Abstract
Background:
Sickle cell disease (SCD) is a major public health concern in tribal community not only in Gujarat but also globally. Gujarat, a western state of India, has 89.12 lakh tribal populations and is expected to have at least 9,00,000 sickle cell trait and 70,000 SCD patients. The aim of the present review is to document the prevalence of SCD in various communities and various screening methods adapted.
Methodology:
An in-depth literature review was carried out using available search engines such as Cochrane Library, PubMed, Scopus etc. and published articles, and government reports/policy documents with reference to SCD were gathered.
Results:
A total of 17 original research articles and 2 policy/program documents are included in this review. The review suggests a prevalence of 0.6%–35% studies conducted among medical students, tribal schoolchildren, and tribal adolescents, with diverse screening methodologies.
Conclusion:
A diverse prevalence is observed in this review. Various screening methods such as dithionite turbidity test/hemoglobin/high-performance liquid chromatography methods were used to estimate the prevalence, citing the need for standardization. It was also found that not only tribal population, but also nontribal population have the risk of getting SCD that needs to be further investigated properly. Qualitative studies with SCD patients are required to understand the quality of life and morbidity pattern.
Keywords: Gujarat, sickle cell, sickle cell diseases
INTRODUCTION
Sickle cell diseases (SCDs) is an emerging public health challenge, not only in India but also globally. It has been estimated that, between 2010 and 2050, about 14.2 million babies will be born with sickle cell anemia (SCA).[1] Three quarters of the total SCD cases of the world occur in Africa, where in few parts, the prevalence of sickle cell trait (SCT) (heterozygous) is as high as 30%.[2] Thus in 2006, the World Health Organization recognized SCD as a global public health problem.[3] Published literature cites multiple warnings regarding the effect of epidemiological and demographic transitions in low-to-middle-income countries and their consequences for SCD burden.[4] Due to high burden, hemoglobinopathies have also been encompassed in the 2010 Global Burden of Diseases, Injuries, and Risk Factors Study.[5]
In India, SCD is distributed geographically in the central and western regions.[6,7] It has been estimated that about 5200 live births have SCD every year. The prevalence of sickle cell gene is as high as 5%–34% in various scheduled tribes (STs), who are socioeconomically disadvantaged and are frequently medically underserved.[8] With the present prevalence of SCD, it is expected that there may be 18 million SCT and 1.4 million SCD patients among the tribal population. As per an Indian Council of Medical Research survey, about 20% of children with SCD expired by age of two and 30% of children with SCD among the tribal community die before they reach adulthood.[9,10] There are reports that provide interesting insights into SCD in India, but most of these are indecisive based on a single institution/region.[11,12,13] In India, it is very difficult to establish the burden of this problem accurately in the absence of gold standard-based screening programs, nationwide reporting system, or registries.
Gujarat with 89.12 lakh tribal populations is expected to have at least 9,00,000 SCT and 70,000 SCD patients.[2] The Dhodia, Dubla, Kukna, Gamit, Chaudhary, Halpati, Varli, Kokni, Kathodi, Kolcha, Kotwadia, etc., are major tribes with documented issues of SCD in Gujarat.[14,15,16,17,18] To combat SCD, Gujarat Sickle Cell Anemia Control Society was established in the year 2011 with a target of no child birth with SCD by 2020 and prevention of SCD with decrease in morbidity.
Objective
The objective of this study was to document the prevalence of SCD in various communities and types of screening methods adapted in Indian studies.
METHODOLOGY
An in-depth literature review was carried out using the PubMed, ScopeMed, Google Scholar, and Cochrane Library. All the published articles, government reports, and policy documents with specific reference to SCD were gathered. Cross-references mentioned in articles were further searched to add new dimensions in exploring various aspects of SCD. Two investigators independently searched for all the potential articles in the above-mentioned search engines; however, the third investigator summarized and cross-checked for duplication and finalized the articles based on the inclusion criteria.
The following keywords were searched in the title or abstract of the papers: “sickle cell(s),” “sickle cell disease(s),” “sickle cell anemia,” “sickle cell crisis,” “sickle cell disorder(s),” “sickle cell condition(s),” “sickle cell trait(s),” “sickle cell hemoglobin(s),” “prevalence,” “India,” “Gujarat,” “screening,” “Ante natal screening,” “Programs,” “Policies,” “Control,” and “IEC.” Several restriction criteria were used in the electronic search: (a) only articles published in English were considered; (b) only studies published between January 1996 and May 2016 were included, to focus on a description of the current use/issues; (c) and only original papers and systematic reviews were included.
