Abstract
Medial knee pain can originate from both osseous and non-osseous soft tissue structures including medial collateral ligament (MCL), creating a raft for patients’ sufferings. Previously published works demonstrated MCL calcification as a rare medial knee pain entity. Alongside physical examination, radio-imaging techniques, namely conventional X-ray, CT/MRI scanning, etc. have been reported to be useful in recognizing MCL calcification. The present study demonstrates MCL calcification in a 60-year-old Asian-Bangladeshi woman, using high frequency diagnostic ultrasonogram and is the first reported study in the literature. To have available literature review, PubMed, Cochrane, Embase, and Scopus databases were used.
Keywords: Medial collateral ligament, calcification, knee pain
Introduction
The medial collateral ligament (MCL) adheres to the medial surface of the femoral condyle to that of the tibia. The MCL comprises two distinct layers: the superficial MCL (sMCL) and deep MCL (dMCL). The dMCL has been further divided into two fragments: the proximal half (meniscofemoral ligament) and the distal half (meniscotibial ligament) (1). However, in the literature, the focus has been on the sMCL, which has been identified as a medial knee ligament, connecting tibia with adjoining femur. The MCL has a triangular shape. It works as a static knee stabilizer against valgus rotation of the knee joint; hence, it prevents separation of medial tibia and femoral condyles following a blow outside the corresponding knee (2).
The MCL is one of the most commonly injured ligamentous structures of the knee joint, particularly during sports such as ice hockey, skiing, and football (3). Nevertheless, in the preceding works, perpetuated calcification has been reported with both traumatized and non-traumatized MCL (4). Besides physical examination, conventional X-ray for knee alone (5) or computed tomography (CT)/magnetic resonance imaging (MRI) scanning was reported to be sufficient for diagnosing MCL calcification (6).
Since MCL calcification is not a frequent knee pain manifestation, exclusion of other confusing clinical mimicries is of paramount importance. Here, in this report, we describe a well-circumscribed calcific deposit in the left femoral condylar attachment of MCL using high frequency ultrasonography (linear probe-10 MHz, Chison CEO1, PR China), reported for the first time in medical literature. The deposit was poorly visible on conventional X-ray. The study was conducted in accordance with the Declaration of Helsinki. A literature review was carried out of studies from the PubMed, Embase, and Cochrane databases using the following key words: “soft tissue calcification,” “medial collateral ligament calcification,” “knee calcification,” and “ligament calcification.”
