Abstract
Percutaneous transhepatic gallbladder drainage followed by laparoscopic cholecystectomy (PTGBD+LC) is one treatment option for patients with moderate to severe acute cholecystitis (AC). However, the impact of PTGBD on operative difficulties in performing LC is controversial. We designed this retrospective study to clarify the surgical outcomes after PTGBD+LC for the management of patients with moderate to severe AC.
The medical records of 85 patients who underwent LC for moderate to severe AC from January 2013 to September 2016 were evaluated. They were divided into 2 groups based on the type of management: group A received PTGBD+LC, and group B received LC without drainage. We compared the patient characteristics, laboratory data which were obtained immediately before surgery or PTGBD at index admission, and surgical outcomes between the 2 groups. We also evaluated possible predictive factors associated with prolonged operative duration after PTGBD+LC.
Patients in group A were older and had more comorbidities than those in group B. The laboratory tests obtained at index admission in group A showed higher serum levels of C-reactive protein (CRP) and alkaline phosphatase, and lower albumin levels than those in group B. The surgical outcomes after LC were similar between the 2 groups. However, operative duration was significantly shorter in group A (P = .012). In group A, a higher serum level of CRP was a predictive factor for a prolonged operation (hazard ratio 1.126; 95% confidence interval 1.012–1.253; P = .029). In conclusion, PTGBD+LC can shorten the operative duration in patients with moderate to severe AC, which might improve surgical outcomes in elderly patients with comorbidities, and elevated CRP values predicted a prolonged operation after PTGBD.
Keywords: cholecystitis, cholecystostomy, laparoscopic cholecystectomy, operative duration
1. Introduction
Based on refinements in laparoscopic technique and increased surgical experience, early laparoscopic cholecystectomy (LC) has become a standard treatment for patients with acute cholecystitis (AC).[1,2] However, some clinical situations such as local advanced inflammation near the gallbladder or a high risk for general anesthesia present surgeons with the dilemma of whether to perform an LC without drainage or to insert a drainage catheter as bridge management.
Since percutaneous transhepatic gallbladder drainage (PTGBD) was first introduced by Radder in 1980,[3] it has been widely used and has had the benefits of a low complication rate, being a simple operation with early symptom relief and improvements in acute inflammation. According to the Tokyo guidelines (TG) for the treatment of AC, PTGBD can be applied selectively for patients with moderate to severe AC, followed by scheduled LC.[4] Despite these positive effects on the management of patients with AC, PTGBD can induce repeated biliary events or catheter-related complications resulting in high readmission rates during the interval to LC. In particular, the effects of PTGBD on operative duration and open conversion rates reflecting surgical difficulties have not been identified clearly in patients with moderate to severe AC. Therefore, we designed this retrospective study to clarify the impact of preoperatively performed PTGBD on surgical difficulties and to evaluate the predictive factors of prolonged operative duration in patients who received LC after PTGBD for moderate to severe AC.
2. Materials and methods
2.1. Patients
The records of 85 consecutive patients who underwent LC for moderate to severe AC from January 2013 to September 2016 were included in this study. We excluded patients with a history of upper abdominal surgery or endoscopic retrograde cholangiography for choledocholithiasis because these situations can have a significant influence on operative difficulty. The patients with acalculous cholecystitis were also excluded in this study. The diagnosis and severity of cholecystitis were assessed using the assessment criteria of TG, and then the patients were divided into 2 groups based on the type of management: group A underwent LC after PTGBD, and group B received LC without drainage. In cases of moderate AC, marked local inflammatory conditions such as gangrenous cholecystitis, pericholecystic abscesses, hepatic abscesses, biliary peritonitis, or emphysematous cholecystitis were diagnosed when imaging studies showed typical features of these conditions on abdominal ultrasonography or computed tomography (CT) at first presentation, because a direct comparison of intraoperative findings between the 2 groups was impossible. Gangrenous cholecystitis was diagnosed when CT scans showed a nonenhanced gallbladder wall image, sloughed membranes, mural striations, and an irregular enhanced wall image with defects.[5]
The study was approved by the Institutional Review Board of Kyungpook National University Hospital. Informed consent was waived because of the retrospective nature of this study (KNUH 2017–02–004).
