Abstract
Nevus lipomatosus cutaneous superficialis is a rare benign hamartomatous skin tumor characterized by dermal deposition of mature adipose tissue. Two clinical forms have been described (classical and solitary types). We describe a case of nevus lipomatosus cutaneous superficialis with a 13-year history of growth in a young woman who had a solitary skin-colored tumoral mass on the right buttock. Histopathological findings were typical and confirmed the diagnosis. In this case, the lesion was a skin-colored isolated mass, as described in the solitary type, but its localization and age of appearance were compatible with the classical type. The combination of simultaneous clinical findings of both types had not been published before.
Keywords: Connective tissue, Hamartoma, Skin neoplasms
INTRODUCTION
Nevus lipomatosus cutaneous superficialis (NLCS) was first described in 1921 by Hoffman and Zurhelle.1 It is an uncommon cutaneous hamartoma defined by the presence of aggregates of mature ectopic adipocytes among the collagen bundles of the dermis.2,3 This neoplasia is usually present at birth or in childhood with no familial tendency nor sex predilection.4,5 Clinically, it is classified into two clinical variants. The classical form is usually composed of multiple and grouped skin-colored, pedunculated nodules. A second and more rare form is characterized by a solitary dome-shaped sessile papule or nodule.6
Although fat deposition in the dermis has been considered to be a consequence of degenerative changes in connective tissues, the pathogenesis of NLCS remains unknown.7 Several theories have been proposed. One of them suggests that multiple type NLCS arises from adipose metaplasia in the course of degenerative changes in the dermal connective tissue. Another theory is that the adipocytes would represent a true nevus from the developmental displacement of adipose tissue.8 A third proposal is that the mature adipocytes grow from mononuclear cells differentiating into lipoblasts in a perivascular area.9
The histopathology of NLCS shows clusters of ectopic mature adipose tissue among collagen fibers in the dermis with no connection to the subcutaneous fat tissue.2 These ectopic adipocytes contain large intracytoplasmic lipid vacuoles and are often associated with vascular structures.9
We described an unusual case of an NLCS with a 13-year history of growth in a young woman.
CASE REPORT
A 20-year-old healthy woman, skin phototype IV, presented with a solitary mass on the right buttock, which had increased in size over the last thirteen years. Despite the unpleasant appearance, the lesion was asymptomatic. The patient reported no family history of similar lesions.
Physical examination revealed a skin-colored, pedunculated soft mass with a cerebriform surface and centrally located comedo-like plugs, measuring 12x8cm, on the right buttock (Figures 1 and 2). We observed no ulceration, excessive hair growth, pigmentation, café-au-lait macules, or induration. Systemic examination was normal.
Figure 1.

Skin-colored pedunculated mass with cerebriform surface on the right buttock
Figure 2.

Detail of the lesion, showing some comedo-like plugs on its surface
An incisional skin biopsy was performed and histopathological analysis showed slight hyperkeratosis, acantosis, and elongation of the rete ridges of the epidermis. Aggregates of mature adipocytes were interposed among the collagen bundles in the reticular dermis, with no connection of these cells to the subcutaneous fat. We found focal spindle cell infiltrates surrounding the blood vessels (Figure 3). These findings supported the clinical diagnosis of NLCS.
Figure 3.
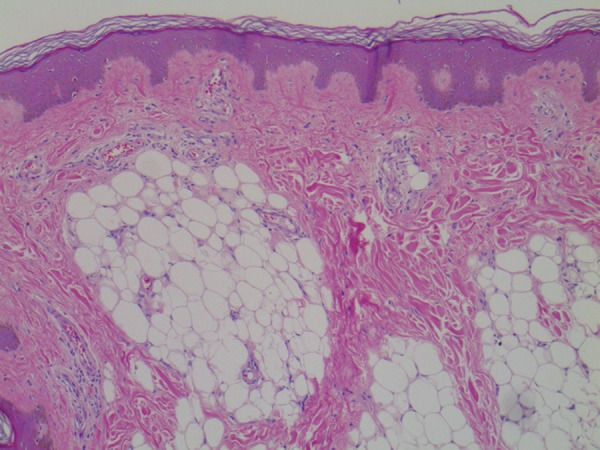
Aggregates of ectopic adipocytes diffusely scattered between collagen fibers in the dermis, without connection with the subcutaneous tissue. (Hematoxylin & eosin X20)
The patient was submitted to a surgical excision with no recurrence at a six-month follow-up.
DISCUSSION
NLCS is a rare idiopathic hamartomatous anomaly that is characterized by ectopically situated mature adipocytes in the dermis.4,7 It may be present at birth or may even begin in infancy. It is classified into two clinical forms. The classical (or multiple) form occurs within the first three decades of life and is characterized by clusters of soft, yellow or skin-colored papules or nodules, with smooth and wrinkled appearance, located on the lower back, pelvic girdle, buttocks and upper thighs in a zosteriform pattern.7 The solitary type can occur anywhere on the skin and usually appears during the third to sixth decades of life as a single nodule, with the same dermatologic appearance.4 This clinical form has been noted in rare sites such as the face, scalp, eyelids, and clitoris.2,7 In our case, although the patient had a solitary mass, the age of appearance, site of the lesion, and the dermatological characteristics were compatible with the classical form.
