Supplemental Digital Content is available in the text
Keywords: burden of disease, healthcare cost, incidence, pneumonia
Abstract
Pneumonia is a leading cause of hospitalization and mortality worldwide. Despite recognition of the importance of community-acquired pneumonia (CAP) in adults, limited epidemiologic information is available in South Korea. This study aimed to evaluate the disease burden of hospitalized CAP in adults aged ≥19 years and its epidemiologic trend using Health Insurance and Review Assessment (HIRA) data.
This is a retrospective study using the HIRA database from year 2009 to 2013. We estimated the incidence rate and direct medical cost of hospitalized CAP in adults aged ≥19 years in South Korea. These were further analyzed with respect to age and underlying medical conditions.
During 2009 to 2013, 1216,916 hospitalizations were recorded. On average, the annual age-adjusted incidence rate of hospitalized CAP was 626 per 100,000 persons, with the rate increasing with age. When stratified by age- and risk groups, elderly people ≥75 years showed the highest incidence rate of hospitalized CAP over 5-year study periods. With respect to the risk groups based on underlying medical conditions, incidence rate ratios were 2.04 to 5.86 for the high-risk group versus the low-risk group and 1.28 to 5.49 for the moderate-risk group versus the low-risk group. Overall, mean direct medical cost for hospitalized CAP was 1851 USD per capita during the 5-year period: 1263 USD in the low-risk group, 2353 USD in the moderate-risk group, and 2841 USD in the high-risk group.
This study shows that the incidence and medical cost of hospitalized CAP were consistently high over the 5-year study period. In particular, elderly people and adults with underlying medical conditions were at increased risk for hospitalized CAP.
1. Introduction
The annual incidence of community-acquired pneumonia (CAP) is approximately 516 to 611 cases per 100,000 persons in adults, and the rate increases with age.[1] In the United States, approximately 5.6 million cases of CAP are reported annually.[2] Among them, 2% to 24% require admission to an intensive care unit (ICU), and 2% to 3% lead to death.[2,3] Similarly, in South Korea, pneumonia is one of the leading causes of death in the most recent 10 years, ranking at 12th in 2003 and jumping to 4th in 2015; it also shows increasing fatality with age.[4]
Influenza and pneumococcal vaccines are widely used to prevent lower respiratory tract infections, and these are included in the national immunization programs of many Western countries.[5] However, there are several kinds of influenza vaccines (unadjuvanted, adjuvanted, and high-dose) and pneumococcal vaccines (13-valent protein conjugate and 23-valent polysaccharide) with different formulations, cost, and efficacy. Each country decides a vaccination strategy considering cost-effectiveness based on local epidemiologic data.
Despite recognition of the importance of CAP in adults, limited epidemiologic information is available in South Korea. Disease burden can be estimated with either a cohort study or a “big data” study using a national health insurance database. In the case of South Korea, a cohort study is difficult to implement because of easy accessibility to distant hospitals outside of the cohort area; however, medical information is limited in these cases. On the other hand, the health insurance database is useful in evaluating disease burden, as it provides complete records of all hospitalizations. Another advantage of this database is the standardized diagnosis code lists that enable secular trend analysis of infectious diseases for a given population. In South Korea, the Health Insurance and Review Assessment (HIRA) data are health insurance claims data that have been publicly available for research since 2009.[6] The HIRA database includes both health insurance (98%) and medical aid (2%), which covers all healthcare providers and citizens in South Korea. Thus, HIRA data may give a reasonable approximation to the burden of hospitalized CAP.
In this study, we investigated the burden of hospitalized CAP and its epidemiologic trends using the HIRA database. The data were further analyzed with respect to age and underlying comorbidities. The results will be useful in developing improved public health policies for prevention and treatment of pneumonia.
2. Methods
2.1. Study design
During study the period between January 2009 and December 2013, we estimated the incidence rate and direct medical cost of hospitalized CAP in adults aged ≥19 years in South Korea using the HIRA database. These data were further analyzed with respect to age and underlying medical conditions. Study subjects were stratified based on their age (19–49, 50–64, 65–74, and ≥75 ys) and risk profile (low-, moderate-, and high-risk groups). This study protocol was exempted for review by the Institutional Review Board of the Korea University Guro Hospital according to the exemption criteria.