2.2. PTGBD timing, technique, and follow-up cholangiography
When a technically complex operation was anticipated because of severe local inflammation and the patients had comorbidities needing further evaluation for general anesthesia or were unfit for early LC, PTGBD was applied as early as possible. After ultrasound-guided transhepatic gallbladder puncture was done using an 18-G needle, a 21-gauge Chiba needle was advanced into the gallbladder followed by sequential dilatation of the tract, and then a 7- to 10-Fr pigtail catheter was inserted using monitoring with fluoroscopy. Bile taken at the time of this procedure was studied to culture and identify any microorganisms. We performed follow-up cholangiography in patients suspected of biliary obstruction, such as an elevated level of serum bilirubin and dilated bile ducts on imaging studies, or in patients with impacted small cystic duct stones. Cholangiography was also performed when the patient was scheduled to remove the catheter. The catheter was routinely left in situ for a minimum of 6 weeks before removal and was removed after confirming that there were no bile duct stones at cholangiography. When the patients recovered from acute illness, organ dysfunction, and completed the evaluation of comorbidities, we performed LC after PTGBD.
2.3. LC procedures
LC was performed with the patient under general anesthesia by one surgeon who had experience in 200 or more LC procedures annually. Most patients received classic 3-port LC with retrograde dissection. When the operation needed a clearer surgical view because of adhesions or inflammatory changes around the gallbladder, another 5-mm trocar was placed below the right costal margin in the midaxillary line. Antegrade gallbladder dissection was performed for those patients with severe inflammation or fibrotic changes that obscured the surgical anatomy at Calot's triangle. When the cystic duct was too wide for clipping, an endoloop was used for secure closure.
2.4. Variables for comparison of 2 groups
We retrospectively reviewed the hospital's medical database for information including age, gender, body mass index, medical comorbidities, symptom duration, body temperature, and presence of a palpable mass at index presentation. Laboratory data such as serum levels of aspartate aminotransferase (AST), alanine aminotransferase (ALT), alkaline phosphatase, white blood cell (WBC) counts, C-reactive protein (CRP), total bilirubin, albumin, and creatinine were obtained immediately before surgery or PTGBD at index admission and compared between the 2 groups. For surgical outcomes, operative duration, open conversion rate, complications according to the Dindo-Clavien classification, and duration of postoperative hospital stay were reviewed.
2.5. Definition of prolonged operative duration among patients in group A
Prolonged operative duration was defined when completion of the LC took more than 90 minutes based on previous reports linking operative duration to outcome in patients undergoing LC.[6,7]
2.6. Statistical analysis
Student independent t tests were used to compare the differences between means of continuous variables, and categorical variables were subjected to χ2 analysis if the sample size was adequate or to Fisher exact test if the sample was small. Variables with P < .2 by univariate analysis were further analyzed by a binary logistic regression analysis to identify independent predictors for a prolonged operation. Subsequently, a cutoff point for an independent predicting factor for long operative duration was determined using a receiver-operating characteristic (ROC) curve. The best cutoff value was defined as the value with the highest sum of sensitivity and specificity on the ROC curve. Statistical analyses were performed using IBM SPSS statistics for Windows (version 20.0; IBM Corp., Armonk, NY), and P < .05 was considered to be statistically significant. Results are presented as the hazard ratio (HR) and 95% confidence interval (CI) or as the mean ± the standard deviation (SD) of the mean.
