Abstract
NIOSH-certified N95 filtering facepiece respirators (FFRs) are used in healthcare settings as a control measure to mitigate exposures to airborne infectious particles. When the outer surface of an FFR becomes contaminated, it presents a contact transmission risk to the wearer. The Centers for Disease Control and Prevention (CDC) guidance recommends that healthcare workers (HCWs) doff FFRs by grasping the straps at the back of the head to avoid contact with the potentially contaminated surface. Adherence to proper doffing technique is reportedly low due to numerous factors including difficulty in locating and grasping the straps. This study compares the impact of tabs placed on FFR straps to controls (without tabs) on proper doffing, ease of use and comfort, and reduction of transfer of contamination to the wearer. Utilizing a fluorescent agent as a tracer to track contamination from FFRs to hand and head areas of 20 human subjects demonstrated that there was no difference in tabbed FFR straps and controls with respect to promoting proper doffing (p = 0.48), but did make doffing easier (p = 0.04) as indicated by 7 of 8 subjects that used the tabs. Seven of the 20 subjects felt that FFRs with tabs were easier to remove, while only 2 of 20 indicated that FFRs without tabs were easier to remove. Discomfort was not a factor for either FFR strap type. When removing an FFR with contaminated hands, the use of the tabs significantly reduced the amount of tracer transfer compared to straps without tabs (p = 0.012). FFRs with tabs on the straps are associated with ease of doffing and significantly less transfer of the fluorescent tracer.
Keywords: Contact transfer, doffing, fomite, healthcare worker, N95 FFR, PPE
Introduction
The response to the Ebola outbreak has played a significant role in emphasizing the importance of personal protective equipment (PPE) in the hierarchy of safety measures to protect health care workers (HCWs) from pathogens encountered while administering patient care.[1] The outbreak of Ebola and subsequent infection of HCWs has heightened awareness regarding procedural gaps with the proper use of PPE. The types of PPE used in healthcare including, gowns and aprons, protective facemasks and respirators, goggles and face shields, and gloves provide a barrier between the HCW and potentially infectious materials. The benefits and shortcomings of PPE use in healthcare are not a new topic and have received substantial consideration for other pathogens encountered in healthcare, such as influenza, severe acute respiratory syndrome (SARS), human immunodeficiency virus (HIV), and tuberculosis (TB).[2–5] PPE is the last category in the hierarchy of safety controls which includes training and administrative controls, engineering controls, and work practice controls, and often represents the last line of physical protection for HCW. Despite its importance, proper PPE use and respiratory protection compliance in healthcare is lacking.[6,7] PPE can be difficult to select and use, uncomfortable to wear, and requires adherence to proper donning and doffing procedures.[8] These issues can lead to improper donning and doffing of PPE, which could increase the potential for PPE fomite transmission of pathogens to the wearer.
One of the reasons PPE is difficult to use is the lack of familiarity that HCWs may have with specific protective garments and ensembles. The recommendations for the specific types of PPE required to protect HCWs are based on a multitude of factors, such as the type of patient contact anticipated, the mode of transmission of the pathogen, the virulence of the pathogen, and PPE durability.[9] PPE recommendations can vary depending on the level of precautions being used. According to the Centers for Disease Control and Prevention (CDC) 2007 Guidelines for isolation precautions, transmission-based precautions are used in addition to standard precautions when standard precautions do not completely interrupt the route(s) of transmission.[9] Transmission based precautions are employed for specific pathogens which may be encountered on an intermittent basis, and may leave little opportunity for HCWs to gain experience with the specific protective devices recommended for the specific pathogen based on route(s) of transmission. PPE that is more intuitive to use could help HCWs traverse the PPE learning curve when emergency situations call for heightened precautions.
One type of PPE that is used on an intermittent basis by HCWs is a National Institute for Occupational Safety and Health (NIOSH)-certified N95 filtering facepiece respirator (FFR). The CDC has recommended the use of N95 FFRs as part of isolation precautions for pathogens transmitted via the airborne route, such as TB, and during certain medical procedures for some epidemiologically important organisms such as Ebola.[10,11] FFRs reduce the wearer’s inhalation exposure to infectious particles and restrict the user from touching his/her mouth and nose, which limits opportunities to transfer pathogens from the hands to the mucosa of the wearer. Studies in various workplaces have demonstrated that fit-tested FFRs, when used in a complete respiratory protection program, are effective at reducing inhalation exposures.[12–14] Like many other interventions (e.g., hand washing, vaccination, etc.), the effectiveness of FFRs is ultimately governed by compliance and proper use, including adherence to proper donning and doffing procedures.
