Abstract
The aim of this study was to investigate the risk factors of wound infection after open reduction and internal fixation of calcaneal fractures.
In all, 299 patients with 318 calcaneal fractures who underwent open reduction and internal fixation by a single surgeon were grouped according to different outcomes. We gathered the data on each patient including sex, age, injury mechanism, body mass index (BMI), time to operation, fracture type, associated injuries, treatment course, tourniquet time, blood loss, bone graft (yes or no), diabetes (yes or no), smoking history, and complications. Univariate analysis and multivariable analysis were used to determine the association between risk factors and wound infection.
Patients who met the entry criteria included 267 males and 32 females with a mean age of 38.6 years. Among them, 5.3% (n = 17) suffered wound infection, and all of the wounds healed after different treatments. According to the univariate analysis, the patients who developed wound infections were active smokers, more obese (higher BMI), had a longer time from injury to operation, and longer tourniquet time. Multivariate analysis indicated that a higher BMI, delayed operation, and active smoking were independent risk factors for wound infection after open reduction and internal fixation of calcaneal fractures.
Patients with calcaneal fractures who were smokers and had a higher BMI had a high risk of wound infections. We suggested that surgeons wait to operate until swellings of the injured foot improved, and we also suggested the operation should be within 14 days after the injury.
Keywords: calcaneal fractures, open reduction and internal fixation, risk factors, wound infection
1. Introduction
Historically, calcaneal fractures were treated nonsurgically.[1,2] Although nonoperative treatment can achieve good result in patients with type I fractures, if nonoperative treatment is used in patients with other types of fractures, the incidence rate of early subtalar arthritis is higher in nonoperative patients than in operative patients.[3] With the development of internal fixation techniques and material application in orthopedics, more and more surgeons have suggested that open reduction and internal fixation can achieve good outcomes.[4–6] However, operative treatment also leads to a series of complications including wound infection, which is devastating for the patient. In the literature, the rate of infection was reported as 5% to 25%,[7–11] and wound dressing, debridement, flaps repair, and even amputation were performed on patients who suffered wound infection. It is a heavy psychological and physiological blow to patients and implies a longer stay in hospital, more expense, and more pain. A series of studies revealed that wound infection is a multifactorial problem and there is no 1 causative factor.[7,8,10–15] Inevitably, there is still a lot of controversy about the risk factors related to wound infection, especially the surgical timing. Therefore, the aim of this study was to identify the risk factors of wound infection after open reduction and internal fixation of calcaneal fractures.
2. Patients and methods
Permission for this study was obtained from the Medical Ethics Committee of The General Hospital of Jinan Military Command.
In all, 469 patients were diagnosed with calcaneal fractures in our institution between January 2006 and June 2014. Exclusion criteria for patients were as follows: (1) age younger than 16 years; (2) open calcaneal fractures; (3) type I calcaneal fracture (Sanders classification); (4) treated conservatively; (5) fractures fixed with the percutaneous technique; and (6) those performed by other surgeons. Among them, 299 patients with 318 calcaneal fractures who underwent open reduction and internal fixation were grouped according to the different outcomes. We gathered the data on each patient including: sex, age, injury mechanism, body mass index (BMI), time to operation, fracture type, associated injuries, treatment course, tourniquet time, blood loss, bone graft (yes or no), diabetes (yes or no), smoking history, and complications. The patients were divided into 2 groups—those with infected wounds and those without wound infection.
X-rays, computerized tomography (CT) scan, and 3-dimensional reconstruction were used to determine the type of fracture. Several classifications are used for calcaneal fractures. The Sanders classification system[16] is popular, so we used it to classified the bone injury. In brief, type I fractures are nondisplaced fractures (displacement <2 mm), type II/III fractures consist of a single or 2 intra-articular fractures that divide the calcaneus into 2/3 pieces, and type IV fractures consist of fractures with more than 3 intra-articular fractures. Type I fractures were nondisplaced fractures and were treated conservatively, and thus excluded. Based on our experiences and the literature, superficial infection was defined as a wound with erythema and/or discharge, but did not need surgical treatment. We defined deep infection as a wound requiring surgical intervention including debridement, fixator removal, or flap repair, and prolonged antibiotic use was also necessary.