RESULTS
Based on the inclusion criteria, 17 original articles and 2 policy documents from Gujarat until May 2016 are included in this review. Majority of the published literature are cross-sectional studies conducted among adolescents focusing on screening. None of the articles (possibly none) were published in journal with documented impact factor more than 1. Methodology adapted for screening and documenting the prevalence was different in different studies.
Screening methodologies and prevalence of sickle cell disease in Gujarat
Screening methodologies adapted by various researchers for screening and documenting the prevalence of SCD in Gujarat ranged from dithionite turbidity test (DTT) followed by electrophoretic test to sophisticated high-performance liquid chromatography (HPLC). Table 1 summarizes the variations of prevalence and types screening tests adapted by studies conducted in Gujarat, India.
Table 1.
Sickle cell disease studies in Gujarat, India - A summary of descriptive review
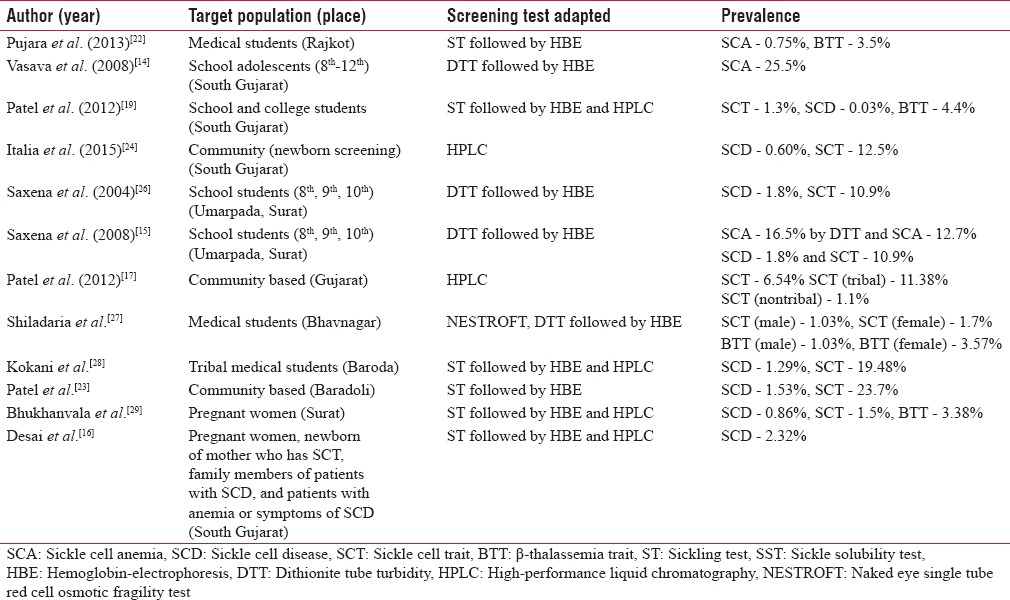
Saxena et al. used DTT against electrophoretic test and estimated a positive predictive value of 93.4% of DTT.[15] Another study conducted in tribal rural block utilized Solubility Test (ST) as screening method followed by HPLC test.[19] In a study conducted by the Indian Red Cross Society, Gujarat State Branch, prevalence of trait was 11.37% in tribal area and 1.1% in nontribal area.[20] In a voluntary community screening program, using HPLC methodology, a prevalence of SCT (15.63%) in Choudhary labeled as general caste (nontribal) against 18.5% in Rathva (ST subpopulation)[21] was cited. A study by Desai et al. documented the prevalence of 2.3% for SCD using panel data methodology.[16]
In a study based on camp approach for screening of SCD using DTT, there was an estimated prevalence of 1.3% among universities and documented Gamits, Vasavas, Mayavanshi, and Chaudhary as the most commonly affected subcastes.[22] Probably, this is the only study documenting SCD among Mayavanshi subcaste (6.9%), which is not documented in any other published literature. Other prevalence studies among adolescents and medical undergraduates suggest the range of SCD from 12.7% to 37.5%. However, as these students were institutional based, they do not reflect the community-level prevalence.[15,25,29,30,31] In Gujarat, the Dhodia, Dubla, Gamit, and Naika tribes have a high documented prevalence of sickle hemoglobin (HbS) (13%–31%).[23] More recently, very extensive population surveys have been done by the Indian Red Cross Society, Gujarat State Branch, where 1,68,498 tribals from 22 districts were screened and the overall prevalence of sickle cell carriers was 11.37%.[20] Some tribal groups in South Gujarat such as Chaudry, Gamit, Rohit, Vasava, and Kukana have shown both a high prevalence of HbS (6.3%–22.7%) as well as β-thalassemia trait (BTT) (6.3%–13.6%).[22] These tribal groups would have the likelihood of co-inheriting both these genes. Another larger community-based study screened 32,857 samples of students from different schools and colleges in South Gujarat, which found that the overall prevalence of BTT and SCT in South Gujarat was 4.4% and 1.3%, respectively. To summarize main subcaste that emerges from the review of literature as Warli, Bhil, Chaudhary, Dhodia Patel, Naika, Vasava, and Halpati.