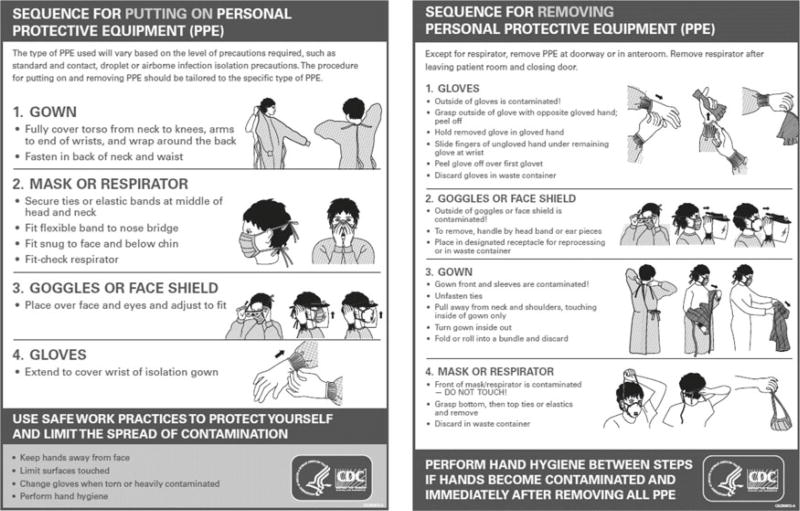
Proper doffing technique is essential to minimize the transfer of infectious materials from PPE to the wearer; however, contact transmission could occur despite following proper use.[15,16] The outer surface of the FFR can become contaminated and serve as a source of pathogens in the contact transmission chain. As detailed in the CDC recommended PPE doffing sequence poster (Figure 1), protective facemasks are the final piece of PPE to be removed and should be removed by grasping the tethering straps at the back of the head. Doffing the FFR by grasping the straps posteriorly allows the wearer to avoid making contact with the potentially contaminated filtering surface of the FFR. Unfortunately, adherence to proper FFR doffing technique is lacking.[17–19] Additionally, a HCWs hands can become contaminated while properly removing other types of PPE such as goggles, facemasks, and gowns. As FFRs and facemasks are the final devices to be removed as outlined in the recommended sequence of PPE doffing, it is possible that contamination can be spread to the head and neck area of the wearer even if the protective facemask is removed using proper technique.
Figure 1.
CDC recommended donning (left) and doffing (right) procedures.
Many potential barriers to proper use of PPE have been identified including deficiency of knowledge, lack of accountability for noncompliance and time constraints.[20] The current design of FFRs is often cited as one of the primary causes of discomfort and unwillingness to properly use and doff the respirator.[21] The FFR straps at the back of the head can become embedded within the wearer’s hair which makes them difficult to find and grasp. Modifications to current FFR strap design might promote proper doffing by making the straps more accessible and easier to grasp.
In this study we aimed to assess the utility of the tabs that are attached to the straps of FFRs in decreasing potential contamination transfer and discomfort during doffing. The purpose of the tabs is to provide an easily accessible “handle” to allow the HCW to remove the FFR without touching its contaminated surfaces, while also minimizing uncomfortable and potentially hazardous contact of the fingers with the hair. Additionally, the tabs could serve as a visual and tactile reminder to use proper FFR doffing technique (i.e., remove the FFR using only the straps).
Methods
Subjects
The study was approved by the National Institute for Occupational Safety and Health (NIOSH)human subjects review board, and all subjects provided oral and written informed consent. A total of 20 subjects between the ages of 18–60 were recruited for this study. Participants currently employed as a HCW, enrolled in a respiratory protection program, and experienced in wearing an FFR were preferred. However, a potential subject was not excluded if all of these qualities were not met. Participants with a history of skin cancer, sensitivity to Ultra Violet (UV) light, or burns from a black light were excluded from the study.