Patients who were considered not suitable for immediate surgery had the injured foot elevated, toe activation was encouraged to reduce swelling, and the ankle joint was fixed by a short plaster until the “wrinkle sign” was positive. Patients were in a lateral position, and a tourniquet bound the thigh root to decrease bleeding All surgical procedures were performed observing the general rules of sterility.
An “L” shaped extensile lateral approach was used, exposing the periosteum of the lateral calcaneus. Full-thickness soft tissue flaps were raised, retraction of flaps was avoided to protect the soft tissue, without drying the flaps, and the flaps were covered with gauze. Kirschner wires were drilled into the talus to retract the flaps and tendons. Kirschner wires were also used to fix the articular surface after the smoothness and anatomy was restored. Stabilization was achieved with an appropriate size plate and screws. The use of a bone graft was judged by the operating surgeon, either an autograft or allograft. The incision was washed with sterile saline, a 2-layered closure was performed, and the skin was closed.
Before the initial fracture surgical procedure, routine prophylactic intravenous antibiotics were used. Additional doses of antibiotics were used if the operative time exceeded 3 hours. The choice of antibiotic treatment was according to local microbiological guidelines. Short-leg plaster fixation was also used for 3 weeks, and full weightbearing was avoided until 12 weeks after the operation.
SPSS Statistics for Windows, Version 12.0 (SPSS Inc., Chicago, IL) was used for the statistical analysis. We used the mean and standard deviation (SD) to demonstrate continuous and discrete variables. We also used the number of patients to present categorical variables, and they were analyzed using the Fisher exact test. Binary logistic regression analysis was used to determine the risk variables. A 2-sided significance level of 0.05 was used for all statistical tests.
3. Results
3.1. General data
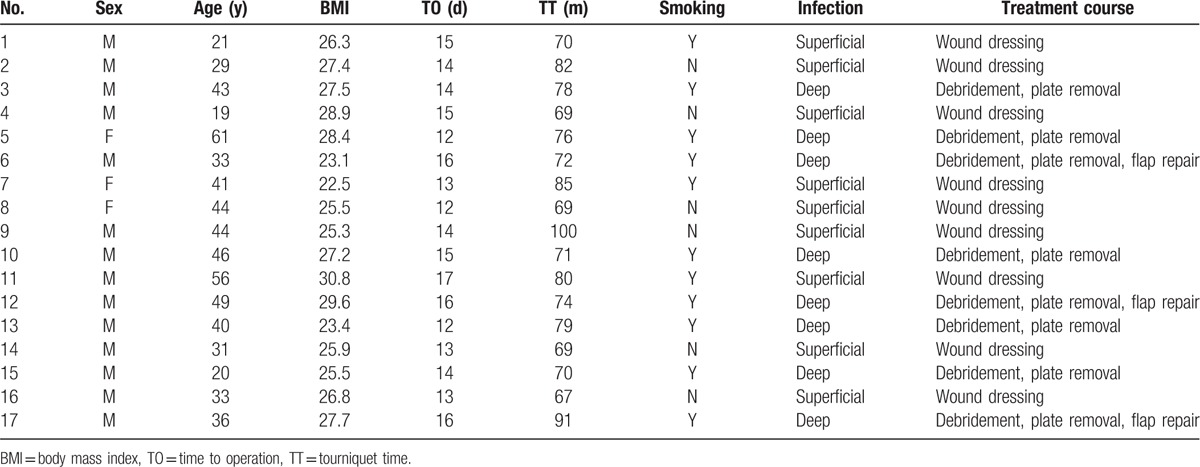
