Abstract
Rationale:
Malignant granular cell tumor is a kind of rare and highly aggressive malignant tumor that commonly occurs in lower extremity, trunk, and peritoneal cavity. Huge malignant granular cell tumor (MGCT) with suprascapular nerve and brachial plexus invasion was extremely rare.
Patient concerns:
We present a special case of a 48-year-old orthopedist who suffered from MGCT. The orthopedist had regarded that he suffered from scapulohumeral periarthritis.
Diagnoses:
The disease was noticed until a painless mass on his right neck was discovered 9 months later. MRI result confirmed a large occupying in axillary fossa, supraclavicular and infraclavicular region.
Interventions:
During the operation, a tumor measuring 22 × 13 × 6 cm with suprascapular nerve and brachial plexus invasion was identified. The tumor was fractional resected carefully to maintain the integrity of nerves and vessels. Lymph nodes were simultaneously resected.
Outcomes:
The motor function and sensation of the upper extremity were same to that of preoperation. The postoperative histological diagnosis was MGCT. At a 12-month follow-up, there was no recurrence of the tumor showed by MRI.
Lessons:
This study presents a rare case of large MGCT with suprascapular nerve and brachial plexus invasion that was successfully managed by surgery.
Keywords: brachial plexus, malignant granular cell tumor, scapulohumeral periarthritis, suprascapular nerve
1. Introduction
Malignant granular cell tumor (MGCT) is a kind of rare and highly aggressive malignant tumor that commonly occurs in lower extremity, trunk, and peritoneal cavity. MGCT is a highly aggressive tumor with high rate of recurrence and metastasis. The prognosis is generally poor.
MGCT with peripheral nerve invasion could present as relevant neurological symptom. We present a case of an orthopedist who suffered from MGCT. The tumor invaded suprascapular nerve at first. The early symptom resembled scapulohumeral periarthritis. A large tumor with suprascapular nerve and brachial plexus invasions was a great challenge for surgeons.
This study presents a rare case of large MGCT with suprascapular nerve and brachial plexus invasion that was successfully managed by surgery without destructing the nerve function.
2. Case report
A 48-year-old orthopedist felt pain and suffered from motion limitation of right shoulder for >10 months. As an experienced orthopedist, he thought he suffered from scapulohumeral periarthritis and paid no attention to the disease. He just took rehabilitation exercises occasionally. The symptoms deteriorated progressively through 9 months. A painless mass was discovered on his right neck.
Physical examination showed the range of motion was 30° for shoulder abduction, 20° for external rotator, 60° for internal rotator, and 50° for anteflexion. The strength of muscles innervated by musculocutaneous nerve, radial nerve, median nerve, and ulnar nerve were M4. Obvious muscle atrophy was only noticed in supraspinatus and infraspinatus.
MRI showed large occupying in axillary fossa, supraclavicular and infraclavicular region. Malignant tumor with multiple enlarged lymph nodes was highly considered (Fig. 1).
Figure 1.
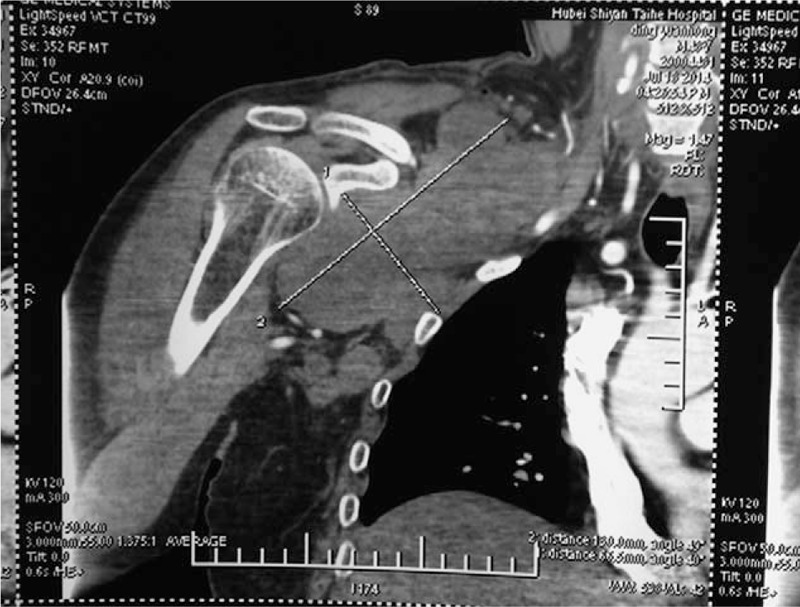
MRI shows large occupying in axillary fossa, supraclavicular and infraclavicular region.
The patient went to our department for further treatment. An open biopsy was made. The pathological diagnosis was MGCT. As an orthopedist, the patient was conscious of the severity of the disease, and strongly hoped to reserve the function of upper extremity to improve life quality.