Innovations for sickle cell disease screening and its management
Only three published documents/studies citing innovations in SCD screening were retrieved:
A village-based model to enhance screening in South Gujarat, focusing more on generating community ownership for screening, however, with a blanket screening program rolled out by the Government of Gujarat, replicability of such models needs to be verified cautiously[23]
Comprehensive care model for SCA: The present innovation was tried by a nongovernmental organization (NGO) in Jhagadia block, Bharuch in Gujarat. They developed a comprehensive care model for SCD including screening, standardized inpatient and outpatient protocols, population management, and health education of community. A high prevalence of pain crisis, hospitalization, and blood transfusion among the patient population was documented. A high lost to follow-up was documented: 20% with no follow-up and only 45% had two or more than two clinical clinic visits. Long-term evaluation of such efforts and its integration with the existing health system will be required
Newborn screening program in South Gujarat: Screening of 5467 newborns, using HPLC, with diagnosis by molecular analysis, across four districts of South Gujarat over 2 years, estimated 0.23% of SC homozygous condition. The SCD babies were followed up clinically and hematologically regularly for 1.5–5 years to describe the course of the disease.[27] However, the study does not conclude whether this mechanism of integrating newborn testing can be feasible. Costing of such model will be required for rolling it out. This study demonstrated feasibility of use of dried blood spot methodology for screening in remote areas and engaging the private agencies within the network of established government system for developing a regional newborn screening system.
Co-existence of sickle and thal gene in Gujarat
One of the important observations from the published literature from Gujarat is that, in contrast to the earlier reports published elsewhere in India citing that SCD in India is clinically mild due to the presence of Xmn I (+/+) polymorphism and high prevalence of alpha thalassemia, SCD in Gujarat is apparently more severe, and in spite of the presence of genetic modifier, almost 21.8% of SCD babies required hospitalization.[27] However, the authors failed to explore the reason for hospitalization and the other confounders that might possibly affect the hospitalization rates. The sample size (32 babies) followed was also not powered enough to generalize the findings. In a similar study for determining the hematological profile of SCD patients in a tertiary care institution from South Gujarat, it was concluded that the mean fetal hemoglobin (HbF) level in SCD patients from South Gujarat was higher when compared to Africans whereas lower when compared to Indian studies.[6] The authors concluded that the different levels of HbF can be due to co-inheritance trait of alpha or β-thalassemia or any strong genetic component which needs to be explored further. There are no other published literature/evidence from Gujarat citing similar co-existence of sickle and thal gene in tribal of Gujarat.
DISCUSSION
Majority of the published studies are focusing on screening knowledge, attitudes and practices or hematological profile of SCD patients. The prevalence of SCD ranged from 0.6% to 35%, however it cannot be generalized as studies have adopted different methodologies with different approaches and different classification of castes and target population. There is also no uniformity in the screening test used and its validity. Published studies have used DTT/HB/HPLC methods to estimate the prevalence, which needs to be structured further. One of the field-based utilities on DTT by Saxena et al. for screening of SCD found that sensitivity of DTT in fields was 93.4%.[15] Another study also narrates the composition of most appropriate DTT test buffer that can enhance sensitivity and specificity which is suitable for the field conditions.[28] Available published literature cites that both tribal and nontribal populations are prone to SCD, but there are no systematic studies to explore the risk of getting SCD among nontribal population. Although state-funded SCD control program is functional since long, none of the published literature or policy document narrates the availability of the registries of the SCD patients in Gujarat.