In all, 299 patients with 318 calcaneal fractures who met the entry criteria were treated from January 2006 to June 2014. They were 267 males and 32 females with a mean age of 38.6 years (range 16–62 years). Nineteen patients had bilateral calcaneal fractures and 280 patients had unilateral calcaneal fractures including 161 left calcaneal fractures and 119 right calcaneal fractures. Falling was the main cause of injury, accounting for 77% of the total cases (n = 244). Among them, 69% (n = 221) suffered only calcaneal fractures without other injured organs; 58 cases and 35 cases were associated with 1 or 2 injured organs respectively; and only 4 cases suffered more than 3 injured organs. According to imaging data, Sanders II and Sanders III type calcaneal fractures accounted for 40% (n = 126) and 44% (n = 139), respectively. Among the patients, 36% (n = 114) were active smokers at admission. Thirty-two patients were diagnosed with diabetes before being injured. Finally, 5.3% (n = 17) of patients were diagnosed with wound infection, and 2.8% (n = 9) of patients with superficial wound infections were treated by wound dressing until the wound healed. Also, 2.5% (n = 8) of patients were diagnosed as deep wound infections, and all of them were treated with plate removal. Five patients underwent multiple debridement and wound dressing, and flap repair was performed on 3 patients to achieve wound healing. The details of patients with wound infections are listed in Table 1.
Table 1.
Details of patients with wound infection.
3.2. Patient-related factors
The univariate analysis of cases is listed in Table 2 and Table 3. The data showed that there was no significant difference with patient-related factors such as age (P = .789) and sex (P = .127) between the 2 groups. The presence of diabetes was higher in the wound infection group, but it did not reach statistical significance (P = .395). The BMI was different between the 2 groups, and patients who had wound infections had a higher mean BMI (P < .001). The data also revealed that the incidence of active smokers was higher in the wound infection group than the group without wound infection, and there was a significant difference between the 2 groups (P < .001).
Table 2.
Univariate analysis for numerical variables.
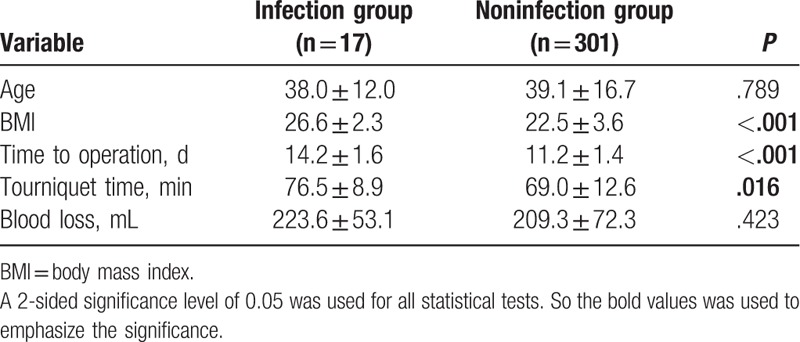
Table 3.
Univariate analysis for categorical variables.
