Abstract
The aim of the study was to investigate whether carbon nanoparticles (CNs) can improve the dissection of lymph nodes and protect parathyroid glands (PGs) during reoperation for patients with papillary thyroid carcinoma (PTC).
PTC patients who previously underwent thyroidectomy and later received reoperation between January 2009 and January 2016 were retrospectively recruited. We compared the patients who had CN suspension injected into the residual thyroid gland with a control group of patients who did not have the injection. The primary endpoints were the number of lymph nodes dissected, the number of PGs identified and reimplanted, and the rate of postoperative hypoparathyroidism.
CN suspension injection was conducted in 55 of 174 patients. The total number of lymph nodes and metastatic lymph nodes dissected between the 2 groups were not different (22.8 ± 13.7 vs 21.0 ± 13.3, P = .481 and 5.5 ± 3.8 vs 4.8 ± 4.0, P = .695). The number of central lymph nodes and metastatic central lymph nodes in the CN group was significantly higher than those dissected in the control group (8.7 ± 6.9 vs 6.2 ± 5.2, P = .037 and 2.7 ± 1.9 vs 2.1 ± 1.6, P = .012). More PGs were identified (2.42 ± 1.15 vs 1.58 ± 1.12, P = .001) and fewer were reimplanted (48 vs 90, P = .040) in the CN group. Patients who had CN suspension injection had a lower rate of transient hypoparathyroidism (14/55 vs 50/119, P = .043) but no significant difference in the rate of permanent hypoparathyroidism (1/55 vs 9/119, P = .173).
CN suspension injection improves dissection of central lymph nodes and identification of PG in PTC patients undergoing reoperation and lowers the rate of postoperative transient hypoparathyroidism.
Keywords: carbon nanoparticles, central lymph node, papillary thyroid carcinoma, parathyroid gland, reoperation
1. Introduction
Papillary thyroid cancer (PTC) is one of the fastest growing group of cancers in recent years.[1–3] Although the majority of PTC patients have an excellent prognosis,[4] it unfortunately involves cervical lymph nodes in 20% to 90% of the patients. Regional lymph nodes metastases may be present even when the primary tumor is small and intrathyroidal.[1,5–8] The standard surgeries for PTC advocated by American Thyroid Association include thyroid lobectomy (LT), near-total thyroidectomy (NTT), and total thyroidectomy (TT). Until now, it is still controversial about prophylactic central lymph nodes dissection (CLND). Recent studies have found that TT in conjunction with prophylactic CLND could decrease locoregional recurrence in PTC patients.[9,10] Therefore, nonstandard surgeries and without prophylactic CLND often lead to gradually increasing recurrence and reoperation rates of PTC.[11]
Reoperation for PTC is usually difficult because of the destruction of normal anatomical structures, adhesion of surrounding tissues, and formation of cicatrization. Hypoparathyroidism, which may seriously affect the postoperative quality of life, is one of the most common and serious complications in PTC reoperation because of accidental parathyroid gland (PG) resection or damage of glandular blood supply. Previous studies have revealed that the incidence of hypoparathyroidism in reoperation was 3 to 5 times higher than in the primary surgery.[12–15] Therefore, a clear identification of PGs and accurate dissection of lymph nodes are essential for reducing hypoparathyroidism and locoregional recurrence during reoperation for PTC patients.
Recently, a lymphatic tracer---carbon nanoparticle (CN)---has been applied in reoperation for PTC. It was reported that CN could effectively guide cervical node dissection and protect PG.[16,17] However, part of thyroid lymphatic network might be damaged in the initial surgery, leading to some lymph nodes unstained black. Therefore, the effect of CN on lymph node dissection and PG protection is still controversial. The aim of the study was to further investigate whether CN could improve lymph nodes dissection and aid to identify and protect PGs during reoperation for PTC patients.
2. Materials and methods
2.1. Patients
PTC patients who previously underwent thyroidectomy and later received reoperation at the Department of Thyroid Surgery of West China Hospital between January 2009 and January 2016 were retrospectively recruited. They were diagnosed as PTC by histopathological examination. According to the application of CN suspension in the reoperation or not, they were divided into 2 groups: the CN group and control group. In the CN group, CN (Lai Mei Pharmaceutical Co, Chongqing, China) suspension (1 mL: 50 mg) was injected into the residual thyroid gland, while it was not used in the control group. All the patients were informed and agreed to follow-up at least 6 months after reoperation. The research was approved by the medical ethics committee of West China Hospital.