CONCLUSION AND WAY FORWARD
There is an urgent need for establishing uniformity in the screening of SCD. The gold standard for screening of SCD needs to be established and nontribal population needs to be targeted in further research studies. As per the state-led SCD control program, all antenatal mothers in tribal block need to be screened for SCA and recorded in mother-to-child tracking system, scoping into the raw data of testing should be taken on priority. With lot of NGOs working in South Gujarat, there is further possibility of pooling the information and developing SCD registries. There is also an urgent need to explore the co-existence of SCA and Thal gene and also the mortality profile and survival analysis of the SCD patients. Qualitative studies among SCD patients are required to understand stigma related to disease, quality of life, and morbidity pattern. Quantitative studies on documenting morbidity profile including crisis, its management, and use of folic acid and hydroxyurea for SCA are also required.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors are grateful to the Departments of Community Medicine, Medicine, Pathology, and Pediatrics, GMC Surat and Valsad and Surat Raktadan Kendra for assistance in literature searching during the initial phase of manuscript. We would also like to acknowledge DST, Government of India and CMC, Vellore, for their special assistance to carry out this work.
REFERENCES
- 1.Piel FB, Hay SI, Gupta S, Weatherall DJ, Williams TN. Global burden of sickle cell anaemia in children under five, 2010-2050: Modelling based on demographics, excess mortality, and interventions. PLoS Med. 2013;10:e1001484. doi: 10.1371/journal.pmed.1001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sickle Cell Anemia Control Program. A New Initiative of Government of Gujarat: Best Health Practices. Gujarat Health and Family Welfare Department, Gujarat. 2013. [Last accessed on 2016 May 11]. Available from: http://www.sickle.cell.gujarat.gov.in/Docs/News_GR_NC/131120_120132.pdf .
- 3.World Health Organization. Fifty-ninth World Health assemblies: Resolutions and decisions, annexes. WHA59/2006/REC/1. Geneva: World Health Organization; 2006. [Google Scholar]
- 4.Weatherall DJ, Clegg JB. Inherited haemoglobin disorders: An increasing global health problem. Bull World Health Organ. 2001;79:704–12. [PMC free article] [PubMed] [Google Scholar]
- 5.Murray CJ, Ezzati M, Flaxman AD, Lim S, Lozano R, Michaud C, et al. GBD 2010: A multi-investigator collaboration for global comparative descriptive epidemiology. Lancet. 2012;380:2055–8. doi: 10.1016/S0140-6736(12)62134-5. [DOI] [PubMed] [Google Scholar]
- 6.Rao VR. Genetics and epidemiology of sickle cell anemia in India. Indian J Med Sci. 1988;42:218–22. [PubMed] [Google Scholar]
- 7.Jain DL, Sarathi V, Upadhye D, Gulhane R, Nadkarni AH, Ghosh K, et al. Newborn screening shows a high incidence of sickle cell anemia in Central India. Hemoglobin. 2012;36:316–22. doi: 10.3109/03630269.2012.691434. [DOI] [PubMed] [Google Scholar]
- 8.Lehmann H, Cutbush M. Sickle-cell trait in Southern India. Br Med J. 1952;1:404–5. doi: 10.1136/bmj.1.4755.404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rupani MP, Vasava BC, Mallick KH, Gharat VV, Bansal R. Reaching community through school going children for sickle cell disease in Zankhvav village of Surat district, Western India. Online J Health Allied Sci. 2012;11:4. [Google Scholar]
- 10.Sickle Cell Anemia Control Project, Ahmedabad. Government of Gujarat 2012. [Last accessed on 2016 May 28]. Available from: http://www.sickle-cell.gujarat.gov.in/SC_Program.aspx .