3. Results
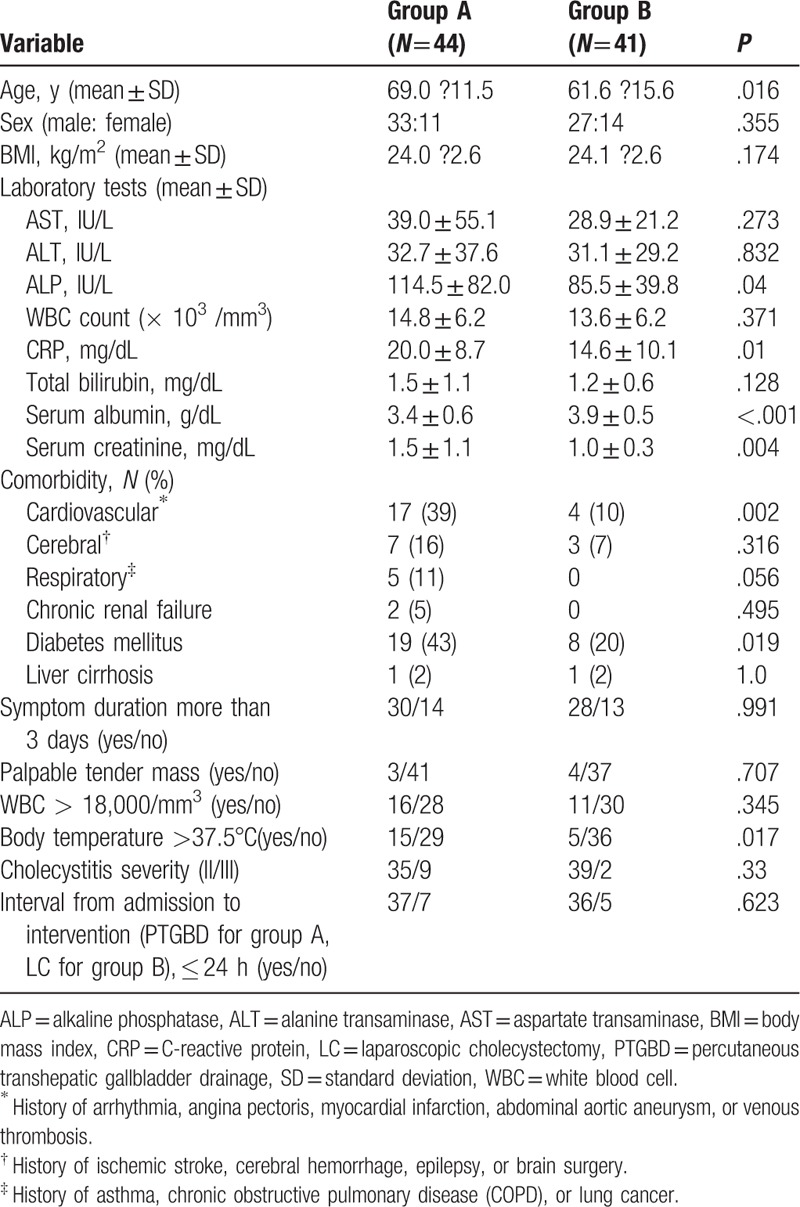
Of 85 patients with moderate to severe AC, 44 treated with LC after PTGBD were classified as group A, and 41 patients who received LC without PTGBD were classified as group B. Eight patients in group A were admitted to an ICU for management of biliary sepsis and there were no patients in group B who needed ICU treatment. In group A, the PTGBD was inserted as early as possible within a mean of 6 hours from index admission, and was successfully inserted without complications in all. However, three patients had to reinsert the catheter because of dislodge during the intervening period. Follow-up cholangiography was performed in 20 patients. Bile cultures grew bacteria in 29 patients from group A. Eighteen patients were discharged with a drainage tube and LC was performed at a mean of 30 days after PTGBD placement. Thirty-six patients in group B received LC within 24 hours of index admission, and 3 patients underwent LC 1 to 3 days after admission. The remaining 2 patients underwent LC more than 7 days after index admission because of hepatic abscesses or a misdiagnosis of AC as enteritis. The demographic features and preoperative investigations of the 2 groups on index admission are listed in Table 1. Male patients predominated in both groups, and patients in group A showed higher frequencies of cardiovascular comorbid conditions and diabetes mellitus than did those in group B. With respect to the TG diagnostic criteria of moderate AC, the presence of an elevated WBC count (>18,000 cells/mm3), a palpable tender mass in the right upper abdominal quadrant, and duration of complaints >72 hours did not show statistically significant differences between the groups, and the proportion of severe cholecystitis was similar. However, laboratory tests performed at the time of the index admission showed higher serum levels of ALP (114.5 ± 82.0 vs 85.5 ± 39.8 IU/L, P = .04), CRP (20.0 ± 8.7 vs 14.6 ± 10.1 mg/dL, P = .01), and creatinine (1.5 ± 1.1 vs 1.0 ± 0.3 mg/dL, P = .004), and lower levels of serum albumin (3.4 ± 0.6 vs 3.9 ± 0.5 g/dL, P < .001) in group A, and a body temperature >37.5°C was also more frequent in group A.
Table 1.
Demographic features and investigations of the 2 groups on index admission.
