Abstract
Early estimation of mortality risk in patients with trauma is essential. In this study, we evaluate the validity of the Emergency Trauma Score (EMTRAS) and Rapid Emergency Medicine Score (REMS) for predicting in-hospital mortality in patients with trauma. Furthermore, we compared the REMS and the EMTRAS with 2 other scoring systems: the Revised Trauma Score (RTS) and Injury Severity score (ISS).
We performed a retrospective chart review of 6905 patients with trauma reported between July 2011 and June 2016 at a large national university hospital in South Korea. We analyzed the associations between patient characteristics, treatment course, and injury severity scoring systems (ISS, RTS, EMTRAS, and REMS) with in-hospital mortality. Discriminating power was compared between scoring systems using the areas under the curve (AUC) of receiver operating characteristic (ROC) curves.
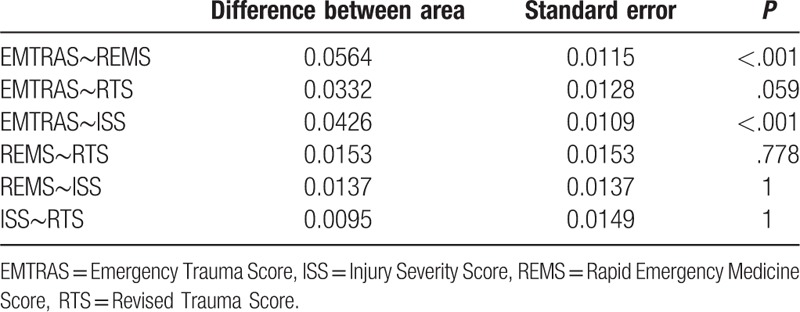
The overall in-hospital mortality rate was 3.1%. Higher EMTRAS and REMS scores were associated with hospital mortality (P < .001). The ROC curve demonstrated adequate discrimination (AUC = 0.957 for EMTRAS and 0.9 for REMS). After performing AUC analysis followed by Bonferroni correction for multiple comparisons, EMTRAS was significantly superior to REMS and ISS in predicting in-hospital mortality (P < .001), but not significantly different from the RTS (P = .057). The other scoring systems were not significantly different from each other.
The EMTRAS and the REMS are simple, accurate predictors of in-hospital mortality in patients with trauma.
Keywords: mortality, trauma severity indices, wound and injuries
1. Introduction
Trauma is defined as a physical injury from an external source. Despite improvements in trauma systems and the consequent reduction in preventable deaths, trauma is still the leading cause of death worldwide. Approximately 5.8 million people die each year due to trauma, representing 10% of the worldwide mortality.[1]
The severity of traumatic injuries plays an important role in the determination of mortality and morbidity in patients with trauma; thus, a proper understanding of the severity of trauma is crucial for improving trauma care. In recent decades, several scoring systems have been developed to assess injury severity among patients with trauma and to provide an objective measure of patients’ initial condition as part of treatment determination. However, there is no generally accepted standard scoring system for assessing trauma severity.[2]
The Revised Trauma Score (RTS) is one of the most common physiologic scoring systems in use; it can be administered early in treatment, even in the prehospital phase.[3] Although calculation of the RTS is complex, this system weakly correlates with mortality.[4]
The Injury Severity Score (ISS) is an anatomic scoring system that provides a score for patients with multiple injuries. It is the only anatomic scoring system currently in use, and these scores correlate with length of hospital stay, other measures of trauma severity, and morbidity and mortality.[5] However, an important limitation of the ISS is the difficulty associated with its early application, as a complete evaluation of all patient injuries may take substantial time following admission to the emergency room.[2,6]
The Acute Physiology and Chronic Health Evaluation (APACHE) II is a validated scale that assesses illness severity among nonsurgical, surgical, and intensive care patients.[7] However, with its reliance on laboratory tests, such as blood chemistry analyses, the use of the APACHE II remains impractical for the rapid assessment of injury severity required in the emergency department (ED) or in the field.[7,8]
New scoring systems are currently being developed to overcome the drawbacks of the systems mentioned above. One of these is the Rapid Emergency Medicine Score (REMS), a simplified version of the APACHE II that allows for rapid score calculation. The REMS is calculated based on the patient's Glasgow Coma Scale (GCS), respiratory rate (RR), oxygen saturation, mean arterial pressure (MAP), heart rate (HR), and age.[7] This score has been shown to be a valid predictor of mortality in non-surgical patients presenting to the ED.[8]
Another new trauma severity scoring system is the Emergency Trauma Score (EMTRAS), which was developed to provide an early assessment of mortality risk in adult patients with trauma. The score is calculated using 4 variables: age, GCS, base excess (BE), and prothrombin time (PT). The EMTRAS uses parameters that are available within 30 minutes of a patient presenting to the ED, does not require a knowledge of anatomic injuries, and accurately predicts mortality.[2]
Hence, the purpose of this study was to evaluate the EMTRAS and REMS as predictors of in-hospital mortality in patients with trauma.
