Abstract
Aims and Objectives:
Self-rated oral health is the key element that has a greater effect on quality of life and found to be authentic and logical to consider this as an indicator for overall oral health status. The aim was to investigate and identify the impact of various social and clinical factors on the perceived self-rated oral health status (PSR-OHS).
Materials and Methods:
A self-administered questionnaire was distributed 600 patients seeking information for age, gender, nationality, educational level, and their last dental visit followed by 15 questions related to social factors (patient self-rated oral health, patient-dentist communication, literacy level of the patient, and dental neglect) followed by estimating the clinical oral health status (decayed, missing, and filled teeth [DMFT] scores as per WHO norms).
Results:
The results were estimated by a single five-point-response-scale question dichotomized into poor and good self-rated oral health. The average mean age for participation in the study is 32.5 years and found to be highly significant (P < 0.01) with inverse relation indicating that younger patients give better PSR-OHS. There were no significant differences in PSR-OHS among other demographic factors. Patients visiting the dentist recently found to be confident about their PSR-OHS and are statistically significant. Pearson correlating scores of social factors and the DMFT scores most concerned in the present study have a significant relation with self-rated oral health status.
Conclusions:
PSR-OHS is governed by various dental health and awareness factors. It can be used as an important tool by a clinician to assess the clinical examination results which helps to achieve more effective time and patient management.
KEYWORDS: Dental neglect, health literacy, patient dentist communication, self-rated oral health status
INTRODUCTION
Oral health status is relentlessly connected with general health and has been proved so with many diseases such as diabetes, cardiovascular diseases, etc.[1] It has been stated that perceived self-rated oral health status (PSR-OHS) is the key element toward a better quality of life.[2,3] Perceived self-rated health refers to both a single question such as “in general, would you say that your health is excellent, very good, good, fair, or poor?” and a survey questionnaire in which participants assess different dimensions of their own health.[4] This self-rated oral health tool is very commonly used in several epidemiological studies to plan and monitor health services and in promoting oral health. Nowadays, this monitoring of self-assessed oral health helps in identifying the importance of the regular dental check-up, assists the dentists in assessing the routine diagnostic procedures to determine required treatment needs and is helpful in collecting the information related to oral health.[2] PSR-OHS is associated with not only the clinical factors such as dental caries but also other social factors such as patient-dentist communication, oral health literacy, and dental neglect.[1,3]
Patient-dentist communication plays a very important role for the motivation of the patient to maintain good oral hygiene, in turn improving the self-rated oral health status and literacy regarding oral health.[5]
“Health literacy in dentistry is defined as the degree to which individuals have the capacity to obtain, process and understand basic health information and services needed to make appropriate oral health decisions and act on them.”[6] Any deficit in oral health literacy would result in inadequate communication of the patient with the dentist as to the nature of their dental problems, ultimately leading to poor oral hygiene. Literature shows that low oral health literacy results in patients having a high risk for oral diseases.[7]
The term “Dental Neglect” can be defined as the behavior and attitudes which are likely to have detrimental consequences for the individual's oral health.[8,9] In other words, dental neglect is the failure to fulfill the known knowledge of oral health care for proper maintenance of oral cavity.[8,10]
The decayed, missing, and filled teeth (DMFT) index is one of the most common methods in oral epidemiology for assessing dental caries prevalence as well as dental treatment needs among populations.
The present study hypothesizes that a greater PSR-OHS should be associated with better patient-dentist communication and health literacy which in turn is associated with increased likelihood of patients seeking regular dental care thus reducing the dental neglect score.
The aim of this study is to assess the correlation of PSR-OHS with various social (Patient-dentist communication, literacy level, and dental neglect score) and clinical (DMFT) factors.
MATERIALS AND METHODS
STUDY POPULATION AND SETTING
The study was conducted at the University Hospital of Riyadh Colleges of Dentistry and Pharmacy, Riyadh, KSA, after approval from the IRB (IRB No: RC/IRB2016/153). Study subjects included the patients visiting the university hospital in the period between September 2016 and March 2017. The study sample size of 588 participants was calculated using a level of precision formula n = (zα+ zβ) 2 pq/d2 (zα: 1.96; zβ: 0.84; p: 25%; q: 75% and d: 5%). Sample size estimation was done setting a power of 80% with confidence interval 95%. A simple random sampling was employed for the selection of participants. The estimated required sample size of 600 participants was overshot during data collection to warrant for dropouts owing to incomplete questionnaires.