Case report
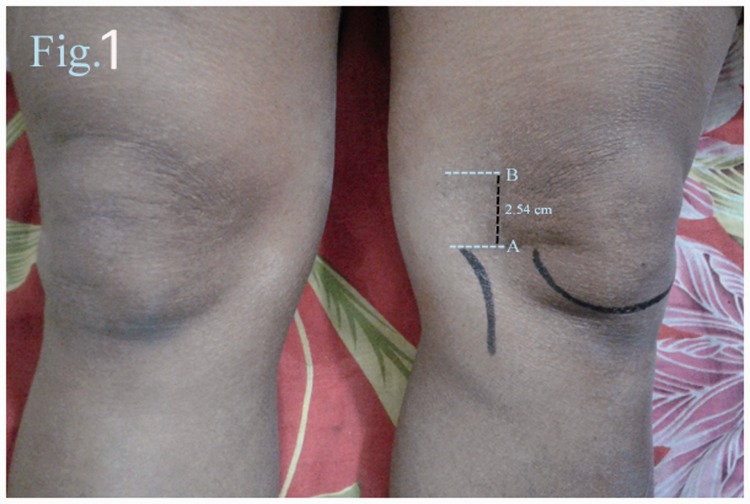
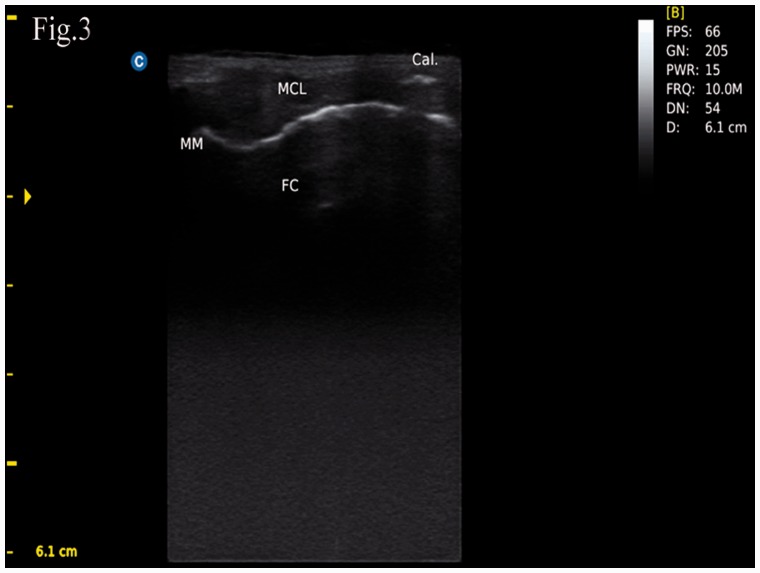
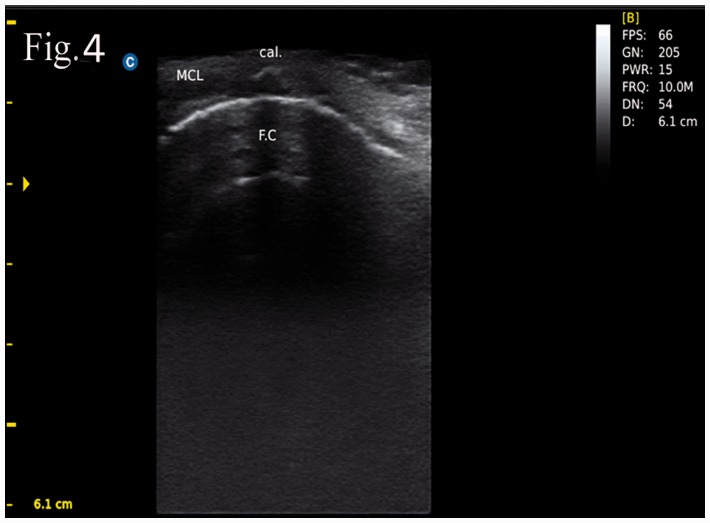
A 60-year-old Asian-Bangladeshi woman presented a complaint of pain in her left knee joint, in particular for its medial aspect, for approximately two months. The pain was aggravated during various daily activities such as standing, sitting, kneeling (while praying), squatting (when using the toilet), ascending and descending stairs, etc. She also felt the discomfort while moving in bed; however, walking relieved some of the pain. There was no joint swelling, knee locking, or audible knee joint sound either. With respect to the patient’s history, she was otherwise healthy two months previously. The symptoms had started when the patient got her left knee stretched after being struck to the pond stairs, with eventual homo-lateral knee pain. On physical examination, she had an antalgic gait and local screening revealed an area of focal tenderness on the medial femoral condyle that was well-localized, 2.5 cm proximal to medial tibio-femoral joint line (Fig. 1). Furthermore, medial collateral ligament stress test was also positive. Clinical examinations revealing synovial fluid such as massage test, fluctuation test, and cross-fluctuation tests were unremarkable. Both the joint line and anserine bursa were neither swollen nor tender. Anterior and posterior drawer tests to observe anterior and posterior cruciate ligaments’ integrity, respectively, were also negative. We further screened the patient’s knee with radiographs and ultrasonogram. X-ray on the left knee (anteroposterior [AP], lateral) revealed patellar osteophytes; however, joint spaces were well-maintained and there was no sclerotic bony change or subchondral cyst in either component of the tibio-femoral joint (Fig. 2). Longitudinal ultrasonogram scanning of medial tibio-femoral joint (using linear probe-10 MHz, Chison CEO1, Guangdong, PR China) revealed a well-circumscribed hyperechoic lesion with posterior acoustic shadowing at the femoral condylar attachment of the medial collateral ligament (MCL) (Figs. 3 and 4). In addition, osteophytic lipping and sclerotic changes were documented in both femoral and tibial condyles; there was minimal collection in supra-patellar recess as well. We did not find any synovial proliferation or double contour sign favoring crystal-induced arthropathy, such as gout. She was non-diabetic and non-hypertensive. After considering all these data, the patient’s clinical entity was diagnosed as “calcification of medial collateral ligament with asymptomatic osteoarthritis of left knee.”