2.2. Surgical procedures
The surgical procedures were performed as follows: after anesthesia intubation, the patients were placed supinely with cervical hyperextension. The original anterior cervical curve incision was selected and extended appropriately in most patients. The front part of residual thyroid gland was exposed after entering along with the outside of the linea alba cervicalis or strap muscles. The lateral and posterior parts of residual thyroid gland were not separated to reduce damage to the thyroid capsule and surrounding thyroid lymphatic network, which could prevent the possibility that the extravasation of the CN suspension affected the surgical field. In the CN group, after the front part of residual thyroid gland was exposed, CN suspension was slowly injected into the gland using a skin test needle at 1 or 2 selected points in the residual thyroid (0.1 mL each point). Injection into lesions or blood vessels was avoided. After the injection at each point, the site was gently pressed for 1 minute with sterile gauze to prevent solution leakage. Then, the surgical resection could be started 10 minutes later. The residual thyroid gland and surrounding lymph nodes were stained black, whereas the PGs were not (Figs. 1 and 2). Suspicious PG was partly sent for intraoperative frozen biopsy in both groups. PG was wrapped in gauze soaked with normal saline solution for later autotransplantation. Intraoperative neuromonitoring (Medtronic NIM-Response 2.0, Medtronic Xomed, Inc.) was used to identify recurrent laryngeal nerve. The indication for reoperation of PTC patients was recurrence in residual thyroid gland and/or lymph nodes.
Figure 1.
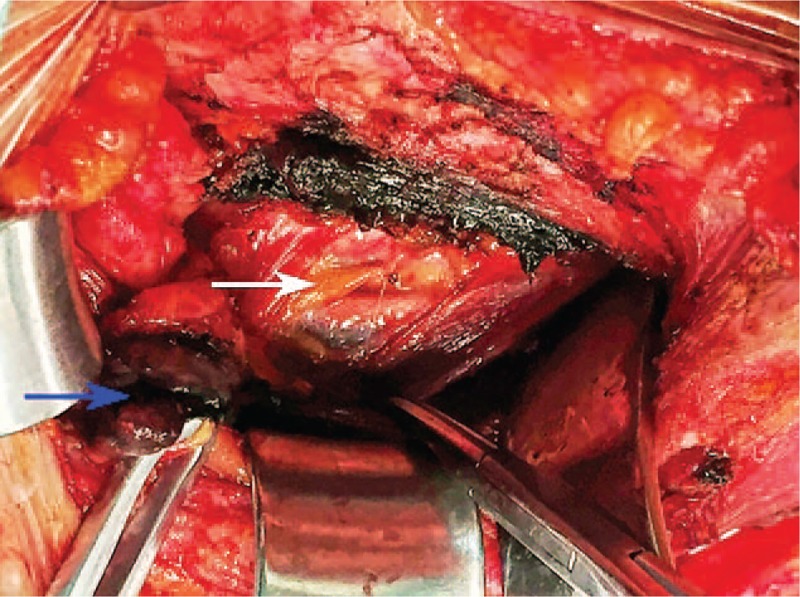
Left inferior parathyroid gland (white arrow) and adjacent black-stained lymph nodes (blue arrow).
Figure 2.
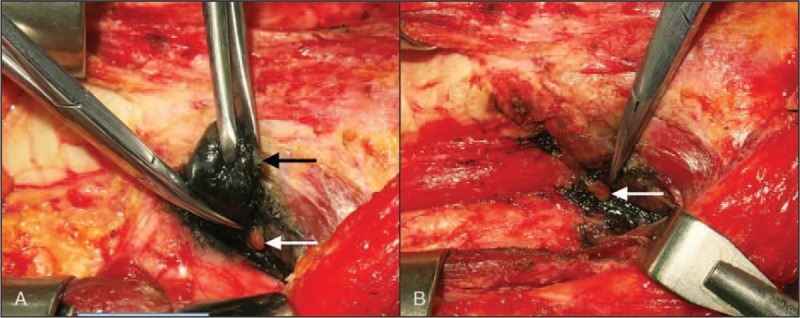
Residual thyroid gland (A, black arrow) and left superior parathyroid gland (A and B, white arrow).
