Abstract
Background:
Cerebrospinal fluid (CSF) drainage via ventricular puncture is an established therapy of elevated intracranial pressure (ICP). In contrast, lumbar CSF removal is believed to be contraindicated with intracranial hypertension.
Methods:
We investigated the safety and efficacy of lumbar CSF drainage to decrease refractory elevated ICP in a small cohort of patients with traumatic brain injury (TBI). A score (0–8 points) was used to assess computed tomography (CT) images for signs of herniation and for patency of the basal cisterns. All patients received lumbar CSF drainage either as a continuous drainage or as a single lumbar puncture (LP). Type and method of CSF drainage, mean ICP 24 h prior and after CSF removal, and adverse events were documented. Outcome was assessed after 3 months (with dichotomized Glasgow outcome scale).
Results:
Eight patients were evaluated retrospectively. n = 5 suffered a moderate, n = 2 a severe TBI (one Glasgow coma score not documented). The CT score was ≥5 in all patients prior to LP and decreased after puncture without clinical consequences in two patients. The amount of CSF removal did not correlate with score changes (P = 0.45). CSF drainage led to a significant reduction of mean ICP (from 22.3 to 13.9 mmHg, P = 0.002). Continuous drainage was more effective than a single LP. Three of eight patients reached a favorable outcome.
Conclusions:
Lumbar CSF removal for the treatment of intracranial hypertension is effective and safe, provided the basal cisterns are discernible, equivalent to ≥5 points in the proposed new score. The score needs further validation.
Keywords: Intracranial hypertension, intracranial pressure, lumbar drainage, multimodality monitoring, score, traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is a major cause of morbidity and mortality and a leading cause of death with an estimated annual incidence of 262 cases per 100,000 population in Europe.[15] An increase in intracranial pressure (ICP) is one of the key pathogenic mechanisms for the development of secondary brain damage and for poor outcome after TBI.[10,16]
Over the last decades, a standardized, evidence-based staircase approach to treat increased ICP was developed.[2,18] Whereas external ventricular drainage of cerebrospinal fluid (CSF) via frontal burr-hole craniostomy is one established method to reduce intracranial hypertension,[13,19] only a few studies have evaluated the safety and usefulness of lumbar CSF removal in the setting of raised intracranial hypertension.[1,8,12,19] Supratentorial and/or infratentorial herniation remains a major concern under these circumstances.[4,6]
The aim of this pilot study was to analyze imaging changes seen in patients undergoing lumbar CSF removal to treat posttraumatic intracranial hypertension, and to develop a score that would permit to estimate the risk of cerebral herniation associated with lumbar CSF drainage.
MATERIALS AND METHODS
Ethical considerations
All data were collected as part of the routine documentation during the hospital stay and evaluated retrospectively. Subsequent analyses were performed on anonymized data. Therefore, Institutional Review Board approval was waived according to Austrian regulations. We consider the publication of this study in accordance with Art. 37 of the Declaration of Helsinki that “unproven interventions (.) should subsequently be made the object of research. In all cases, new information must be recorded and, where appropriate, made publicly available.”
Study setting
All patients were treated in the neurosurgical intensive care unit of the Neurosurgical Department of the Medical University of Innsbruck, Innsbruck, Austria, a class III trauma center.
Indication for lumbar cerebrospinal fluid removal
The decision to place a lumbar drainage (LD) was based on an interdisciplinary consensus of clinicians with expertise in neurosurgery and neurointensive care. The patients belonged to two groups: (1) they either had already narrow ventricles, so that ventricular puncture was believed to be difficult and/or only of short-term efficacy, or (2) they demonstrated a discrepancy between ICP measured with intraparenchymal devices and morphological findings on CT scans believed to cause elevated ICP, such as diffuse brain swelling.
Procedures
All patients undergoing lumbar CSF removal for the treatment of refractory ICP after moderate or severe TBI between November 2011 and December 2014 were included. All patients had an intraparenchymal ICP monitoring device in place. Recommended guidelines for the care of patients with TBI were followed in all patients. Refractory ICP was defined as ICP >25 mmHg after having received standardized and escalating nonsurgical treatment, according to standard operating procedures (e.g., deepening of sedation, hyperosmolar therapy, and mild hyperventilation) and following the guidelines of the Brain Trauma Foundation.[2] Once medical therapy had failed, lumbar CSF removal was contemplated to avoid an undue prolongation of sedation[5,14] or as an intermediate step prior to proceed with decompressive craniotomy or barbiturate coma.