- 11.Kumar R, Panigrahi I, Dalal A, Agarwal S. Sickle cell anemia – Molecular diagnosis and prenatal counseling: SGPGI experience. Indian J Pediatr. 2012;79:68–74. doi: 10.1007/s12098-011-0510-1. [DOI] [PubMed] [Google Scholar]
- 12.Bhukhanvala DS, Sorathiya SM, Shah AP, Patel AG, Gupte SC. Prevalence and hematological profile of ß-thalassemia and sickle cell anemia in four communities of Surat city. Indian J Hum Genet. 2012;18:167–71. doi: 10.4103/0971-6866.100752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rao SS, Goyal JP, Raghunath SV, Shah VB. Hematological profile of sickle cell disease from South Gujarat, India. Hematol Rep. 2012;4:e8. doi: 10.4081/hr.2012.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vasava B, Chudasama R, Godara N, Srivastava R. Prevalence of sickle cell disease in tribal adolescents of the South Gujarat region, India. Internet J Trop Med. 2008;6:1–7. [Google Scholar]
- 15.Saxena D, Moitra M, Shah H, Rao S, Keerti V. Field based utility on dithionate turbidity test for reliable estimation of sickle cell anemia. J Community Med. 2008;4:32–5. [Google Scholar]
- 16.Desai G, Dave K, Banerjee S, Babaria P, Gupta R. Initial outcomes of a comprehensive care model for sickle cell disease among a tribal population in rural Western India. Int J Community Med Public Health. 2016;3:1282–7. [Google Scholar]
- 17.Patel AP, Naik MR, Shah NM, Sharma N, Parmar P. Prevalence of common hemoglobinopathies in Gujarat: An analysis of a large population screening programme. Natl J Community Med. 2012;3:112–6. [Google Scholar]
- 18.Director, Developing Castes Welfare. Department of Social Justice and Empowerment, Gandhinagar. Government of Gujarat, India. 2016. [Last updated on 2016 May 27; Last accessed on 2016 Jun 06]. Available from: https://www.sje.gujarat.gov.in/ddcw/showpage.aspx?contentid=1&lang=english .
- 19.Patel AG, Shah AP, Sorathiya SM, Gupte SC. Hemoglobinopathies in South Gujarat population and incidence of anemia in them. Indian J Hum Genet. 2012;18:294–8. doi: 10.4103/0971-6866.107979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bhatia HM, Rao VR. Genetic Atlas of Indian Tribes. Bombay: Institute of Immunohematology, Indian Council of Medical Research (ICMR); 1987. [Google Scholar]
- 21.Bhukhanvala DS, Sorathiya SM, Shah AP, Patel AG, Gupte SC. Prevalence and hematological profile of ß-thalassemia and sickle cell anemia in four communities of Surat city. Indian J Hum Genet. 2012;18:167–71. doi: 10.4103/0971-6866.100752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pujara K, Dhruva G, Oza H, Agravat A, Dadhania B. Prevalence of anemia, thalassemia and sickle cell anemia in medical students: A three year cross-sectional study in P.D.U. Medical college, Rajkot. Int J Res Med. 2013;2:29–32. [Google Scholar]
- 23.Patel J, Patel B, Gamit N, Serjeant GR. Screening for the sickle cell gene in Gujarat, India: A village-based model. J Community Genet. 2013;4:43–7. doi: 10.1007/s12687-012-0116-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Italia Y, Krishnamurti L, Mehta V, Raicha B, Italia K, Mehta P, et al. Feasibility of a newborn screening and follow-up programme for sickle cell disease among South Gujarat (India) tribal populations. J Med Screen. 2015;22:1–7. doi: 10.1177/0969141314557372. [DOI] [PubMed] [Google Scholar]
- 25.Rajput JH, Naik JP, Italia YM. Clinical evaluation and enhancement of dithionite tube turbidity (DTT) test reagents used for field screening of sickle haemoglobin (HbS) Int J Pharm Life Sci. 2015;6:4280–7. [Google Scholar]
- 26.Saxena D, Mohua M, Kantharia SL. A study on the prevalence of sickle cell disease in the students of three randomly selected schools of Umarpada Taluka. Healthline J Indian Assoc Prev Soc Med. 2004;5:19–21. [Google Scholar]
- 27.Shiladaria DP, Patel DS, Oza HV. Prevalence of anemia, thalassemia and sickle cell disorder in young adults of Gujarat. Natl J Integr Res Med. 2013;4:61–3. [Google Scholar]
- 28.Kokani MJ, Parikh H, Modi MH. Study of hemoglobinopathies in various subcaste of tribal medical students. Int J Med Sci Public Health. 2016;5:505–9. [Google Scholar]
- 29.Bhukhanvala DS, Sorathiya SM, Sawant P, Colah R, Ghosh K, Gupte SC. Antenatal screening for identification of couples for prenatal diagnosis of severe hemoglobinopathies in Surat, South Gujarat. J Obstet Gynaecol India. 2013;63:123–7. doi: 10.1007/s13224-012-0271-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chavda J, Goswami P, Goswami A. Hematological profile of sickle cell disorder in tertiary care hospital. IOSR J Dent Med Sci. 2015;14:51–4. [Google Scholar]
- 31.Patel MR, Prajapti N, Anavadiya J. Comparative study of hypertensive disorder in pregnant women with sickle cell disease and trait. Int J Sci Res. 2015;4:279–80. [Google Scholar]


