Abstract
OBJECTIVES
To evaluate the relationship between gait speed, recall memory, and mortality.
DESIGN
A cohort study (last follow-up December 2009).
SETTING
Tuscany, Italy.
PARTICIPANTS
Individual data from 1,014 community-dwelling older adults aged 60 years or older with baseline gait speed and recall memory measurements and follow-up for a median time of 9.10 (IQR 7.1;9.3) years. Participants were a mean (SD) age of 73.9 (7.3) years, and 55.8% women. Participants walking faster than 0.8 m/s were defined as fast walkers; good recall memory was defined as a score of 2 or 3 in the 3-word delayed recall section of the Mini-Mental State Examination.
MEASUREMENTS
All-cause mortality.
RESULTS
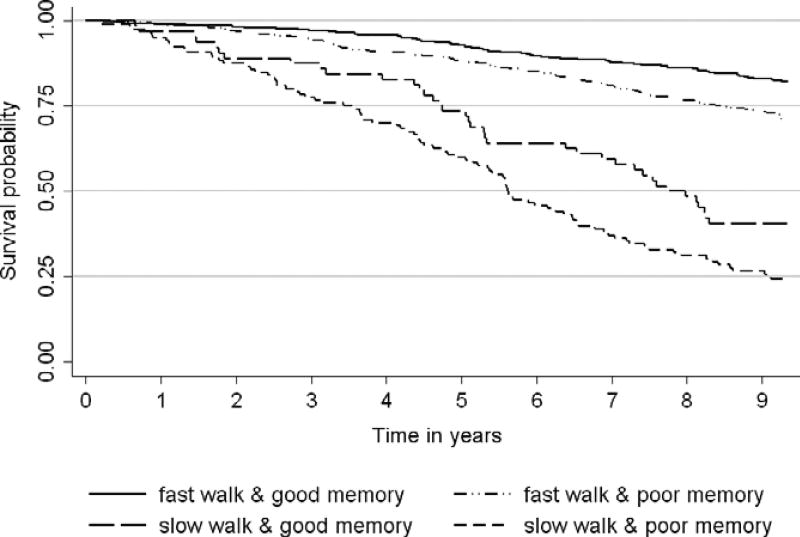
There were 302 deaths and the overall 100 person-year death rate was 3.77 (95% CI: 3.37–4.22). Both low gait speed and poor recall memory were associated with mortality when analysed separately (HR = 2.47; 95% CI: 1.87–3.27 and HR = 1.47; 95% CI: 1.16–1.87, respectively). When we grouped participants according to both recall and gait speed, death rates (100 person-years) progressively increased from those with both good gait speed and memory (2.0; 95% CI: 1.6–2.5), to those with fast walk but poor memory (3.4; 95% CI: 2.8–4.2), to those with slow walk and good memory (8.8; 95% CI: 6.4–12.1), to those with both slow walk and poor memory (13.0; 95% CI: 10.6–16.1). In multivariate analysis, poor memory significantly increases mortality risk among persons with fast gait speed (HR = 1.40; 95% CI: 1.04–1.89).
CONCLUSION
In older persons, gait speed and recall memory are independent predictors of expected survival. Information on memory function might better stratify mortality risk among persons with fast gait speed.
Keywords: gait speed, recall memory, survival, older persons
Since the changes in worldwide demography that started about a century ago, resulting in an ageing population, studying factors associated with survival has become of great interest for clinicians, researchers and health policy makers. The attention of researchers focused on aspects other than those traditionally linked to mortality (e.g., acute or chronic diseases) that could better explain trajectories of survival in the old population and open new lines of research on ageing.