Lumbar CSF drainage was initiated either by single lumbar puncture (LP) with the patient in the lateral recumbent position, or by placing an intermittently open LD (both referred to as LP), or by placing a continuously open LD. In all patients with a continuous drainage, CSF was drained at the level of the foramen of Monroe. LP was performed between days 1 and 13 after trauma. ICP values and adverse events were recorded. For data interpretation the hourly ICP values of the 24 h preceding and the 24 h following the lumbar CSF access were averaged. Clinical outcome was determined after 3 months using the Glasgow outcome score (GOS), dichotomized into favorable (GOS 4 and 5) and unfavorable (GOS 1–3).
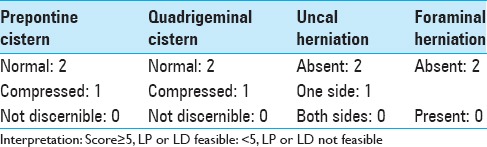
All patients underwent CT scanning within 8 h prior and after LP or LD. Spatial intracranial relationships were evaluated systematically by analyzing the width of the prepontine cistern, the width of the quadrigeminal cistern, and evaluate signs of uncal and/or foraminal herniation. Uncal herniation was defined as either present or absent in case of prolapse of the uncus temporalis below the linea of the upper tentorial margin. Foraminal herniation was defined as the cerebellar tonsil(s) at or below the level of the occipital foramen. A point value was assigned to alterations associated with each item based on empirical grounds [Table 1]. A minimum score of 5 or higher was believed to be necessary to ensure a safe removal of lumbar CSF.
Table 1.
Score to assess the safety of lumbar CSF drainage
Statistical analysis
Standard methods of descriptive and inferential statistics were used. A P value <0.05 was considered statistically significant. Values are expressed as mean ± SD. Unpaired Student's t-test was used to test for significance between groups because all measures were adequately normally distributed. Statistical calculations were performed by using a statistical software package (IBM® SPSS® Statistics, Version 21.0).
RESULTS
Clinical data of eight patients is summarized in Table 2. The average age was 54.1 years (range 27–70 years). Six patients were males (75%). The initial Glasgow coma score (GCS) ranged from 3 to 15. The patients had either suffered severe (n = 2) or moderate (n = 5) TBI. In one patient the initial GCS was not documented. Five patients underwent prior evacuation of an intracranial hematoma either by osteoplastic (n = 2) or by osteoclastic (n = 3) craniotomy.
Table 2.
Demographics and clinical data
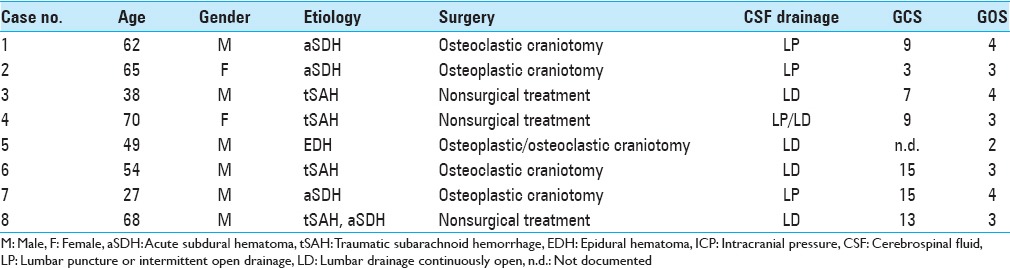
CSF removal via the lumbar route was accomplished by either single puncture/intermittently open drainage (LP, n = 4) or by continuous drainage (LD, n = 5). One patient underwent a single puncture initially and a continuous drainage thereafter.
The amount of CSF removed by either LP or LD was 23.5 ml/24 h (mean, SD 16.41, range 0–40 ml) following lumbar access [Table 3].
Table 3.