2.2. Data source
The HIRA database includes demographic information, diagnostic codes (International Classification of Diseases, 10th Revision, ICD-10 codes), dates of admission and discharge, drug prescription, and treatment fees through computerized management.[7] ICD-9 codes were used in the case of procedure codes (organ transplantation), and Korea Drug (KD) codes were used to find immunosuppressant users. The data used for analysis were provided by the HIRA service, which processed the data to encrypt any personal identifiers.
Hospitalized CAP cases were identified using primary or secondary diagnostic codes (ICD-10 diagnostic codes), which include J10.0, J11.0, J12.0, J12.1, J12.2, J12.3, J12.8, J12.9, J13, J14, J15.0, J15.1, J15.2, J15.3, J15.4, J15.6, J15.7, J15.8, J15.9, J16.0, J16.8, J17.0, J17.1, J17.8, J18.0, J18.1, J18.2, J18.8, and J18.9 (Supplementary Table 1). Multiple episodes of CAP in a single study year were included as independent cases only if they were separated by ≥180 days. Based on the diagnostic codes, underlying medical conditions were classified as high-, moderate-, and low-risk (Supplementary Table 1). The high-risk group was defined as immunocompromised patients including asplenia (D73.0), hematologic malignancy (C81–96, D46, D55–64), solid cancer (C00–80, C97), human immunodeficiency virus (HIV)-related diseases (B20–24), chronic kidney diseases (N18, N19, I12.0, I13.2), solid organ transplantation (55.61, 55.69, 50.51, 50.59, 33.50, 33.51, 33.52, 37.5, 52.80, 52.81, 52.82, 52.83, 52.84, 52.85, 52.86), and immunosuppressant use (KD codes for etanercept, infliximab, adalimumab, and rituximab). The moderate-risk group was defined as immunocompetent subjects with following comorbidities: diabetes (E10-E14, E15–16), chronic lung diseases (J41, J42, J43, J44, J45, J47, J60–65, J84), chronic liver diseases (B18, K70.3, K71.7, K73, K74), or chronic heart diseases (I21–25, I34–37, I42–43, I50). Other immunocompetent subjects were classified into the low-risk group.
2.3. Study measures
In South Korea, the government conducts a population and housing census every 5 years. The government census office performs population projection based on births, deaths, and immigration using cohort component methods (www.nso.go.kr). In this study, population and housing census data from 2010 were used for calculating the incidence of hospitalized CAP. In each year from 2009 through 2013, population and age/risk distribution were extrapolated from annual population projection and HIRA data based on the population and housing census data of 2010. Using these specific populations as denominators, the annual and age group-specific incidence rates of hospitalized CAP were calculated. During 5-year periods, average incidence of hospitalized CAP was estimated using 5-year pooled data, and further analyzed according to age/risk groups (Supplementary Table 2). National Health Insurance (NHI)-covered medical costs were estimated per capita in the same manner.
2.4. Statistical analysis
Data were analyzed using SAS version 9.4 (SAS Institute Inc., Cary, NC). Incidence rates of hospitalized CAP cases were estimated by age and risk groups, and they were expressed per 100,000 persons. In each study year, age-adjusted incidence rate was also calculated using the distribution of Korean adult population (Supplementary Table 2). Age-specific incidence was multiplied by the proportion of each age group in the adult population. These age-specific results were summed to get the age-adjusted incidence rates. Rate ratios for pneumonia incidence were estimated in moderate- and high-risk groups versus the age-matched low-risk group using Poisson regression.