Multiple prognostic indices and models have been developed1 in order to predict life expectancy in the older population, but it has been demonstrated that a simple mobility test, gait speed, has a similar accuracy.2 Gait speed could be considered a summary indicator of vitality because it integrates known and unrecognized disturbances in multiple organ systems, many of which affect survival.2 There is evidence that the predictive value of gait speed for mortality is increased when used in combination with some cognitive tests, in particular the so-called functional neuropsychological tests, such as the digit symbol and the trial making test.3 Indeed, executive function and speed compared to other cognitive tests may be reflective of systemic vascular disorders and for that reason linked to higher mortality.4 This “vascular” hypothesis was strengthened by Verghese and colleagues who described a motoric cognitive risk syndrome characterized by slow gait and subjective cognitive complains, highly predictive of vascular dementia and of increased mortality in older persons.5 Our hypothesis was that cognitive domains other than functional could be linked to mortality and increase the predictive value of gait speed. This hypothesis raises from the proved link between Alzheimer’s disease with early mortality, even in the preclinical stages;6 thus, we evaluated the cognitive domain early affected by this neurodegenerative disease, memory. Indeed, memory decline could be not only etiologic, e.g., it reflects an ongoing beta amyloid and neurodegenerative process, but also syndromic, e.g., it reflects biological frailty.7 As a memory test, we employed the 3-word delayed recall section of the MiniMental State Examination8 because it is simple and short to administered, well-known and spread in clinical practice and epidemiological studies.
The purpose of this study is therefore to evaluate the association of a mobility test, gait speed, and a cognitive test, recall memory, with mortality in older adults and to determine if the combination of these two tests improves the prediction of survival, after accounting for sociodemographic and health factors.
METHODS
Study Design
The InCHIANTI study is a population-based study of older people living in the Chianti, Tuscany, Italy.9 The Italian National Research Council on Aging Ethical Committee ratified the study protocol.
Participants
In August 1998, 1,530 were randomly selected from the population registry from Greve in Chianti and Bagno a Ripoli, (Tuscany, Italy). Of the 1,530 persons sampled, 1,453 (94%) agreed to participate. Those who agreed signed a participant consent form. Participants responded to a home interview and underwent a medical and functional examination. Two hundred fifty participants were excluded because they were younger than 60 years and 189 because of missing data in either gait speed or recall memory test; the final analytic sample for this specific project was 1,014 (last follow-up 2009). Data on mortality were derived from the municipality register.
Gait Speed
To measure walking speed on a 4-m course, two photocells connected with a recording chronometer were placed at the beginning and end of a 4-m course. Subjects were instructed to stand with both feet touching the starting line and to walk at their usual pace, immediately after a verbal command. Walking speed lower than 0.8 m/s identified slow walker participants.10
Recall Memory
The Mini-Mental State Examination (MMSE) was employed to assess cognitive status.8 The MMSE is a 30-point questionnaire frequently used to screen cognitive impairment. It allows the assessment of different cognitive domains, i.e., temporal and spatial orientation (5 + 5 points), registration (3 points) and recall memory (3 points), attention and calculation (5 points), language and ability to follow simple commands (6 points). The recall memory domain (delayed recall of three words) was employed to test the association between performance in this particular cognitive function and survival. A score ≤1 identified participants with poor memory.
Covariates
Socio-demographic Characteristics
Socio-demographic variables (age, gender, education) were assessed through survey questions.
Participants were classified according to smoking habits in two groups, never smokers and current or former smokers. Daily alcohol (g/d) were estimated by the European Prospective Investigation Into Cancer and Nutrition Food Frequency Questionnaire.11 Weight and height were measured using objective standard techniques and used to calculate body mass index (BMI, kg/m2).
Comorbidities
Medical conditions were diagnosed combining selfreported history, medical records, and a clinical medical examination. Diagnostic algorithms were modified versions of those created for the Women’s Health and Aging Study.12 The following were assessed: stroke (and/or transient ischemic attack), hypertension, atrial fibrillation, and diabetes. Depressive symptoms were assessed by the standard Center for Epidemiologic Studies Depression scale (CES-D).13 Possible range of scores is zero to 28, with the higher scores indicating the presence of more symptoms and scores >16 are considered indicative of high depressive symptoms.
Statistical Analysis
All persons aged 60 years or older were included in the initial sample. They were stratified according to gait speed (≤0.8 vs >0.8 m/s) and memory function (good/poor memory: 2–3 vs 0–1 words recalled). Association between categorical variables was examined comparing the relative frequencies and using the Pearson chi-squared test. Comparison between groups with respect to numerical variables was done using t-test on means in cases of normal distribution or comparing the medians and using the nonparametric Wilcoxon Mann–Whitney test otherwise.