CT score prior and after CSF drainage
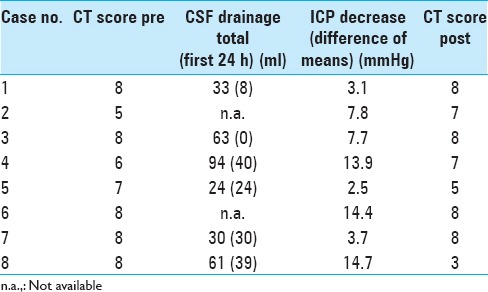
The CT score ranged between a minimum of 5 and a maximum of 8 before starting CSF drainage and between 3 and 8 after CSF drainage [Table 3]. In four patients the score showed no alteration. The score decreased (indicating a reduction of the cisternal space) after CSF drainage in two patients, and increased in two patients. The decrease was without clinical consequences. Narrowing was observed in the prepontine cistern and the quadrigeminal cistern. One patient showed an uncal herniation on both sides after lumbar CSF withdrawal without mydriasis or other clinical signs of cerebral herniation [Table 3]. Regarding the amount of CSF removed within the first 24 h, there was no statistically significant difference between the patients with a worsening of the imaging score (31.5 ml, SD 10.6) and those with a stable or improved imaging score (19.5 ml, SD 18.64, P = 0.45).
Lumbar CSF removal led to a reduction of ICP in all patients [Figure 1; Table 3]. Mean ICP was 22.3 mmHg (SD 3.0) before CSF drainage and was 13.9 mmHg (SD 4.7) after drainage (P = 0.002). A constantly open lumbar CSF drainage was significantly more effective than a single LP [Figure 1]. The ICP decreased by 13.2 mmHg (mean, SD 3.0) with constant drainage and by 2.7 mmHg (mean, SD 1.3) with intermittent open or single LP (P = 0.0003).
Figure 1.
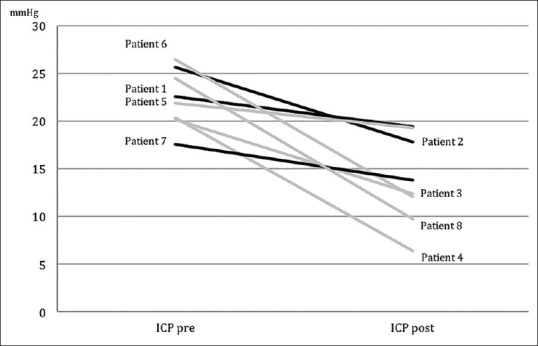
A decrease of the mean intracranial pressure before (ICP pre) and after (ICP post) lumbar CSF removal was observed in all patients. Continuous LD (grey) lowers ICP more effectively than single puncture/intermittent drainage (black). Numbers denote case number [Table 2]
No severe adverse events were registered in association with the procedure in this cohort, especially no clinically evident case of herniation or infection associated with lumbar CSF removal. However, in one patient we observed radiological signs of uncal herniation on one CT scan.
A favorable outcome after 3 months was observed in three patients (37.5%). Four patients attained a GOS of 3, whereas one patient remained in a persistent vegetative state (GOS 2).
DISCUSSION
The main findings of this study are, first, that it is safe to perform lumbar CSF removal in the setting of an increased ICP provided the basal cisterns are discernible and bilateral uncal herniation is absent. Second, the use of a score provides a structured approach to prepuncture image analysis and may add to the safety of the procedure. Third, continuous removal of CSF might be more effective than intermittent drainage.
TBI-related intracranial hypertension is associated with poor outcome.[1] Drainage of CSF in patients with intracranial hypertension is known to be an effective way to decrease ICP.[12,19] However, lumbar CSF removal under these circumstances remains a controversial procedure due to the perceived risk of cerebral herniation and the risk of infection.[4,9] As a matter of fact, we performed the procedure only in selected patients attended in the neurosurgical intensive care unit, where a high level of nursing expertise regarding LD is available, after carefully evaluating all options for ICP management by interdisciplinary discussion.
