Abstract
Objectives:
Mechanical diagnosis and therapy is one of the most common approaches for the management of low back pain. In mechanical diagnosis and therapy, a great emphasis is placed on patient education so that patients can manage their problems by themselves. However, there has been no evidence that mechanical diagnosis and therapy actually enhances patient’s self-management skills. This study aimed to preliminarily investigate whether self-reported skills of self-management for musculoskeletal problems are enhanced through the course of mechanical diagnosis and therapy.
Method:
Outpatients with musculoskeletal disorders in a local orthopedic clinic were included. The primary outcome measures were the “Self-monitoring and Insight” and “Skill and Technique Acquisition” scores of the Health Education Impact Questionnaire, where higher scores indicate greater self-management skills. Mechanical diagnosis and therapy was undertaken up to a maximum of twice per week for 1 month. The Self-monitoring and Insight and Skill and Technique Acquisition scores before and 1 month after the mechanical diagnosis and therapy interventions were compared. Proportions of patients who exceed the threshold for “reliable change” in the Health Education Impact Questionnaire scores (% >positive “reliable change”) and proportions of patients with the net positive “reliable change” (% net positive “reliable change”) were investigated.
Results:
Forty-five patients participated and 97.8% completed the 1-month follow-up. The Self-monitoring and Insight and Skill and Technique Acquisition scores significantly increased at the follow-up (Self-monitoring and Insight, p = 0.002; Skill and Technique Acquisition, p < 0.001. The % >positive “reliable change” (Self-monitoring and Insight = 22.2%, Skill and Technique Acquisition = 48.9%) and % net positive “reliable change” (Self-monitoring and Insight = 13.3%, Skill and Technique Acquisition = 46.7%) in this study were comparative to or greater than self-management programs in previous studies (%> positive “reliable change’: Self-monitoring and Insight = 20.5%, Skill and Technique Acquisition = 30.7%; % net positive “reliable change”: Self-monitoring and Insight = 14.1%, Skill and Technique Acquisition = 23.0%).
Conclusion:
This study provides a preliminary evidence that mechanical diagnosis and therapy enhances patient’s self-management skills, particularly in the self-monitoring skills for symptoms/functions and the self-management skill for symptoms/problems.
Keywords: Musculoskeletal pain, physical therapy specialty, self-care
Introduction
Mechanical diagnosis and therapy (MDT)1–3 is one of the most common approaches for the management of low back pain.4–7 A study8 demonstrated that certified MDT practitioners had more bio-psycho-social perspectives than general physiotherapists. MDT has also been applied for the management of a variety of musculoskeletal disorders9–15 and a great emphasis is placed on patient education regardless of the site of problems.1–3 It is important in MDT to educate patients to manage their symptoms and problems by themselves and to undertake self-care as promoting self-care is associated with satisfaction for care16 and patient education is considered to be effective for maximizing treatment effects and preventing recurrence of problems.17–20
A study demonstrated that education of self-care was essential in patients with low back pain, but that acceptance of this message was not automatic.21 Providing educational material alone does not appear to change behavior.22 Therefore, in MDT, patient education is undertaken through physical evaluations, in which patients are actively involved. Symptom and functional responses to mechanical loading are important for decision-making in MDT. MDT therapists maximize patient’s opportunities to realize what mechanical loading makes their symptoms worse and/or better (self-monitoring skills for symptoms/functions) through physical evaluations and empower self-efficacy for managing their symptoms (self-management skill for symptoms/problems). However, as far as the author knows, there has been neither evidence for enhancement of the self-monitoring skills for symptoms/functions nor the self-management skill for symptoms/problems through the course of an episode of care with MDT.
A randomized controlled trial (RCT) with a wait-and-see control group is a standard method to investigate an effect of a certain intervention, and using patients in a clinical setting is clinically meaningful. However, an RCT requires substantial cost and effort. Furthermore, it is ethically difficult to undertake an RCT with patient allocation into a wait-and-see control intervention or unfavorable interventions in a clinical setting. However, it is possible to establish a preliminary evidence of an effect of a certain intervention when a reference score of the effect is established.
The Health Education Impact Questionnaire (HeiQ) is a reliable and valid self-reporting questionnaire for self-management skills.23–26 The HeiQ has an established threshold for “reliable change” and benchmark scores from previous multiple studies with self-management programs (Benchmarks for Change on the Scales of the Health Education Impact Questionnaire Based on a Sample of 3221 Australian Respondents, Deakin University, Victoria, Australia). The threshold and benchmark scores are useful to preliminarily investigate whether pre–post differences are clinically meaningful or not without a wait-and-see control group.