2.3. Perioperative management
Parathyroid hormone (PTH), serum calcium, and thyroid function were routinely measured before reoperation. Thyroid ultrasound and laryngoscope were also carried out in each patient. PTH was routinely measured 1 day, 3 days, 30 days, and 3 months after reoperation. When a PTH measurement was below 1.6 pmol/L (normal range, 1.6–6.9 pmol/L), it was defined as postoperative hypoparathyroidism. Oral calcium supplement or intravenous substitution of calcium therapy was conducted to the patients with symptomatic hypocalcemia. A final PTH measurement was done to these patients 6 months after reoperation. If PTH did not recover to normal, hypoparathyroidism was defined as permanent, otherwise it was defined as transient.
2.4. Data Collection
General characteristics, preoperative tests, intraoperative factors, pathologic examination, the number of lymph nodes and metastatic lymph nodes retrieved in the resected specimens, and postoperative complications were collected retrospectively. Accidental PG resection was defined as not finding PG during reoperation (including careful inspection of the resected specimens) but finding it in the final pathological examination. The seventh edition of American Joint Committee on Cancer (AJCC) staging was used for all the recruited patients.[18] The primary endpoints were the number of lymph nodes dissected, the number of PGs identified and reimplanted, and the rate of postoperative hypoparathyroidism.
2.5. Statistical analysis
All the continuous variables were presented as mean ± standard deviation. Statistical analyses were performed by using SPSS computer software (version 19.0, SPSS, Inc, Chicago, IL). Statistical comparisons were done between the CN group and control group by using the χ2 test or the Student t test. P < .05 was considered statistically significant.
3. Results
3.1. Patient characteristics
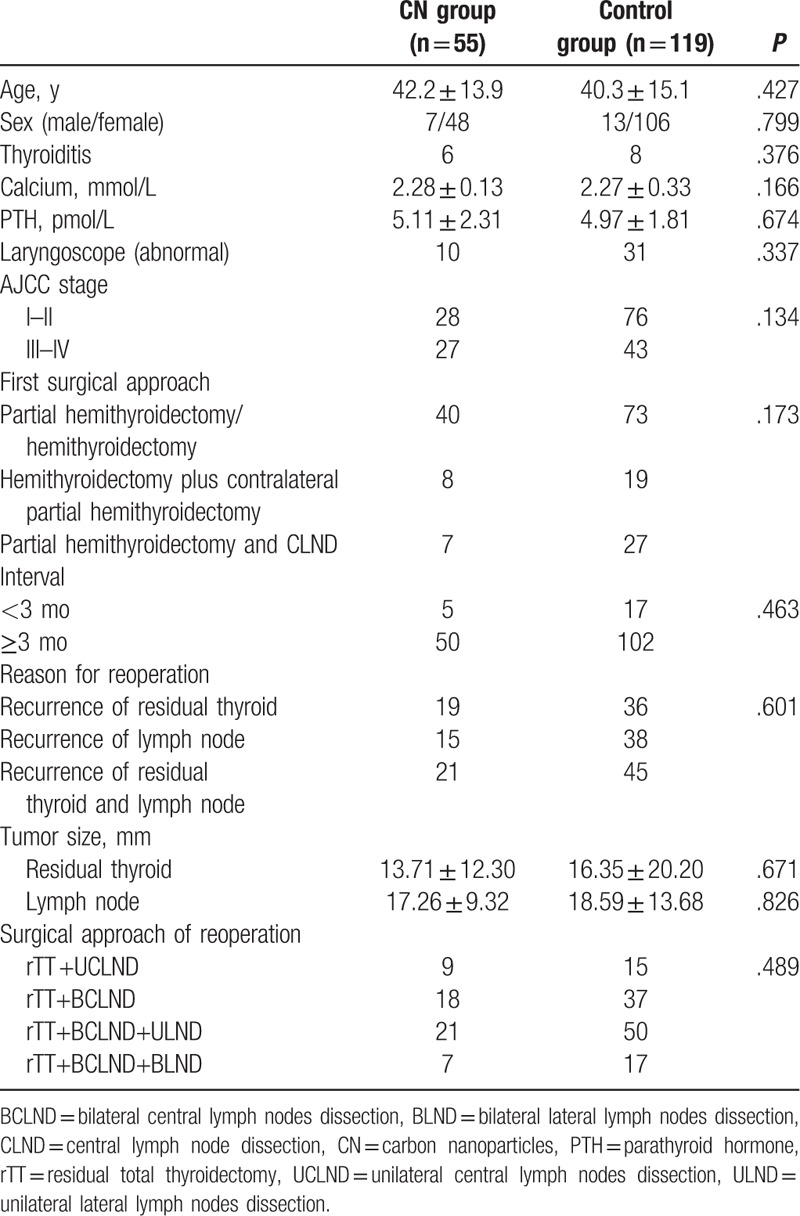