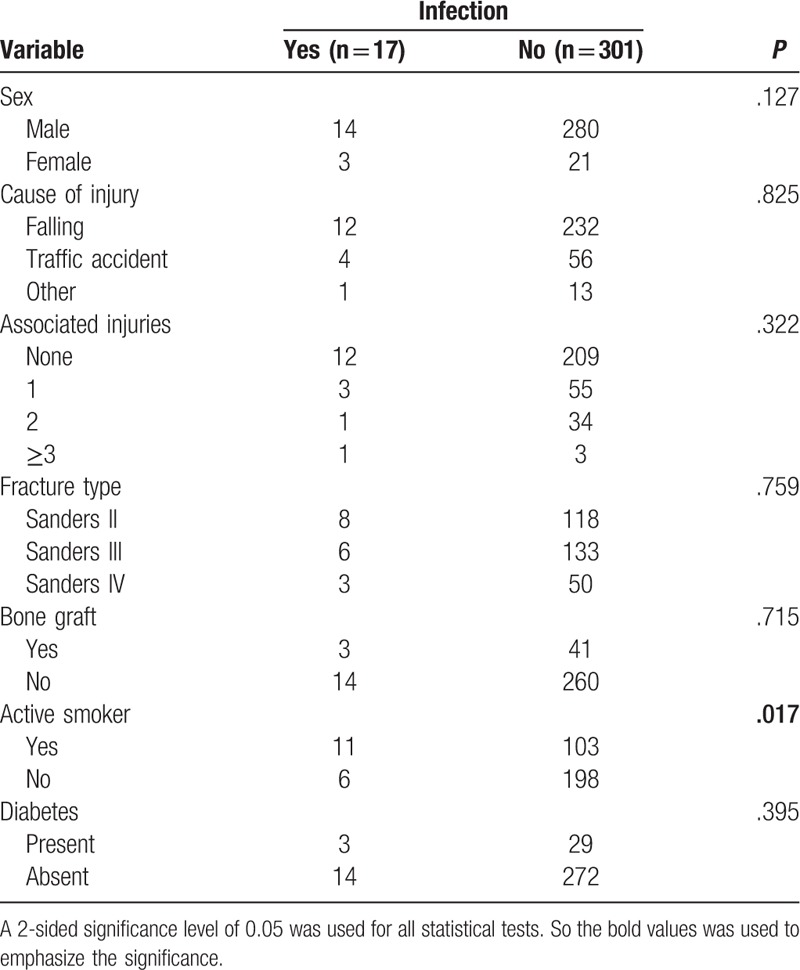
3.3. Injury-related factors
The main cause of injury in the 2 groups was falling, the second cause was a traffic accident, and there was no significant difference between the 2 groups (P = .825). The proportion of Sanders II fractures was the largest in the wound infection group. However, the proportion of Sanders III fractures was the largest in the group without wound infection, and there was no significant difference between the 2 groups (P = .759). Most cases had only calcaneal fractures without any organ injuries (70% in the wound infection group and 69% in the group without wound infection), and there was no different difference between the 2 groups (P = .322).
3.4. Surgery-related factors
All patients were treated with open reduction and internal fixation by a single surgeon. Surgery-related factors were also analyzed to determine their effect on wound infections. Time from injury to operation was 14.2 ± 1.6 days in the wound infection group, it was significantly longer compared with the group without wound infection (11.2 ± 1.4 days), and there was significant difference (P < .001). Therefore, the delay of the operation can increase the rate of wound infection. The mean tourniquet time in the wound infection group and the group without wound infection was 76.5 ± 8.9 minutes and 69.0 ± 12.6 minutes, respectively, and the difference was significant between the 2 groups (P = .016). Blood loss in the infection group was 223.6 ± 53.1 mL, and although it was more than in the group without wound infection, there was no significant difference (P = .423). Moreover, 18% patients (n = 3) in the infection group and 14% patients (n = 41) in the group without wound infection were treated with bone grafting, and there was also no significant difference (P = .715).
3.5. Multivariable analysis
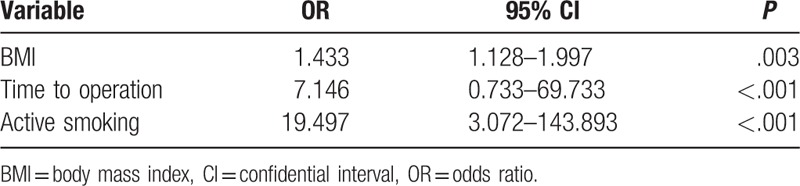
The univariate analysis showed that a higher BMI, longer time from injury to operation, longer tourniquet time, and active smoking were associated with wound infection after open reduction and internal fixation. Multivariable analysis was performed using these covariates (Table 4). Multivariable logistic regression analysis showed that BMI (odds ratio [OR] 1.433, P = .003), time to operation (OR 7.146, P < .001), and active smoking (OR 19.497, P < .001) were the independent risk factors.