The purpose of this study was to preliminarily investigate whether an episode of care with MDT would enhance the self-monitoring skills for symptoms/functions and the self-management skill for symptoms/problems in people with musculoskeletal disorders using a before–after study design. The preliminary evidence would open further investigations about optimal forms of education and behavioral modification of patients to maximize prevention from recurrence of musculoskeletal problems.
Methods
Design
The study design was a before–after study. Target sample size information of the trial registration (UMIN000020818) was updated and increased when sample size estimation was undertaken in March 2016. Outcome measures at baseline and 1 month after the initial consultation (end-point) were compared. For patients who discharged before the end-point assessment, a postal survey including the outcome measures was conducted. This study was approved by the institutional review board of the Saitama Prefectural University. Participants provided a written consent form before data collection.
Participants
Participants were recruited via advertising in a local orthopedic clinic in Saitama, Japan. Inclusion criteria of participants were as follows: (1) individuals with a musculoskeletal disorder diagnosed by orthopedic surgeons, (2) individuals without contraindications to manual therapy techniques such as fracture, infection, or severe osteoporosis, (3) individuals who attended outpatient physiotherapy in the local orthopedic clinic, and (4)≥20 years of age. Exclusion criteria were as follows: (1) individuals with an order of physiotherapy after a surgical intervention, (2) individuals who have a diagnosed cognitive disorder or neurological disorders, and (3) any co-interventions other than MDT.
Intervention
The MDT was conducted by a credentialed MDT physical therapist, who also passed the MDT diploma clinical training, which is the highest level of training in the MDT program, consisting of both clinical and theoretical components. The MDT interventions1–3 (20–40 min) were undertaken up to a maximum of twice a week in the orthopedic clinic as a matter of convenience, including history taking, physical evaluations, managements corresponding with MDT classifications, troubleshooting in follow-ups, and progression and adjustment of exercises and manual therapy techniques.
Outcome measures
Primary outcome
The HeiQ has 40 items and eight factors (Self-monitoring and Insight (SMI), Skill and Technique Acquisition (STA), Health-Directed Behavior (HDB), Positive and Active Engagement in Life (PAEL), Emotional Distress (ED), Constructive Attitudes and Approaches (CAA), Social Integration and Support (SIS), and Health Services Navigation (HSN)). Participants rate their agreement for each item on a 4-point Likert scale (1 = Strongly disagree, 2 = Disagree, 3 = Agree, 4 = Strongly agree). A mean score is calculated for each factor. A greater score indicates enhanced self-management skill in the five factors except the ED scores. A lower ED score indicates better emotional status.
In this study, the self-monitoring skills for symptoms/functions and the specific self-management skill for symptoms/problems were primary concerns, and thus the primary outcome measures in this study were the SMI and STA scores. The SMI scores indicate the individuals’ ability to monitor their condition, and their physical and/or emotional responses that lead to insight and appropriate actions to self-manage (e.g. “I carefully watch my health and do what is necessary to keep as healthy as possible”).25 The STA scores indicate the knowledge-based skills and techniques that persons acquire to help them cope with symptoms and health problems (e.g. “When I have symptoms, I have skills that help me cope”).25 These primary outcome measures were assessed at the baseline and the end-point.
Secondary outcome
Secondary outcome measures in this study were as follows: (1) the P4, (2) the 7-point Global Perceived Change Scale (GPCS), (3) eight health status (physical function, role physical, bodily pain, general health, vitality, social function, role emotional and mental health) assessed by the Medical Outcomes Study 36-Item Short-Form Health Survey version 2-week (SF-36v2-week), and (4) the six factor scores of the HeiQ (HDB, PAEL, ED, CAA, SIS, and HSN). The secondary outcome measures except the GPCS were assessed at the baseline and the end-point. The GPCS was assessed at the end-point.
The P4 is a self-reporting questionnaire for pain intensity, whose validity and reliability have been established.27 The P4 has four 0–10 numerical rating scales (0 = no pain, 40 = the highest possible pain level).
The SF-36v2-week is a self-reporting measure for health status, whose validity and reliability have been established.28,29 A higher value (0–100) indicates better health status during the last week.30
The GPCS is a self-reporting questionnaire to quantify a patient’s improvement, whose validity and reliability have been established.31,32 The scale has three labels (−3 = Very much worse, 0 = Unchanged, 3 = Completely recovered). According to the recommendation of the use of the GPCS,31,33 the score ≥2 was considered to be a clinically meaningful improvement of symptoms in this study.