Inclusion criteria were patients aged between 18 and 50 years who were physically and mentally fit. Exclusion criteria were those participants not adhering to the above limits, patients visiting a dentist for the first time and differently abled individuals.
Informed consent and ethical approval were obtained before the start of the study.
STUDY INSTRUMENT
The survey was composed of a self-administered questionnaire combined from previously published studies[1,6] gathering information about age, gender, nationality, educational level and their last visit to a dentist followed by 15 questions related to patient self-rated oral health (1 question), dental care pattern (1 question), patient-dentist communication (4 questions), dental literacy level (3 questions) of the patient, and dental neglect (6 questions).
To avoid inappropriate answers by the patients who were not well acquainted with English, an English-Arabic version of the questionnaire was formulated. The concept of translation was to obtain an instrument with conceptual equivalence in a different cultural group. The original English questionnaire was translated into Arabic language by a bilingual native Arabic speaker and thereafter blindly back-translated by another bilingual native Arabic speaker. Through these rigorous cycles of translation and back translation, it was confirmed that the original meaning of the questionnaire was maintained. A pilot study was carried out using this bilingual instrument to ensure equivalence, clarity, and comprehension. After computing the cumulative score, we estimated the Cronbach alpha as a measure of internal consistency which was found to be good (0.83).
ORAL EXAMINATION
Examination of the patient to record the DMFT scores (World Health Organization caries diagnostic criteria)[11] was noted by two of the examiners. They were trained after the discussion of how to calibrate DMFT under the supervision of experienced dental specialists, later each examiner scored in 10 patients independently. Inter- and intra-examiner's values were computed, and differences were compared and discussed until a full agreement was achieved for all the sample patients. The intra- and inter-examiner variability was nullified by examining and reexamining these 10 patients (these patients are later excluded from the study). Examination procedures were standardized for validity and reproducibility of data before and during the survey. The DMFT scores were noted for each participant after answering the questionnaire.
DATA COLLECTION
A brief description of the questionnaire was given to the patients to enable them to answer appropriately. DMFT scores were noted for the same participants who answered the questionnaire.
STATISTICAL ANALYSIS
The data collected was analyzed using SPSS software SPSS 16.0 (SPSS, Inc., Chicago, IL, USA). All the variables were examined in bivariate tables using Chi-square tests to determine their independent associations with one outcome variable. Pearson's correlation coefficients were calculated for each of the independent variables to examine for autocorrelation.
RESULTS
After excluding the dropouts in participants who had provided incomplete data in their questionnaires 600 participants (305 males, 295 females) aged 18–50 years were analyzed.
Table 1 shows the PSR-OHS against the demographic distribution, dental visit history, and dental care pattern of participants. Chi-square test was used to perform this comparison. A dichotomous division of the rating by participants was done to “poor” (fair/poor) and “good” (good/very good/excellent) self-rated oral health. Poor PSR-OHS was found among 149 (24.8%) participants. No significant difference in PSR-OHS was seen between the participants based on gender, nationality, level of education, and dental care patterns. The mean age for participation in the study was found to be 34.5 years, and an inverse correlation was found indicating that the PSR-OHS decreased with age. This finding was highly significant (P < 0.01). Most of the participants were found to have visited the dentist within the past 12 months at the time and gave a high PSR-OHS rating which was statistically significant (P < 0.01). More than half of the population was found to visit the dentist only when they have a problem and believed that their PSR-OHS is good though not significant.
Table 1.