3. Results
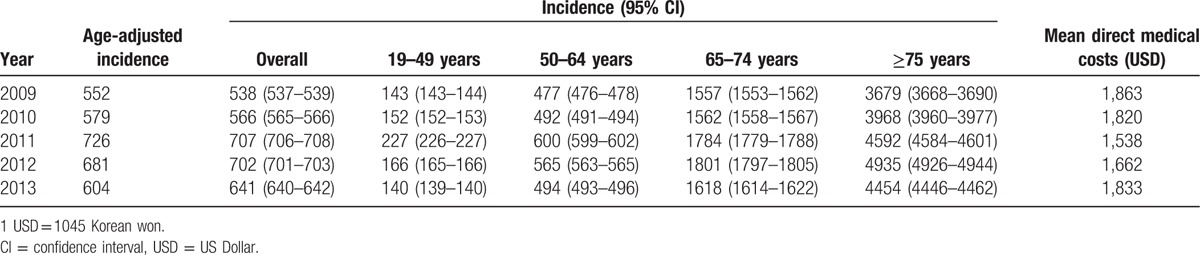
From 2009 to 2013, 1,216,916 hospitalized CAP cases were recorded. The average annual incidence rate of hospitalized CAP was 631 cases per 100,000 persons (age-adjusted rate, 626 cases per 100,000 persons), and this rate increased with age (Table 1). In each year during the study period, the estimated annual incidence rates and mean direct medical costs for hospitalized CAP were 538 to 707 cases per 100,000 persons (age-adjusted rates, 552–726 cases per 100,000 persons) and 1538 to 1863 USD per capita, respectively (Table 1). The incidence of hospitalized CAP was higher in 2011 and 2012 compared with other years, particularly in adults aged 19 to 64 years.
Table 1.
Estimated annual incidence (per 100,000 persons) and direct medical costs (USD) of community-acquired pneumonia.
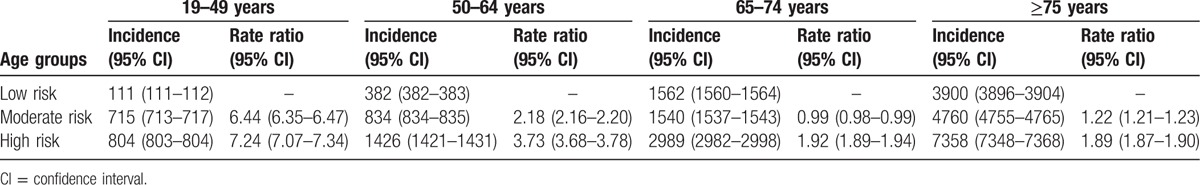
When stratified by age and risk groups, the elderly people aged ≥75 years showed the highest incidence rate of hospitalized CAP over 5-year study periods (Table 2). As for the underlying medical conditions, the incidence rates of hospitalized CAP were remarkably higher in moderate- or high-risk groups compared with the low-risk group (rate ratios in moderate- and high-risk groups: 6.44 and 7.24 in 19 to 49 years, 2.18 and 3.73 in 50 to 64 years, 0.99 and 1.91 in 65 to 74 years, and 1.22 and 1.89 in ≥75 years) (Table 2).
Table 2.
Estimated annual incidences (per 100,000 persons) of hospitalized community-acquired pneumonia and rate ratios based on age and risk in the years 2009 to 2013.
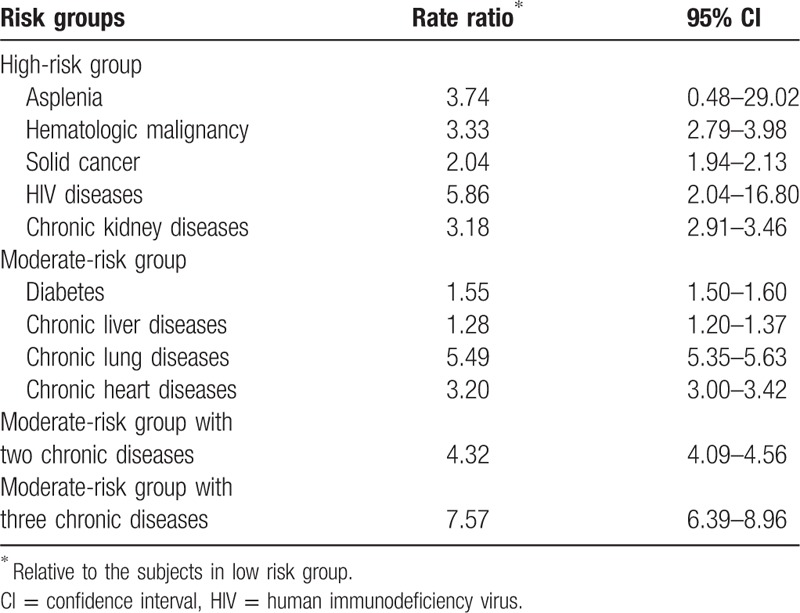
When the pooled population was analyzed irrespective of age, the incidence rate ratios for the high-risk group were 2.04 to 5.86 (vs the low-risk group) depending on the underlying medical conditions (Table 3). In the case of the moderate-risk group, the incidence rate ratios (vs low-risk group) ranged from 1.28 to 5.49 and increased with the number of chronic medical conditions.