Of the 174 patients recruited in the study, 55 received CN suspension injection and 119 were in the control group. As summarized in Table 1, no significant difference was noted for clinical characteristics between the 2 groups. There was also no significant difference between them in terms of PTC pathological stages, the first surgical approach, the interval between the first surgery and reoperation, reason for reoperation, tumor size, and the surgical approach of reoperation. None of them accepted radioactive iodine ablation after the initial surgery because of the residual thyroid gland.
Table 1.
Clinical characteristics of the patients in the 2 groups.
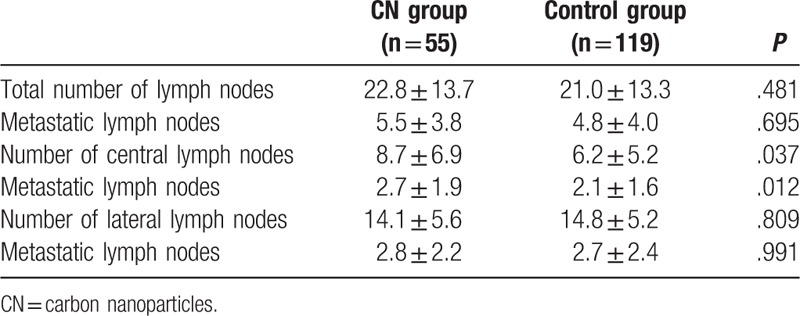
3.2. Lymph nodes dissection
In the CN group, a total of 479 central lymph nodes and 775 lateral lymph nodes were dissected, with an average of 22.8 ± 13.7 per patient. Among them, 303 lymph nodes (24.2%) were confirmed to be metastatic lymph nodes. The metastatic rates of central lymph nodes and lateral lymph nodes were 31.1% (149/479) and 19.9% (154/775), respectively. In the control group, a total of 2499 lymph nodes were dissected, with an average of 21.0 ± 13.3 per patient. The difference of the total number of lymph nodes and metastatic lymph nodes between the 2 groups was not statistically significant (P = .481 and P = .695). But the number of central lymph nodes and metastatic central lymph nodes in the CN group was significantly higher than those dissected in the control group (P = .037 and P = .012) (Table 2).
Table 2.
Lymph nodes dissection per patient in the 2 groups.
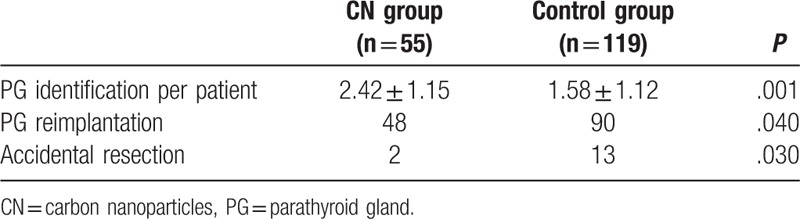
3.3. PG identification and protection
A total of 133 and 188 PGs were identified, respectively, in the CN group and control group. Forty-eight PGs (36.1%) in the CN group and 90 (47.9%) in the control group were reimplanted (P = .040). Final pathological examination revealed 2 cases of accidental PG resection in the CN group, whereas 13 cases of accidental PG removal occurred in the control group. There was statistically significant difference between the 2 groups (P = .030) (Table 3).