Operation (Figs. 2 and 3): An incision from the infraclavicular region to the supraclavicular region was made. A hard mass measuring 22 cm × 13 cm × 6 cm, with unclear boundary and abundant blood supply, was identified. The superior border of the tumor was above the clavicle. The inferior border of the tumor was parallel with the 8th rib. The anterior border was the posterior border of sternocleidomastoid and superficial fascia. The posterior border was the anterior border of trapezius and the medial border of the scapula. The ribs and the scapular were invaded by the tumor. Multiple enlarged lymph nodes were discovered. The cord and branch of brachial plexus and vessels were oppressed to the ribs. The tumor was fractional resected carefully to maintain the integrity of nerves and vessels. Lymph nodes were resected simultaneously. Intraoperative electromyography did not record compound muscle action potential (CMAP) at infraspinatus by stimulating the suprascapular nerve. CMAP was recorded by stimulating axillary nerve, musculocutaneus nerve, median nerve, radial nerve, and ulnar nerve. After the operation, the motor function and sensation of the upper extremity were same to that of preoperation.
Figure 2.
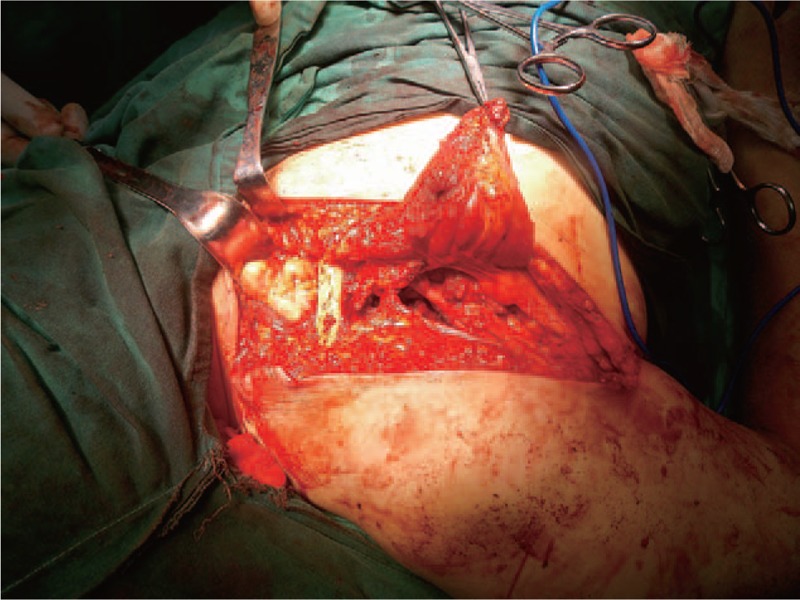
The tumor was exposed.
Figure 3.

The tumor was fractional resected.
The postoperative histological pathologic diagnosis was MGCT (Fig. 4). Immunohistochemical staining demonstrated that S100 (+), vimentin (+), SMA (+), CD34 (+), CD68 (+), NSE (+), CK (−), EMA (−), Desmin (−), NF (−), Ki67 (10%+).
Figure 4.
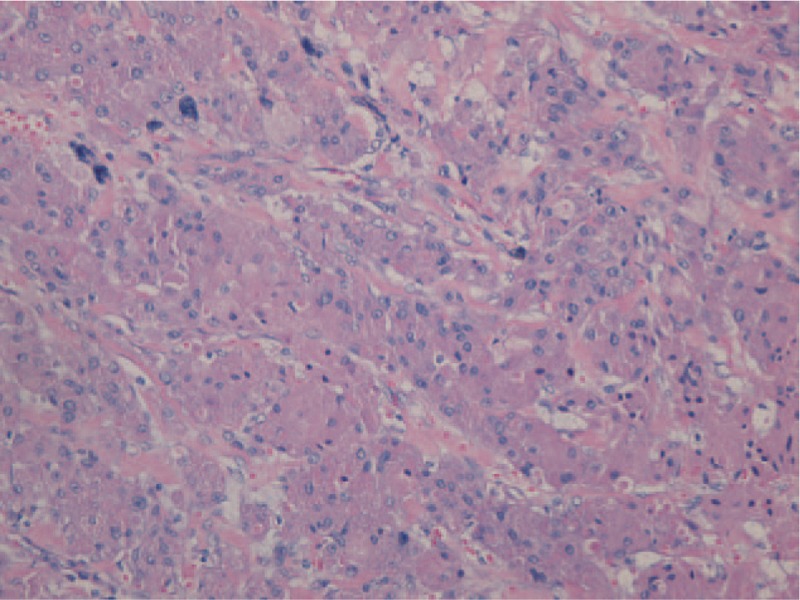
The postoperative histological pathologic diagnosis was malignant granular cell tumor.
After the surgery, the patient did not take chemotherapy or radiotherapy. At a 1-year follow-up, no recurrence of the tumor was discovered by MRI. No sensory disturbance or dyskinesia was discovered.
The patient agreed to authorize us to share the figures and the experiences during his treatment procedure in our department. Informed consent was obtained.
3. Discussion
MGCT is a kind of rare malignant tumor that comprises <2% of all granular cell tumors. It has a female dominance of approximately 2:1 and mainly afflicts people aged 30 to 70 years old.
