Abstract
Cutaneous lymphomas are classified according to their cellular origin into T-cell lymphoma and B-cell lymphoma. The annual incidence rate is 0.3 per 100,000 population. We report a case of a 56-year-old male patient who presented with a two-month history of nodules of varying sizes, some ulcerated, on the face, abdomen, and upper limbs. Histopathological examination and immunohistochemical study confirmed the diagnosis of primary cutaneous centrofollicular lymphoma. Studies have shown an increased incidence of non-Hodgkin lymphomas in the last decade. We report an infrequent case that should be kept as a differential diagnosis of patients with nodules and cutaneous papules.
Keywords: Lymphoma, Skin, Skin neoplasms
INTRODUCTION
Cutaneous lymphomas are classified according to their cellular origin into T-cell lymphoma and B-cell lymphoma. The annual incidence rate is 0.3 per 100,000 population. 65% of cases are T cells, 25% are B-cells, and 10% are true histiocytic lymphomas or other rare types of lymphomas. From the dermatological point of view, B-cell lymphomas are characterized by few lesions, which are in general nodules or infiltrates, presenting relatively fast growth. Unlike T-cell lymphomas, they show no pruritus.1 Primary cutaneous follicle-center B-cell lymphoma is the most common subtype, representing about 55% of cases.2
CASE REPORT
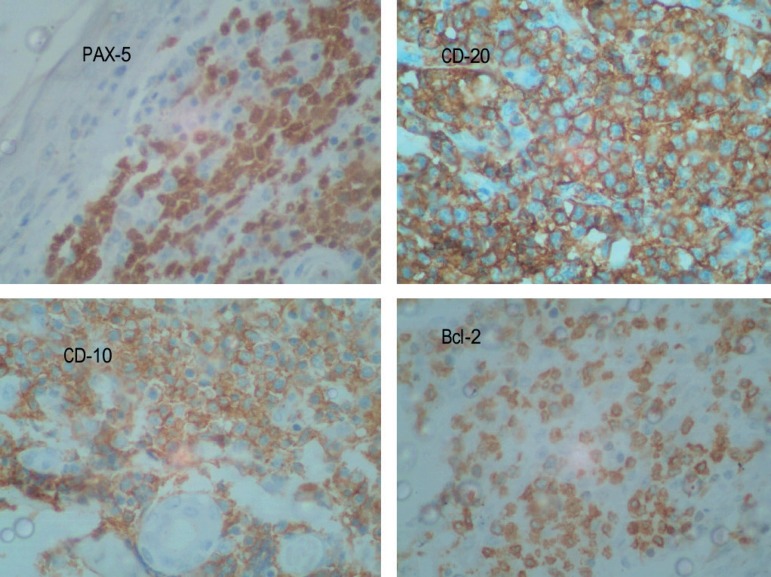
A 56-year-old brown male patient, trader, noticed the appearance of "balls" on the abdomen 2 months before. He reported progressive growth and the emergence of new similar lesions associated with mild local pain. He denied itching or secretion drainage, as well as previous treatment. On physical examination, we found nodules of varying sizes, with a smooth and glossy surface, some ulcerated and erythematous on the face, abdomen, and upper limbs (Figures 1 and 2). A biopsy of one of the nodules revealed on histopathological examination atrophic epidermis and nodular neoplastic infiltration of the dermis under the Grenz zone at all levels. The subcutaneous tissue revealed dense aggregates of epithelioid cells with scant eosinophilic cytoplasm, vesicular nuclei, more than two nucleoli, nuclear-cellular pleomorphism, and frequent atypical mitosis figures. These findings were compatible with atypical lymphoid infiltrate. Therefore, we performed an immunohistochemical study to complete diagnosis, as well as blood count, chest, abdomen, head, and neck CT scans. These complementary exams showed no change (Figure 3). Immunohistochemical examination showed positivity for CD20, PAX-5, CD10, BCL-2, and BCL-6 (Figure 4). The patient was diagnosed with primary cutaneous follicle-center lymphoma and referred to a state oncology reference hospital. There, he was submitted to six chemotherapy sessions with the R-CHOP regimen (Rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) with complete remission of the skin lesions, which remained unchanged to imaging tests (Figure 5). The patient has been followed without signs of relapsing.
Figure 1.

Erythematous nodules of varying sizes, some ulcerated, others covered by smooth and shiny skin
Figure 2.