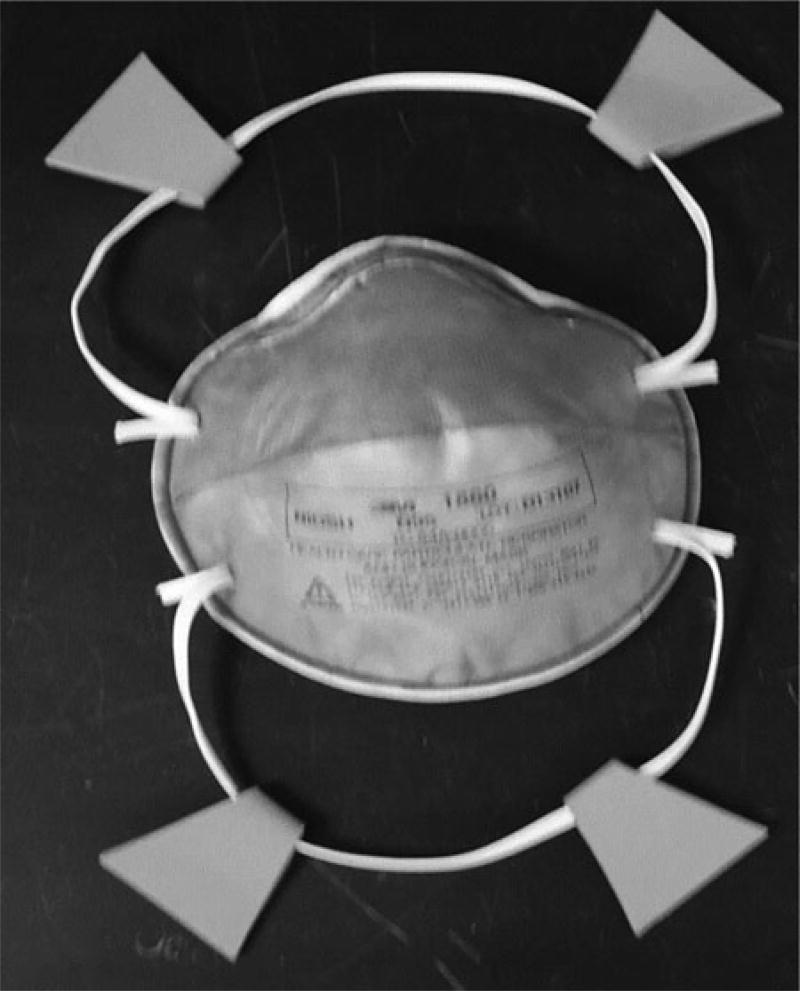
N95 FFR and tab modification
The Model 1860 N95 respirator (3M, St. Paul, MN) used for this study is a NIOSH-approved N95 FFR commonly used by HCWs and is FDA cleared for use as a surgical respirator. Some of the 3 M 1860 FFRs used in this research study were modified by placing 4 red foam tabs on the straps (Figure 2). It is important to note that modifying FFRs in such a manner in the workplace may result in the device being in an unapproved configuration. The use of modified devices should be limited to research and development efforts and not used in devices intended for protection in actual workplaces. The tabs were cut into a “bow tie” shape and folded around the strap to form a trapezoidal shape with a one sided surface area of approximately 11 cm2. The design of the tabs was influenced by a brief search of the literature concerning the effectiveness of warning labels. Based on these studies, we determined that both the color red and triangular shape (truncated to a trapezoidal shape for durability) were two characteristics of warning labels that were readily recognized and recalled.[22–25] The tabs measured 3.81 cm (1.5′) in length; preliminary trials assessing the comfort of grasping the tabs found that area of the tabs was sufficient to accommodate the volar surface of the index and middle finger on one side of the tab and the volar surface of the thumb on the opposite side.[26,27]
Figure 2.
FFR straps with tabs.
Fluorescent tracer
Simulation of contamination transfer was visualized through the use of a non-toxic, UV-light reactive fluorescent tracer. The fluorescent tracer was prepared by suspending 1 g of GloGerm (Glo Germ Company; Moab, UT) powder suspended in 25 mL of mineral oil. To contaminate the FFRs, 7 mL of fluorescent tracer was brushed onto the entire outer surface of the test FFRs. For each subject, six FFRs were contaminated with the fluorescent tracer; three with tabs and three without tabs. As only the outer surface of the FFR was contaminated with the fluorescent tracer, transfer from the FFR to the hands would only occur if the FFR was doffed improperly by grasping the contaminated surface. For the final test conducted by each subject, 1 mL of fluorescent tracer was also applied and rubbed into the hands of the test subject before removal of a clean FFR with or without tabs.
Subject testing procedure
Doffing contaminated FFRs (transfer from FFRs to hands)
To test the utility of the tabs to serve as a reminder to properly doff the FFR and thus limit contamination transfer, a total of six FFR doffings were performed by each subject. Three FFRs with tabs and three FFRs without tabs were tested in random order. Each subject was monitored for the duration of each donning and doffing procedure and all observations were recorded in a laboratory notebook. Each doffing was recorded as either proper or improper. A proper rating was given if the subject utilized either the straps at the back of the head or the tabs connected to the straps of the FFR. An improper rating was recorded if the subject grasped the front surface of the FFR or grasped the straps near the location where the straps attach to the FFR (near the cheek).