3.1. Operative results
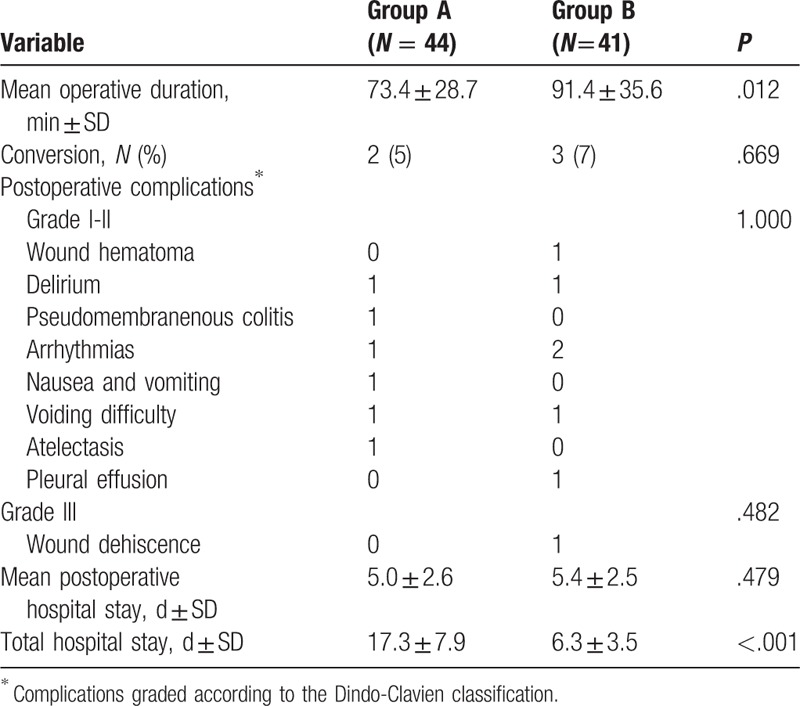
The surgical outcomes such as mean operative duration, conversion rate, postoperative complications according to the Dindo-Clavien classification, postoperative hospital stay, and total hospital stay are listed in Table 2. Five patients were converted to an open cholecystectomy. In group A, 2 cases were converted to open cholecystectomy because of severe adhesions and chronic inflammation with fibrosis near the Calot's triangle, respectively, whereas adhesions were the reason for all 3 cases of conversion in group B. The mean hospital stay after surgery was 5 days in both groups, and there was one wound dehiscence in group B. There were no biliary complications requiring surgical or radiological interventions. Importantly, the operative time was significantly shorter in group A (73.4 ± 28.7 min in group A vs 91.4 ± 35.6 min in group B, P = .012), despite higher serum levels of inflammatory markers, a higher frequency of body temperature >37.5°C and a higher frequency of comorbidities than in group B.
Table 2.
Surgical outcomes of the 2 study groups.
3.2. Factors predictive of long operative duration in group A
Table 3 lists the predictive factors associated with prolonged operative duration in group A identified from univariate analyses. The presence of respiratory comorbidities, higher serum levels of CRP, and lower levels of serum albumin at index admission all showed P < .2 and so were further included in the binary logistic regression analysis. In this, a higher serum level of serum CRP (HR 1.126; 95% CI 1.012–1.253; P = .029) was an independent predictive factor for a prolonged operative duration in group A. The ROC analysis revealed that a cutoff point of the serum level of CRP at 21.3 mg/dL gave a sensitivity of 80.0% and a specificity of 66.7% for predicting a long operative duration (Fig. 1).
Table 3.
Univariate analysis of predictive factors associated with prolonged operative duration for laparoscopic cholecystectomy performed after percutaneous transhepatic gallbladder drainage.
