Abstract
Background:
Pretreatment loss to follow-up (PTLFU) is used as performance indicator of Revised National Tuberculosis Control Programme (RNTCP) of India.
Objective:
To document the PTLFU, identify additional indicators and examine documentation of all the diagnosed sputum positive pulmonary tuberculosis (PTB) patients under RNTCP.
Methodology:
Tuberculosis (TB) laboratory, referral for treatment registers, and referral forms were perused for information on sputum positive PTB patients diagnosed from January to June 2014, in 3 TB Units in Chennai.
Results:
PTLFU was 24% (572 out of 2361). However, in pursuance with the principle of ensuring that all diagnosed patients must be started on treatment following referral, it was inflated to 44% (1046 out of 2361).
Conclusion:
The existing PTLFU indicator does not reflect the proportion of treatment initiation of all diagnosed smear-positive PTB patients. We propose additional indicators for monitoring referral and treatment initiation of all diagnosed sputum positive PTB patients.
Keywords: Indicator, Revised National Tuberculosis Control Programme, smear positive, treatment initiation, tuberculosis
INTRODUCTION
Globally, in 2014, there were 9.6 million new cases and 1.5 million deaths due to tuberculosis (TB). India accounted for 2.2 million incident TB cases and 0.25 million deaths among them.[1] Treatment initiation of all diagnosed sputum positive pulmonary TB (PTB) patients is important for reducing transmission of disease within the community. The Revised National TB Control Programme (RNTCP) of India uses “Initial Defaulter,” currently known as pretreatment loss to follow-up (PTLFU), as a performance indicator for treatment initiation of diagnosed sputum positive pulmonary TB patients.[2] “Initial Defaulter” or PTLFU under RNTCP is defined as a patient who was diagnosed as a sputum smear-positive case as per the records at the RNTCP laboratory but who had not been placed on RNTCP treatment regimen and also had not been referred for treatment outside the district.[2] It is imperative that information about treatment initiation is available for all the diagnosed sputum positive PTB patients to reduce ongoing disease transmission by bringing them under treatment cover. It is not certain whether PTLFU rate fulfills this program expectation target efficiently. As part of an evaluation study done under RNTCP, we analyzed the PTLFU, examined documentation, and identified potential indicators and its benefits in ensuring treatment initiation of all the diagnosed sputum positive patients under RNTCP.
METHODOLOGY
In 2013, in the 10 tuberculosis units (TUs) in Chennai city Municipal Corporation, Tamil Nadu, South India, 34% of sputum positive PTB patients had delayed treatment initiation of beyond 7 days of diagnosis (unpublished data). An evaluation study to assess the referral and treatment initiation was undertaken in June–July 2015, in the top 3 TUs in which >38% of sputum positive PTB patients had delayed treatment initiation of beyond 7 days of diagnosis. The selected TUs have 23 Microscopy Centres (MC) of the total 67 in Chennai Corporation area. TB laboratory and referral for treatment registers and referral forms from MCs were reviewed to identify sputum positive PTB patients diagnosed from January 1, 2014, to June 30, 2014. The information pertaining to referral within the district, outside the district, and treatment initiation was elicited. This study was approved by the Institutional Ethics Committee of National Institute of Epidemiology.
