Abstract
Objective
To elicit patient stakeholders’ experience and perspectives about patient-centred care.
Design
Qualitative.
Setting
A large urban healthcare system.
Participants
Four patient stakeholders who are prostate cancer survivors.
Main outcome measures
Experience and perspectives of patient stakeholders regarding patient-centred care and treatment decisions.
Results
Our patient stakeholders represented a diverse socio-demographic group. The patient stakeholders identified engagement and dialogue with physicians as crucial elements of patient-centred care model. The degree of patient-centred care was observed to be dependent on the situations. High severity conditions warranted a higher level of patient involvement, compared to mild conditions. They agreed that patient-centred care should not mean that patients can demand inappropriate treatments.
Conclusions
An important attribute of patient-centred outcomes research model is the involvement of stakeholders. However, we have limited knowledge about the experience of patient stakeholders in patient-centred outcomes research. Our study indicates that patient stakeholders offer a unique perspective as researchers and policy-makers aim to precisely define patient-centred research and care.
Keywords: Qualitative research, communication, patients, prostate cancer
Introduction
Established as part of the U.S. Patient Protection and Affordable Care Act of 2010, the main objective of the Patient-Centered Outcomes Research Institute is to fund comparative effectiveness research to help stakeholders – patients, caregivers, clinicians, employers, insurers and policy makers – make informed health decisions.1–3 Patient-Centered Outcomes Research Institute emphasises involving patients and stakeholders in the entire research spectrum.2 This model is atypical compared to the investigator-driven approach of traditional clinical research, as it focuses on patient and patient-centred outcomes.1,2
The conceptual model of patient-centered outcomes research presents required elements for patient-centered outcomes research, a way to describe patient-centredness in research.1 Eventually, patient-centered outcomes research depends on patient stakeholders’ involvement to provide accurate reports of their health status.1–5 As part of our Patient-Centered Outcomes Research Institute-funded study, an advisory board consisting of physicians, researchers and four patient stakeholders, who are prostate cancer survivors, was created. In this article, we present the perspective of patient stakeholders regarding the patient-centred care model.
Methods
We recruited four patient stakeholders from outpatient offices of a large, urban health system to participate as advisory board members of our Patient-Centered Outcomes Research Institute funded study. We posed the question: What is a patient stakeholder’s perspective regarding patient-centred care and patient-centred outcomes research? From a list of about 15 broad discussion points, 10 were retained after 2 iterative reviews by the research team. We shared this list with our patient stakeholders to generate a detailed discussion. This study was approved by the University of Pennsylvania’s Institutional Review Board.
Results
Our patient stakeholders represent a diverse socio-demographic group. Patient stakeholder #1 is 71 years old and underwent open radical prostatectomy with subsequent radiation and hormone therapy. Patient stakeholder #2 is 59 years old and received a robotic radical prostatectomy. The 74-year-old patient stakeholder #3 received proton therapy. Finally, patient stakeholder #4 is a 65-year-old retiree who received radical prostatectomy and subsequent radiation treatments. Perspectives of patient stakeholders are summarised in Table 1 and their detailed discussion follows.
Table 1.
Summary of patient stakeholders’ perspectives.
| Themes | Patient stakeholders’ perspectives |
|---|---|
| 1. Views about patient-centred care | • Had not heard of the term ‘patient-centred care’ prior to being part of the research advisory group. It is essentially a focus on the relationship between a physician and a patient. |
| 2. Roles of patients and physicians in patient-centred care | • Two terms describe the roles of patients and physicians: ‘communication’ and ‘transparency’. Different degrees of patient involvement in patient-centred care are warranted depending on the reason for treatment. |
| 3. Patient stakeholders in patient-centered outcomes research | • Involving patients from the beginning and engaging them as active members of the investigative team offers a unique advantage. |
| 4. Acceptability of patient-centred care | • Increased long-overdue popularity of patient-centred care is warranted. |
| 5. Harms and benefits of patient-centred care | • No obvious harms noted. Physicians must determine whether the patient is capable and has the information needed to make a good treatment decision. |
| 6. Impact of patient-centred care on the quality of care | • Quality of care can improve if a patient has a say in his treatment. It can lead to increased satisfaction with the treatment decision and less regret. |
| 7. Role of patients in decision-making | • A more central role for patient is desired in decision-making. Patient must be presented with all treatment options and complications/side-effects. |
| 8. Experience and opinion in participating patient-centered outcomes research | • Positive experience with being a part of the research advisory board. Primary reason for participation was being able to help prostate cancer patients in the future. |
| 9. Recommendation for patient-centered outcomes research | • Direct recruitment of patients for research advisory board or study participation from doctor’s offices can be more beneficial than community outreach events or seminars. |
| 10. Impact of patient-centred care on cost | • Cost may be decreased using this approach as patients will be able to pick a possibly timelier, cost-conscious, or less invasive option when presented with all treatments. However, it is possible that cost will not be affected if the patient has medical insurance. |
Extent of knowledge
None of the patient stakeholders had a prior understanding of the terms ‘patient-centred care’ or ‘patient-centred outcomes research’. ‘I had seen brochures and pamphlets in my doctor’s offices, but it didn’t make me interested in the subject or make me want to know more … I just glanced at them while I waited’ (Patient stakeholder #4). Patient stakeholders agreed that patient-provider relationship is the foundation of patient-centred care.