Fig. 1.
Image of both knees: (A) dotted line indicates area of left medial tibio-femoral joint line; (B) dotted line refers to an area of digital tenderness (2.54 cm away from A line).
Fig. 2.

X-ray left knee (antero-posterior view). Asterisk (*) indicates an area of radiological opacification at femoral condylar attachment of medial collateral ligament.
Fig. 3.
Ultrasonographic appearance of hyperechoic calcific deposit in femoral condylar attachment of left medial collateral ligament. Cal, calcification; MM, medial meniscus; MCL, medial collateral ligament; FC, femoral condyle.
Fig. 4.
Ultrasonographic appearance of hyperechoic calcific deposit in femoral condylar attachment of left medial collateral ligament. Cal, calcification; MCL, medial collateral ligament; FC, femoral condyle.
Discussion
MCL calcification is a very rare clinical entity. Clinical scenarios that are often confused with this medial knee pain variety are osteoarthritis (OA) of the tibio-femoral joint (TFJ), medial plica syndrome, anserine syndrome, medial meniscus tear, semi-membranosus tendinitis (SMT), fibromyalgia, Pellegrini Stieda disease, and others (7–11).
Besides medial knee pain, joint line tenderness, joint space narrowing, tibio-femoral condylar osteophytes, bony sclerosis, and subchondral bone cyst are associated with OA-TFJ. Inner aspect knee pain, joint swelling, and joint locking are unique to medial meniscus tear. In medial plica syndrome, plica—a redundancy of the joint synovium, develops medially causing acute medial knee pain in patients after irresistible usual activities.
Anserine syndrome, a condition of infero-medial knee pain originating from either overused anserine tendon and or inflamed underlying bursa, is frequently misdiagnosed and treated inappropriately as of knee joint sourced clinical entity, generating diagnostic dilemma as well (7,8). Similar is the case with SMT, with or without semi-membranosus bursitis; though prevalent in young athletes, the condition has also been documented in middle-aged to older patients (11). In addition, secondary SMT can be seen in OA knee (result from osteophytic irritation of adjacent semi-membranosus tendon) and following total knee replacement (11). A focal area of tenderness near the knee, just proximal to the joint line, is also included in the fibromyalgia classification criteria (10). In Pellegrini Stieda syndrome (9,12), patients usually complain of distal medial thigh pain. Knee joint pain, due to avulsion fracture of medial femoral condyle at the insertion of proximal portion of medial collateral ligament, is another differential diagnosis of medial knee pain. All these possibilities were excluded in our evaluation.
Soft tissue calcification in the form of tendinitis is frequent in shoulder and supraspinatus tendon (80%) is the most commonly involved site. After the shoulder, the hip is the second frequent location for tendinitis followed by the elbow, wrist, hand, and ankle/foot. In the knee, calcification is frequent near osseous attachments of the ligaments or the popliteal tendon (12). Since the patient in this study did not have any systemic or focal knee ailment, previous knee trauma with subsequent dystrophic calcification in MCL might potentiate the patient’s suffering. According to the literature, it takes about 2–6 weeks to develop post-traumatic calcific deposit (12); however, in the present study, the patient reported two months after the incident.