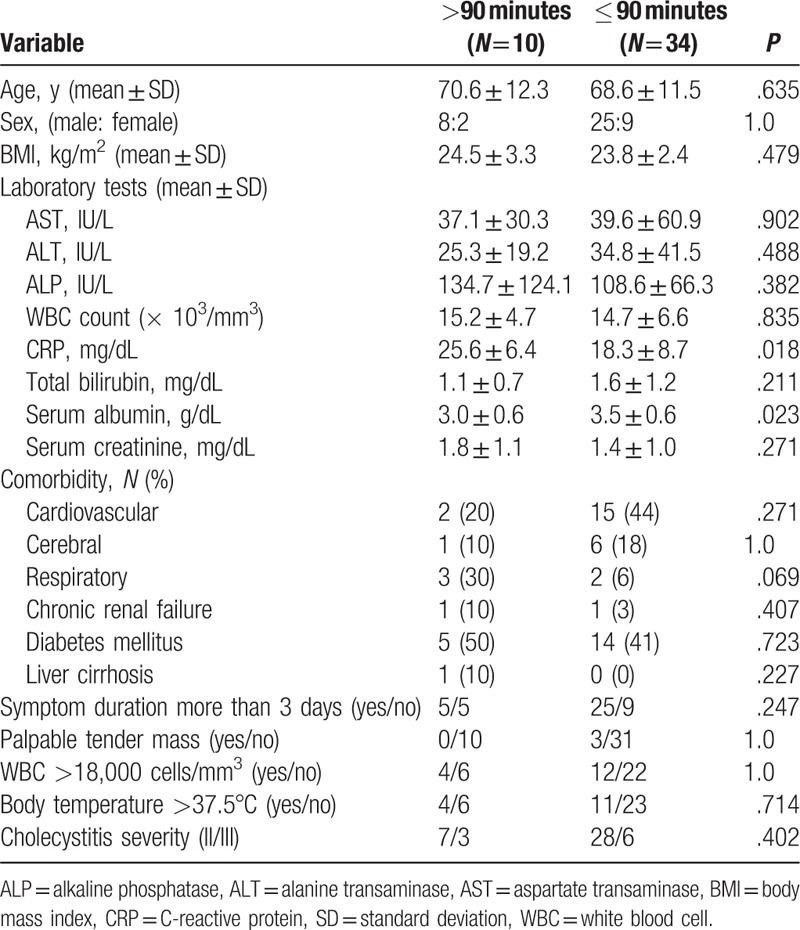
Figure 1.
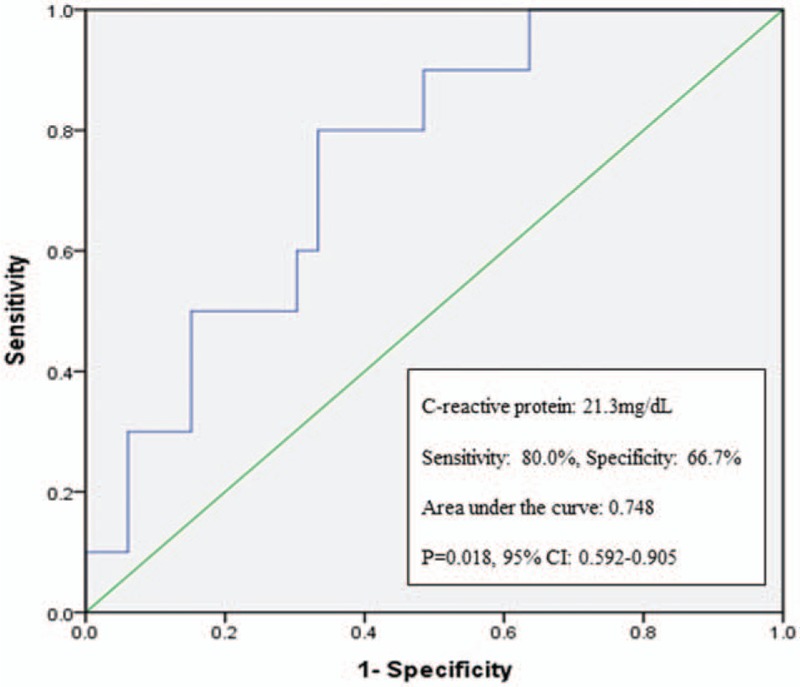
Results of the receiver-operating characteristic curve analysis of C-reactive protein levels.