Table 3.
The details of PG identification and protection in the 2 groups.
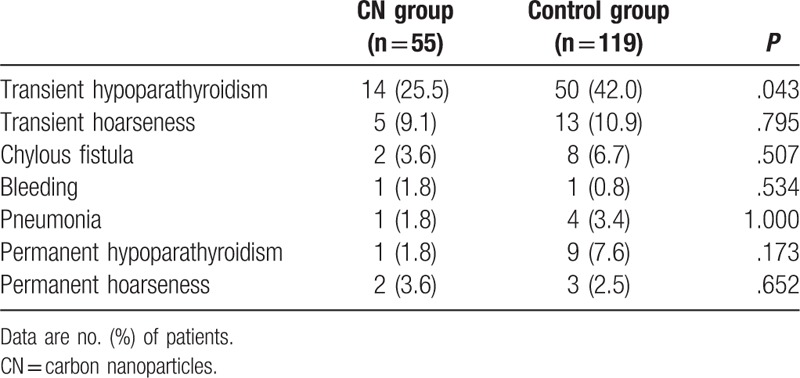
3.4. Postoperative complications and follow-up
Table 4 summarizes the postoperative complications in the 2 groups. Transient hypoparathyroidism was documented in 14 of the 55 patients (25.5%) in the CN group and in 50 of the 119 patients (42.0%) in the control group (P = .043). No significant differences were found between the 2 groups in terms of occurrence of transient hoarseness, chylous fistula, bleeding, and pneumonia. All the patients completed a 6-month follow-up. One patient (1.8%) in the CN group and 9 (7.6%) in the control group were diagnosed as permanent hypoparathyroidism (P = .173). Permanent hoarseness was found in 2 patients (3.6%) in the CN group and 3 (2.5%) in the control group. There was no statistically significant difference between the 2 groups (P = .652).
Table 4.
The postoperative complications in the 2 groups.
4. Discussion
In recent years, the increasing incidence of PTC in China is accompanied by the elevated reoperation rate. The primary causes of reoperation are insufficient resection in the initial surgery and postoperative cervical recurrence of residual thyroid or regional lymph node (s). The aforementioned standard surgeries for PTC only include LT, NTT, and TT. However, subtotal or partial hemithyroidectomy, partial thyroidectomy, and tumorectomy are always performed in the initial surgery in China because of the serious medical environment and lack of well-trained thyroid surgeons and intraoperative frozen biopsy. The reported incidence of cervical recurrence was 20% in low-risk PTC patients and 59% in high-risk PTC patients.[19–21] Although there is no direct relationship between reoperation and the development of extracervical metastasis as well as the reduction of survival time, reoperation is independently associated with a high incidence of postoperative complications.[20,22]
Hypoparathyroidism is a common complication after thyroid surgery, especially after reoperation.[23] In literature, the incidence of transient hypoparathyroidism after resurgery is reported to be 0% to 47.3%, while that of permanent hypoparathyroidism is 0% to 7.6%.[24–26] In the present study, the incidences of transient hypoparathyroidism and permanent hypoparathyroidism were 36.8% (64/174) and 5.7% (10/174), respectively, which are consistent with the previous studies. Patients with mild transient hypoparathyroidism often present as hand and foot numbness, while severe cases always have hypocalcemic tetany. These symptoms can return to normal after oral or intravenous administration of calcium. Moreover, transient hypoparathyroidism can rapidly improve during the next 1 to 2 months after reoperation.[26] However, hypocalcemic tetany, depression, confusion of consciousness, and other mental symptoms frequently occur in patients with permanent hypoparathyroidism. Therefore, long-term oral or intravenous supplement of calcium and medical testing are required to keep the level of serum calcium, which would cause a heavy physical, mental, and economic burden to them and also lead to medical disputes.