Lower extremity, trunk, and peritoneal cavity were the most commonplace involved MGCT reported in literature. However, tumor that involves the peripheral nerve of upper extremity is rare. The nerves reported in literature associated with MGCT include radial nerve,[1,2] ulnar nerve,[3] and brachial plexus.[4] Such a large MGCT (22cm × 13cm × 6 cm) with suprascapular nerve and the brachial plexus invasion has not been reported.
MGCT with peripheral nerve invasion could present as relevant neurological symptom, such as numbness, hyperesthesia, and neural paralysis.[5] As the tumor invaded suprascapular nerve at first, the early symptom presented as pain and motion limitation of the shoulder, which resembled scapulohumeral periarthritis. Despite being an experienced orthopedist, the patient still paid no attention to the disease, and missed the opportunity for early diagnosis and treatment. However, although the brachial plexus was oppressed by the tumor severely, there was no obvious neurological symptom. Through this case, it should be emphasized that excluding tumor's oppressing suprascapular nerve is necessary when diagnosed the patients whose symptom resembles scapulohumeral periarthritis.
The immunohistochemical staining studies, S-100 protein, and NSE were strongly positive in almost all MGCTs. CD68 was positive in part of the cases. NF and demsin were often negative. The immunohistochemical staining of our case revealed positive in S-100 protein, NSE and CD68, which conformed to the literature.
It is widely acknowledged that wide local excision and regional lymph nodes dissection were the first choice of treatment. The tumor of our patient was large and invaded suprascapular nerve and brachial plexus. These all increased the difficulties for operation. In consideration of the advanced course of the disease and the patient's request, protecting the nerve and keeping the function of the upper extremity to improve life quality were extremely important. We separated suprascapular nerve and brachial plexus, and resected the tumor meticulously and cautiously during the surgery. Considering the tumor was large and seriously adherent to nerve and vessels, fractional resection was made instead of completely resection. After the operation, the motion function and sensation of the upper extremity were same to that of preoperation.
The effect of both chemotherapy and radiotherapy for MGCT is considered to be unsatisfactory.[6] Our patient took neither chemotherapy nor radiotherapy.
The prognosis of MGCT is generally poor, with high rate of local recurrence and metastasis. Poor prognostic factors include advanced age, large tumor size, increased mitotic activity, and Ki-67 >10%.[7] The most probable place for metastasis is regional lymph nodes and lung. The other regions for distant metastasis include liver, spleen, pancreas, bone, and kidney.[8] The mean survival time for MGCT patient is approximately 2.5 years. At a 1-year follow-up, there was no recurrence of the tumor showed by MRI in our patient
4. Conclusions
This study presents a rare case of large MGCT with suprascapular nerve and brachial plexus invasion that was successfully managed by surgery. It should also be emphasized that excluding tumor's oppressing suprascapular nerve is necessary when diagnosed the patients whose symptom resembles scapulohumeral periarthritis.
Footnotes
Abbreviations: CMAP = compound muscle action potential, MGCT = malignant granular cell tumor.
The present study was sponsored by the Scientific Research project supported by Huashan Hospital, Fudan University (Shanghai, China, grant no. 2013QD05).
XJ and CC equally contributed to the work and should be regarded as co-first authors.
The authors have no conflicts of interest to disclose.
References
- [1].Usui M, Ishii S, Yamawaki S, et al. Malignant granular cell tumor of the radial nerve: an autopsy observation with electron microscopic and tissue culture studies. Cancer 1977;39:1547–55. [DOI] [PubMed] [Google Scholar]
- [2].Sonobe H, Iwata J, Furihata M, et al. Malignant granular cell tumor: report of a case and review of the literature. Pathol Res Pract 1998;194:507–13. [DOI] [PubMed] [Google Scholar]
- [3].Papachristou DJ, Palekar A, Surti U, et al. Malignant granular cell tumor of the ulnar nerve with novel cytogenetic and molecular genetic findings. Cancer Genet Cytogenet 2009;191:46–50. [DOI] [PubMed] [Google Scholar]
- [4].Go MH, Kim SH, Cho KH. Brachial plexus tumors in a consecutive series of twenty one patients. J Korean Neurosurg Soc 2012;52:138–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Di Tommaso L, Magrini E, Consales A, et al. Malignant granular cell tumor of the lateral femoral cutaneous nerve: report of a case with cytogenetic analysis. Hum Pathol 2002;33:1237–40. [DOI] [PubMed] [Google Scholar]
- [6].Wang J, Zhu XZ, Zhang RY. [Malignant granular cell tumor: a clinicopathologic analysis of 10 cases with review of literature]. Zhonghua Bing Li Xue Za Zhi 2004;33:497–502. [Chinese]. [PubMed] [Google Scholar]
- [7].Fanburg-Smith JC, Meis-Kindblom JM, Fante R, et al. Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation. Am J Surg Pathol 1998;22:779–94. [DOI] [PubMed] [Google Scholar]
- [8].Pérez-González YC, Pagura L, Llamas-Velasco M, et al. Primary cutaneous malignant granular cell tumor: an immunohistochemical study and review of the literature. Am J Dermatopathol 2015;37:334–40. [DOI] [PubMed] [Google Scholar]