In both types, the lesions are asymptomatic, as seen in our patient. Ulceration occurs rarely, especially after external traumas or ischemia.2,7 Furthermore, café-au-lait macules, leukodermic spots, overlying hypertrichosis and comedo-like alterations can coexist.3,7 Similarly, in this report, the surface of the nevus was studded with some open comedones.
The histopathology of NLCS usually reveals proliferation of ectopic mature adipocytes in the reticular dermis that varies from 10-50% of the lesion.5,10 The adipocytes most commonly form small aggregates around blood vessels or eccrine glands, but may also be present as solitary adipocytes between collagen bundles.1,2 In some cases, there is an increased density of collagen fibers, fibroblasts, and a perivascular infiltration of mononuclear and spindle-shaped cells.7,10 The epidermis exhibits acanthosis, basket weave hyperkeratosis, increased basal pigmentation, and obliteration with focal elongation of rete ridges. Adnexal structures may be unaffected or reduced in some cases, and may show perifollicular fibrosis.10
In our patient, the histological findings were consistent with NLCS, showing more than 15% of the dermis replaced by adipose tissue, with focal spindle-shaped cell infiltration surrounding the blood vessels. However, disagreeing with the literature, we observed no other dermal alterations such as increased density of collagen fibers, decreased elastic tissue, or adnexal fibrosis.
Clinically, NLCS should be differentiated from nevus sebaceous, connective tissue nevus, neurofibroma, lymphangioma, hemangioma, and focal dermal hypoplasia (Goltz syndrome).2,7 Histopathological studies usually help in differentiation and a biopsy should be performed to confirm diagnosis. Similar dermal collections of adipocytes are also present in some melanocytic nevi, pedunculated lipofibromas, and in Goltz syndrome. In the case of Goltz syndrome, besides the clusters of adipocytes in the dermis, there is an extensive attenuation of collagen in the atrophic dermis and skin appendages are absent.2,3
Treatment is indicated only for cosmetic reasons since malignant degeneration and systemic abnormalities are rare.3 Due to the rarity of recurrent lesions, surgical excision is the best choice of treatment.4,7 For this reason, that was our procedure in the present case with an excellent outcome.
We report a case of NLCS to highlight its rarity and the importance of early diagnosis since the lesions can grow to large sizes causing aesthetic concerns to the patient. Our case was rare because the patient had a solitary mass that was clinically compatible with the classical type concerning age, site of appearance and lesion's characteristics. The histopathological findings were typical and allowed us to confirm the diagnosis and guide the surgical procedure. A long-term follow-up is necessary to verify if no other similar lesions will appear in the patient, confirming that this was the case of a solitary-type NLCS with atypical clinical characteristics.
Footnotes
Conflict of interest: none.
Work performed at the Hospital Universitário Antônio Pedro - Universidade Federal Fluminense (HUAP-UFF) - Niterói (RJ), Brazil
Financial support: none.
REFERENCES
- 1.Dotz W, Prioleau PG. Nevus lipomatosus cutaneous superficialis. Arch Dermatol. 1984;120:376–379. [PubMed] [Google Scholar]
- 2.Dhamija A, Meherda A, D'Souza P, Meena RS. Nevus lipomatosus cutaneous superficialis: an unusual presentation. Indian Dermatol Online J. 2012;3:196–198. doi: 10.4103/2229-5178.101819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pujani M, Choudhury M, Garg T, Madan NK. Nevus lipomatosus superficialis: a rare cutaneous hamartoma. Indian Dermatol Online J. 2014 Jan;5:109–110. doi: 10.4103/2229-5178.126069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ranjkesh MR, Herizch QH, Yousefi N. Nevus lipomatosus cutaneous superficialis: a case report with histologic findings. J Turk Acad Dermatol. 2009;3:1–3. [Google Scholar]
- 5.Avhad G, Jerajani H. Nevus lipomatosus cutaneous superficialis. Indian Dermatol Online J. 2013;4:376–377. doi: 10.4103/2229-5178.120660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goucha S, Khaled A, Zéglaoui F, Rammeh S, Zermani R, Fazaa B. Dermatol Ther. Vol. 1. Heidelb: 2011. Nevus lipomatosus cutaneous superficialis: report of eight cases; pp. 25–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patil SB, Narchal S, Paricharak M, More S. Nevus lipomatosus cutaneous superficialis: a rare case report. Iran J Med Sci. 2014;39:304–307. [PMC free article] [PubMed] [Google Scholar]
- 8.Kim YJ, Choi JH, Kim H, Nam SH, Choi YW. Recurrence of Nevus Lipomatosus Cutaneous Superficialis after CO2 Laser Treatment. Arch Plast Surg. 2012;39:671–673. doi: 10.5999/aps.2012.39.6.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones EW, Marks R, Pongsehirun D. Naevus superficialis lipomatosus. A clinicopathological report of twenty cases. Br J Dermatol. 1975;93:121–133. [PubMed] [Google Scholar]
- 10.Buch AC, Panicker NK, Karve PP. Solitary nevus lipomatosus cutaneous superficialis. J Postgrad Med. 2005;51:47–48. [PubMed] [Google Scholar]