The subject received a brief training and education session on proper donning and doffing techniques prior to the start of the test as per the CDC’s donning and doffing recommendation posters (Figure 1). The subjects were not given specific instructions regarding the use of the tabs. The subjects then washed their hands following the World Health Organization (WHO) hand washing protocol[28] and put on a clean pair of nitrile gloves. The subject was instructed to don the first FFR following CDC recommended donning procedures; assistance was provided only if improper technique was used. The subject discarded the gloves using proper technique to minimize contamination transfer to their hands. The subject’s hands were then checked for fluorescent contamination under UVA light. The subject was instructed to wash hands again if any contamination was present. After donning the FFR, the subject completed a computer based simulation of an interaction with an influenza patient. The purpose of the simulation was to remind the subject that he or she was a HCW wearing an FFR in the presence of an infected patient and to provide a distraction so that the subject was not focusing on proper donning and doffing technique. The subject was then instructed to doff the FFR and discard it in a labeled bin. Both the hands and hair were then photographed under UVA light. This procedure was repeated for each of the remaining FFRs.
Proper doffing with contaminated hands (transfer from hands to head)
To assess the ability of the tabs to limit contamination transfer from hands to the head and hair of the wearer while using proper doffing technique, each subject doffed one randomly assigned FFR with or without tabs. Only one FFR type was used for each subject, as it was not practical to have the subject wash their hair and face between trials. Following the WHO protocol, subjects washed hands and then donned the final FFR. 1 mL of fluorescent tracer was aliquoted onto the subject’s palms and the subject rubbed hands together for 30 s to disperse the tracer evenly. The subject was then instructed to properly doff the FFR and to place it in a labeled bin. Photographs were taken under UVA light and the length of the subject’s hair was measured from the back of the head to determine the effect of hair length on FFR comfort and ease of use.
Post-test subject survey (ease of use and comfort)
Each subject was asked to answer a brief, three-question survey regarding comfort and ease of donning and doffing of FFRs with tabs compared to FFRs without tabs.
Imaging and analysis
Fluorescent contamination transfer to the hands or head area of test subjects was captured under UVA lighting (Utilitech Fluorescent Light Fixture TL 8W 05UV Hughesville, PA) with a Nikon D3000 digital still camera (Nikon Corp., Japan). The camera was maintained at a fixed distance of approximately 33 cm from the target surface (hands or head area). The camera shutter speed was fixed at 1/8 s. Photographs were saved to a Secure Digital (SD) memory card on the camera and imported into a desktop computer.
The photographs were analyzed using Adobe Photoshop CS4 version 11 (Adobe Systems Incorporated, San Jose, CA) by quantitatively measuring the intensity/brightness (lumens: brightness or intensity of a light source in a picture) and the surface area of each region of fluorescent contamination. Each image was analyzed in triplicate by using the Lasso tool (in Photoshop) to measure and generate histogram values corresponding to each zone of visual contamination.
Statistical analysis
Characteristics of FFR compliance were analyzed using McNemar’s test to assess the differences in correlation between properly doffing and improperly doffing FFRs with both strap types. Average luminosity values of fluorescent contamination were compared using a two-tailed t-test to test the prediction that there is less contamination transfer present when using tabs on FFR straps. Questionnaire data concerning comfort and ease of use were analyzed using a Fisher’s exact test. A statistical significance was accepted when p < 0.05. The tests were conducted using SPSS software (IBM Corporation, Armonk, New York).
Results
A total of 20 subjects participated in this study and completed the tests: 5 male and 15 female. Seventeen of the 20 subjects had been formally fit tested for N95 FFR use within a year of testing. Only 6 of the subjects responded that they had used an N95 FFR as part of their duties as a HCW.
For the 60 trials involving contaminated FFRs with tabs (examining the transfer from FFRs to hands), 83% of doffings were conducted properly, while 17% were completed using improper technique. Of these 50 occurrences of proper doffing, 25 were performed using the straps even though tabs were present, 21 were conducted using the tabs, and 4 were observed to use a combination of tabs and straps. For the 10 occurrences of improper doffing, 9 were performed by grasping the filtering surface of the FFR, while 1 was conducted by grasping the straps near the location where the straps attach to the FFR. For the 60 trials involving contaminated FFRs without tabs, 87% of doffings could be characterized as using proper technique, while 13% of the trials were completed using improper techniques. For the eight occurrences of improper doffing, seven were performed by grasping the filtering surface of the FFR, while one was conducted by grasping the straps near the location where the straps attach to the FFR. There was no significant difference in occurrence of proper doffing of FFRs with tabs compared to FFRs without tabs (p = 0.4795).