The main causes of postoperative hypoparathyroidism include accidental PG resection and damage of PG or its blood supply.[27,28] Surgical experience and good familiarity of the normal anatomical variations of the PGs are essential for diminishing the incidence of postoperative hypoparathyroidism. However, as to the PTC reoperation, these factors are necessary but not sufficient because of accidental resection or devascularization of the PGs during the first surgery. In addition, due to the disappearance of the anatomical structures and formation of strong adhesions, it is more difficult to seek and identify the PGs.[14]
Several strategies have been applied to visualize PGs intraoperatively. Use of loupes magnification and microsurgical technique can facilitate PGs identification and avoid their devascularization.[29] Although 99mtechnetium-sestamibi (99mTC-MIBI) is always used as a radiotracer for intraoperative localization of adenomatous PGs, it can label normal PGs for gamma probe identification.[30,31] Staining agents play an important role in the PGs identification. Methylene blue is the most widely used agent. It can sensitively stain enlarged PGs, such as parathyroidoma. However, it may falsely stain thyroid, lymph nodes, and normal PGs. Toxic metabolic encephalopathy occasionally occurs in patients taking serotonin reuptake inhibitors and serotonergic medication after intravenous application of methylene blue.[32] In recent years, some studies have reported that the application of CN suspension could significantly improve the dissection of lymph nodes and reduce the incidence of postoperative hypoparathyroidism during TT with CLND, regardless of the first surgery or resurgery.[16,17,33–35] The crucial components for CN suspension injection are nanocarbon granules with an average diameter of 150 nm, which could only pass through the lymphatic capillaries rather than the blood capillaries due to the difference in permeability. There are rich lymphatics and lymphatic capillaries in the thyroid, whereas almost none within the PGs. In addition, there are anatomically independent external capsules between them.[36] Therefore, CN can make the thyroid gland and the surrounding lymph nodes black-stained, but not for PGs. After rapidly identifying PGs and distinguishing them from thyroid and surrounding lymph nodes by CN, complete lymph nodes dissection and preservation of PGs become feasible.[37]
However, in the present study, CN could not significantly improve lymph nodes dissection, except for the CLND. The main reasons are as follows: Partial thyroid capsule and surrounding thyroid lymphatic network may be destroyed in the previous surgery, resulting in some lymph nodes maintaining original color. CN may stain the central lymph nodes around the recurrent laryngeal nerve, particularly the smaller ones underneath it, leading to more radical CLND. Black-stained lymph nodes, especially the small ones, are more easily identified by pathologists. Lateral lymph nodes dissection is performed standard in our center. Sample size of the study is limited. In accordance with the previous studies, CN could not only effectively aid in identifying PGs but also significantly reduce the accidental resection and reimplantation rates during PTC reoperation, resulting in the significantly lower incidence of transient hypoparathyroidism (25.5% vs 42.0%). Although the difference was insignificant, the incidence of permanent hypoparathyroidism was lower in the CN group than in the control group (1.8% vs 7.6%). The main causes of the aforementioned results may be the small sample size and experienced surgeons. Meanwhile, application of CN did not increase the postoperative complications and no adverse side effects were found in the study, which further confirmed the safety.
5. Conclusion
The present study shows that CN suspension injection improves dissection of central lymph nodes and identification of PG in PTC patients undergoing reoperation and lowers the rate of postoperative transient hypoparathyroidism.
Footnotes
Abbreviations: CN = carbon nanoparticles, PG = parathyroid gland, PTC = papillary thyroid cancer, LT = thyroid lobectomy, NTT = near-total thyroidectomy, TT = total thyroidectomy, CLND = central lymph nodes dissection, PTH = parathyroid hormone.
Both Su AP and Wang B contributed equally to this study.
Funding/support: The study was supported by the National Natural Science Fund (81502612) and Scientific Research Fund of Science and Technology Department of Sichuan Province (2016SZ0045).
The authors report no conflicts of interest.