The HDB scores relate to a tangible change in lifestyle, specifically related to healthful behaviors such as exercise and relaxation/recreation (e.g. “On most days of the week, I do at least one activity to improve my health (e.g. walking, relaxation, exercise).”25 The PAEL scores indicate motivation to be actively engaged in life-fulfilling activities (e.g. “I am doing interesting things in my life”).25 The ED scores indicate overall negative affect including worry, depression, and anger (e.g. “I often worry about my health”).25 The CAA scores indicate individual’s view of the impact of their condition on their life (e.g. “I do not let my health problems control my life.”25 The SIS scores indicate the positive impact of social engagement and support that evolves through interaction with others (e.g. “If I need help, I have plenty of people I can rely on”).25 The HSN scores indicate an individual’s understanding of and ability to interact with a range of health organizations and health professionals, including confidence and ability to communicate with healthcare providers to get needs met (e.g. “I communicate very confidently with my doctor about my healthcare needs”).25
Data analysis
An a priori sample size estimation was conducted in the internal pilot study as Sandvik et al.34 recommended using 10 participants. The G*Power 335 demonstrated that 43 participants were required to detect a pre–post significant difference in the SMI scores (0.2β and 0.05α, 0.44 effect size d) and 8 participants in the STA scores (0.2β and 0.05α, 1.17d). Considering 5% drop-out, it was decided to recruit 45 participants in a final study. The 10 participants in the pilot study were included in the final study as there was no change in the data collection method.
SPSS version 21.0 (IBM Corporation, NY, USA) was used for statistical analyses. Descriptive statistics were used to summarize characteristic of the participants and the GPCS. An intention-to-treat analysis was used, where all values at the end-point were treated the same as the scores at baseline in the drop-out participants.
Parametric statistics were used in this study, where two-tailed matched paired sample t-tests were used to compare outcome measures between the baseline and the end-point. An effect size of the difference was calculated using Hedges’ g (large 0.8, medium 0.5, small 0.2), which is more robust than Cohen’s d in limited samples.36 Pearson’s r was calculated between the GPCS and the change in the HeiQ scores. The level of statistical significance was set at 5%.
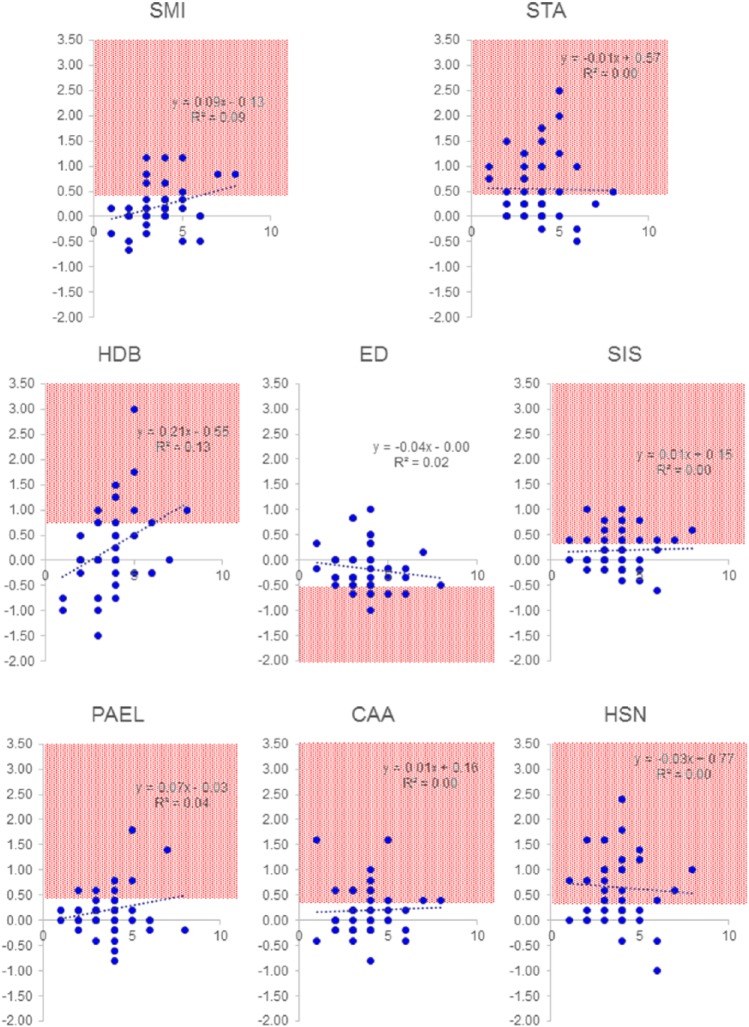
Proportions of participants who exceed the threshold for positive “reliable change” in the HeiQ scores (%> positive “reliable change”) and proportions of participants with the net positive “reliable change” (% net positive “reliable change”) were calculated. The HeiQ established benchmark scores from previous multiple studies with self-management program (n = 3221). The %> positive “reliable change” and the % net positive “reliable change” in this study were descriptively analyzed with those benchmark scores. Furthermore, scatter plots between the number of sessions and change in the HeiQ scores in each of the eight factors were created.