In total, 35% of subjects (n = 20) felt that the respirator with tabs was easier to remove, 10% felt that the respirator without tabs was easier to remove, and 55% of subjects felt that there was no difference in removing each of the respirators. In terms of overall discomfort experienced by the wearer, 80% of the subjects did not experience any discomfort during respirator use; two subjects felt they experienced discomfort using a respirator with tabs, one subject felt there was discomfort using a respirator without tabs, and only one subject reported discomfort in using both types of respirators. Seven of eight subjects, including 5 of the 6 HCWs, that used tabs to properly doff the FFRs, indicated that the FFRs with tabs were easier to remove (p = 0.0387). Of the subjects that felt doffing an FFR with tabs was easier, 86% were females with long hair. The survey questionnaire and results are outlined in Table 1.
Table 1.
Subject questionnaire and results.
| Survey Questions | Responses | |||
|---|---|---|---|---|
| Which Respirator was easier to remove? | a. With tabs | b. Without tabs | c. There was no difference between respirator types. | |
| Results: | 7a/20 (35) | 2/20 (10) | 11/20 (55) | |
| Did you experience discomfort with your hair being pulled while doffing the facemask? | a. Yes | b. No | ||
| Results: | 4/20 (20) | 16/20 (80) | ||
| If you answered yes to the previous question, which respirator were you doffing when you experienced the discomfort? | a. With tabs | b. Without tabs | c. Do not remember | d. Both respirator types |
| Results: | 2/4 (50)b | 1/4 (25)b | 0/4 (0)b | 1/4 (25)b |
Note Numbers in parentheses are percentage.
Subjects used the tabs to doff FFRs.
Represents the percent of participants who answered “yes.”
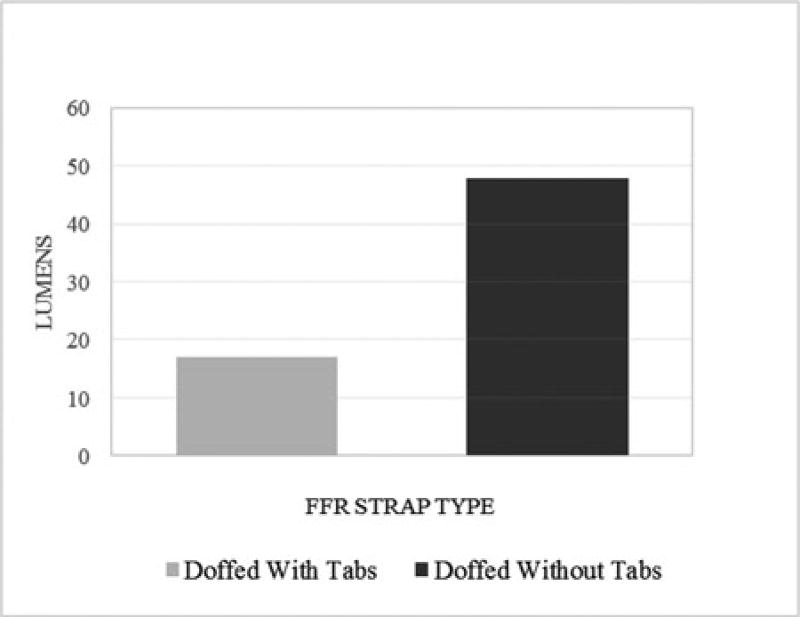
For the 10 trials involving the proper doffing of FFRs with contaminated hands (examining the transfer from hands to the head), 100% of subjects transferred contamination to the head, face, and/or hair areas when FFRs without tabs were used. In contrast, for the 10 trials involving the proper doffing of FFRs with contaminated hands, only 30% of subjects transferred contamination to the head or hair when FFRs with tabs were used. As shown in Figure 3, the average intensity of the amount of fluorescent contamination measured was significantly reduced (p = 0.0002) when tabs were used (55.19 lumens) compared to when not used (97.12 lumens).
Figure 3.
Measured fluorescent contamination from FFRs to the user.
Discussion
In this study we assessed the utility of tabs attached to the straps of FFRs to provide an easily accessible “handle” to allow HCWs to remove the FFR without touching the contaminated filtering surface while minimizing contact with their hair.