2. Methods
2.1. Study population and data abstraction
The study included patients with trauma, aged 15 years or older, admitted to South Korea's Gyeongsang National University Hospital between July 2011 and June 2016. Patients who were dead upon arrival, discharged from the ED before termination of emergency treatment, <15 years of age, or who had burns or drowning-related injuries were excluded from the study. Patients with insufficient medical record data to calculate the EMTRAS, REMS, ISS, and RTS were also excluded. On the basis of these criteria, 6905 patients met the final inclusion criteria. Data abstracted from patient medical records included demographic characteristics, treatment course, injury trauma scoring systems (ISS, RTS, EMTRAS, and REMS), and in-hospital mortality.
2.2. Scoring calculations
The ISS is an anatomical scoring system for patients with multiple injuries. Each injury is assigned an abbreviated injury scale (AIS) score and is allocated to 1 of the following 6 body regions: head, face, chest, abdomen, extremities (including the pelvis), and external. The scores for the 3 most severely injured body regions are squared and then summed to obtain the ISS score, which can range from 0 to 75. If an injury is assigned an AIS of 6 (unsurvivable injury), the ISS is automatically scored as 75.[5]
The RTS is scored from the first set of patient data obtained, and is based on 3 physiological parameters: GCS, systolic blood pressure (SBP), and RR. The magnitude of the disturbance in each parameter is scored from 0 to 4. The RTS score ranges from 0 to 7.8408 and is calculated as follows[9]:
RTS = (0.9368 × GCS score) + (0.7326 × SBP score) + (0.2908 × RR score)
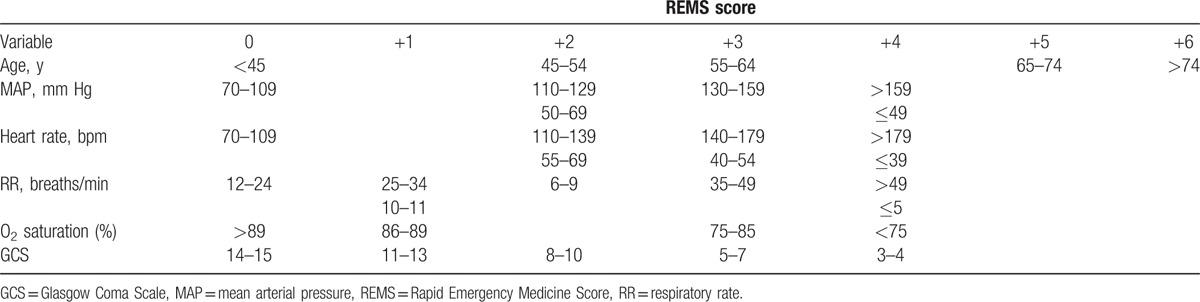
Calculating the REMS requires the patient's RR, HR, MAP, GCS, age, and oxygen saturation; age is assigned a value from 0 to 6, and the remaining 5 variables are each assigned values from 0 to 4 (see Table 1). The maximum REMS value is 26; higher scores are associated with worse prognoses.[6,7]
Table 1.
REMS scoring system.
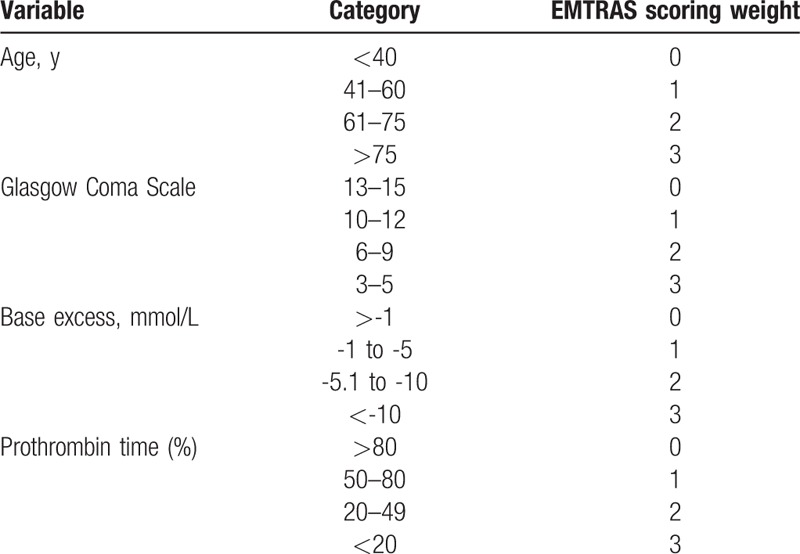
The EMTRAS is calculated using 4 variables: age, GCS, BE, and PT. These 4 factors are weighted equally to arrive at a final score (Table 2). The final score is a simple arithmetic sum of the integer subscores, and ranges from 0 to 12.[6]
Table 2.