Results
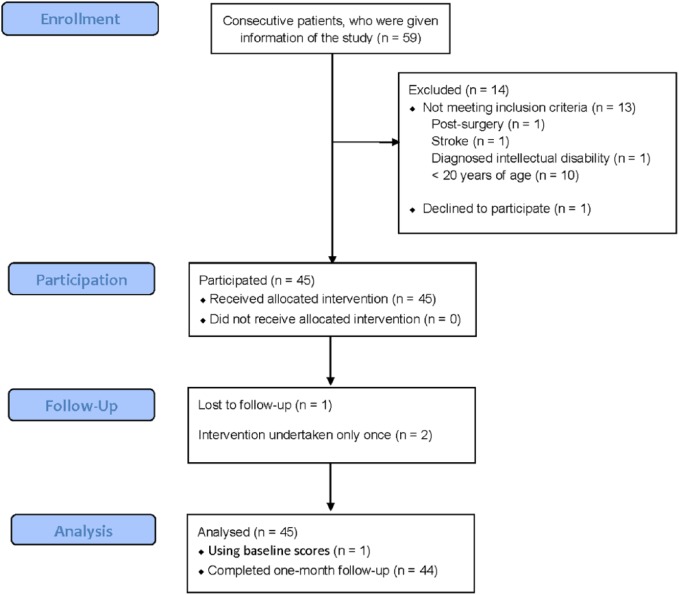
Figure 1 presents a flow of the participants. Recruitment of participants started in February 2016 and ended in August 2016 as the estimated sample size was obtained. One participant did not appear at the third session although their symptoms had been reduced and they had been confident to manage their symptoms by themselves. The follow-up rate was 97.8%. There were no missing data of the HeiQ except in the lost patient. Table 1 presents demographic and basic information.
Figure 1.
Flow of the participants.
Table 1.
Demographic and basic information.
| Age (years), mean (SD) | 43.4 (18.3) |
| Gender, n (%) | |
| Male | 24 (53.3) |
| Female | 21 (46.7) |
| Site of the body part treated, n (%) | |
| Neck | 8 (17.9) |
| Thoracic | 1 (2.2) |
| Back | 27 (60.0) |
| Shoulder | 1 (2.2) |
| Elbow | 0 (0) |
| Wrist–finger | 0 (0) |
| Hip | 2 (4.4) |
| Knee | 4 (8.9) |
| Ankle–foot | 2 (4.4) |
| Symptom duration (months), mean (SD) | 39.3 (83.2) |
| MDT classification, n (%) | |
| Derangement | 37 (82.3) |
| Articular dysfunction | 1 (2.2) |
| Posture | 1 (2.2) |
| Structurally compromised | 2 (4.4) |
| Mechanically inconclusive | 4 (8.9) |
| Number of MDT sessions during the 1 month, mean (SD) | 3.8 (1.4) |
SD: standard deviation; MDT: mechanical diagnosis and therapy.
At the end-point, 32 participants (71.1%) reported clinically meaningful improvement with the GPCS, where 5 patients (11.1%) rated +3 (Completely recovered), 27 patients (60.0%) rated +2, 10 patients rated +1, and 3 patients rated 0 (Unchanged). Table 2 demonstrates the difference between the baseline and the end-point of other outcome measures. The SMI scores improved with a medium effect size and the STA scores improved with a large effect size. Pearson’s r (p-value) between the GPCS and the change in the HeiQ scores was as follows: 0.34 (0.022) in the SMI, 0.023 (0.880) in the STA, 0.135 (0.378) in the HDB, 0.047 (0.760) in the PAEL, −0.234 (0.122) in the ED, 0.267 (0.077) in the CAA, 0.118 (0.439) in the SIS, and 0.253 (0.094) in the HSN, respectively.
Table 2.