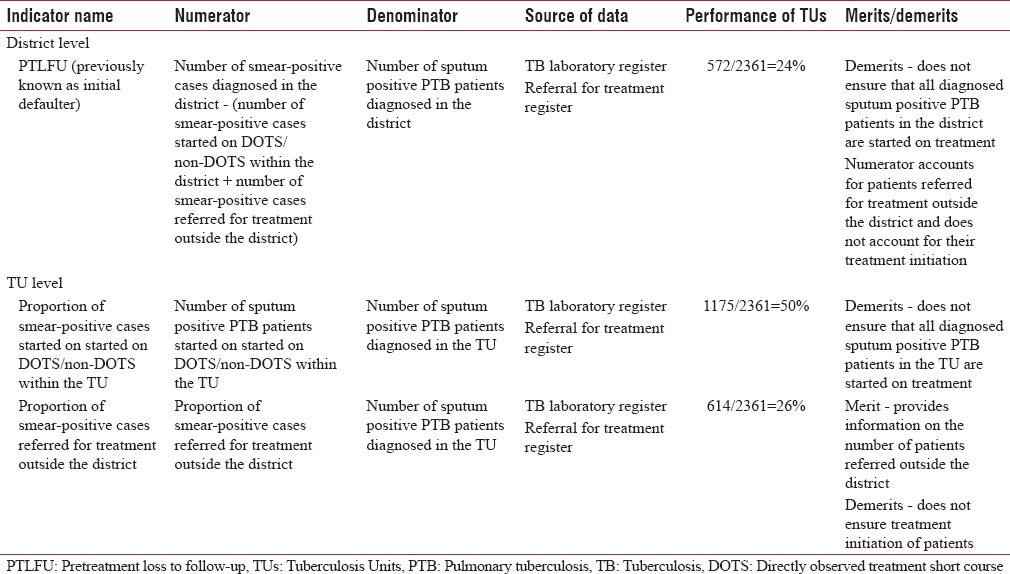
According to RNTCP procedures, sputum positive PTB patients diagnosed in the MCs under RNTCP are required to be referred to treatment centers close to their residence for convenience of initiating DOT. Feedback on treatment initiation is to be obtained, and entries are required to be made by RNTCP designated staff in the TB laboratory and referral for treatment registers. Every attempt has to be made to put all the referred TB patients on treatment as early as possible. If information regarding treatment of such referred patients is not available or if patients have not been initiated on RNTCP regimen, these patients are listed as PTLFU. The District TB Officer has to find out the reasons for PTLFU and make attempts to reduce number of pretreatment losses.[2] The list of PTLFU patients is compiled at the district level and is included in the RNTCP Quarterly reports based on documentation of treatment and referral details in the remarks' column of TB laboratory register and Referral register.[2,3] PTLFU rate under RNTCP was calculated as outlined in Table 1 with the use of other TU level indicators.[2] The merits/demerits of these indicators are also mentioned in Table 1.
Table 1.
Previous indicators at district and tuberculosis unit level for monitoring treatment initiation of diagnosed sputum positive pulmonary tuberculosis patients
The proposed indicators for monitoring treatment initiation of diagnosed sputum positive PTB patient with its merits are described in Table 2.
Table 2.
Proposed indicators at district and tuberculosis unit level for monitoring treatment initiation of diagnosed sputum positive pulmonary tuberculosis patients
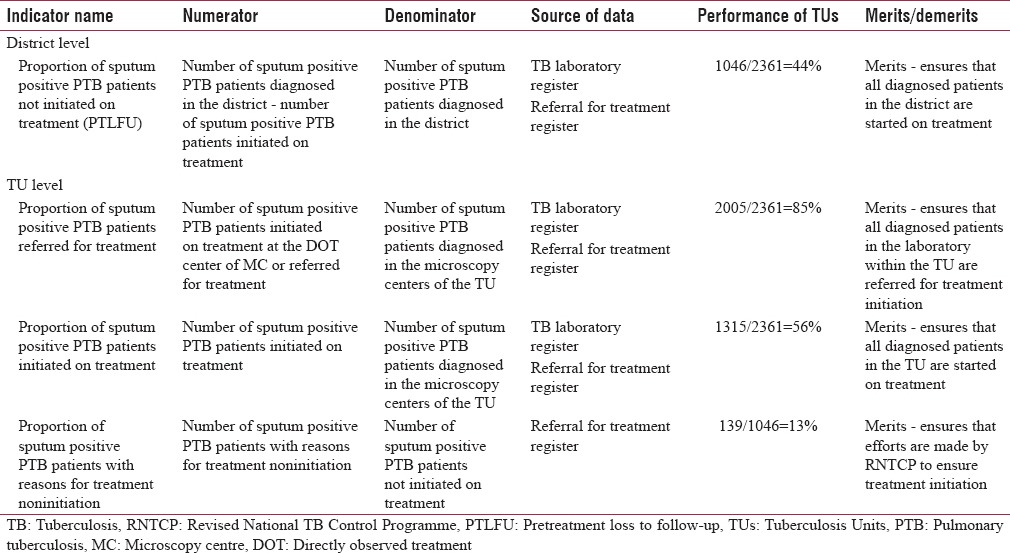
District level indicator
Pretreatment loss to follow-up
Proportion of sputum positive PTB patients not initiated on treatment among those diagnosed in the district.