4. Discussion
This study shows that PTGBD+LC can shorten the operative duration in patients with moderate to severe AC, despite higher serum levels of inflammatory markers, a higher frequency of body temperature >37.5°C and a higher frequency of comorbidities than in group B and elevated CRP values predicts a prolonged operation after PTGBD. Currently, published guidelines including those of SAGES and WSES recommend early cholecystectomy for the treatment of AC.[1,2] However, patients with AC present with a diverse spectrum of acute inflammation linked to operative difficulty, and the severity assessment criteria were first presented in the TG. From the flowchart for the management of patients with AC in the TG, early LC is the mainstay of treatment, but there are some indications for PTGBD to alleviate local inflammation or to recover from critical illnesses.[4] From a clinical point of view, PTGBD shows positive aspects with a high success rate of puncture, early remission of the symptoms, and low complication rates.[8] However, there is a controversy as to whether PTGBD followed by LC is better than LC without drainage for patients with moderate to severe AC in terms of surgical difficulties. Lo et al[9] reported that urgent LC without PTGBD had comparable surgical outcomes as that of PTGBD followed by elective LC for the management of gallbladder perforation, and PTGBD had the adverse outcome of a longer hospital stay. Sanjay et al[10] studied 53 patients with moderate to severe AC and showed a 67% conversion rate to an open cholecystectomy when LC followed PTGBD, which was inserted at a median of 3 days after admission. Another retrospective analysis, which comprised 639 patients who underwent delayed LC with or without PTGBD, showed greater conversion rates and longer operative times in patients with acute cholecystitis receiving PTGBD compared with a patient cohort not receiving this procedure; this result was possibly associated with the ongoing inflammatory processes and adhesions that might develop during the intervening period. In these patients, PTGBD was inserted at a mean of 3.4 days after index presentation.[11] Conversely, Kim et al[12] reported that elective delayed LC after applying PTGBD might lower the conversion and complication rates of patients with complicated AC. In our study, the demographics and laboratory results of patients at index admission showed some differences between the 2 groups. Group A patients were older and had more comorbidities and inflammatory conditions such as elevated body temperature, and serum CRP levels were worse than in group B. Nevertheless, patients in group A had a shorter mean operative duration, and the complication rate and postoperative hospital stay duration were similar to those in group B. We inserted the PTGBD as early as possible, with a mean interval of 6 hours from index admission, which was shorter than in other studies showing higher conversion rates and longer operative durations in patients receiving PTGBD.[10,11] We thought that early drainage of infected bile could reduce local inflammation effectively and might facilitate operative procedures. Regarding this, Bickel et al[13] also reported that early PTGBD decreased the conversion rate of delayed LC and recommended early percutaneous cholecystostomy to halt the propagation of the inflammatory process for selected patients.
Here, the serum CRP level at index admission was a predictive factor for a prolonged operation in group A, and a serum level of 21.3 mg/dL gave a sensitivity of 80.0% and a specificity of 66.7% for predicting this outcome. Recent reports have shown a link between serum CRP levels and the severity of cholecystitis.[14,15] In addition, Wevers et al[16] demonstrated that an elevated serum CRP level set at a cutoff level of 16.5 mg/dL was an independent predictor for conversion. In fact, in this retrospective study, the surgical outcomes after LC without drainage did not differ from that of LC after PTGBD except for operative duration. However, this can be critical when managing elderly patients or those with comorbidities. Jackson et al[6] studied the association of complications with operative time and concluded that it can be considered to be a potentially important determinant of patient outcome. Similarly, Procter et al[7] reported that operative duration was independently associated with increased infectious complications.
Our study had some limitations. First, many patients received PTGBD before LC because of our institutional policy on general anesthesia and logistic considerations. However, most of the patients in group A had a predictive factor for failure of conservative treatment, such as age >70 years, WBC count >15000 cells/mm3, diabetes, or elevated body temperature.[17] In addition, the aim of this study was not to justify the liberal use of PTGBD but to evaluate the clinical impact of this procedure followed by LC in patients with moderate to severe cholecystitis. Second, when comparing groups A and B, only imaging study findings were used as the criteria for marked local inflammation. This approach might have given an inaccurate diagnosis of such a problem. Finally, the small-scale, retrospective nature of the study might have influenced the results. Therefore, a large-scale prospective randomized trial would be ideal for investigating the impact of PTGBD on patients with moderate to severe AC.
5. Conclusions
In conclusion, PTGBD before elective LC for patients with moderate to severe AC can shorten the operative duration, and the incidence of postoperative complications were similar between 2 groups despite worse condition in group A. Our analyses also suggest that elective LC after PTGBD for the management of moderate to severe AC should be prepare with caution in patients with elevated serum CRP levels, because this factor predicts the likelihood of a difficult operation.
Footnotes
Abbreviations: ALP = alkaline phosphatase, ALT = alanine transaminase, AST = aspartate transaminase, BMI = body mass index, CRP = C-reactive protein, LC = laparoscopic cholecystectomy, PTGBD = percutaneous transhepatic gallbladder drainage, SD = standard deviation, WBC = white blood cell.
The authors declare conflict of interest.