Characteristics of Participants by Perceived Self-Rated Oral Health Status
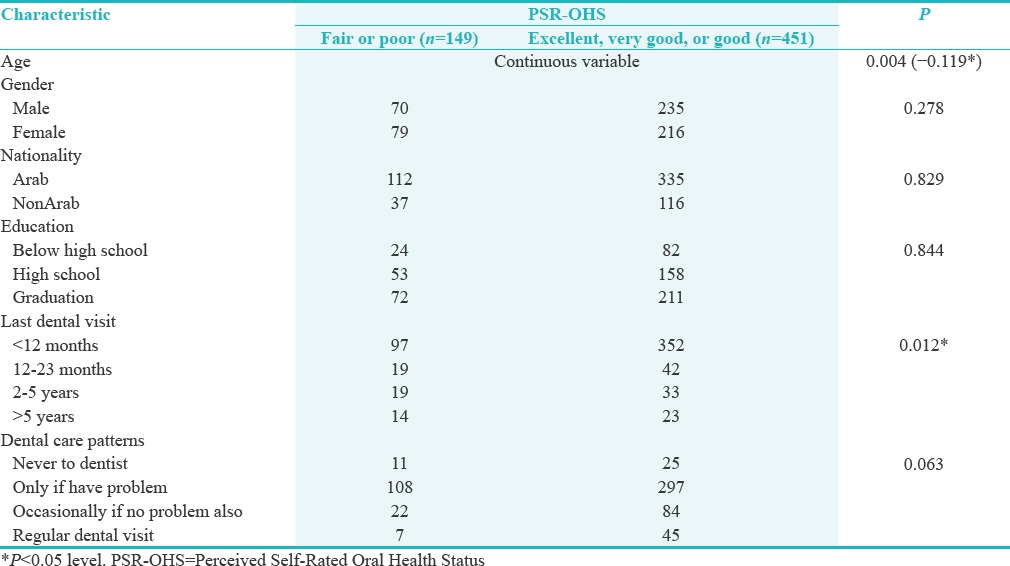
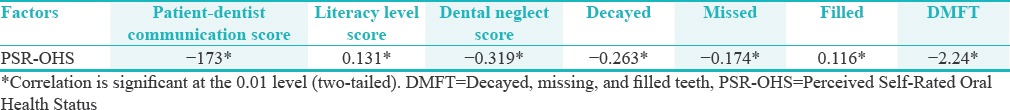
Table 2 shows the correlation of PSR-OHS with various dental health and awareness factors, both subjective and clinical. Pearson correlation coefficient among the factors, namely, patient-dentist communication, health literacy, dental neglect, and the DMFT scores was carried out. A significant and positive correlation were seen with patient-dentist communication score (0.173) (P < 0.01) and also with dental literacy level score (0.131) (P < 0.01). Negative correlation was seen with regard to dental neglect score (−0.319) showing high significance (P < 0.01). Likewise, a negative correlation was also observed between the DMFT and PSR-OHS (−0.305) and was highly significant in this study (P < 0.01).
Table 2.
Pearson correlations of social and clinical factors affecting Perceived Self-Rated Oral Health Status
DISCUSSION
PSR-OHS is a legitimate and valuable conclusive signal for oral health status being utilized as a part of epidemiologic studies the world over.[2] In our study, 75.1% of individuals rated their oral health as excellent/very good/good and only 24.9% as fair to poor in par with other studies done in various populations conducted in Brazil (74.3%),[12] South Africa (76.3%),[13] and Australia (83%).[14] The very recent study[15] conducted in India reported only 48.7% as excellent as their self-rated oral health.
This study is the first, to the best of our knowledge, to examine and report an association of various factors (social and clinical) in relation to PSR-OHS. However, there is little data available whether there is relationship of DMFT (clinical factor) with PSR-OHS wherein this study has its own uniqueness in cross-examining the patient comparing to his/her self-rated oral health status. This study exclusively confirms the patient's opinion about his/her self-rated oral health status by one-to-one interaction with the examiner.
This self-rated oral health gives a quick oral health assessment without the complex clinical examination allows us to perform oral examination and assess large population groups, thereby saving resources and may even yield significant policy implications for dental care.
In the present study, a negative correlation between age and PSR-OHS was found with high significance. This was in concurrence with another study,[12,13,14,15,16,17,18] which demonstrated that as age advanced among older individuals, the probability of cleaning their teeth twice daily diminished, conversely the younger patients having good oral hygiene, with good periodontal health make them rate their oral health as good.