Table 4.
Multivariate analysis for variable test.
4. Discussion
With the development of surgical techniques and a deeper understanding of calcaneal fractures, more and more patients who suffer calcaneal fractures are treated by open reduction and internal fixation. Accordingly, the number of patients with wound complications is also increasing. It was reported that the incidence rate of wound infections is from 5% to 25%.[7–11] For patients who are diagnosed with superficial infections, a good outcome can be achieved after active treatment. However, it is devastating to patients who are diagnosed with deep infections, even though there is low morbility. Many studies have been done to identify factors associated with the risk of wound infections. Based on the literature, it is thought to be a multifactorial problem including increasing age, active smoking, time to surgery, diabetes, and complex fractures.[12–15,17–19] However, there were several limitations in previous studies, such as not a single surgeon or the number of patients was small. Therefore, to obtain a reliable result, we designed a retrospective study including 318 patients who were treated by a single surgeon from January 2006 to June 2014.
Appropriate surgical timing is very important to calcaneal fractures. However, there is still a controversy about when is the most suitable surgical time. Many surgeons performed surgery after detumescence of the injured foot and suggested that it is critical to avoid soft tissue complications.[20,21] Al-Mudhaffar et al[21] did a retrospective study and indicated that more patients with wound complications underwent operation within 7 days after the injury. Others, however, hold the opposite view.[15,22,23] Koski et al[15] did a retrospective analysis of 126 consecutive patients with 148 fractures and concluded that a longer delay in surgery was a positive risk factor for wound complications. Abidi et al[22] also reported that the incidence of infection rose if the surgery was performed more than 5 days after injury. Additionally, Ho et al[19] divided patients into 3 groups based on the timing of surgery, and concluded that time to surgery did not affect postoperative infection rates. In our study, the average time to surgery in the infection group (14.2 days) was longer than in the group without wound infection (11.2 days). Generally, calcaneal fractures are caused by high-energy impacts, and the relatively thin coverage of soft tissue on the heel also suffers severe injury. If early surgery is performed, the soft tissue again suffers trauma, which is bad for wound healing and may increase the incidence rate of wound infections. In our experience, we would rather perform surgery when the patient has a positive “wrinkle test”. We also suggest that surgery be performed within 14 days after injury based on our results.
A few scholars suggested that active smoking is not significantly associated with wound complications.[12,15,23] In contrast, more studies have confirmed that active smoking is not conducive to wound healing. Assous and Bhamra[24] reported that 70% of patients were active smokers in their infection group and 15% patients were smokers in their noninfection group. Soni et al[17] reviewed 81 patients and concluded that all the patients who developed deep infections were smokers. Our data revealed similar results, that the patients who developed deep infections were smokers. Univariate analysis showed that active smoking was associated with wound infection after open reduction and internal fixation, and multivariable logistic regression analysis showed that active smoking was an independent risk factor. Therefore, we suggest that active smoking is a risk factor of wound infection. Cigarettes contain a lot of harmful substances, such as nicotine, and produce carbon monoxide, which can cause vasospasms and lead to wound complications. Abidi et al[22] indicated that cessation of smoking for 5 days before the operation can decrease the rate of wound infection. However, this suggestion was only experience from surgeons and lacked systematic analysis. In our study, we did not investigate the relationship between cessation of smoking and wound infections.
In our study, we found that a higher BMI was a risk factor of wound infection and was an independent risk factor. This view was also pointed out in the literature.[22] The main cause of calcaneal injury was falling from heights. Patients with a higher BMI means higher energy was exerted on the calcaneus, which could cause complex fractures. This implies that soft tissue around the calcaneus also suffers from the higher energy. The condition of soft tissue is an important factor that impacts wound healing, and therefore, a higher BMI is negative to wound healing. In this study, 13 patients were overweight, the highest BMI was 30.8, and there was a significant difference between the 2 groups.