References
- [1].Hundahl SA, Fleming ID, Fremgen AM, et al. A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 1985-1995. Cancer 1998;83:2638–48. [DOI] [PubMed] [Google Scholar]
- [2].Leenhardt L, Bernier MO, Boin-Pineau MH, et al. Advances in diagnostic practices affect thyroid cancer incidence in France. Eur J Endocrinol 2004;150:133–9. [DOI] [PubMed] [Google Scholar]
- [3].Sonkar AA, Rajamanickam S, Singh D. Papillary thyroid carcinoma: debate at rest. Indian J Cancer 2010;47:206–16. [DOI] [PubMed] [Google Scholar]
- [4].LiVolsi VA. Papillary thyroid carcinoma: an update. Mod Pathol 2011;24:S1–9. [DOI] [PubMed] [Google Scholar]
- [5].Grebe SK, Hay ID. Thyroid cancer nodal metastases: biologic significance and therapeutic considerations. Surg Oncol Clin N Am 1996;5:43–63. [PubMed] [Google Scholar]
- [6].Chow SM, Law SC, Chan JK, et al. Papillary microcarcinoma of the thyroid: prognostic significance of lymph node metastasis and multifocality. Cancer 2003;98:31–40. [DOI] [PubMed] [Google Scholar]
- [7].Ito Y, Uruno T, Nakano K, et al. An observation trial without surgical treatment in patients with papillary microcarcinoma of the thyroid. Thyroid 2003;13:381–7. [DOI] [PubMed] [Google Scholar]
- [8].Abboud B, Tannoury J. Surgical treatment of papillary thyroid carcinoma. J Med Liban 2011;59:206–12. [PubMed] [Google Scholar]
- [9].Wang TS, Cheung K, Farrokhyar F, et al. A meta-analysis of the effect of prophylactic central compartment neck dissection on locoregional recurrence rates in patients with papillary thyroid cancer. Ann Surg Oncol 2013;20:3477–83. [DOI] [PubMed] [Google Scholar]
- [10].Zhu W, Zhong M, Ai Z. Systematic evaluation of prophylactic neck dissection for the treatment of papillary thyroid carcinoma. Jpn J Clin Oncol 2013;43:883–8. [DOI] [PubMed] [Google Scholar]
- [11].Dralle H, Lorenz K, Machens A. State of the art: surgery for endemic goiter: a plea for individualizing the extent of resection instead of heading for routine total thyroidectomy. Langenbecks Arch Surg 2011;396:1137–43. [DOI] [PubMed] [Google Scholar]
- [12].Onkendi EO, McKenzie TJ, Richards ML, et al. Reoperative experience with papillary thyroid cancer. World J Surg 2014;38:645–52. [DOI] [PubMed] [Google Scholar]
- [13].Ito Y, Kihara M, Kobayashi K, et al. Permanent hypoparathyroidism after completion total thyroidectomy as a second surgery: how do we avoid it? Endocr J 2014;61:403–8. [DOI] [PubMed] [Google Scholar]
- [14].Lefevre JH, Tresallet C, Leenhardt L, et al. Reoperative surgery for thyroid disease. Langenbecks Arch Surg 2007;392:685–91. [DOI] [PubMed] [Google Scholar]
- [15].Kim MK, Mandel SH, Baloch Z, et al. Morbidity following central compartment reoperation for recurrent or persistent thyroid cancer. Arch Otolaryngol Head Neck Surg 2004;130:1214–6. [DOI] [PubMed] [Google Scholar]
- [16].Chaojie Z, Shanshan L, Zhigong Z, et al. Evaluation of the clinical value of carbon nanoparticles as lymph node tracer in differentiated thyroid carcinoma requiring reoperation. Int J Clin Oncol 2016;21:68–74. [DOI] [PubMed] [Google Scholar]
- [17].Gao B, Tian W, Jiang Y, et al. Application of carbon nanoparticles for parathyroid protection in reoperation of thyroid diseases. Int J Clin Exp Med 2015;8:22254–61. [PMC free article] [PubMed] [Google Scholar]
- [18].NCCN Clinical Practice Guidelines in Oncology. NCCN Guidelines: Thyroid Carcinoma. Version 3. 2011. [Google Scholar]
- [19].Cady B, Rossi R. An expanded view of risk-group definition in differentiated thyroid carcinoma. Surgery 1988;104:947–53. [PubMed] [Google Scholar]
- [20].Mazzaferri EL. NCCN thyroid carcinoma practice guidelines. Oncology (Huntingt) 1999;13:391–442. [Google Scholar]