Roles defined
Per our patient stakeholders, two words characterise the roles of providers and patients – transparency and communication. Patients need to be honest and transparent and the providers need to make sure that patients can trust them. As in any relationship, without good communication, the relationship does not go far. The provider is responsible for explaining all treatment options and their ramifications, without being biased.
This process of information exchange is vital for an informed consent as the idea of consent assumes that an adult patient has the capacity and competency to make a voluntary, well-informed and reasonable treatment choice, including that of no treatment, to suit his specific circumstances, based on the available information. However, it should also be noted that this concept may not be fully applicable for certain patient situations such as children, patients without capacity, etc. Our patient stakeholders strongly felt that complete communication between patient and provider is an essential component of the patient-centred care model.
Experience
Our patient stakeholders examined their own experience of prostate cancer care. The options and what to expect were explained, and ultimately the treatment choice was up to them. However, reaching a decision was confusing. There was a lot to consider and this led to a feeling of being overwhelmed. One of the patient stakeholders visited several doctors, but this only added to his confusion when each suggested a different treatment related to his/her expertise.
The surgeons told me to go for surgery, the urologists that don’t do surgery told me to take hormone therapy, and the radiation oncologist said that radiation was the best treatment for me, and they don’t tell you what the other options are. (Patient stakeholder #2)
Informed decisions
Our patient stakeholders noted that there is a lot of information on the internet, but not on telling a patient how to make a choice.
I had read about things like radiation seeds and watchful waiting on the government websites, and different types of prostate removal surgery on another site, and that’s all I could find. I felt as though I was obviously not hunting in all the right directions. Specifically, I wanted information on ‘after treatment, this is what you’re going to face in life’, and by ‘this’, I am speaking of the side effects that came with his particular treatment plan. (Patient stakeholder #2)
Unanimously, the patient stakeholders agreed that discussion of post-treatment side-effects was crucial for informed decision-making.
Satisfaction with outcome
Although I was satisfied with the treatment I received and would probably pick the same treatment if I had to do so again, I would have liked more information regarding side effects. This would have made me more prepared for the type and severity of the side effects that I experienced. (Patient stakeholder #2)
Specifically, patients are told that they might experience some urinary incontinence and erectile dysfunction, but not about its severity and effects on daily life.
I was not envisioning if I coughed, stood up, or sat down, it would happen. If I knew of these specific things, I could have been better prepared and also more accepting of these side effects, thus making it easier to cope. (Patient stakeholder #2)
When my doctor presented my treatment plan, it was done with rosy-coloured glasses. I do not think that the doctor presented complete information in regards to side effects either. I was told that I would have some sexual dysfunction but not a complete loss of it. (Patient stakeholder #3)
Our patient stakeholders thought that though doctors tend to give limited information about the side-effects, if a patient thinks that a certain side-effect or outcome is life changing, he will work to alleviate it.
Knowing of the possibility of incontinence after surgery, I was more cognizant regarding the importance of doing Kegel exercises before surgery and relentlessly after to avoid the side effect as much as possible. Because of those measures, I do not have many complications and am satisfied with my decision. (Patient stakeholder #1)
Thus, prior to treatment, a patient must have necessary information to prepare physically and mentally for the post-treatment outcomes.
Advisory board experience
The reason our patient stakeholders wanted to be involved was to help future patients. For some, it was relatively easy to get involved, whereas others took a while to get on board. They believed that involvement in the research advisory board was more beneficial than community outreach events and online community support groups. ‘To get more people involved, you can have a slip asking to be part of an advisory group in the bunch of papers that you have to fill out every time you go to the doctor’s office’ (Patient stakeholder #3).
Moving forward with the patient-centred care model
Patient involvement can enhance the quality of care. However, our patient stakeholders agreed that we need to be careful and consider following questions: Where are the patients getting their information from? What are they centring it on? The problem with the patient-centred care model is patients demanding inappropriate care. Patients differ in their willingness and ability to be involved, and thus the physicians have to help them reach the appropriate decision.
Discussion
As perceived by our patient stakeholders, patient-centredness revolves around a theme of respect, and dialogue between physician and patient. Instead of care being centred on one particular individual, be it patient or provider, it must be viewed as a collaborative process. Patients want to be involved in treatment decisions, not simply told what to do. However, this does not imply that the physician and patient are equal in terms of health knowledge. Apprehensions about the patient-centred care model arise from concerns that patients may want complete control over decisions, even if they lack sufficient information. However, our patient stakeholders strongly believed that most patients understand that it is the physician’s role to provide high-value care and minimise treatment harms. Therefore, patient–physician communication and trust are imperative for making informed decisions together.