We originally proposed to solely test HCWs as they should be accustomed to the protocols and special techniques required to doff FFRs due to the potential contact with infectious pathogens on the filtering surface. However, we were not able to recruit the proposed number of HCWs, thus the testing protocol was amended and approved to allow non-HCWs to participate. The subject pool did consist of 5 males and 15 females, a ratio that accurately reflects the reported healthcare gender distribution.[29] A broader pool of human subject recruits subsequently required a brief training and education session on proper donning and doffing techniques prior to the start of the tests. This factor, along with the absence of typical workplace distractions, may have influenced the rate in which the FFRs were doffed properly (85%), and may not be indicative of what is seen in a healthcare setting, where adherence has been reported at only 43% (respirators were doffed using the straps correctly).[6] The observed high adherence rate to proper doffing technique experienced in this study cannot properly discern the value of the tabs in increasing compliance to proper doffing; however, it demonstrates the value of timely education and training prior to the use of an N95 FFR.
The tabs were created as an extension of the tethering straps to allow the user to more easily locate and grasp the FFR at the back of the head without coincidentally grabbing their hair, thus causing discomfort. Specific mentions of discomfort associated with the straps getting entangled in the hair or inadvertent pulling of the hair when doffing was not an issue identified by the subjects; therefore, the effect on comfort could not be determined. As for ease of doffing, a cursory view of the results suggests that the tabs on the FFR straps did not make doffing easier as most subjects indicated that there was no noticeable difference between the FFRs with tabs and the FFRs without tabs (Table 1). However, all but one of the subjects that used the tabs to doff the FFRs found the tabs to be easier to use (Table 1). Furthermore, the results indicate that the use of tabs may be more helpful in cases of longer hair. As only 8 of the 20 subjects used the tabs, it can be concluded that the use of the tabs to doff FFRs was not intuitive, but as with all PPE and new technologies, training and education are imperative to improve compliance and proper use.
There is a high potential for the hands to become contaminated before removing the FFR. Hands can become contaminated while administering patient care in the event that a HCW is not using gloves.[30–33] Even if HCWs are protecting their hands with the use of gloves, the sequence of proper PPE doffing (Figure 1) dictates that the FFR or mask is the last piece of PPE to be removed. If the hands do become contaminated during the process of PPE doffing, it is easy to remove potential infectious organisms by performing hand hygiene. In fact, the updated CDC recommended procedure and sequence for PPE removal states to “perform hand hygiene between steps if hands become contaminated and immediately after removing all PPE.”[16] Proper hand hygiene compliance in healthcare settings is deficient.[34] Moreover, if pathogens are unknowingly transferred to the head or neck region of the HCW, removal of the pathogens would not occur until the HCW presumably showers after his or her shift. During the time between contamination and contamination removal, the HCW’s head and hair serve as a source of pathogens for further transmission. Using the tabs to doff FFRs reduces the contact between the hands and the hair and head of the wearer, thus minimizing the potential for contact transmission. The tabs did not prohibit all contact between the hands and the hair and head of the subject, especially in cases where the subject’s hair was long or curly; however, proper training and perhaps improved tab design can increase the protective efficacy of the tabs.
Subsequent to the onset of this investigation, a Grand Challenge Partnership (Fighting Ebola: A Grand Challenge for Development) was launched to help HCW provide safe and efficient care to affected individuals and to prevent further spread of the Ebola virus in West Africa. Some of the innovations resulting from the Grand Challenge employed tabs on various forms of PPE as a way to promote easier doffing.[35]
Conclusions
The results of this investigation provide an initial assessment of tabs placed on PPE, particularly FFRs as a means to increase proper doffing technique thereby limiting self-contamination, make PPE more comfortable to use, and reduce contamination transfer from PPE to the wearer even when proper doffing techniques are used. The use of the tabs was not intuitive and it could be concluded that the tabs had little influence in promoting proper doffing technique during this study. However, the tabs did make doffing easier and limited contamination transfer from hands to the head and neck areas when proper techniques were used.
Acknowledgments
The authors wish to express our sincere gratitude to Dr. Raymond Roberge, Dr. Deborah Novak, and Dr. William Lindsley for their suggestions and contributions.
Footnotes
Disclaimer
The findings and conclusions in this manuscript have not been formally disseminated by the NIOSH and should not be construed to represent any agency determination or policy. Mention of any company, product, policy, of the inclusion of any reference does not constitute endorsement by NIOSH.