Death rates (per 100-person years) were estimated according to memory function and gait speed categories. Cox models were employed to analyze the associations of recall memory and gait speed with survival. Univariate and multivariate Cox regression models were run to check the significance of the two main predictors after accounting for potential confounders, including age, gender, education, smoking, alcohol, hypertension, atrial fibrillation, stroke, diabetes, depression, and BMI. Further, gait speed and recall memory were used to stratify the sample into four groups: fast walkers/good memory, fast walkers/poor memory, slow walkers/good memory, slow walkers/poor memory; the association with survival was investigated using Kaplan-Meier survival function and tested with univariate and multivariable Cox models. Formal test for interaction between gait and memory was tested in a multivariable model.
Thirty-nine participants had at least one missing data, 6 (0.6%) for alcohol, 24 (2.4%) for CES-D and 15 (1.5%) for BMI. These three variables were not associated with mortality.
RESULTS
Table S1 shows socio-demographic and clinical characteristics of participants according to gait speed; 830 persons were classified as fast walkers (81.9%) and 184 as slow walkers (18.1%). Slow walkers were older, more likely to be female, with a lower number of years of schooling; they were also more likely to be affected by diabetes, hypertension, atrial fibrillation, cerebrovascular diseases, and depression.
According to recall memory score, 433 (42.7%) of the participants had a score of 0 or 1 (poor memory) and 581 (57.3%) a score of 2 or 3 (good memory). Table S2 shows socio-demographic and clinical characteristics of participants according to recall memory score. Those with poor memory were older and with a lower number of years of schooling than those with good memory; they were also more likely to be affected by cerebrovascular diseases.
Of the 1,014 initial participants, followed up for a median time of 9.10 (IQR 7.1; 9.3) years, 302 died during the follow-up (3.77 deaths per 100 person-years; 95% CI: 3.37–4.22). Death rate (100-person year) was 11.39 (95% CI: 9.57–13.55) and 2.54 (95% CI: 2.19–2.94) for slow and fast gait speed categories separately; while according to recall memory score the death rate was 5.47 (95% CI: 4.72–6.34) and 2.64 (95% CI: 2.22–3.14) for poor and good memory, respectively. A Cox regression model adjusted for multiple confounders showed that slower gait speed was directly associated with mortality (HR = 2.47; 95% CI: 1.87–3.27). The same model was run using recall memory instead of gait speed, showing that poor recall memory was directly associated with mortality (HR = 1.47; 95% CI: 1.16–1.87).
When gait speed and recall memory were included in the same multivariable model both predictors were significantly associated with the risk of death independently of confounding factors (Table 1). The addition of the recall memory variable to the model including gait speed only, improved the overall goodness of fit of the model (LR test P-value = .032).
Table 1.
Cox Regression Model Testing the Association of Gait Speed and Recall Memory with Survival Separately and Concurrently
| Unadjusted | Fullya adjusted | |||||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Separately | Concurrently | Separately | Concurrently | |||||
|
|
|
|
|
|||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Fast | 1.00 | 1.00 | 1.00 | 1.00 | ||||
|
| ||||||||
| Slow walk | 4.99 | 3.96–6.29 | 4.45 | 3.51–5.63 | 2.47 | 1.87–3.27 | 2.34 | 1.76–3.11 |
|
| ||||||||
| Good | 1.00 | 1.00 | 1.00 | 1.00 | ||||
|
| ||||||||
| Poor memory | 2.13 | 1.70–2.68 | 1.66 | 1.31–2.10 | 1.47 | 1.16–1.87 | 1.31 | 1.02–1.67 |
Full model includes: age, sex, education, smoking status, hypertension, atrial fibrillation, diabetes, and cerebrovascular disease.
HR = hazard ratio; CI = confidence intervals.
We then grouped participants according to both recall memory and gait speed in four mutually exclusive categories and we found 120 (11.8%) slow walkers with poor memory, 64 (6.3%) slow walkers with good memory, 313 (30.9%) fast walkers with poor memory, and 517 (51.0%) fast walkers with good memory. Figure 1 shows Kaplan-Meier survival curves according to the four groups. Death rates (100 person-years) progressively increased from those with both good gait speed and memory (2.0; 95% CI: 1.6–2.5), to those with fast walk but poor memory (3.4; 95% CI: 2.8–4.2), to those with slow walk and good memory (8.8; 95% CI: 6.4–12.1), to those with both slow walk and poor memory (13.0; 95% CI: 10.6–16.1). Table 2 shows the Cox regression model estimates including the combination of gait speed and recall memory categories; there was a dose-response relationship with an increase in hazard as the joint gait speed-memory variable becomes worse. According to the results of the adjusted Cox model, persons with slow gait speed and poor memory had a 3-fold increase risk of death compared to those with fast gait speed and good memory. Although the interaction term between memory and gait speed was not statistically significant (P-value = .437), poor memory significantly increased the risk of death among persons with fast gait speed (HR = 1.40 95% CI: 1.04–1.82)
Figure 1.