Tuberculosis unit level indicators
Referral of diagnosed sputum positive PTB patient for treatment center: Proportion of sputum positive PTB patients referred for treatment
Treatment initiation: Proportion of sputum positive PTB patients initiated on treatment
Efforts by RNTCP to ensure treatment initiation: Proportion of patients with reasons for treatment noninitiation.
Data were entered in Excel 7.0 and analyzed using Epi Info version 7.0 (Centers for disease control and prevention, Atlanta, Georgia, USA). Proportions were computed.
RESULTS
The 3 study TUs were considered to represent the district for the purpose of analysis. Of a total of 2361 sputum positive PTB patients diagnosed in the MCs, 1175 (50%) were started on treatment within the district, 614 (26%) were referred for treatment outside the district, and 572 (24%) were PTLFU as per the existing indicators [Table 1]. However, in pursuance with the principle of ensuring that all diagnosed patients must be started on treatment following referral, records verified suggest that 1046 of 2361 diagnosed smear-positive PTB patients were not started on treatment, thereby inflating the true PTLFU rate to 44% [Table 2].
Overall compilation of data from individual TUs for the proposed additional indicators showed that 2005 (85%) of 2361 diagnosed patients had documentation of treatment initiation and or referral to treatment centers; while 15% had no documentation [Table 2]. Information on treatment initiation was available for 1175 (85%) and 140 (23%) of 1391 and 614 who were referred to within and outside district, respectively. Hence, information on treatment initiation was available for a total of 1315 (1175 + 140) (56%) of 2361 diagnosed patients [Table 2]. Of 1046 with no information or not initiated on treatment, reasons (unwilling, not located, died) for treatment noninitiation were available for 139 (13%) [Table 2].
Additional documentation
The technical and operational guideline for TB 2016 has revised the TB laboratory register to capture treatment initiation details (TB no. and TU details/Referral for treatment).[4] In addition to this information, entering date for referral and start of treatment will help in assessing the time delay. The reasons for treatment noninitiation could be entered in the “Remarks” column.
DISCUSSION
The existing calculation of PTLFU rate under RNTCP did not ensure that all the diagnosed sputum positive PTB patients are started on treatment since it accounted only for referral of patients outside the district and not treatment initiation of those patients. Our analysis showed that PTLFU rate would be much higher as 44% compared to 24% if treatment initiation of all diagnosed patients irrespective of within or outside district is taken into account. The PTLFU indicator which we propose at the district level can be used to monitor treatment initiation of all diagnosed smear-positive PTB patients in the district.
Documentation of treatment initiation is of prime importance since PTLFU rate is a record-based indicator. A previous study in India has shown that 47.5% patients who had been placed on treatment, had been incorrectly reported as Initial defaulters due to poor documentation.[5] We did not verify this information in our study. Nevertheless, we identified documentation of treatment initiation in 56% of diagnosed PTB patients with poor contribution from patients referred outside the district. This reflects on the efficiency of the feedback mechanism and documentation. Coordinated efforts at the district level among program managers are essential to achieve appropriate information on patients referred outside the district. This emphasizes the need for indicators at the TU level to closely monitor treatment initiation of all diagnosed smear-positive PTB patients.