References
- 1.Fischer WA, Hynes NA, Perl TM. Protecting health care workers from Ebola: Personal protective equipment is critical but is not enough. Ann. Intern. Med. 2014;161(10):753–754. doi: 10.7326/M14-1953. [DOI] [PubMed] [Google Scholar]
- 2.Akduman D, Kim LE, Parks RL, et al. Use of personal protective equipment and operating room behaviors in four surgical subspecialties: personal protective equipment and behaviors in surgery. Infect. Control. 1999;20(02):110–114. doi: 10.1086/501601. [DOI] [PubMed] [Google Scholar]
- 3.Daugherty EL, Perl TM, Needham DM, Rubinson L, Bilderback A, Rand CS. The use of personal protective equipment for control of influenza among critical care clinicians: a survey study. Crit. Care Med. 2009;37(4):1210–1216. doi: 10.1097/CCM.0b013e31819d67b5. [DOI] [PubMed] [Google Scholar]
- 4.Loutfy MR, Wallington T, Rutledge T, et al. Hospital preparedness and SARS. Emerg. Infect. Dis. 2004;10(5):771. doi: 10.3201/eid1005.030717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jarvis WR, Bolyard EA, Bozzi CJ, et al. Respirators, recommendations, and regulations: the controversy surrounding protection of health care workers from tuberculosis. Ann. Intern. Med. 1995;122(2):142–146. doi: 10.7326/0003-4819-122-2-199501150-00011. [DOI] [PubMed] [Google Scholar]
- 6.Peterson K, Novak D, Stradtman L, Wilson D, Couzens L. Hospital respiratory protection practices in 6 U.S. states: a public health evaluation study. Am. J. Infect. Control. 2015;43(1):63–71. doi: 10.1016/j.ajic.2014.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Beckman S, Materna B, Goldmacher S, et al. Evaluation of respiratory protection programs and practices in California hospitals during the 2009–2010 H1N1 influenza pandemic. Am. J. Infect. Control. 2013;41(11):1024–1031. doi: 10.1016/j.ajic.2013.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gosch ME, Shaffer RE, Eagan AE, Roberge RJ, Davey VJ, Radonovich LJ. B95: a new respirator for health care personnel. Am. J. Infect. Control. 2013;41(12):1224–1230. doi: 10.1016/j.ajic.2013.03.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Siegel JD, Rhinehart E, Jackson M, Chiarello L, Committee HCICPA. 2007 guideline for isolation precautions: preventing transmission of infectious agents in health care settings. Am. J. Infect. Control. 2007;35(10):S65–S164. doi: 10.1016/j.ajic.2007.10.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention (CDC), National Center for Emerging & Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP) Guidance for the Selection and use of Personal Protective Equipment (PPE) in Healthcare Settings: PPE Use in Healthcare Settings. [accessed April 2015]; Available at http://www.cdc.gov/vhf/ebola/healthcare-us/ppe/guidance.html.
- 11.Centers for Disease Control and Prevention (CDC), National Center for Emerging & Zoonotic Infectious Diseases (NCEZID), Division of Healthcare Quality Promotion (DHQP) Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus Disease in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing) [accessed April 2015]; Available at http://www.cdc.gov/media/releases/2014/fs1020-ebola-personal-protective-equipment.html.
- 12.Han D. Correlations between workplace protection factors and fit factors for filtering facepieces in the welding workplace. Industr. Health. 2002;40(4):328–334. doi: 10.2486/indhealth.40.328. [DOI] [PubMed] [Google Scholar]
- 13.Zhuang Z, Coffey CC, Jensen PA, Campbell DL, Lawrence RB, Myers WR. Correlation between quantitative fit factors and workplace protection factors measured in actual workplace environments at a steel foundry. Am. Indust. Hyg. J. 2003;64:730–738. doi: 10.1202/475.1. [DOI] [PubMed] [Google Scholar]
- 14.Janssen LJ, TJN, Cuta KT. Workplace protection factors for an N95 filtering facepiece respirator. J. Occup. Environ. Hyg. 2007;4(9):698–707. doi: 10.1080/15459620701517764. [DOI] [PubMed] [Google Scholar]
- 15.Casanova L, Alfano-Sobsey E, Rutala WA, Weber DJ, Sobsey M. Virus transfer from personal protective equipment to healthcare employees’ skin and clothing. Emerg. Infect. Dis. 2008;14(8):1291–1293. doi: 10.3201/eid1408.080085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Sequence for Removing Personal Protective Equipment (PPE) [Online] Available at http://www.cdc.gov/hai/pdfs/ppe/PPE-Sequence.pdf.