Kaplan-Meier survival curves according to recall memory and gait speed.
Table 2.
Cox Regression Model Testing the Association of Gait Speed and Recall Memory Combination with Survival
| Unadjusted | Age-Sex Adjusted |
Fully Adjusteda | ||||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| HR | 95% CI | HR | 95% CI | HR | 95% CI | |
| Fast-good | 1.00 | 1.00 | 1.00 | |||
|
| ||||||
| Fast-poor | 1.71 | 1.27–2.30 | 1.41 | 1.05–1.90 | 1.40 | 1.04–1.89 |
|
| ||||||
| Slow-good | 4.68 | 3.20–6.84 | 3.11 | 2.07–4.67 | 2.65 | 1.75–4.02 |
|
| ||||||
| Slow-poor | 7.37 | 5.48–9.92 | 3.30 | 2.34–4.66 | 3.05 | 2.16–4.32 |
Full model includes: age, sex, education, smoking status, hypertension, atrial fibrillation, diabetes and cerebrovascular disease.
HR = hazard ratio; CI = confidence intervals.
CONCLUSION
Findings from this study showed that two simple tests, gait speed and recall memory, are useful independent predictors of expected survival in older persons. Furthermore, information on memory function might better stratify mortality risk among persons with fast gait speed. The main advantages of these two tests are on one hand that both gait speed and recall memory could be administered in every clinical setting as they do not need special equipment and they take just a few minutes to be measured, and on the other hand that they are highly informative.
The association between gait speed and survival is well known. The best evidence was provided by Studenski and colleagues who analyzed gait speed in a large sample of individual data from diverse populations of communitydwelling elders.2 It is unknown why gait speed is strongly predictive of adverse outcomes. Some hypotheses have been developed: slow walking speed may be a marker of reduced mobility that in itself plays a causal role in health deterioration; biological and physiological conditions that contribute to reduced speed are also primarily responsible for subsequent negative health events; poor mobility develops when a critical threshold of energy scarcity has been passed, a condition that is associated with high mortality risk.14 It has also been postulated that the age-associated decline in walking speed is a reliable barometer of the impact of biological aging on health. Finally, functional measures like walking speed, may capture the cumulative effect of multimorbidity on the health status of older people. As a result, gait speed might help identify older adults with a high probability of living for a certain number of years, who may be appropriate targets for preventive interventions or might be used to stratify risks from surgery or chemotherapy.2
The association between recall memory and survival has rarely been studied. Wagner and colleagues found that the number of words recalled from a list of ten nouns was associated with mortality in older adults.15 In a population of older adults free of dementia, mortality was 52% greater in persons with the lowest memory score (0) in the 3-word recall item of the MMSE vs. persons with the highest score (3).16 Amnestic MCI has been found to be associated with a higher risk of mortality.17 Several hypotheses can be proposed about the association between memory deficits and survival; persons with memory deficits may underreport signs or symptoms, leading to late diagnosis of diseases affecting survival; another hypothesis is that altered memory reflects alteration in brain structure/functioning (i.e., reduced cognitive reserve due to ischemic lesions and/or B-amyloid deposition) and its control of physiological systems by neurotransmitters and hormones which could affect survival. Finally, memory can reflect cognitive frailty due to the presence of depression, use of anticholinergic medications, polypharmacy, infections, sleep problems and other conditions associated with higher mortality risk.