The patients visiting the dentist within this 1 year rated themselves as better PSR-OHS and is statistically significant (P < 0.05) similar to the previous study conducted in 2017.[15] Another cohort study conducted in Sweden[19] reported that patients not using dental care in the earlier year were more disappointed and underrated their PSR-OHS. Similar results were observed in a study conducted in Brazil.[12] This suggests that previous dental visit definitely bring confidence and give a better PSR-OHS leading to encouragement in maintaining his oral hygiene.
A positive correlation was seen with patient-dentist communication score (0.173) showing that, as communication between the dentist and the patient increased, patients were more aware of their dental health issues and could maintain their health better, leading to a better PSR-OHS.[1] Likewise, a significant and positive correlation with dental literacy level score (0.131) showed that PSR-OHS ratings were higher owing to the fact that such patients possessed a better comprehension of dental literature and information as well as instructions from a dental clinic.[1] It is vital to enhance the ways that dental practitioners convey facts about oral health to their patients with low dental health literacy. Dental practitioners should frequently engage in conversation with these patients making them realize the importance of oral hygiene using simple terms. In addition, providing them with leaflets for future reference is another effective tool. All these help improve patient-dentist communication and dental literacy levels. These findings were in concurrence with a study conducted by Guo et al.,[1] which stated that higher health literacy levels were associated with better patient-dentist communication which in turn corresponded with better self-rated oral health.[1] Note that this dental health literacy measure references participants' capacity to search, understand, assess, and utilize dental health information. It requires the understanding of what their dentist narrates to them about their dental condition. Individuals who are more educated, have less difficulty in accessing and comprehending dental care instructions for tasks such as daily brushing and flossing. The findings of the study at hand are in agreement with several previous studies[20,21] while simultaneously being in contrast with Lee et al. in 2012,[6] who failed to find any significance between dental literacy and PSR-OHS ratings.
Skaret et al.[8,22] evaluated the reliability and construct validity of the Dental Neglect Scale given by Thomson et al.[10] and concluded that the scale may be a relevant instrument for population surveys which aim at identifying risk groups based on information about oral health, oral health-related behavior and attitudes. The study at hand showed that a negative correlation was seen with regard to dental neglect score (−0.319) which denoted that patients who did not neglect their dental hygiene were in a position to rate PSR-OHS higher. This finding was on par with the study conducted by Lee et al. in 2012.[6]
The correlation between the DMFT score and the PSR-OHS is not direct, and it has been explained that high DMFT scores are associated with anxiety levels,[23] which in turn are associated with PSR-OHS.[24] Thus, the presence of anxiety has a great influence on PSR-OHS. In the present study, a highly significant (P < 0.01) negative correlation was also observed between the DMFT and PSR-OHS (−0.305) depicting that an increase in DMFT score would direct the patients to rate their oral hygiene as poor. Moreover, significant correlations (P < 0.01) were observed individually between number of DMFT and PSR-OHS using the Pearson's correlation coefficient (r = −0.263, −0.174, 0.116, respectively). These findings supported the relationship between PSR-OHS and caries experience in which the patients with increased decayed and missing teeth showed poor PSR-OHS while those with more filled teeth showed good PSR-OHS ratings. This could possibly be attributed to increased anxiety in patients with decayed or missing teeth leading them to avoid or postpone treatment, while those who have filled teeth may be associated with reduced anxiety levels and a better scoring of PSR-OHS. Similar correlations were observed in studies conducted by Kojima et al.[2] and Samorodnitzky and Levin.[23]
Therefore, as per our conjecture, PSR-OHS serves as an immediate indicator for the population's oral health and thereby contributes to health-care planning according to the population's needs.