- 17.Baig AS, Knapp C, Eagan AE, Radonovich LJ., Jr Health care workers’ views about respirator use and features that should be included in the next generation of respirators. Am. J. Infect. 2010;38(1):18–25. doi: 10.1016/j.ajic.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chora JSY, Padab SK, Stephensonc I, et al. Differences in the compliance with hospital infection control practices during the 2009 influenza H1N1 pandemic in three countries. J. Hosp. Infect. 2012;81(2):98–103. doi: 10.1016/j.jhin.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 19.Mitchell R, Toju Ogunremi M, Astrakianakis PG, Bryce ME, Gervais MR, Gravel BD, et al. Impact of the 2009 influenza A (H1N1) pandemic on Canadian health care workers: a survey on vaccination, illness, absenteeism, and personal protective equipment. Am. J. Infect. Control. 2012;40(7):611–616. doi: 10.1016/j.ajic.2012.01.011. [DOI] [PubMed] [Google Scholar]
- 20.Pyrek KM. Addressing the Challenges of PPE Non-Compliance. [accessed June 3, 2015]; Available at http://www.infectioncontroltoday.com/articles/2011/10/addressing-the-challenges-of-ppe-non-compliance.aspx.
- 21.Locatelli SML, Sherri L, Gosch M. Health care workers’ reported discomfort while wearing filtering facepiece respirators. Workplace Health Saf. 2014;62(7):362–368. doi: 10.3928/21650799-20140804-03. [DOI] [PubMed] [Google Scholar]
- 22.Wogalter MSL, Kenneth R. Warning! Sign and Label effectiveness. Curr. Direct. Physiol. Sci. 1996;5(2):33–37. [Google Scholar]
- 23.Elliot AJ, Maier MA. Color psychology: Effects of perceiving color on psychological functioning in humans. Ann. Rev. Psychol. 2014;65:95–120. doi: 10.1146/annurev-psych-010213-115035. [DOI] [PubMed] [Google Scholar]
- 24.Young SL. Increasing the noticeability of warnings: Effects of pictorial, color, signal icon and border. Proc. of the Human Factors and Ergonomics Society Annual Meeting. 1991;35(9):580–584. [Google Scholar]
- 25.Riley MW, Cochran DJ, Ballard JL. An investigation of preferred shapes for warning labels. Hum. Fact. J. Hum. Fact. Ergonom. Soc. 1982;24(6):737–742. [Google Scholar]
- 26.Murai M, Lau HK, Pereira BP, Pho RW. A cadaver study on volume and surface area of the fingertip. J. Hand Surg. 1997;22(5):935–941. doi: 10.1016/S0363-5023(97)80094-9. [DOI] [PubMed] [Google Scholar]
- 27.Domalain M, Vigouroux L, Danion F, Sevrez V, Berton E. Effect of object width on precision grip force and finger posture. Ergonomics. 2008;51(9):1441–1453. doi: 10.1080/00140130802130225. [DOI] [PubMed] [Google Scholar]
- 28.World Health Organization. WHO Guidelines on Hand Hygiene in Health Care. Geneva, Switzerland: WHO Pess; 2009. [Google Scholar]
- 29.Department of Human Resources for Health. Gender and Health Workforce Statistics. In: World Health Organization, editor. Spotlight on Statistics: A Fact File n Health Workforce Statistics. Geneva, Switzerland: WHO; 2008. [Google Scholar]
- 30.Khodavaisy S, Nabili M, Davari B, Vahedi M. Evaluation of bacterial and fungal contamination in the health care workers? hands and rings in the intensive care unit. J. Prevent. Med. Hyg. 2015;52(4) [PubMed] [Google Scholar]
- 31.Landelle C, Verachten M, Legrand P, Girou E, Barbut F, Buisson CB. Contamination of healthcare workers’ hands with Clostridium difficile spores after caring for patients with C. difficile infection. Infect. Control. 2014;35(01):10–15. doi: 10.1086/674396. [DOI] [PubMed] [Google Scholar]
- 32.Duckro AN, Blom DW, Lyle EA, Weinstein RA, Hayden MK. Transfer of vancomycin-resistant enterococci via health care worker hands. Arch. Intern. Med. 2005;165(3):302–307. doi: 10.1001/archinte.165.3.302. [DOI] [PubMed] [Google Scholar]
- 33.Morgan DJ, Liang SY, Smith CL, et al. Frequent multidrug-resistant Acinetobacter baumannii contamination of gloves, gowns, and hands of healthcare workers. Infect. Control. 2010;31(07):716–721. doi: 10.1086/653201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gould D, Drey N, Moralejo D, Grimshaw J, Chudleigh J. Interventions to improve hand hygiene compliance in patient care. J. Hosp. Infect. 2008;8(3):193–202. doi: 10.1016/j.jhin.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 35.Tricoukes ND, Russell B, Shara K, Good T. PPE Design Retrofit Concepts. [accessed May 2014]; Available at https://d3gxp3iknbs7bs.cloudfront.net/attachments/cbdd3dd1-d4db-40bf-a0d4-5aa6c7a80710.pdf.