YN. Perioperative management of pheochromocytoma. 2017. [DOI] [PubMed] [Google Scholar]
- 16.Pacak K. Preoperative management of the pheochromocytoma patient. Journal of Clinical Endocrinology and Metabolism 2007. 92 4069–4079. [DOI] [PubMed] [Google Scholar]
- 17.Kinney MA, Warner ME, Vanheerden JA, Horlocker TT, Young YW, Jr, Schroeder DR, Maxson PM, Warner MA. Perianesthetic risks and outcomes of pheochromocytoma and paraganglioma resection. Anesthesia and Analgesia 2000. 91 1118–1123. [DOI] [PubMed] [Google Scholar]
- 18.Conzo G, Tartaglia E, Gambardella C, Esposito D, Sciascia V, Mauriello C, Nunziata A, Siciliano G, Izzo G, Cavallo F. Minimally invasive approach for adrenal lesions: systematic review of laparoscopic versus retroperitoneoscopic adrenalectomy and assessment of risk factors for complications. International Journal of Surgery 2016. 28 S118–S123. ( 10.1016/j.ijsu.2015.12.042) [DOI] [PubMed] [Google Scholar]
- 19.Ramachandran R, Rewari V. Current perioperative management of pheochromocytomas. Indian Journal of Urology Iju Journal of the Urological Society of India 2017. 33 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Randle RW, Balentine CJ, Pitt SC, Schneider DF, Sippel RS. Selective versus non-selective alpha-blockade prior to laparoscopic adrenalectomy for pheochromocytoma. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Strajina V, Dy BM, Farley DR, Richards ML, Mckenzie TJ, Bible KC, Que FG, Nagorney DM, Young WF, Thompson GB. Surgical treatment of malignant pheochromocytoma and paraganglioma: retrospective case series. Annals of Surgical Oncology 2017. 1–5. [DOI] [PubMed] [Google Scholar]
- 22.Conzo G, Pasquali D, Gambardella C, Della PC, Esposito D, Napolitano S, Tartaglia E, Mauriello C, Thomas G, Pezzolla A. Long-term outcomes of laparoscopic adrenalectomy for Cushing disease. International Journal of Surgery 2014. 12 S107–S111. ( 10.1016/j.ijsu.2014.05.036) [DOI] [PubMed] [Google Scholar]
- 23.Zhang X, Lang B, Ouyang JZ, Fu B, Zhang J, Xu K, Wang BJ, Ma X. Retroperitoneoscopic adrenalectomy without previous control of adrenal vein is feasible and safe for pheochromocytoma. Urology 2007. 69 849–853. ( 10.1016/j.urology.2007.01.078) [DOI] [PubMed] [Google Scholar]
- 24.Castellucci SA, Curcillo PG, Ginsberg PC, Saba SC, Jaffe JS, Harmon JD. Single port access adrenalectomy. Journal of Endourology 2008. 22 1573–1576. ( 10.1089/end.2008.0100) [DOI] [PubMed] [Google Scholar]
- 25.Zhang JY, Yan LX, Tang JL, Ma JX, Guo XL, Zhao WH, Zhang XF, Li JH, Chu J, Bi ZQ. Estimating daily salt intake based on 24 h urinary sodium excretion in adults aged 18–69 years in Shandong, China. BMJ Open 2014. 4 e005089 ( 10.1136/bmjopen-2014-005089) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weingarten TN, Cata JP, O'Hara JF, Prybilla DJ, Pike TL, Thompson GB, Grant CS, Warner DO, Bravo E, Sprung J. Comparison of two preoperative medical management strategies for laparoscopic resection of pheochromocytoma. Urology 2010. 76 6–11. ( 10.1016/j.urology.2010.08.024) [DOI] [PubMed] [Google Scholar]
- 27.Zhu Y, He HC, Su TW, Wu YX, Wang WQ, Zhao JP, Shen Z, Zhang CY, Rui WB, Zhou WL. Selective α 1 -adrenoceptor antagonist (controlled release tablets) in preoperative management of pheochromocytoma. Endocrine 2010. 38 254 ( 10.1007/s12020-010-9381-x) [DOI] [PubMed] [Google Scholar]
- 28.Proye C, Thevenin D, Cecat P, Petillot P, Carnaille B, Verin P, Sautier M, Racadot N. Exclusive use of calcium channel blockers in preoperative and intraoperative control of pheochromocytomas: hemodynamics and free catecholamine assays in ten consecutive patients. Surgery 1989. 106 1149–1154. [PubMed] [Google Scholar]
- 29.Lenders JW, Eisenhofer G, Mannelli M, Pacak K. Phaeochromocytoma. Lancet 2005. 366 665–675. ( 10.1016/S0140-6736(05)67139-5) [DOI] [PubMed] [Google Scholar]
- 30.Xu J, Wang M, Chen Y, Zhen B, Li J, Luan W, Ning F, Liu H, Ma J, Ma G. Estimation of salt intake by 24-hour urinary sodium excretion: a cross-sectional study in Yantai, China. BMC Public Health 2014. 14 136 ( 10.1186/1471-2458-14-136) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Prys-Roberts C, Farndon JR. Efficacy and safety of doxazosin for perioperative management of patients with pheochromocytoma. World Journal of Surgery 2002. 26 1037–1042. ( 10.1007/s00268-002-6667-z) [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a