LIMITATIONS AND CONTROVERSIES
This was a cross-sectional study. A prospective cohort or intervention study may provide information beyond what is presented here
All participants were recruited from Riyadh Colleges of Dentistry and Pharmacy. This may limit the ability to extrapolate these findings to the general population. To overcome this, sample size has to be increased to get the appropriate results
Cross-sectional surveys that depend on self-reported data have more chances of bias because of individual's judgement on how they interpret themselves[25]
We did not consider possible related factors, such as socioeconomic status, and psychosocial variables
We did not examine the presence of subjective oral manifestations, for example, pain due to dental caries
REALD-30 which being more valid in estimating the literacy of a patient was not used to test the Literacy level of patients
Self-rated oral health status assessment was not considered in patients visiting the dentist for the first time.
FUTURE TRENDS
As self-rated oral health is the key component that has a greater effect on quality of life (2), it is very vital to prevent the clinical factors (DMFT) that affect the quality of life. This can be accomplished by monitoring the health from very early age group. Alongside, it is imperative to educate children from very young age group, the importance of health literacy and abstain from ignoring the dental health which would help them to correctly assessing their self-rated oral health. Future research should include a large group of population to identify specific factors related to self-rated oral health status.
CONCLUSIONS
Within the limitations of this study, it can be concluded that
PSR-OHS is governed by various dental health and awareness factors; some in a positive manner while others in a negative manner
PSR-OHS can be used as an important indicator/tool by a clinician to assess the clinical examination results which helps to achieve more effective time and patient management.
FINANCIAL SUPPORT AND SPONSORSHIP
Nil.
CONFLICTS OF INTEREST
There are no conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Dr. Avidapu Rajshekhar for helping us in statistics.
We also thank patients who cooperated for our study.
REFERENCES
- 1.Guo Y, Logan HL, Dodd VJ, Muller KE, Marks JG, Riley JL, 3rd, et al. Health literacy: A pathway to better oral health. Am J Public Health. 2014;104:e85–91. doi: 10.2105/AJPH.2014.301930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kojima A, Ekuni D, Mizutani S, Furuta M, Irie K, Azuma T, et al. Relationships between self-rated oral health, subjective symptoms, oral health behavior and clinical conditions in Japanese university students: A cross-sectional survey at Okayama University. BMC Oral Health. 2013;13:62. doi: 10.1186/1472-6831-13-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ng ST, Tengku-Aizan H, Tey NP. Perceived health status and daily activity participation of older Malaysians. Asia Pac J Public Health. 2011;23:470–84. doi: 10.1177/1010539510374751. [DOI] [PubMed] [Google Scholar]
- 4.Ware JE, Jr, Gandek B. Overview of the SF-36 health survey and the international quality of life assessment (IQOLA) project. J Clin Epidemiol. 1998;51:903–12. doi: 10.1016/s0895-4356(98)00081-x. [DOI] [PubMed] [Google Scholar]
- 5.Logan HL, Marek C. The anxious or fearful dental patient. In: Stefanac SJ, Nesbit SP, editors. Treatment Planning in Dentistry. 2nd ed. St. Louis, MO: Mosby Elsevier; 2007. pp. 339–65. [Google Scholar]
- 6.Lee JY, Divaris K, Baker AD, Rozier RG, Vann WF., Jr The relationship of oral health literacy and self-efficacy with oral health status and dental neglect. Am J Public Health. 2012;102:923–9. doi: 10.2105/AJPH.2011.300291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Horowitz AM, Kleinman DV. Oral health literacy: A pathway to reducing oral health disparities in Maryland. J Public Health Dent. 2012;72(Suppl 1):S26–30. doi: 10.1111/j.1752-7325.2012.00316.x. [DOI] [PubMed] [Google Scholar]