Al-Mudhaffar et al[21] retrospectively reviewed 33 calcaneal fracture patients who were treated with open reduction and internal fixation, and identified that a tourniquet time in excess of 1.5 hours is a risk factor for postoperative wound complications. We also found that tourniquet time was longer in the infection group than in the noninfection group. In univariate analysis, tourniquet time was positively associated with wound infections, whereas after adjustment for potential risk factors, tourniquet time no longer showed a significant association with wound infection.
Folk et al[13] reported that diabetes can increase the incidence rate of wound infections after open reduction and internal fixation. However, there were no significant correlations between diabetes and wound infections in the current study. In our experience, good perioperative management can significantly reduce the impact of diabetes on wounds. Complex fracture patterns were also thought to cause wound infections.[17,19] However, with the use CT, we can clearly recognize the details of fractures and develop a reasonable surgical plan to reduce unnecessary damage of the soft tissue. We did not find a correlation between complex fracture pattern and wound infection. We paid more attention to soft tissue conditions, applied a more reasonable surgical approach, and thus we found that there was no correlation between wound infection and surgical approach[21,22] or stitching method.[22] Zhang et al collected 10 observational studies involving 1559 patients with 1651 fractures and did a meta-analysis. The results revealed that a bone graft was a risk factor for wound infections.[25] However, based on our results, there was no significant difference between the infection group and the noninfection group. This was possibly because few bone grafts were performed, but a larger sample is needed to confirm this. It is worth mentioning that several scholars thought low surgical experience can increase wound infection.[12,26] To get an accurate result, we selected only 1 surgeon who did all the operations.
There are several limitations to our study. First, the sample size is small even though it is larger than most previous studies. There are only 17 infected patients admitted in the study. Second, the present study was not prospective but retrospective.
5. Conclusions
Open reduction and internal fixation is accepted by most surgeons, but wound infection is a problem, even though the surgical technology has quickly developed in the past 2 decades. Based on our results, we found that patients who had a higher BMI and were smokers had a high risk of wound infections. We suggest that surgeons do not operate until the swelling of the injured foot has improved, and we also suggest that the operation should be done within 14 days of the injury.
Footnotes
Abbreviations: BMI = body mass index, CT = computerized tomography, OR = odds ratio odds ratio, SD = standard deviation.
All authors declare that they have no conflicts of interest concerning this article.
References
- [1].Lindsay WR, Dewar FP. Fractures of the os calcis. Am J Surg 1958;95:555–76. [DOI] [PubMed] [Google Scholar]
- [2].Jarvholm U, Korner L, Thoren O, et al. Fractures of the calcaneus. A comparison of open and closed treatment. Acta Orthop Scand 1984;55:652–6. [DOI] [PubMed] [Google Scholar]
- [3].Agren PH, Wretenberg P, Sayed-Noor AS. Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am 2013;95:1351–7. [DOI] [PubMed] [Google Scholar]
- [4].Zwipp H, Rammelt S, Barthel S. Calcaneal fractures: open reduction and internal fixation (ORIF). Injury 2004;35(suppl 2):SB46–54. [DOI] [PubMed] [Google Scholar]
- [5].Buckley R, Tough S, McCormack R, et al. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am 2002;84-A:1733–44. [DOI] [PubMed] [Google Scholar]