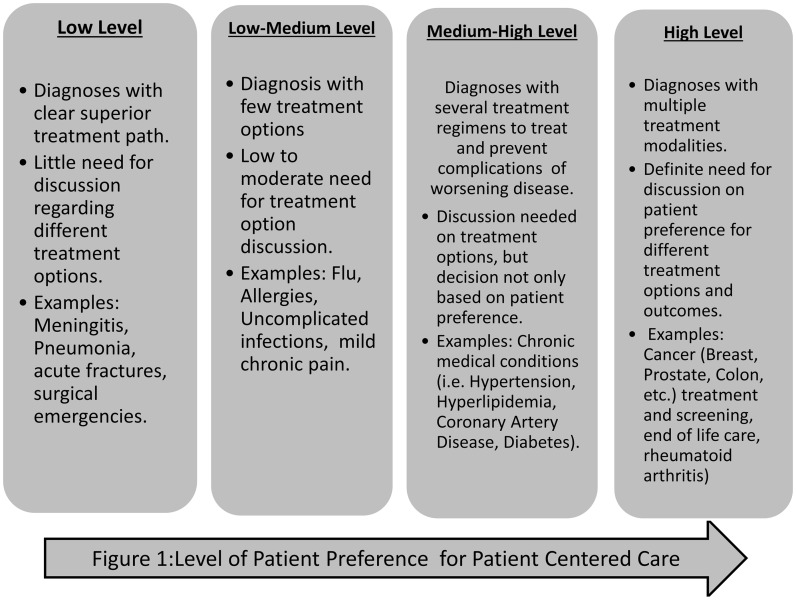
As shown in Figure 1, for some health conditions, treatment options are limited and the patient’s individual preferences play a minor role in treatment decisions. For diseases that involve several possible treatment paths, as in many cancers, all treatment options, including no treatment, should be presented, taking the patient’s needs and values into consideration.6
Figure 1.
Level of patient preference for patient-centred care.
Patients are increasingly engaged in the planning and conduct of biomedical research.5 However, one of the barriers to understanding and implementing the patient-centred care model is the lack of evidence regarding patients’ views and perspectives about this model.7,8 Therefore, our manuscript makes an important contribution by providing a depiction of how patient stakeholders view the patient-centred care model.
Acknowledgements
The authors would like to thank the patient stakeholders.
Declarations
Competing Interests
None declared.
Funding
The study was funded by Patient-Centered Outcomes Research Institute, CE-12-11-4973.
Ethical approval
This study was approved by the University of Pennsylvania Institutional Review Board.
Guarantor
RJ.
Contributorship
All authors made substantial contribution to the design and analysis and critically revised and approved the article.
Provenance
Not commissioned; peer-reviewed by Philemon Gukop.
References
- 1.Frank L, Forsythe L, Ellis l, Schrandt S, Sheridan S, Gerson J, et al. Conceptual and practical foundations of patient engagement in research at the Patient-Centered Outcomes Research Institute. Qual Life Res 2015; 24: 1033–1041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Costlow MR, Landsittel DP, James AE, Kahn JM, Morton SC. Model for a patient-centered comparative effectiveness research center. Clin Trans Sci 2015; 8: 155–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Frank L, Basch E, Selby JV. The PCORI perspective on patient-centered outcomes research. JAMA 2014; 312: 1513–1514. [DOI] [PubMed] [Google Scholar]
- 4.Bardes CL. Defining ‘patient-centered medicine’. N Engl J Med 2012; 366: 782–783. [DOI] [PubMed] [Google Scholar]
- 5.Selby JV, Forsythe L, Sox HC. Stakeholder-driven comparative effectiveness research: an update from PCORI. JAMA 2015; 314: 2235–2236. [DOI] [PubMed] [Google Scholar]
- 6.Barry MJ, Edgman-Levitan S. Shared decision making – the pinnacle of patient-centered care. N Engl J Med 2012; 366: 780–781. [DOI] [PubMed] [Google Scholar]
- 7.Haywood K, Brett J, Salek S, Marlett N, Penman C, Shklarov S, et al. Patient and public engagement in health-related quality of life and patient-reported outcomes research: what is important and why should we care? Findings from the first ISOQOL patient engagement symposium. Qual Life Res 2015; 24: 1069–1076. [DOI] [PubMed] [Google Scholar]
- 8.Absolom K, Holch P, Woroncow B, Wright EP, Velikova G. Beyond lip service and box ticking: how effective patient engagement is integral to the development and delivery of patient-reported outcomes. Qual Life Res 2015; 24: 1077–1085. [DOI] [PubMed] [Google Scholar]