- 8.Sarkar P, Dasar P, Nagarajappa S, Mishra P, Kumar S, Balsaraf S, et al. Impact of dental neglect scale on oral health status among different professionals in Indore City – A cross- sectional study. J Clin Diagn Res. 2015;9:ZC67–70. doi: 10.7860/JCDR/2015/14321.6674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thomson WM, Locker D. Dental neglect and dental health among 26-year-olds in the dunedin multidisciplinary health and development study. Community Dent Oral Epidemiol. 2000;28:414–8. doi: 10.1034/j.1600-0528.2000.028006414.x. [DOI] [PubMed] [Google Scholar]
- 10.Thomson WM, Spencer AJ, Gaughwin A. Testing a child dental neglect scale in South Australia. Community Dent Oral Epidemiol. 1996;24:351–6. doi: 10.1111/j.1600-0528.1996.tb00875.x. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Oral Health Survey: Basic Methods. 4th ed. Geneva: World Health Organization; 1997. [Google Scholar]
- 12.Andrade FB, Lebrão ML, Santos JL, Duarte YA, Teixeira DS. Factors related to poor self-perceived oral health among community-dwelling elderly individuals in São Paulo, Brazil. Cad Saude Publica. 2012;28:1965–75. doi: 10.1590/s0102-311x2012001000014. [DOI] [PubMed] [Google Scholar]
- 13.Olutola BG, Ayo-Yusuf OA. Socio-environmental factors associated with self-rated oral health in South Africa: A multilevel effects model. Int J Environ Res Public Health. 2012;9:3465–83. doi: 10.3390/ijerph9103465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mejia G, Armfield JM, Jamieson LM. Self-rated oral health and oral health-related factors: The role of social inequality. Aust Dent J. 2014;59:226–33. doi: 10.1111/adj.12173. [DOI] [PubMed] [Google Scholar]
- 15.Singh A, Purohit BM. Exploring patient satisfaction levels, self-rated oral health status and associated variables among citizens covered for dental insurance through a national social security scheme in India. Int Dent J. 2017;67:172–9. doi: 10.1111/idj.12285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Olusile AO, Adeniyi AA, Orebanjo O. Self-rated oral health status, oral health service utilization, and oral hygiene practices among adult Nigerians. BMC Oral Health. 2014;14:140. doi: 10.1186/1472-6831-14-140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lawal FB, Olawole WO, Sigbeku OF. Self rating of oral health status by student dental surgeon assistants in Ibadan, Nigeria – A pilot survey. Ann Ib Postgrad Med. 2013;11:12–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Iwuala SO, Umeizudike KA, Ozoh OB, Fasanmade OA. Oral self-care practices, dental attendance and self-perceived oral health status among internal medicine residents in Nigeria. Eur J Genet Dent. 2015;20:79–86. [Google Scholar]
- 19.Ståhlnacke K, Söderfeldt B, Unell L, Halling A, Axtelius B. Patient satisfaction with dental care in one Swedish age cohort. Part II – What affects satisfaction. Swed Dent J. 2007;31:137–46. [PubMed] [Google Scholar]
- 20.Haridas R, Supreetha S, Ajagannanavar SL, Tikare S, Maliyil MJ, Kalappa AA, et al. Oral health literacy and oral health status among adults attending dental college hospital in India. J Int Oral Health. 2014;6:61–6. [PMC free article] [PubMed] [Google Scholar]
- 21.Jones K, Brennan DS, Parker EJ, Mills H, Jamieson L. Does self-efficacy mediate the effect of oral health literacy on self-rated oral health in an Indigenous population? J Public Health Dent. 2016;76:350–5. doi: 10.1111/jphd.12162. [DOI] [PubMed] [Google Scholar]
- 22.Skaret E, Astrøm AN, Haugejorden O, Klock KS, Trovik TA. Assessment of the reliability and validity of the dental neglect scale in Norwegian adults. Community Dent Health. 2007;24:247–52. [PubMed] [Google Scholar]
- 23.Samorodnitzky GR, Levin L. Self-assessed dental status, oral behavior, DMF, and dental anxiety. J Dent Educ. 2005;69:1385–9. [PubMed] [Google Scholar]
- 24.Furuta M, Ekuni D, Takao S, Suzuki E, Morita M, Kawachi I, et al. Social capital and self-rated oral health among young people. Community Dent Oral Epidemiol. 2012;40:97–104. doi: 10.1111/j.1600-0528.2011.00642.x. [DOI] [PubMed] [Google Scholar]
- 25.Peer E, Gamliel E. Too reliable to be true? response bias as a potential source of inflation in paper-and-pencil questionnaire reliability. Pract Assess Res Eval. 2011;16:1–8. [Google Scholar]