Table 3.
Risk assessment of hospitalized community-acquired pneumonia according to underlying medical conditions.
Overall, the mean direct medical cost for hospitalized CAP was 1851 USD per capita during 5-year periods: 1263 USD in the low-risk group, 2353 USD in the moderate-risk group, and 2841 USD in the high-risk group. The medical cost tended to increase with increasing age and was particularly high in the high-risk group irrespective of age (Fig. 1).
Figure 1.
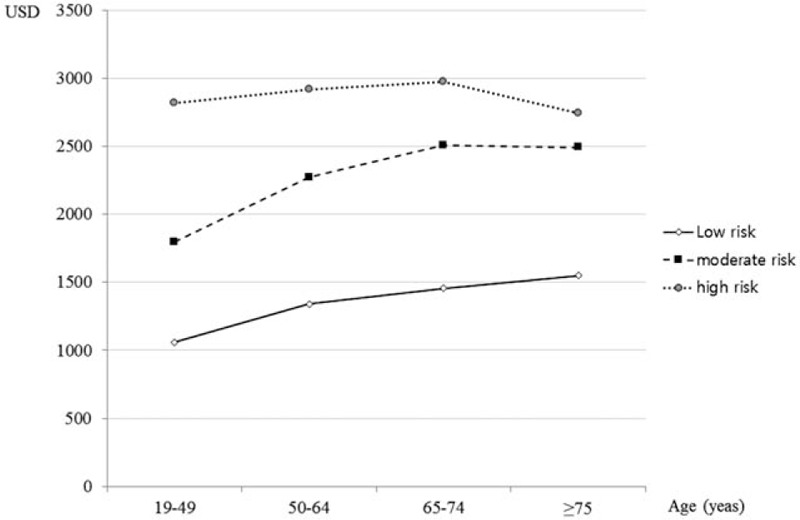
Age- and risk-specific direct medical cost (per-capita).
4. Discussion
In this study, we estimated nationwide incidence rate and direct medical cost per capita of hospitalized CAP over a 5-year period. The average annual rate of hospitalized CAP was 631 cases per 100,000 persons, similar to previous reports.[1,8] Although reported variably according to the study design, periods and areas, the incidence rates of CAP were particularly high in the elderly aged 65 years and older, ranging from 1000 to 2500 cases per 100,000 persons.[1,8–12] Similarly in this study, the incidence rates were estimated to be 1500 to 1800 cases per 100,000 persons in the elderly aged 65 to 74 years, and 3500 to 5000 cases per 100,000 persons among those aged ≥75 years (Table 1). Considering significantly high disease burden in the elderly, Korean government have subsidized influenza and pneumococcal vaccines for the old adults aged ≥65 years since 1997 and 2013 years, respectively.[13,14] As for the pneumococcal national immunization program (NIP), free 23-valent pneumococcal polysaccharide vaccine (PPV23) vaccine has been provided for all people aged ≥65 years with a target coverage of 60%.[13] As of 2016, the coverage rates of influenza vaccine and PPV23 were estimated to be about 80% and 60%, respectively.[13,15]
On the other hand, the incidence rate and direct medical cost showed annual variation with an inverse correlation. During 2011 to 2012, incidence rates were rather high compared with other study periods (702–707 cases/100,000 people vs 538–641 cases/100,000 persons) (Table 1). This difference might be related to the epidemic of Mycoplasma pneumoniae pneumonia among Korean adults around 2011.[16]M. pneumoniae pneumonia epidemics are reported to occur every 3 to 7 years.[17,18] During the 2011 epidemic of M. pneumoniae pneumonia, large number of young adults were affected; 58.6% of adults belonged to the 26 to 40 years.[16] The patients were hospitalized for short periods (mean, 7.3 days) compared with previous reports in South Korea (mean, 9–10 d).[16,19,20] This epidemic pattern (young adult patients with short-term hospitalization) around 2011 might explain the relatively lower direct medical costs around this time compared with the average annual estimate (1851 USD per capita). The average direct medical cost per capita was comparable with the previous report by multicenter hospital-based study in South Korea (1862 USD per capita).[20]
Although this study did not include outpatient CAP cases, 97.7% to 100% of patients with CAP were reported to receive inpatient care in South Korea because of several unique characteristics of this healthcare system (easy accessibility and high coverage level of NHI), the propensity of doctors and patients, and business-related factors.[19,21–23] Thus, the results of this study may reflect the real disease burden of CAP in South Korea; 1% to 2% of mild outpatient CAP cases might not be included, but overestimation of direct medical costs would not be remarkable.