- [21].Hay ID, McConahey WM, Goellner JR. Managing patients with papillary thyroid carcinoma: insights gain from the Mayo Clinic's experience of treating 2,512 consecutive patients during 1940 through 2000. Trans Am Clin Climatol Assoc 2002;113:241–60. [PMC free article] [PubMed] [Google Scholar]
- [22].Esnaola NF, Cantor SB, Sherman SI, et al. Optimal treatment strategy in patients with papillary thyroid cancer: a decision analysis. Surgery 2001;130:921–30. [DOI] [PubMed] [Google Scholar]
- [23].Ban EJ, Yoo JY, Kim WW, et al. Surgical complications after robotic thyroidectomy for thyroid carcinoma: a single center experience with 3,000 patients. Surg Endosc 2014;28:2555–63. [DOI] [PubMed] [Google Scholar]
- [24].Seiler CA, Vorburger SA, Bürgi U, et al. Extended resection for thyroid disease has less operative morbidity than limited resection. World J Surg 2007;31:1005–13. [DOI] [PubMed] [Google Scholar]
- [25].Pironi D, Panarese A, Candioli S, et al. Reoperative thyroid surgery: personal experience and review of the literature. G Chir 2008;29:407–12. [PubMed] [Google Scholar]
- [26].Pelizzo MR, Variolo M, Bernardi C, et al. Complications in thyroid resurgery: a single institutional experience on 233 patients from a whole series of 4,752 homogeneously treated patients. Endocrine 2014;47:100–6. [DOI] [PubMed] [Google Scholar]
- [27].Ahn D, Sohn JH, Park JY. Surgical complications and recurrence after central neck dissection in cN0 papillary thyroid carcinoma. Auris Nasus Larynx 2014;41:63–8. [DOI] [PubMed] [Google Scholar]
- [28].Shen WT, Ogawa L, Ruan D, et al. Central neck lymph node dissection for papillary thyroid cancer: comparison of complication and recurrence rates in 295 initial dissections and reoperations. Arch Surg 2010;145:272–5. [DOI] [PubMed] [Google Scholar]
- [29].D’Orazi V, Panunzi A, Di Lorenzo E, et al. Use of loupes magnification and microsurgical technique in thyroid surgery: ten years experience in a single center. G Chir 2016;37:101–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Pasta V, Monteleone F, Del Vecchio L, et al. Original technique for preoperative preparation of patients and intraoperative localization of parathyroid adenomas. G Chir 2015;36:97–100. [PMC free article] [PubMed] [Google Scholar]
- [31].Grubbs EG, Mittendorf EA, Perrier ND, et al. Gamma probe identification of normal parathyroid glands during central neck surgery can facilitate parathyroid preservation. Am J Surg 2008;196:931–6. [DOI] [PubMed] [Google Scholar]
- [32].Patel HP, Chadwick DR, Harrison BJ, et al. Systematic review of intravenous methylene blue in parathyroid surgery. Br J Surg 2012;99:1345–51. [DOI] [PubMed] [Google Scholar]
- [33].Gu J, Wang J, Nie X, et al. Potential role for carbon nanoparticles identification and preservation in situ of parathyroid glands during total thyroidectomy and central compartment node dissection. Int J Clin Exp Med 2015;8:9640–8. [PMC free article] [PubMed] [Google Scholar]
- [34].Yu W, Cao X, Xu G, et al. Potential role for carbon nanoparticles to guide central neck dissection in patients with papillary thyroid cancer. Surgery 2016;160:755–61. [DOI] [PubMed] [Google Scholar]
- [35].Zhu J, Tian W, Xu Z, et al. Expert consensus statement on parathyroid protection in thyroidectomy. Ann Transl Med 2015;3:230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Huang K, Luo D, Huang M, et al. Protection of parathyroid function using carbon nanoparticles during thyroid surgery. Otolaryngol Head Neck Surg 2013;149:845–50. [DOI] [PubMed] [Google Scholar]
- [37].Li J, Li X, Wang Z. Negative developing of parathyroid using carbon nanoparticles during thyroid surgery. Gland Surg 2013;2:100–1. [DOI] [PMC free article] [PubMed] [Google Scholar]