Soft tissue calcification can occur in the following conditions: tissue injury, chondrocalcinosis, hyperparathyroidism, renal failure (following chemo-radiotherapy), injection granulomas, tumoral calcinosis (soft tissue over joints), calcific tendinitis, soft tissue osteosarcoma, metastatic osteosarcoma, dermatomyositis, CREST (calcinosis, Raynaud phenomenon, esophageal dysmotility, sclerodactyly, and telangiectasia) syndrome, and sarcoidosis, cysticercosis (rice-grain calcification) (13). However, the most common condition is of dystrophic variety, which develops when tissues get injured, being often microscopic; nonetheless, it can be apparent on radiographic examination (13).
Digital tenderness over the medial femoral condyle favors MCL calcification diagnosis. Alongside clinical examination, radio-imaging approaches help in evaluating medial knee pain. Till date, calcific deposit in MCL has been surfaced in six clinical reports (Table 1). Kamawal et al. documented MCL calcification using both conventional X-ray and MRI of knee (12). Chang et al. also depicted the condition using both technologies (4). In an interesting report, Gokcen et al. described the condition using both X-ray and CT/MRI scanning simultaneously, in a young man who experienced knee disarticulation (14). Song et al. carried out a similar study on a 46-year-old woman (6). Muschol et al. reported that mere conventional knee X-ray was enough for diagnosing knee MCL calcification (5). Nevertheless, in a recent work, Vampertzis et al. (15) demonstrated MCL calcification in a patient with asymptomatic knee OA as in our study.
Table 1.
Published reports documenting medial collateral ligament calcification.
| Report | Patients (n)/ sex | Preceding trauma event | Methods of evaluation | Methods of treatment |
|---|---|---|---|---|
| Muschol et al. (5) | 5, age range between 55 and 66 year | Not mentioned | Clinical examination, conventional X-ray | 1, Conservative 4, open resection |
| Chang et al. (4) | 1, 72-year-old F | No previous trauma event | Clinical examination, MRI, conventional X-ray knee | Surgical removal |
| Song et al. (6) | 1, 46-year old F | Not mentioned | Clinical examination, CT, MRI, conventional X-ray | Arthroscopic excision of calcific deposit |
| Gokcen et al. (14) | 1, 31-year-old M | Motor vehicle accident/ knee disarticulation | Clinical examination, MRI, CT, conventional X-ray | Not mentioned |
| Kamawal et al. (12) | 1, 50-year-old F | Not mentioned | Clinical examination, MRI, conventional X-ray knee | Surgical removal |
| Vampertzis et al. (15) | 1, 69-year-old F | No preceding trauma | Clinical examination, MRI, conventional X-ray knee | Surgical removal |
Considering its wide margin of safety in terms of radiation exposure, recently diagnostic utility of ultrasonography in various musculoskeletal conditions including soft tissue rheumatisms has increased. Although MRI is a valuable tool in delineating meniscal tears, ligamentous injury, and soft tissue calcification, it may provide clinically irrelevant information, though not related to the patients' symptoms at all, increasing healthcare cost further (12,16). MRI exposure also contraindicates in patients with metal implants, such as cardiac pacemakers (17). However, in the absence of physical signs negative for meniscal tears and cruciate ligament injuries, MRI is not warranted; an important reason why we did not examine this in the present study. On the other hand, diagnostic ultrasound is cost-effective and there is a real-time assessment option available to visualize structure under study as well. Sometimes, conventional X-ray is enough to figure out MCL calcification (5); however, it is even more apparent on ultrasonogram (17) as observed in our patient. To the best of our knowledge, this study is the first to report this procedure in a medical literature.
Non-steroidal anti-inflammatory drugs (NSAIDs) and analgesics are the cornerstone of the MCL calcification treatment (12). If they fail, a shockwave therapy-dry needling-local corticosteroid injection regime can be employed (12). However, open resection or image-guided aspiration of calcific mass, sometimes, may be required even in acute cases (4–6,12). Here, for our study patient, intralesional steroid injection provided patient’s pain relief, making surgical intervention unnecessary.
In conclusion, while performing medial knee pain evaluation, physicians should consider the possibility of MCL calcification. Nonetheless, searching calcification within the MCL through MRI scanning is useful, cost-effective high-frequency ultrasonogram can serve as an alternative option for evaluating MCL pathology, preferably where the healthcare facility does not accommodate MRI.