Change in the outcome measures through the course of mechanical diagnosis and therapy for 1 month.
| Outcome measures | Baseline (n = 45) | After 1 month (n = 45) | p-Value (95% CIs of the difference) | Hedges’ g |
|---|---|---|---|---|
| SMI-HeiQa,b | 2.5 (0.5) | 2.8 (0.5) | 0.002 (0.1 to 0.3) | 0.59 |
| STA-HeiQa,b | 2.2 (0.6) | 2.8 (0.6) | <0.001 (0.4 to 0.7) | 0.99 |
| HDB-HeiQb | 2.5 (0.8) | 2.7 (0.7) | 0.057 (0.0 to 0.5) | 0.26 |
| PAEL-HeiQb | 2.9 (0.5) | 3.1 (0.5) | 0.007 (0.1 to 0.4) | 0.40 |
| ED-HeiQc | 2.1 (0.6) | 2.0 (0.6) | 0.014 (−0.3 to 0.0) | 0.17 |
| CAA-HeiQb | 2.9 (0.5) | 3.1 (0.5) | 0.007 (0.1 to 0.4) | 0.40 |
| SIS-HeiQb | 2.8 (0.5) | 3.0 (0.5) | 0.002 (0.1 to 0.3) | 0.40 |
| HSN-HeiQb | 1.9 (0.6) | 2.6 (0.6) | <0.001 (0.4 to 0.9) | 1.16 |
| Physical function—SF36b | 83.1 (19.5) | 91.6 (9.7) | 0.001 (−13.1 to −3.8) | 0.55 |
| Role physical—SF36b | 80.0 (23.6) | 90.8 (18.0) | 0.001 (−17.1 to −4.5) | 0.51 |
| Bodily pain—SF36b | 47.6 (19.8) | 67.2 (24.1) | <0.001 (−26.5 to −12.6) | 0.89 |
| General health—SF36b | 60.0 (15.2) | 63.9 (14.0) | 0.014 (−7.0 to −0.8) | 0.26 |
| Vitality—SF36b | 58.2 (22.5) | 67.4 (16.1) | 0.002 (−14.9 to −3.4) | 0.47 |
| Social function—SF36b | 81.7 (26.7) | 90.8 (18.0) | 0.007 (−15.7 to −2.6) | 0.40 |
| Role emotional—SF36b | 81.1 (27.3) | 91.3 (16.1) | 0.002 (−16.5 to −3.8) | 0.45 |
| Metal health—SF36b | 65.4 (14.0) | 70.6 (10.4) | 0.012 (−9.1 to −1.2) | 0.42 |
| P4c | 17.7 (9.8) | 8.3 (7.5) | <0.001 (−12.7 to −6.2) | 1.07 |
CI: confidence interval; SMI: Self-monitoring and Insight; HeiQ: Health Education Impact Questionnaire; STA: Skill and Technique Acquisition; HDB: Health-Directed Behavior; PAEL: Positive and Active Engagement in Life; ED: Emotional Distress; CAA: Constructive Attitudes and Approaches; SIS: Social Integration and Support; HSN: Health Services Navigation; SF-36: Medical Outcomes Study 36-Item Short-Form Health Survey version 2-week.
Primary outcome measures.
A greater score indicates enhanced self-management skill.
A lower score indicates better emotional status.
Table 3 presents the %> positive “reliable change” and the % net positive “reliable change” in this study and benchmark scores. It was likely that the effect of MDT on the HeiQ scores in this study was comparative to previous self-management programs in six factors except the STA and HSN scores. Compared with the previous self-management programs, this study had 1.6–2.0 times greater proportion of the participants with positive “reliable change” in the STA scores and 3.3–6.0 times greater proportion of the participants with positive “reliable change” in the HSN scores.
Table 3.
Proportions of participants who exceed the threshold for positive “reliable change” in the HeiQ scores (%> positive “reliable change”) and proportions of participants with the net positive “reliable change” (% net positive “reliable change”) in this study and established benchmark values.
| Outcome measures | %> Positive “reliable change” |
% Net positive “reliable change” |
||
|---|---|---|---|---|
| This study | Benchmark value | This study | Benchmark value | |
| SMI-HeiQa | 22.2 | 20.5 | 13.3 | 14.1 |
| STA-HeiQa | 48.9 | 30.7 | 46.7 | 23.0 |
| HDB-HeiQ | 31.1 | 22.2 | 15.6 | 17.1 |
| PAEL-HeiQ | 20.0 | 21.1 | 15.6 | 16.4 |
| ED-HeiQ | 13.3 | 17.5 | 6.7 | 10.1 |
| CAA-HeiQ | 26.7 | 17.4 | 24.4 | 10.3 |
| SIS-HeiQ | 20.0 | 16.1 | 17.8 | 9.1 |
| HSN-HeiQ | 53.3 | 16.1 | 51.1 | 8.5 |
SMI: Self-monitoring and Insight; HeiQ: Health Education Impact Questionnaire; STA: Skill and Technique Acquisition; HDB: Health-Directed Behavior; PAEL: Positive and Active Engagement in Life; ED: Emotional Distress; CAA: Constructive Attitudes and Approaches; SIS: Social Integration and Support; HSN: Health Services Navigation.