EMTRAS scoring system.
2.3. Data analysis
Continuous variables were described using means and standard deviations, and categorical variables were described using frequencies and percentages. We calculated P values using Fisher exact or Pearson Chi-square tests for categorical variables and t tests for continuous variables. Sensitivity and specificity were plotted using receiver operating characteristic (ROC) curves. The discriminant power of the EMTRAS, REMS, ISS, and RTS were compared using area-under-the-curve (AUC) analyses, and Bonferroni corrections for multiple comparisons were performed. In addition, the optimal cut-off values were estimated using the Youden index.[10] Missing data were not replaced or imputed. Significant associations and differences were identified using P values < .05. All analyses were performed using R, version 3.3.4 for Windows (R Foundation for Statistical Computing, Vienna, Austria).
2.4. Ethics approval
Due to the retrospective nature of this study, the requirement of informed consent was waived. The study protocol was approved by the Institutional Review Board of Gyeongsang National University Hospital (approval number: GNUH 2017–06–010).
3. Results
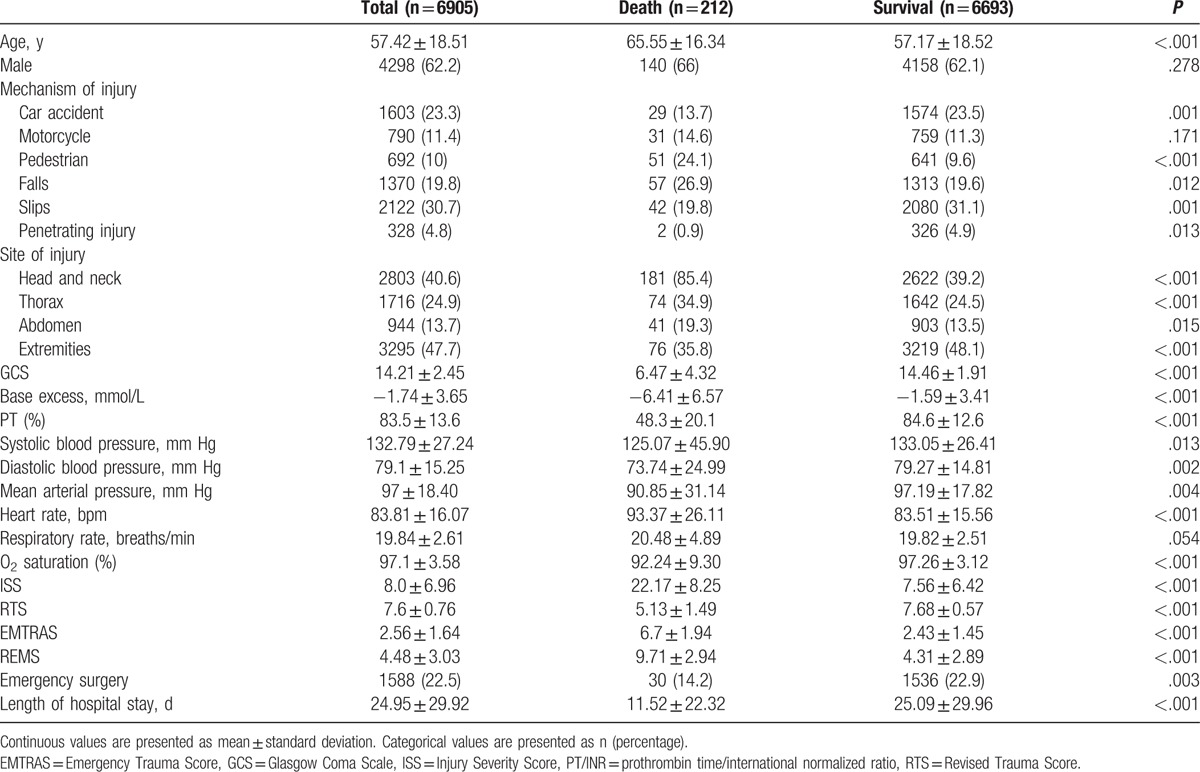
Of the 6905 patients included in the study, 6693 (96.9%) survived and 212 (3.1%) died in-hospital. Table 3 summarizes the demographic and clinical characteristics of the study population. The mean age was 57.4 years, and the majority of patients were male (62.2%). The main causes of trauma were slips (30.7%), car accidents (23.3%), and falls (19.8%). Most injuries involved the extremities (47.7%), and 22.5% were managed by emergency surgery. The mean length of hospital stay was 25.0 days. The mean values for the ISS, RTS, EMTRAS, and REMS were 8.0, 7.6, 2.56, and 4.48, respectively. Patients who survived had a mean age of 57.2 years, and 62.1% were male. Among the