Our analysis showed that 15% of diagnosed sputum smear-positive PTB patients have no documentation on treatment initiation and or referral to treatment centers. This is a matter of concern, and this indicator underscores the need for efforts by RNTCP staff to reduce this. Documentation of reasons for treatment noninitiation was in 13% of patients. Reasons for initial default have been documented in previous studies which include death and treatment in private sector.[5,6] It is imperative that reasons are documented for all diagnosed patients not started on treatment under program settings. Since PTLFU is an important issue for good TB control at facility, national and global level more attention has to be paid to find out what happens to smear-positive patients.[7]
The revised technical and operational guideline for TB 2016 has monitoring indicator for time to treatment initiation after diagnosis.[4] It has not emphasized on monitoring indicators to ensure referral and treatment initiation of all smear-positive TB patients diagnosed at the laboratory.
The limitation of the analysis is that data used for analysis are limited to 34% of the MCs in the district. The data are based on documentation available in TB laboratory and referral registers as per the RNTCP guidelines that existed during the study period. We did not quantify the missed documentation. NIKSHAY entry had begun in the 3TUs in 2014, and the data were being updated.
CONCLUSION
This communication was to highlight the deficiency in the indicator that was used to ensure treatment initiation of diagnosed sputum smear-positive PTB patients. Program managers could consider district and TU level indicators for referral and treatment initiation of diagnosed sputum smear-positive PTB patients. In addition, the e-portal NIKSHAY offers scope as source of data for the monitoring indicators as per the revised RNTCP guidelines. This could potentially support in monitoring and help to identify lacunae in the performance of activities pertaining to treatment initiation under RNTCP.
Financial support and sponsorship
This study was supported by National Institute of Epidemiology, Field Epidemiology training Programme.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We wish to thank the Commissioner of Chennai and the Health Officer for granting permission to do this study. We wish to thank the staff of RNTCP for their cooperation in providing the required data.
REFERENCES
- 1.World Health Organization. Global Tuberculosis Report 2015. Geneva: World Health Organization; 2015. [Last accessed on 2015 Dec 10]. Available from: http://www.apps.who.int/iris/bitstream/10665/191102/1/9789241565059_eng.pdf?ua=1 . [Google Scholar]
- 2.Central TB Division. Revised National TB Control Programme. Managing RNTCP in Your Area – A Training Course (Module 5-9) [Last accessed on 2015 Dec 10]. Available from: http://www.tbcindia.nic.in/showfile.php?lid=2911 .
- 3.Central TB Division. Revised National TB Control Programme. Managing RNTCP in Your Area – A Training Course (Module 1-4) [Last accessed on 2015 Dec 10]. Available from: http://www.tbcindia.nic.in/showfile.php?lid=2907 .
- 4.Central TB Division. Revised National TB Control Programme. Technical and Operational Guidelines for Tuberculosis Control in India. 2016. [Last accessed on 2016 Apr 02]. Available from: http://www.999projects.co.in/tb-1/files/Download/Revised%20Technical%20and%20operational%20Guidelines%20for%20TB.pdf.pdf .
- 5.Sai Babu B, Satyanarayana AV, Venkateshwaralu G, Ramakrishna U, Vikram P, Sahu S, et al. Initial default among diagnosed sputum smear-positive pulmonary tuberculosis patients in Andhra Pradesh, India. Int J Tuberc Lung Dis. 2008;12:1055–8. [PubMed] [Google Scholar]
- 6.Botha E, Den Boon S, Verver S, Dunbar R, Lawrence KA, Bosman M, et al. Initial default from tuberculosis treatment: How often does it happen and what are the reasons? Int J Tuberc Lung Dis. 2008;12:820–3. [PubMed] [Google Scholar]
- 7.Harries AD, Rusen ID, Chiang CY, Hinderaker SG, Enarson DA. Registering initial defaulters and reporting on their treatment outcomes. Int J Tuberc Lung Dis. 2009;13:801–3. [PubMed] [Google Scholar]