In agreement with previous studies, we found that under these circumstances lumbar removal of CSF is highly effective and safe in the situation of elevated ICP after TBI.[1,8,11,19] Our data show a clear advantage of the use of a continuous LD as opposed to intermittent drainage or single LP. This is controversial. Nwachuku et al. tested the efficacy of intermittent versus continuous CSF removal via a supratentorial external ventricular drainage. They were able to show that a continuously open external ventricular drain was associated with significantly better ICP control.[13] In contrast, Kim et al.[7] failed to show a difference between intermittent and continuous drainage in the setting of subarachnoid hemorrhage.
In our opinion, the most important step when evaluating a patient as a potential candidate for LD in the setting of an elevated ICP is the careful analysis of CT scans. Prior studies did only partially elaborate on this point.[1,8,11,19] By assigning a point value to the visibility of the basal cisterns and to the imaging signs of uncal and foraminal herniation, a structured approach to image analysis was accomplished with acceptable clinical results. Whether the score presented here, tentatively called the “Innsbruck Intracranial Reserve Score,” is able to distinguish patients in whom LP is feasible from those in whom this may not be the case, remains to be validated in internal as well as external prospective studies.
Although not statistically significant in our small, retrospective patient series, the amount of CSF removed via the lumbar route may play a role in patients whose imaging score worsened. We suggest that the lowest amount that effectively reduces the ICP should be removed. Future studies need to elaborate on this aspect.
We did not record any infection associated with lumbar CSF drainage. LD, especially when performed as a continuous drainage, might be associated with an increased risk of CSF infection.[3] However, Schade and Schinkel[17] reported that the risk of infection with continuous lumbar CSF drainage and the infection-associated death remains low.
This study has limitations. The sample size is small and data analysis is retrospective. We therefore limited our analysis to the immediate effects of lumbar CSF removal on the ICP course. Whether this influenced the clinical outcome remains highly speculative.
CONCLUSION
Lumbar CSF drainage represents an efficient and safe treatment to reduce intracranial hypertension, provided the images prior to LP are carefully analyzed, the right conclusions are drawn, and nursing expertise in handling of the drainage is guaranteed. The newly introduced “Innsbruck Intracranial Reserve Score”, an image-based score to predict the safety of lumbar CSF drainage, needs further validation in a larger prospective trial before its use can be recommended on a more general basis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
We thank the medical and nursing staff of the Neurosurgical Intensive Care Unit for their support.
Footnotes
Contributor Information
Marlies Bauer, Email: Marlies.Bauer@tirol-kliniken.at.
Florian Sohm, Email: florian.sohm@mailbox.org.
Claudius Thomé, Email: Claudius.Thome@i-med.ac.at.
Martin Ortler, Email: Martin.Ortler@i-med.ac.at.
REFERENCES
- 1.Abadal-Centellas JM, Llompart-Pou JA, Homar-Ramirez J, Perez-Barcena J, Rossello-Ferrer A, Ibanez-Juve J. Neurologic outcome of posttraumatic refractory intracranial hypertension treated with external lumbar drainage. J Trauma. 2007;62:282–6. doi: 10.1097/01.ta.0000199422.01949.78. [DOI] [PubMed] [Google Scholar]
- 2.Carney N, Totten A, O’Reilly C, Ullman J, Hawryluk G, Bratton S, et al. Guidelines for the Management of Severe Traumatic Brain Injury. 4th Edition. 2016. [Last accessed on 2017 Jun 24]. Available from https://braintrauma.org/uploads/03/12/Guidelines_for_Management_of_Severe_TBI_4th_Edition.pdf . [DOI] [PubMed]