The combination of cognitive functioning and gait speed as predictor of survival has not been clarified yet. Previous studies showed mixed findings and had several limitations. Some were done only in women or men,18 some only in selected populations, e.g., very old persons19 or older adults free of stroke or cognitive impairment at baseline.3 Some have used batteries of several cognitive or functional tests which are time consuming or difficult to perform in primary care. One study performed in nonagenarian Danes showed that the chair stand score combined with MMSE was a way to estimate overall chance of survival in very old adults.19 Ensrud and colleagues evaluated the combination of functional and cognitive tests as a predictor of mortality in older women finding that the 5-year mortality risk was substantially increased among women with deficits in mobility even after accounting for cognition.18 Studies that found the trail-making or the digit symbol tests predictive of mortality postulated that the association was due to their connection with mobility; they are functional neuropsychological tests. Mobility limitations are common in community-dwelling older adults but are largely understudied, particularly regarding the role of the central nervous system.20 Neuroimaging approaches have the potential to reveal the neural networks and their interactions. Neuroimaging has shown that the trail making test enhances frontal activities and other cortical areas involved in movement control.21
The novelty of our study relies in the combination of a recall memory test and gait speed which increased the prediction of survival. Poor recall memory could add some additional and diverse information on cerebral functioning and neuroplasticity compared to other global or specific tests.22 Hypothetically, persons with good memory and fast gait may be the ones with the major brain reserve and plasticity leading at the end to longer survival.
The interpretation of these findings needs to address some limitations. We did not find a statistically significant interaction to formally support the hypothesis of an effect modification between mobility and cognition for mortality risk prediction, but our power to detect such an interaction was probably limited. Furthermore, although our analytic approach accounted for several prognostic indicators of survival late in life a residual confounding effect cannot be completely ruled out.
Gait speed is the most relevant physical ability with strong prognostic value for survival in older age. This extraordinary prognostic information could be increased by recall memory, being superior to traditional medical information.
Supplementary Material
Table S1. Socio-Demographic and Clinical Characteristics of Participants According to Gait Speed
Table S2. Socio-Demographic and Clinical Characteristics of Participants According to the Recall Memory Score
Acknowledgments
Sponsor’s Role: The sponsor had no role in study design, data collection, data analysis, data interpretation, the writing of the report, or in the decision to submit the paper for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Footnotes
Conflicts of Interest: All authors declare: no support from any organization for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; and no other relationships or activities that could appear to have influenced the submitted work.
Financial Disclosure: The InCHIANTI Study (Invecchiare in Chianti, aging in the Chianti area) is currently supported by a grant from the National Institute on Aging (NIH, NIA, Bethesda, MD USA) and is coordinated by the Tuscany Regional Health Agency in a partnership with the Florence Health Care Agency, the local Administrators and the primary care physicians of Greve in Chianti and Bagno a Ripoli, the two small towns in the countryside of Tuscany were the study was conducted. The study was initially managed by the National Institute on Research and Care of the Elderly (INRCA, Ancona, Italy) and it was funded by Italian Health Ministry and by a NIH contract.
Author Contributions: AM and SV designed the study. EM and SV did the statistical analyses. AM and SV drafted the manuscript. All authors critically revised the manuscript for important and intellectual content. AM is the guarantor. All authors, external and internal, had full access to all of the data (including statistical reports and tables) in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis.
Ethical approval: This study was approved by the Italian National Research Council on Aging and informed consent was obtained from all participants.