When stratified by age/risk groups, the overall incidence rate of hospitalized CAP was remarkably higher in moderate- and high-risk groups compared with the low-risk group. However, such differences were blunted with increasing age. Particularly, in older adults aged ≥65 years, there was no remarkable difference between low and moderate risk groups (incidence rate ratio, 0.99 in adults aged 65 to 74 years and 1.22 in adults aged ≥75 years) (Table 2). These findings might mean that older adults aged ≥65 years become susceptible to pneumonia irrespective of underlying medical conditions because of aging immunity and unrecognized comorbidities, among other reasons. Consistent with previous studies, the incidence of CAP increased markedly with increasing age in all 3 risk groups irrespective of underlying medical conditions.[24,25] With respect to underlying medical conditions, the moderate-risk group with 2 to 3 chronic medical conditions are at an even higher risk for pneumonia than the high-risk group, consistent with a previous report.[24]
There are some limitations in this study. First, the HIRA data were secondary data based on diagnostic codes used for insurance claims, so uninsured costs were not considered. Second, this study did not include outpatient CAP cases. Because diagnostic codes of outpatients were known to be incorrect, we decided to just include hospitalized CAP cases. Third, the proportion of high-risk group might be lower in this study compared with the real practice (Supplementary Table 2). We did not include all kinds of immunosuppressant use considering diverse degree of immunosuppression. Finally, we could not estimate the case-fatality rate of CAP. Because the HIRA database does not have a death-specific code, data on mortality were not available.
In conclusion, the incidence and medical cost of hospitalized CAP were consistently high over the last 5 years. In particular, elderly people and adults with underlying medical conditions were at increased risk for hospitalized CAP. This study emphasized the importance of an age- and risk-based influenza and pneumococcal vaccination strategy. It is warranted to evaluate the impacts of current vaccination strategies whether these might decrease pneumonia disease burden or not.
Supplementary Material
Footnotes
Abbreviations: CAP = community-acquired pneumonia, HIRA = Health Insurance and Review Assessment, ICU = intensive care unit, ICD = International Classification of Diseases, KD = Korea Drug, HIV = human immunodeficiency virus, PPV23 = 23-valent pneumococcal polysaccharide vaccine, NIP = National Immunization Program.
This work was supported by the National Research Foundation of Korea (NRF) Grant funded by the Korean Government (MSIP) (NRF-2016R1A5A1010148).
The authors declare no conflicts of interest.
Supplemental Digital Content is available for this article.