- [6].Randle JA, Kreder HJ, Stephen D, et al. Should calcaneal fractures be treated surgically? A meta-analysis. Clin Orthop Relat Res 2000;377:217–27. [DOI] [PubMed] [Google Scholar]
- [7].Palarcik J, Bucek P, Vopelka J. [Surgical treatment of (selected) calcaneal fractures]. Rozhl Chir 1997;76:231–8. [PubMed] [Google Scholar]
- [8].Chan S, Ip FK. Open reduction and internal fixation for displaced intra-articular fractures of the os calcis. Injury 1995;26:111–5. [DOI] [PubMed] [Google Scholar]
- [9].Zwipp H, Tscherne H, Thermann H, et al. Osteosynthesis of displaced intraarticular fractures of the calcaneus. Results in 123 cases. Clin Orthop Relat Res 1993;290:76–86. [PubMed] [Google Scholar]
- [10].Bezes H, Massart P, Fourquet JP. [Osteosynthesis of calcaneus impression fractures. Indication, technic and results in 120 cases]. Unfallheilkunde 1984;87:363–8. [PubMed] [Google Scholar]
- [11].Stromsoe K, Mork E, Hem ES. Open reduction and internal fixation in 46 displaced intraarticular calcaneal fractures. Injury 1998;29:313–6. [PubMed] [Google Scholar]
- [12].Court-Brown CM, Schmied M, Schutte BG. Factors affecting infection after calcaneal fracture fixation. Injury 2009;40:1313–5. [DOI] [PubMed] [Google Scholar]
- [13].Folk JW, Starr AJ, Early JS. Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma 1999;13:369–72. [DOI] [PubMed] [Google Scholar]
- [14].Dickens JF, Kilcoyne KG, Kluk MW, et al. Risk factors for infection and amputation following open, combat-related calcaneal fractures. J Bone Joint Surg Am 2013;95:e24. [DOI] [PubMed] [Google Scholar]
- [15].Koski A, Kuokkanen H, Tukiainen E. Postoperative wound complications after internal fixation of closed calcaneal fractures: a retrospective analysis of 126 consecutive patients with 148 fractures. Scand J Surg 2005;94:243–5. [DOI] [PubMed] [Google Scholar]
- [16].Sanders R, Fortin P, DiPasquale T, et al. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res 1993;290:87–95. [PubMed] [Google Scholar]
- [17].Soni A, Vollans S, Malhotra K, et al. Association between smoking and wound infection rates following calcaneal fracture fixation. Foot Ankle Spec 2014;7:266–70. [DOI] [PubMed] [Google Scholar]
- [18].Benirschke SK, Kramer PA. Wound healing complications in closed and open calcaneal fractures. J Orthop Trauma 2004;18:1–6. [DOI] [PubMed] [Google Scholar]
- [19].Ho CJ, Huang HT, Chen CH, et al. Open reduction and internal fixation of acute intra-articular displaced calcaneal fractures: a retrospective analysis of surgical timing and infection rates. Injury 2013;44:1007–10. [DOI] [PubMed] [Google Scholar]
- [20].Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am 2000;82:225–50. [DOI] [PubMed] [Google Scholar]
- [21].Al-Mudhaffar M, Prasad CV, Mofidi A. Wound complications following operative fixation of calcaneal fractures. Injury 2000;31:461–4. [DOI] [PubMed] [Google Scholar]
- [22].Abidi NA, Dhawan S, Gruen GS, et al. Wound-healing risk factors after open reduction and internal fixation of calcaneal fractures. Foot Ankle Int 1998;19:856–61. [DOI] [PubMed] [Google Scholar]
- [23].Tennent TD, Calder PR, Salisbury RD, et al. The operative management of displaced intra-articular fractures of the calcaneum: a two-centre study using a defined protocol. Injury 2001;32:491–6. [DOI] [PubMed] [Google Scholar]
- [24].Assous M, Bhamra MS. Should Os calcis fractures in smokers be fixed? A review of 40 patients. Injury 2001;32:631–2. [DOI] [PubMed] [Google Scholar]
- [25].Zhang W, Chen E, Xue D, et al. Risk factors for wound complications of closed calcaneal fractures after surgery: a systematic review and meta-analysis. Scand J Trauma Resusc Emerg Med 2015;23:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Poeze M, Verbruggen JP, Brink PR. The relationship between the outcome of operatively treated calcaneal fractures and institutional fracture load. A systematic review of the literature. J Bone Joint Surg Am 2008;90:1013–21. [DOI] [PubMed] [Google Scholar]