Additional Supporting Information may be found in the online version of this article:
References
- 1.Yourman LC, Lee SJ, Schonberg MA, et al. Prognostic indices for older adults: A systematic review. JAMA. 2012;307:182–192. doi: 10.1001/jama.2011.1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305:50–58. doi: 10.1001/jama.2010.1923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rosano C, Newman AB, Katz R, et al. Association between lower digit symbol substitution test score and slower gait and greater risk of mortality and of developing incident disability in well-functioning older adults. J Am Geriatr Soc. 2008;56:1618–1625. doi: 10.1111/j.1532-5415.2008.01856.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rostamian S, van Buchem MA, Westendorp RG, et al. Executive function, but not memory, associates with incident coronary heart disease and stroke. Neurology. 2015;85:783–789. doi: 10.1212/WNL.0000000000001895. [DOI] [PubMed] [Google Scholar]
- 5.Ayers E, Verghese J. Motoric cognitive risk syndrome and risk of mortality in older adults. Alzheimers Dement. 2016;12:556–564. doi: 10.1016/j.jalz.2015.08.167. [DOI] [PubMed] [Google Scholar]
- 6.Vos SJ, Xiong C, Visser PJ, et al. Preclinical Alzheimer’s disease and its outcome: As longitudinal cohort study. Lancet Neurol. 2013;12:957–965. doi: 10.1016/S1474-4422(13)70194-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nishiguchi S, Yamada M, Fukutani N, et al. Differential association of frailty with cognitive decline and sarcopenia in community-dwelling older adults. J Am Med Dir Assoc. 2015;16:120–124. doi: 10.1016/j.jamda.2014.07.010. [DOI] [PubMed] [Google Scholar]
- 8.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 9.Ferrucci L, Bandinelli S, Benvenuti E, et al. Subsystems contributing to the decline in ability to walk: bridging the gap between epidemiology and geriatric practice in the InChianti study. J Am Geriatr Soc. 2000;48:1618–1625. doi: 10.1111/j.1532-5415.2000.tb03873.x. [DOI] [PubMed] [Google Scholar]
- 10.Lauretani F, Russo CR, Bandinelli S, et al. Age-associated changes in skeletal muscles and their effect on mobility: An operational diagnosis of sarcopenia. J Appl Physio (1985) 2003;95:1851–1860. doi: 10.1152/japplphysiol.00246.2003. [DOI] [PubMed] [Google Scholar]
- 11.Kaaks R, Riboli E. Validation and calibration of dietary intake measurements in the EPIC project: Methodological considerations. European Prospective Investigation into Cancer and Nutrition. Int J Epidemiol. 1997;26(Suppl 1):S15–S25. doi: 10.1093/ije/26.suppl_1.s15. [DOI] [PubMed] [Google Scholar]
- 12.Guralnik JM, Fried LP, Simonsick EM, et al., editors. The Women’s Health and Aging Study: Health and Social Characteristics of Older Women with Disability. Bethesda, MD: National Institute on Aging; 1995. [Google Scholar]
- 13.Radloff LS. The CES-D scale: A self report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401. [Google Scholar]
- 14.Schrack JA, Simonsick EM, Ferrucci L. The energetic pathway to mobility loss: An emerging new framework for longitudinal studies on aging. J Am Geriatr Soc. 2010;58(Suppl 2):S329–S336. doi: 10.1111/j.1532-5415.2010.02913.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wagner DC, Short JL. Longitudinal predictors of self-rated health and mortality in older adults. Prev Chronic Dis. 2014;11:E93. doi: 10.5888/pcd11.130241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Villarejo A, Bermejo-Pareja F, Trincado R, et al. Memory impairment in a simple recall task increases mortality at 10 years in non-demented elderly. Int J Geriatr Psychiatry. 2011;26:182–187. doi: 10.1002/gps.2512. [DOI] [PubMed] [Google Scholar]
- 17.Bermejo-Pareja F, Contador I, Trincado R, et al. Prognostic significance of mild cognitive impairment subtypes for dementia and mortality: Data from the NEDICES cohort. J Alzheimers Dis. 2015;50:719–731. doi: 10.3233/JAD-150625. [DOI] [PubMed] [Google Scholar]
- 18.Ensrud KE, Lui LY, Paudel ML, et al. Study of Osteoporotic Fractures (SOF). Effects of mobility and cognition on risk of mortality in women in late life: A prospective study. J Gerontol A Biol Sci Med Sci. 2016;71:759–765. doi: 10.1093/gerona/glv220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thinggaard M, McGue M, Jeune B, et al. Survival prognosis in very old adults. J Am Geriatr Soc. 2016;64:81–88. doi: 10.1111/jgs.13838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rosso AL, Studenski SA, Chen WG, et al. Aging, the central nervous system, and mobility. J Gerontol A Biol Sci Med Sci. 2013;68:1379–1386. doi: 10.1093/gerona/glt089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zakzanis KK, Mraz R, Graham SJ. An fMRI study of the trial making test. Neuropsychologia. 2005;43:1878–1886. doi: 10.1016/j.neuropsychologia.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 22.Sorond FA, Cruz-Almeida Y, Clark DJ, et al. Aging, the central nervous system, and mobility in older adults: Neural mechanisms of mobility impairment. J Gerontol A Biol Sci Med Sci. 2015;70:1526–1532. doi: 10.1093/gerona/glv130. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Socio-Demographic and Clinical Characteristics of Participants According to Gait Speed
Table S2. Socio-Demographic and Clinical Characteristics of Participants According to the Recall Memory Score