Greater values indicate enhanced self-management skills.
Primary outcome measures.
Figure 2 presents scatter plots between the number of sessions and change in the HeiQ scores in each of the eight factors. Generally, the change in the HeiQ scores did not exceed the positive “reliable change” in the benchmark with one session.
Figure 2.
Scatter plots between the number of sessions and change in the HeiQ scores in each of the eight factors.
SMI: Self-monitoring and Insight; STA: Skill and Technique Acquisition; HDB: Health-Directed Behavior; PAEL: Positive and Active Engagement in Life; ED: Emotional Distress; CAA: Constructive Attitudes and Approaches; SIS: Social Integration and Support; HSN: Health Services Navigation.
Shade area indicates the positive “reliable change” in the benchmark.
X-axis indicates the number of sessions.
Y-axis indicates change in the HeiQ scores.
Discussion/conclusion
This study demonstrated statistically significant improvement in the SMI and STA scores through the course of a 1-month MDT program in individuals with musculoskeletal disorders. Furthermore, it can be assumed that the effect of MDT on the positive “reliable change” in the SMI and STA scores in this study was comparative to or greater than previous self-management programs. These indicate a preliminary evidence that MDT enhances patient’s self-monitoring skills for symptoms/functions and self-management skill for symptoms/problems.
The preliminary evidence will provide a rationale for an RCT and open further investigations in relation to patient education in MDT. It is required to comprehensively investigate whether MDT is a superior approach for enhancing patient’s self-management/self-care skills to other approaches. MDT therapists usually do not use hands-on techniques from the beginning of evaluation and treatments and provide patients opportunities to feel a difference by doing specific exercises. Passive treatments alone using therapists’ hands-on techniques would deprive a chance for patients to realize that patients can manage their symptoms by themselves to some extent and a chance of patient empowerment. Therefore, a promising future study could be an RCT with intervention arms of MDT and a certain approach focusing on hands-on techniques, which will enhance our understanding of important factors to enhance patient education and behavioral modification. As the pre–post change scores in the SMI statistically correlated with the GPCS, it may be possible that enhancing self-monitoring of symptoms and functions is important for allowing patients to recognize improvements.
This study demonstrated statistically significant improvement of the P4 and SF-36v2-week scores. Furthermore, 71.1% of the participants reported the clinically meaningful improvement, which was achieved with an average of 3.8 sessions. These effects are likely to be greater than the effect of general self-management modalities19 and indicate effective management strategy of MDT for musculoskeletal disorders.
The scatter plots between the number of sessions and change in the HeiQ scores in each of the eight factors indicated that the change in the HeiQ scores generally did not exceed the positive “reliable change” in the benchmark with one session. These indicate that only one session is inadequate to enhance patient’s self-management skills. Thus, follow-ups after the initial session are likely to be important not only for confirmation of the classification, progression of loading strategies, and troubleshooting of exercises but also for patient’s education.
Study limitations
This study had at least three limitations. The first limitation is in generalizability of findings. In this study, a convenience sample was used, but almost all eligible patients participated in the study and thus data of this study would reflect the clinical situation. However, this study included limited participants and therapist, outpatients with musculoskeletal disorders in a local hospital, and a solo physiotherapist who passed the MDT diploma clinical training. It could be possible that the specific relationship between the patients and the therapist results in the change in the HeiQ scores and it is uncertain whether credentialed MDT therapists who have not undertaken the MDT diploma program can also achieve the same education of patients. It is also uncertain whether self-management skills measured by the HeiQ are enhanced in other populations, such as in-hospital patients. Further studies will be required including multiple MDT therapists and variety of the patient populations.
The second limitation is that it is uncertain whether MDT classification is associated with the magnitude of the change in the HeiQ scores. Most patients (82.2%) had the MDT classification of derangement. The derangement syndrome has a directional preference, which is a direction of mechanical loading resulting in quick and lasting improvement of symptoms. Therefore, patients with the derangement syndrome may better understand the importance of self-monitoring of symptoms and functions and self-management skills with specific loading exercises than patients with other MDT classifications. It was not considered reasonable to undertake a post hoc analysis due to a very limited number of participants with non-derangement classifications in this study. Further studies with larger samples with non-derangement classifications will be required to investigate the most sensitive populations to MDT in terms of acquiring self-management skills.