survivors, the mean values of the ISS, RTS, EMTRAS, and REMS were 7.56, 7.68, 2.43, and 4.31, respectively, and the mean length of hospital stay was 25.1 days. Patients who died had a mean age of 65.6 years; 66% were male. Within this group, the mean scores for the 4 instruments were 22.17, 5.13, 6.7, and 9.71, respectively, and the mean length of hospital stay was 11.5 days. Almost all of these variables differed significantly between survivor and nonsurvivor groups. However, there were no significant differences in sex (P = .278), motorcycle-related injuries (P = .171), or RRs (P = .054), between groups.
Table 3.
Demographic and clinical characteristics of study population (n = 6905).
All trauma scores had discriminant power, with AUCs of 0.957 (EMTRAS), 0.915 (ISS), 0.9 (REMS), and 0.924 (RTS) (Fig. 1). After correcting for multiple comparisons, the EMTRAS was superior to both REMS and ISS for predicting in-hospital mortality (P < .001), but it was not significantly different from the RTS (P = .057). No significant differences were found between the other trauma scores (Table 4). An EMTRAS of 5 was evaluated as the cut-off value for in-hospital mortality; at this cut-off value, the sensitivity and specificity for predicting mortality were 85.4% and 91.9%, respectively. The positive predictive value (PPV) was 25.1% and the negative predictive value (NPV) was 99.5%. A cut-off value of 7 was used to predict in-hospital mortality using the REMS, with a sensitivity, specificity, PPV, and NPV of 84.4%, 77.3%, 10.5%, and 99.4%, respectively.
Figure 1.
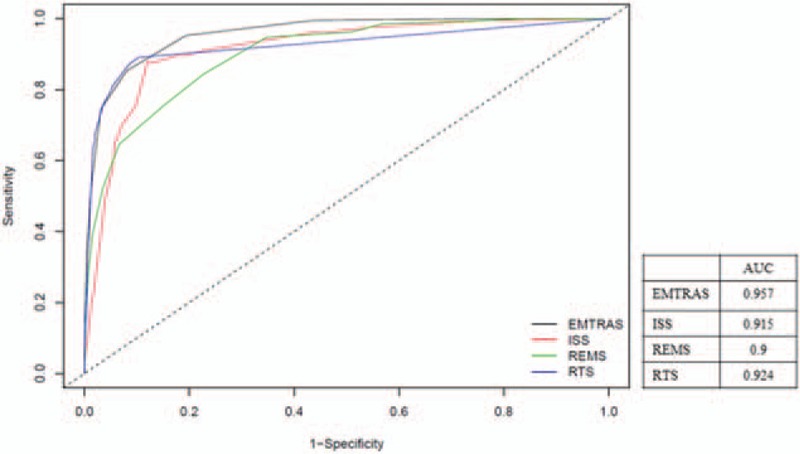
Receiver operating characteristic curves of the scoring systems. AUC = area under the curve, EMTRAS = emergency trauma score, ISS = injury severity score, REMS = rapid emergency medicine score, RTS = revised trauma score.
Table 4.
Pairwise comparison of area under the curve between different scoring systems.