Declaration of conflicting interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
This research received no specific grant from any funding body in the public, commercial, or not-for-profit sectors.
References
- 1.Liu F, Yue B, Gadikota HR, et al. Morphology of the medial collateral ligament of the knee. J Orthop Surg Res 2010; 5: 69–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.LaPrade RF, Moulton SG, Nitri M, et al. Clinically relevant anatomy and what anatomic reconstruction means. Knee Surg Sports Traumatol Arthrosc 2015; 23: 2950–2959. [DOI] [PubMed] [Google Scholar]
- 3.Phisitkul P, James SL, Wolf BR, et al. MCL injuries of the knee: current concepts review. Iowa Orthop J 2006; 26: 77–90. [PMC free article] [PubMed] [Google Scholar]
- 4.Chang WC, Huang GS, Lee CH, et al. Calcification of medial collateral ligament of the knee: an uncommon cause of medial knee pain. J Clin Rheumatol 2006; 12: 204–205. [DOI] [PubMed] [Google Scholar]
- 5.Muschol M, Muller I, Petersen W, et al. Symptomatic calcification of the medial collateral ligament of the knee joint: a report about five cases. Knee Surg Sports Traumatol Arthrosc 2005; 13: 598–602. [DOI] [PubMed] [Google Scholar]
- 6.Song K, Dong J, Zhang Y, et al. Arthroscopic management of calcific tendinitis of the medial collateral ligament. Knee 2013; 20: 63–65. [DOI] [PubMed] [Google Scholar]
- 7.Calmbach WL, Hutchens M. Evaluation of patients presenting with knee pain: part II. Differential diagnosis. Am Fam Physician 2003; 68: 917–922. [PubMed] [Google Scholar]
- 8.Helfenstein M, Jr, Kuromoto J. Anserine syndrome. Bras J Rheumatol 2010; 50: 313–327. [PubMed] [Google Scholar]
- 9.Altschuler EL, Bryce TN. Pellegrini–Stieda syndrome. N Engl J Med 2006; 354: e1–e1. [DOI] [PubMed] [Google Scholar]
- 10.Wolfe F, Smythe HA, Yunus MB, et al. The American College of Rheumatology 1990 Criteria for the Classification of Fibromyalgia. Report of the Multicenter Criteria Committee. Arthritis Rheum 1990; 33: 160–172. [DOI] [PubMed] [Google Scholar]
- 11.Ray M, Clancy W, Lemon R. Semimembranosus tendonitis: an overlooked cause of medial knee pain. Am J Sports Med 1988; 16: 347–347. [DOI] [PubMed] [Google Scholar]
- 12.Kamawal Y, Steinert AF, Barthel T. Case report – calcification of the medial collateral ligament of the knee with simultaneous calciifying tendinitis of the rotator cuff. BMC Musculoskelet Disord 2016; 17: 283–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Steewart VL, Herling P, Dalinka MK. Calcification in soft tissues. JAMA 1983; 250: 78–81. [PubMed] [Google Scholar]
- 14.Gokcen N, Kelle B, Kozanoglu E. Intraligamentous Calcification of the medial collateral ligament mimicking Pellegrini-Stieda syndrome in a lower-extremity amputee. Turk J Phys Med Rehab 2015; 61: 70–72. [Google Scholar]
- 15.Vampertzis T, Agathangelidis F, Gkouliopoulou E, et al. Massive non-traumatic calcification of the medial collateral ligament of the knee. BMJ Case Rep 2016; 23: 2016–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pompan DC. Reassessing the role of MRI in the evaluation of knee pain. Am Fam Physician 2012; 85: 221–224. [PubMed] [Google Scholar]
- 17.Blankstein A. Ultrasound in the diagnosis of clinical orthopedics: The orthopedic stethoscope. World J Orthop 2011; 18: 13–24. [DOI] [PMC free article] [PubMed] [Google Scholar]