R.L. contributed to the analysis of the data and drafted the article. H.H., Y.S.H., and H.J.K. did the interpretation of the data for the work. H.R contributed to the concept and critically revised the work. J.M.C designed the study and finalized the manuscript. All authors approved the final version.
References
- [1].Overby DW, Apelgren KN, Richardson W, et al. SAGES guidelines for the clinical application of laparoscopic biliary tract surgery. Surg Endosc 2010;24:2368–86. [DOI] [PubMed] [Google Scholar]
- [2].Ansaloni L, Pisano M, Coccolini F, et al. 2016 WSES guidelines on acute calculous cholecystitis. World J Emerg Surg 2016;11:25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Radder RW. Ultrasonically guided percutaneous catheter drainage for gallbladder empyema. Diagn Imaging 1980;49:330–3. [PubMed] [Google Scholar]
- [4].Miura F, Takada T, Strasberg SM, et al. TG13 flowchart for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 2013;20:47–54. [DOI] [PubMed] [Google Scholar]
- [5].Chawla A, Bosco JI, Lim TC, et al. Imaging of acute cholecystitis and cholecystitis-associated complications in the emergency setting. Singap Med J 2015;56:438–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Jackson TD, Wannares JJ, Lancaster RT, et al. Does speed matter? The impact of operative time on outcome in laparoscopic surgery. Surg Endosc 2011;25:2288–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Procter LD, Davenport DL, Bernard AC, et al. General surgical operative duration is associated with increased risk-adjusted infectious complication rates and length of hospital stay. J Am Coll Surgeons 2010;210:60–5. [DOI] [PubMed] [Google Scholar]
- [8].Melloul E, Denys A, Demartines N, et al. Percutaneous drainage versus emergency cholecystectomy for the treatment of acute cholecystitis in critically ill patients: does it matter? World J Surg 2011;35:826–33. [DOI] [PubMed] [Google Scholar]
- [9].Lo HC, Wang YC, Su LT, et al. Can early laparoscopic cholecystectomy be the optimal management of cholecystitis with gallbladder perforation? A single institute experience of 74 cases. Surg Endosc 2012;26:3301–6. [DOI] [PubMed] [Google Scholar]
- [10].Sanjay P, Mittapalli D, Marioud A, et al. Clinical outcomes of a percutaneous cholecystostomy for acute cholecystitis: a multicentre analysis. HPB (Oxford) 2013;15:511–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Mizrahi I, Mazeh H, Yuval JB, et al. Perioperative outcomes of delayed laparoscopic cholecystectomy for acute calculous cholecystitis with and without percutaneous cholecystostomy. Surgery 2015;158:728–35. [DOI] [PubMed] [Google Scholar]
- [12].Kim HO, Son BH, Yoo CH, et al. Impact of delayed laparoscopic cholecystectomy after percutaneous transhepatic gallbladder drainage for patients with complicated acute cholecystitis. Surg Laparosc Endosc Percutan Tech 2016;19:20–4. [DOI] [PubMed] [Google Scholar]
- [13].Bickel A, Hoffman RS, Loberant N, et al. Timing of percutaneous cholecystostomy affects conversion rate of delayed laparoscopic cholecystectomy for severe acute cholecystitis. Surg Endosc 2016;30:1028–33. [DOI] [PubMed] [Google Scholar]
- [14].Mok KWJ, Reddy R, Wood F, et al. Is C-reactive protein a useful adjunct in selecting patients for emergency cholecystectomy by predicting severe/gangrenous cholecystitis? Int J Surg 2014;12:649–53. [DOI] [PubMed] [Google Scholar]
- [15].Ambe PC, Papadakis M, Zirngibl H. A proposal for a preoperative clinical scoring system for acute cholecystitis. J Surg Res 2016;200:473–9. [DOI] [PubMed] [Google Scholar]
- [16].Wevers KP, van Westreenen HL, Patijn GA. Laparoscopic cholecystectomy in acute cholecystitis: C-reactive protein level combined with age predicts conversion. Surg Laparosc Endosc Percutan Tech 2013;23:163–6. [DOI] [PubMed] [Google Scholar]
- [17].Barak O, Elazary R, Appelbaum L, et al. Conservative treatment for acute cholecystitis: clinical and radiographic predictors of failure. Isr Med Assoc J 2009;11:739–43. [PubMed] [Google Scholar]