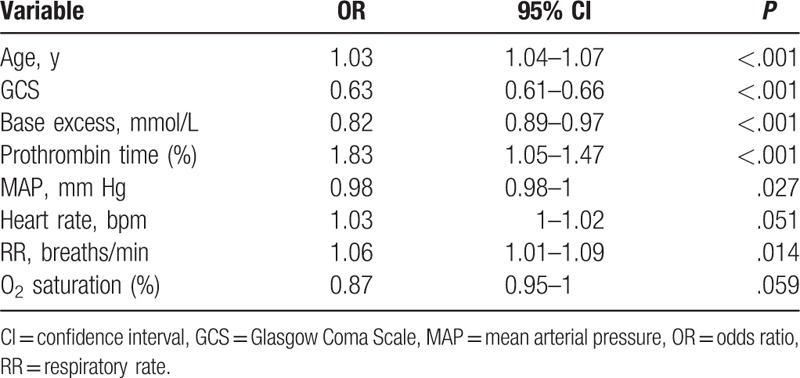
An assessment of the independent predictors of in-hospital mortality, using multivariable logistic regression, showed that HR (P = .051) and oxygen saturation (P = .059) did not predict mortality, individually, whereas GCS, BE, PT, MAP, and RR did. The strongest predictor of mortality was GCS (odds ratio, 0.63; 95% confidence interval, 0.61–0.66; P < .001) (Table 5).
Table 5.
Multiple logistic regression for all parameters in EMTRAS and REMS.
4. Discussion
In the present study, we analyzed 4 scoring systems used to assess injury-related trauma relative to in-hospital mortality in patients with trauma. Both the EMTRAS and REMS demonstrated acceptable predictive values for in-hospital mortality. Olsson et al[7] found that the REMS was a strong predictor of in-hospital mortality in patients seen in the ED, and had a higher predictive value than other scoring systems. This group also found that the REMS was a strong predictor of mortality in nonsurgical patients.[11,12] Even after incorporating the Charlson comorbidity index into the analysis, the REMS was highly predictive of mortality in nonsurgical patients.[13] In another study involving 3680 patients, Imhoff et al[6] found that higher REMS values were associated with higher mortality in patients with trauma. In that study, the REMS performed similarly to RTS in predicting mortality, but it outperformed other traditionally used trauma scoring systems, including the ISS and Shock Index.[6] Lee et al[8] compared the utility of the REMS and EMTRAS for predicting in-hospital mortality in nonsurgical ED patients and found both instruments had acceptable predictive validity, with the REMS performing similarly to EMTRAS.
The EMTRAS was developed in 2009 by Raum et al[2] and was based on a retrospective observational study conducted in 2 trauma centers in the Netherlands. The authors were able to accurately predict mortality based on 4 parameters assessed early in the emergency room. They suggested that the EMTRAS is a simple and robust tool that adequately predicts mortality compared with existing scores that are not suitable for early use in trauma management.[2] Mangini et al[14] also showed that the EMTRAS has a statistically significant association with mortality risk. All 4 parameters of the score are rapidly available, allowing physicians to quickly estimate injury severity before other examinations, such as computed tomography scans, are performed.[14] In another study conducted on 3318 patients, Joosse et al[15] found that the EMTRAS discriminated between surviving and nonsurviving patients with trauma. When applied to all trauma patients, predicted mortality was systematically high, compared with actual mortality, in patients with low-to-medium expected risk.[15]
Slight differences can be observed between the various studies evaluating the EMTRAS and REMS as predictors of in-hospital mortality. These differences likely stem from differences in the survey settings; each trauma scoring system has its own specific advantages and limitations.[16,17] An ideal scoring system for use in emergency setting should involve relatively few variables and be easy to use. An important limitation of the ISS and RTS is the difficulty associated with their early application. In this regard, both the EMTRAS and REMS are good candidates for application in emergency settings. On the basis of calculated AUCs, the present study showed that the predictive values for in-hospital mortality, for both the REMS (AUC = 0.9) and EMTRAS (AUC = 0.957), are excellent.
Several limitations to this study should be noted. First, we excluded records of patients from our study if they were missing the data required to calculate trauma scores. Second, data for the study were collected retrospectively, and as with all trauma registries, recorded data may suffer from some degree of inaccuracy. However, despite being a retrospective study, our results are valid due to the strength of the study since it involved a larger sample size. Finally, the study population was selected from a single hospital, which may have introduced selection bias that may limit generalization to other patients with trauma. Accurate prospective studies are needed to extend our findings.
5. Conclusion
The ability to predict in-hospital mortality quickly and accurately could lead to improved patient outcomes. In this study, we showed that the EMTRAS and REMS tools are simple, accurate predictors of in-hospital mortality in patients with trauma. We anticipate that the EMTRAS and REMS can be more easily used in ED settings as predictors of in-hospital mortality.