The third limitation is in the study design of a single arm before–after study. Therefore, a caution will be required not to overestimate the effect of MDT on the change in patient’s self-management skills due to potential biases of Hawthorne effect and natural recovery for patient’s self-management skills. However, the biases can be compensated to a certain extent by interpreting the pre–post changes with established “reliable change” scores of the HeiQ. At least, this study provides a preliminary evidence that MDT enhances self-reported skills of self-management for musculoskeletal problems and will be a foundation for subsequent studies.
Conclusion
This study found a preliminary evidence that MDT is an effective management strategy for various musculoskeletal disorders and enhances patient’s self-management skills, particularly in the self-monitoring skills for symptoms/functions and the self-management skill for symptoms/problems.
Acknowledgments
The author wishes to acknowledge Dr Stephen May for peer-reviewing this paper prior to submission and Dr Satoru Aoki for assisting inclusion of the patient.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from The Saitama Prefectural University (27018).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
Trial registration: The study is registered at UMIN000020818.
References
- 1. McKenzie R, May S. The human extremities: mechanical diagnosis and therapy. Raumati Beach: Spinal Publications New Zealand Ltd, 2000. [Google Scholar]
- 2. McKenzie R, May S. The lumbar spine: mechanical diagnosis and therapy. 2nd ed. Waikenae: Spinal Publications New Zealand Ltd, 2003. [Google Scholar]
- 3. McKenzie R, May S. The cervical and thoracic spine: mechanical diagnosis and therapy. Raumati Beach: Spinal publications New Zealand Ltd, 2006. [Google Scholar]
- 4. Battie MC, Cherkin DC, Dunn R, et al. Managing low back pain: attitudes and treatment preferences of physical therapists. Phys Ther 1994; 74: 219–226. [DOI] [PubMed] [Google Scholar]
- 5. Ladeira CE, Samuel Cheng M, Hill CJ. Physical therapists’ treatment choices for non-specific low back pain in Florida: an electronic survey. J Man Manip Ther 2015; 23: 109–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Foster NE, Thompson KA, Baxter GD, et al. Management of nonspecific low back pain by physiotherapists in Britain and Ireland. A descriptive questionnaire of current clinical practice. Spine 1999; 24: 1332–1342. [DOI] [PubMed] [Google Scholar]
- 7. Davies C, Nitz AJ, Mattacola CG, et al. Practice patterns when treating patients with low back pain: a survey of physical therapists. Physiother Theory Pract 2014; 30: 399–408. [DOI] [PubMed] [Google Scholar]
- 8. Takasaki H, Saiki T, Iwasada Y. McKenzie therapists adhere more to evidence-based guidelines and have a more biopsychosocial perspective on the management of patients with low back pain than general physical therapists in Japan. Open J Ther Rehabil 2014; 2: 173–181. [Google Scholar]
- 9. Takasaki H, Herbowy S. Immediate improvement in the cranio-cervical flexion test associated with MDT-based interventions: a case report. J Man Manip Ther 2016; 24: 285–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Takasaki H, May S. Mechanical diagnosis and therapy has similar effects on pain and disability as “wait and see” and other approaches in people with neck pain: a systematic review. J Physiother 2014; 60: 78–84. [DOI] [PubMed] [Google Scholar]
- 11. Takasaki H. Agreement of mechanical diagnosis and therapy classification in people with extremity conditions. Phys Ther 2016; 96: 1525–1532. [DOI] [PubMed] [Google Scholar]
- 12. Hiroshi T, Kousuke O, Richard R. Inter-examiner classification reliability of mechanical diagnosis and therapy for extremity problems—systematic review. Musculoskelet Sci Pract 2017; 27: 78–84. [DOI] [PubMed] [Google Scholar]
- 13. May SJ, Rosedale R. A survey of the McKenzie classification system in the extremities: prevalence of mechanical syndromes and preferred loading strategies. Phys Ther 2012; 92: 1175–1186. [DOI] [PubMed] [Google Scholar]
- 14. Rosedale R, Rastogi R, May S, et al. Efficacy of exercise intervention as determined by the McKenzie system of mechanical diagnosis and therapy for knee osteoarthritis: a randomized controlled trial. J Orthop Sports Phys Ther 2014; 44: 173–181. [DOI] [PubMed] [Google Scholar]
- 15. Kaneko S, Takasaki H, May S. Application of mechanical diagnosis and therapy to a patient diagnosed with de Quervain’s disease: a case study. J Hand Ther 2009; 22: 278–284. [DOI] [PubMed] [Google Scholar]