Nodules on the back
Figure 3.
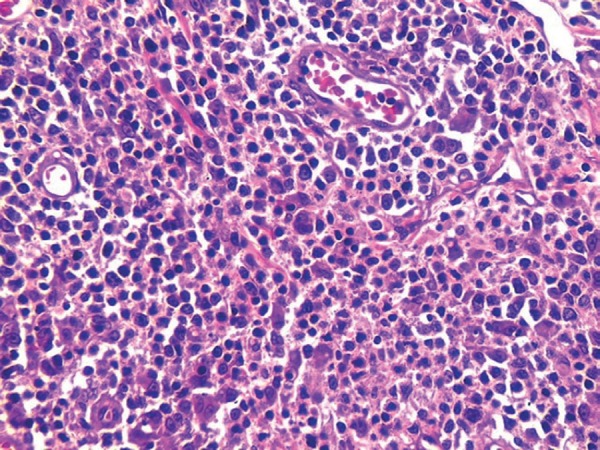
Dense aggregates of epithelioid cells with scant eosinophilic cytoplasm, vesicular nuclei, more than two nucleoli, nuclear-cellular pleomorphism, and frequent atypical mitosis figures. Hematoxylin & eosin, X40
Figure 4.
Immunohistochemistry. Magnification X40
Figure 5.

Remission of the skin lesions after treatment
DISCUSSION
In the last decade, studies show increased incidence of non-Hodgkin lymphoma compared to other subtypes of skin cancer. Cutaneous lymphomas can be primary or secondary. The former is that of exclusively cutaneous involvement at the time of diagnosis and up to six months after, as evidenced in the present case by physical examination and complementary imaging tests. Although the two variants are identical in morphological appearance, they have different clinical behaviors. Primary cutaneous lymphoma features a more indolent natural history than the secondary form of the disease, with good prognosis.3 It manifests itself at an average age of 58 years, consistent with our patient's age, with a 5-year survival rate of 95%. Cutaneous manifestations can be papules or nodules and their most frequent location are the head, scalp, and trunk.4 Some authors believe that this type of lymphoma can be caused by prolonged antigenic stimulation possibly caused by chronic infection by specific microorganisms, especially by species of Borrelia. It should also be noted that these types of bacteria have been described in HIV patients and in patients undergoing methotrexate therapy, thereby suggesting that immune dysregulation may act in the development of these neoplasms.5 Clinical history and physical examination help the diagnosis of primary cutaneous B-cell lymphomas. Confirmation, however, is obtained essentially by histological and immunohistochemical examinations.2 Follicular center cells usually express CD20+, CD79a+, BCL-6+, and BCL-2- (possibly with a weak BCL-2 expression in a minority of B cells), with variable CD43 and CD106 expression. Treatment of choice is based on histology, anatomical location, and number of tumor lesions.2 Radiation therapy is one of the preferred options in cases of a few lesions or if they are restricted to a single area. Although it can also be used in cases of late recurrences, the optimal dose and the number of treatment sessions has not yet been well established.6 Chemotherapy with cyclophosphamide, hydroxydoxorubicin, vincristine, prednisone, and rituximab (R-CHOP) is another option, particularly for patients with multifocal and extensive skin disease and for patients who develop extra-cutaneous manifestations. In the present case, due to the large amount and distribution of nodules, we opted for chemotherapy, resulting in a complete remission of the skin lesions.7 We report an infrequent case that should be kept as a differential diagnosis of patients with nodules and cutaneous papules.
Footnotes
Conflict of interest: none.
Work performed at the Dermatology Service at Universidade do Estado do Pará (UEPA) - Belém (PA), Brazil.
Financial support: none.
REFERENCES
- 1.Nunes MG, Morais JCO, Pierro APSM, Coutinho MFV, Morais JCO, Carneiro SCS, Azulay DR. Linfoma cutâneo de células B: relato de caso. An Bras Dermatol. 2004;79:715–720. [Google Scholar]
- 2.Arenas CM, Mariño ML, Calderón JE, González MI, Robayo MP. Linfoma cutáneo de células B tipo centro folicular con infiltración a médula ósea: reporte de un caso. Rev Fac Med. 2012;20:84–89. [Google Scholar]
- 3.Sousa ARD, Costa IS, Araújo EF, Filho, Jucá NBH, Miranda WLL. Linfoma cutâneo primário de grandes células B de apresentação atípica - Relato de caso. An Bras Dermatol. 2011;86:549–551. [Google Scholar]
- 4.Moricz CZM, JA Sanches., Jr. Processos linfoproliferativos da pele: Parte 1 - Linfomas cutâneos de células B. An Bras Dermatol. 2005;80:461–471. [Google Scholar]
- 5.Bolognia JL, Jorizzo JL, Rapini RP. Dermatologia. 2. ed. Rio de Janeiro: Elsevier; 2011. traduzida. [Google Scholar]
- 6.Suárez AL, Querfeld C, Horwitz S, Pulitzer M, Moskowitz A, Myskowski PL. Primary cutaneous B-cell lymphomas: part II. Therapy and future directions. J Am Acad Dermatol. 2013;69:343.e1–343.e11. doi: 10.1016/j.jaad.2013.06.011. [DOI] [PubMed] [Google Scholar]
- 7.Fernandez-Flores A, Smucler-Simonovich A, Escalante F, Manjon JA. The differential diagnosis between primary cutaneous large B-cell lymphoma and cutaneous follicular lymphoma: prognostic and therapeutic implications. Am J Dermatopathol. 2011;33:819–826. doi: 10.1097/DAD.0b013e3181fe9746. [DOI] [PubMed] [Google Scholar]