References
- [1].Marrie TJ, Huang JQ. Epidemiology of community-acquired pneumonia in Edmonton, Alberta: an emergency department-based study. Can Respir J 2005;12:139–42. [DOI] [PubMed] [Google Scholar]
- [2].Mandell LA. Epidemiology and etiology of community-acquired pneumonia. Infect Dis Clin North Am 2004;18: 761-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Phua J, Dean NC, Guo Q, et al. Severe community-acquired pneumonia: timely management measures in the first 24 hours. Crit Care 2016;20:237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Statistics Korea. Mortality statistics. Available at: http://www.index.go.kr/potal/main/EachDtlPageDetail.do?idx_cd=1012. Accessed May 17, 2017. [Google Scholar]
- [5].Castiglia P. Recommendations for pneumococcal immunization outside routine childhood immunization programs in Western Europe. Adv Ther 2014;31:1011–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kim JA, Yoon S, Kim LY, et al. Towards actualizing the value potential of Korea Health Insurance Review and Assessment (HIRA) data as a resource for health research: strengths, limitations, applications, and strategies for optimal use of HIRA data. J Korean Med Sci 2017;32:718–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Skull SA, Andrews RM, Byrnes GB, et al. ICD-10 codes are a valid tool for identification of pneumonia in hospitalized patients aged > or = 65 years. Epidemiol Infect 2008;136:232–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Ramirez JA, Wiemken TL, Peyrani P, et al. Adults hospitalized with pneumonia in the United States: incidence, epidemiology and mortality. Clin Infect Dis 2017;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- [9].Griffin MR, Zhu Y, Moore MR, et al. U.S. hospitalizations for pneumonia after a decade of pneumococcal vaccination. N Engl J Med 2013;369:155–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Jackson ML, Neuzil KM, Thompson WW, et al. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis 2004;39:1642–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Simonsen L, Taylor RJ, Schuck-Paim C, et al. Effect of 13-valent pneumococcal conjugate vaccine on admissions to hospital 2 years after its introduction in the USA: a time series analysis. Lancet Respir Med 2014;2:387–94. [DOI] [PubMed] [Google Scholar]
- [12].Thomas CP, Ryan M, Chapman JD, et al. Incidence and cost of pneumonia in medicare beneficiaries. Chest 2012;142:973–81. [DOI] [PubMed] [Google Scholar]
- [13].Heo JY, Seo YB, Choi WS, et al. Cost-effectiveness of pneumococcal vaccination strategies for the elderly in Korea. PLoS One 2017;12:e0177342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kee SY, Lee JS, Cheong HJ, et al. Influenza vaccine coverage rates and perceptions on vaccination in South Korea. J Infect 2007;55:273–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Korean Centers for Disease Control and Prevention. Guideline for influenza national immunization program in 2017–2018 season. Available at: https://nip.cdc.go.kr/irgd/index.html. Accessed on September 26 2017. [Google Scholar]
- [16].Seo YB, Yang TU, Kim IS, et al. Clinical and epidemiologic characteristics of Mycoplasma pneumoniae pneumonia in adults during 2011 epidemic. Infect Chemother 2012;44:367–71. [Google Scholar]
- [17].Atkinson TP, Balish MF, Waites KB. Epidemiology, clinical manifestations, pathogenesis and laboratory detection of Mycoplasma pneumoniae infections. FEMS Microbiol Rev 2008;32:956–73. [DOI] [PubMed] [Google Scholar]
- [18].Waites KB, Talkington DF. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev 2004;17:697–728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Chong YP, Jung K-S, Lee KH, et al. The bacterial etiology of community-acquired pneumonia in Korea: a nationwide prospective multicenter study. Infect Chemother 2010;42:397–403. [Google Scholar]
- [20].Yoo KH, Yoo CG, Kim SK, et al. Economic burden and epidemiology of pneumonia in Korean adults aged over 50 years. J Korean Med Sci 2013;28:888–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Choi MJ, Song JY, Cheong HJ, et al. Clinical usefulness of pneumococcal urinary antigen test, stratified by disease severity and serotypes. J Infect Chemother 2015;21:672–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kim HI, Kim SW, Chang HH, et al. Mortality of community-acquired pneumonia in Korea: assessed with the pneumonia severity index and the CURB-65 score. J Korean Med Sci 2013;28:1276–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Kim JE, Kim UJ, Kim HK, et al. Predictors of viral pneumonia in patients with community-acquired pneumonia. PLoS One 2014;9:e114710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Pelton SI, Shea KM, Farkouh RA, et al. Rates of pneumonia among children and adults with chronic medical conditions in Germany. BMC Infect Dis 2015;15:470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Shea KM, Edelsberg J, Weycker D, et al. Rates of pneumococcal disease in adults with chronic medical conditions. Open Forum Infect Dis 2014;1:ofu024. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