- 3.Citerio G, Signorini L, Bronco A, Vargiolu A, Rota M, Latronico N, et al. External ventricular and lumbar drain device infections in ICU patients: A prospective multicenter Italian study. Crit Care Med. 2015;43:1630–7. doi: 10.1097/CCM.0000000000001019. [DOI] [PubMed] [Google Scholar]
- 4.Creutzfeldt CJ, Vilela MD, Longstreth WT., Jr Paradoxical herniation after decompressive craniectomy provoked by lumbar puncture or ventriculoperitoneal shunting. J Neurosurg. 2015;123:1170–5. doi: 10.3171/2014.11.JNS141810. [DOI] [PubMed] [Google Scholar]
- 5.Judith J, Gilles L. F, Douglas B, Coursin M. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002:30. doi: 10.1097/00003246-200201000-00020. [DOI] [PubMed] [Google Scholar]
- 6.Jung HJ, Kim DM, Kim SW. Paradoxical transtentorial herniation caused by lumbar puncture after decompressive craniectomy. J Korean Neurosurg Soc. 2012;51:102–4. doi: 10.3340/jkns.2012.51.2.102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim GS, Amato A, James ML, Britz GW, Zomorodi A, Graffagnino C, et al. Continuous and intermittent CSF diversion after subarachnoid hemorrhage: A pilot study. Neurocrit Care. 2011;14:68–72. doi: 10.1007/s12028-010-9401-y. [DOI] [PubMed] [Google Scholar]
- 8.Levy D, Rekate H. Controlled lumbar drainage in pediatric head injury. J Neurosurg. 1995;83:453–60. doi: 10.3171/jns.1995.83.3.0453. [DOI] [PubMed] [Google Scholar]
- 9.Liang H, Zhang L, Gao A, Li Y, Jiang Z, Hu F, et al. Risk factors for infections related to lumbar drainage in spontaneous subarachnoid hemorrhage. Neurocrit Care. 2016;25:243–9. doi: 10.1007/s12028-015-0239-1. [DOI] [PubMed] [Google Scholar]
- 10.Maas AIR, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728–41. doi: 10.1016/S1474-4422(08)70164-9. [DOI] [PubMed] [Google Scholar]
- 11.Muench E, Vajkoczy P. Therapy of malignant intracranial hypertension by controlled lumbar cerebrospinal fluid drainage. Crit Care Med. 2001;29:976–81. doi: 10.1097/00003246-200105000-00016. [DOI] [PubMed] [Google Scholar]
- 12.Murad A, Ghostine S, Colohan AR. A case for further investigating the use of controlled lumbar cerebrospinal fluid drainage for the control of intracranial pressure. World Neurosurg. 2012;77:160–5. doi: 10.1016/j.wneu.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 13.Nwachuku EL, Puccio AM, Fetzick A, Scruggs B, Chang YF, Shutter LA, et al. Intermittent versus continuous cerebrospinal fluid drainage management in adult severe traumatic brain injury: Assessment of intracranial pressure burden. Neurocrit Care. 2014;20:49–53. doi: 10.1007/s12028-013-9885-3. [DOI] [PubMed] [Google Scholar]
- 14.Oddo M, Crippa IA, Mehta S, Menon D, Payen JF, Taccone FS, et al. Optimizing sedation in patients with acute brain injury. Crit Care. 2016;20:128. doi: 10.1186/s13054-016-1294-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peeters W, van den Brande R, Polinder S, Brazinova A, Steyerberg EW, Lingsma HF, et al. Epidemiology of traumatic brain injury in Europe. Acta Neurochir (Wien) 2015;157:1683–96. doi: 10.1007/s00701-015-2512-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saul T, Ducker T. Effect of intracranial pressure monitoring and aggressive treatment on mortality in severe head injury. J Neurosurg. 1982;56:498–503. doi: 10.3171/jns.1982.56.4.0498. [DOI] [PubMed] [Google Scholar]
- 17.Schade R, Schinkel J. Bacterial meningitis caused by the use of ventricular or lumbar cerebrospinal fluid catheters. J Neurosurg. 2005;102:229–34. doi: 10.3171/jns.2005.102.2.0229. [DOI] [PubMed] [Google Scholar]
- 18.Stocchetti N, Maas AI. Traumatic intracranial hypertension. N Engl J Med. 2014;370:2121–30. doi: 10.1056/NEJMra1208708. [DOI] [PubMed] [Google Scholar]
- 19.Tuettenberg J, Czabanka M, Horn P, Woitzik J, Barth M, Thome C, et al. Clinical evaluation of the safety and efficacy of lumbar cerebrospinal fluid drainage for the treatment of refractory increased intracranial pressure. J Neurosurg. 2009;110:1200–08. doi: 10.3171/2008.10.JNS08293. [DOI] [PubMed] [Google Scholar]