Acknowledgment
We acknowledge the outstanding contributions of the technicians and nursing staff at the Gyeongsang National University Hospital.
Footnotes
Abbreviations: AIS = Abbreviated Injury Scale, APACHE = Acute Physiology and Chronic Health Evaluation, AUC = area under the curve, BE = base excess, ED = emergency department, EMTRAS = Emergency Trauma Score, GCS = Glasgow Coma Scale, HR = heart rate, ISS = Injury Severity Score, MAP = mean arterial pressure, NPV = negative predictive value, PPV = positive predictive value, PT = prothrombin time, REMS = Rapid Emergency Medicine Score, ROC = receiver operating characteristic, RR = respiratory rate, RTS = Revised Trauma Score, SBP = systolic blood pressure.
The authors declare no conflicts of interest.
References
- [1].Lendrum RA, Lockey DJ. Trauma system development. Anaesthesia 2013;68:30–9. [DOI] [PubMed] [Google Scholar]
- [2].Raum MR, Nijsten MW, Vogelzang M, et al. Emergency trauma score: an instrument for early estimation of truma severity. Crit Care Med 2009;37:1972–7. [DOI] [PubMed] [Google Scholar]
- [3].Kondo Y, Abe T, Kohshi K, et al. Revised trauma scoring system to predict in-hospital mortality in the emergency department: Glasgow Coma Scale, Age, and Systolic Blood Pressure score. Crit Care 2011;15:R191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Moore L, Lavoie A, LeSage N, et al. Statistical validation of the Revised Trauma Score. J Trauma 2006;60:305–11. [DOI] [PubMed] [Google Scholar]
- [5].Baker SP, O’Neill B, Haddon W, Jr, et al. The Injury Severity Score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma 1974;14:187–96. [PubMed] [Google Scholar]
- [6].Imhoff BF, Thompson NJ, Hastings MA, et al. Rapid emergency medicine score (REMS) in the trauma population: a retrospective study. BMJ Open 2014;4:e004738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Olsson T, Terent A, Lind L. Rapid Emergency Medicine score: a new prognostic tool for in-hospital mortality in nonsurgical emergency department patients. J Intern Med 2004;255:579–87. [DOI] [PubMed] [Google Scholar]
- [8].Lee SH, Park JM, Park JS, et al. Utility of the Rapid Emergency Medicine Score (REMS) for predicting hospital mortality in severely injured patients. J Korean Soc Emerg Med 2016;27:199–205. [Google Scholar]
- [9].Champion HR, Sacco WJ, Copes WS, et al. A revision of the trauma score. J Trauma 1989;29:623–9. [DOI] [PubMed] [Google Scholar]
- [10].Ruopp MD, Perkins NJ, Whitcomb BW, et al. Youden index and optimal cut-point estimated from observations affected by a lower limit of detection. Biom J 2008;50:419–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Olsson T, Lind L. Comparison of the Rapid Emergency Medicine score and APACHE II in nonsurgical emergency department patients. Acad Emerg Med 2003;10:1040–8. [DOI] [PubMed] [Google Scholar]
- [12].Olsson T, Terent A, Lind L. Rapid Emergency Medicine Score can predict long-term mortality in nonsurgical emergency department patients. Acad Emerg Med 2004;11:1008–13. [DOI] [PubMed] [Google Scholar]
- [13].Olsson T, Terent A, Lind L. Charlson Comorbidity Index can add prognostic information to Rapid Emergency Medicine Score as a predictor of long-term mortality. Eur J Emerg Med 2005;12:220–4. [DOI] [PubMed] [Google Scholar]
- [14].Mangini M, Valvasone SDi, Greco C, et al. Validation of the new proposed Emergency Trauma Score (EMTRAS). Crit Care 2010;14:252. [Google Scholar]
- [15].Joosse P, de Jong WJ, Reitsma JB, et al. External validation of the Emergency Trauma Score for early prediction of mortality in trauma patients. Crit Care Med 2014;42:83–9. [DOI] [PubMed] [Google Scholar]
- [16].Owen JL, Bolenbaucher RM, Moor ML. Trauma registry databases: a comparison data abstraction, interpretation, and entry at two level I trauma centres. J Trauma 1999;46:1100–4. [DOI] [PubMed] [Google Scholar]
- [17].Park HO, Kang DH, Moon SH, et al. Risk factors for pneumonia in ventilated trauma patients with multiple rib fractures. Korean J Thorac Cardiovasc Surg 2017;50:345–54. [DOI] [PMC free article] [PubMed] [Google Scholar]