- 16. May SJ. Patient satisfaction with management of back pain. Part 1: what is satisfaction? Review of satisfaction with medical management. Physiotherapy 2001; 87: 4–20. [Google Scholar]
- 17. Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American college of physicians and the American pain society. Ann Intern Med 2007; 147: 478–491. [DOI] [PubMed] [Google Scholar]
- 18. National Guideline Clearinghouse. Guideline for the evidence-informed primary care management of low back pain. Rockville, MD: Agency for Healthcare Research and Quality (AHRQ), 2011. [Google Scholar]
- 19. Oliveira VC, Ferreira PH, Maher CG, et al. Effectiveness of self-management of low back pain: systematic review with meta-analysis. Arthritis Care Res 2012; 64: 1739–1748. [DOI] [PubMed] [Google Scholar]
- 20. Savigny P, Watson P, Underwood M, et al. Early management of persistent non-specific low back pain: summary of NICE guidance. BMJ 2009; 338: b1805. [DOI] [PubMed] [Google Scholar]
- 21. May S. Patients’ attitudes and beliefs about back pain and its management after physiotherapy for low back pain. Physiother Res Int 2007; 12: 126–135. [DOI] [PubMed] [Google Scholar]
- 22. Shorthouse FM, Roffi V, Tack C. Effectiveness of educational materials to prevent occupational low back pain. Occup Med. Epub ahead of print 2016. DOI: 10.1093/occmed/kqw072. [DOI] [PubMed] [Google Scholar]
- 23. Osborne RH, Elsworth GR, Whitfield K. The health education impact questionnaire (heiQ): an outcomes and evaluation measure for patient education and self-management interventions for people with chronic conditions. Patient Educ Couns 2007; 66: 192–201. [DOI] [PubMed] [Google Scholar]
- 24. Morita R, Arakida M, Osborne RH, et al. Adaptation and validation of the Japanese version of the Health Education Impact Questionnaire (heiQ-J) for the evaluation of self-management education interventions. Jpn J Nurs Sci 2013; 10: 255–266. [DOI] [PubMed] [Google Scholar]
- 25. Elsworth GR, Nolte S, Osborne RH. Factor structure and measurement invariance of the Health Education Impact Questionnaire: does the subjectivity of the response perspective threaten the contextual validity of inferences? SAGE Open Med 2015; 3: 2050312115585041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Osborne RH, Batterham R, Livingston J. The evaluation of chronic disease self-management support across settings: the international experience of the health education impact questionnaire quality monitoring system. Nurs Clin North Am 2011; 46: 255–270. [DOI] [PubMed] [Google Scholar]
- 27. Spadoni GF, Stratford PW, Solomon PE, et al. The evaluation of change in pain intensity: a comparison of the P4 and single-item numeric pain rating scales. J Orthop Sports Phys Ther 2004; 34: 187–193. [DOI] [PubMed] [Google Scholar]
- 28. Fukuhara S, Bito S, Green J, et al. Translation, adaptation, and validation of the SF-36 health survey for use in Japan. J Clin Epidemiol 1998; 51: 1037–1044. [DOI] [PubMed] [Google Scholar]
- 29. Fukuhara S, Ware JE, Kosinski M, et al. Psychometric and clinical tests of validity of the Japanese SF-36 health survey. J Clin Epidemiol 1998; 51: 1045–1053. [DOI] [PubMed] [Google Scholar]
- 30. Fukuhara S, Suzukamo Y. Manual of SF-36v2 Japanese version. Kyoto: Institute for Health Outcomes & Process Evaluation Research, 2004. [Google Scholar]
- 31. Kamper SJ, Maher CG, Mackay G. Global rating of change scales: a review of strengths and weaknesses and considerations for design. J Man Manip Ther 2009; 17: 163–170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Preston CC, Colman AM. Optimal number of response categories in rating scales: reliability, validity, discriminating power, and respondent preferences. Acta Psychol 2000; 104: 1–15. [DOI] [PubMed] [Google Scholar]
- 33. van der Roer N, Ostelo RW, Bekkering GE, et al. Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain. Spine 2006; 31: 578–582. [DOI] [PubMed] [Google Scholar]
- 34. Sandvik L, Erikssen J, Mowinckel P, et al. A method for determining the size of internal pilot studies. Stat Med 1996; 15: 1587–1590. [DOI] [PubMed] [Google Scholar]
- 35. Faul F, Erdfelder E, Lang AG, et al. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 2007; 39: 175–191. [DOI] [PubMed] [Google Scholar]
- 36. Fritz CO, Morris PE, Richler JJ. Effect size estimates: current use, calculations, and interpretation. J Exp Psychol Gen 2012; 141: 2–18. [DOI] [PubMed] [Google Scholar]