Abstract
A cross-sectional serosurvey was performed to identify environmental features or practices of dairy farms associated with risk for exposure to vaccinia-like viruses in dairy cattle in Brazil. Sera from 103 cows from 18 farms in Minas Gerais state were examined for Orthopoxvirus-neutralizing antibodies. A database of 243 binary or multiple-selection categorical variables regarding the physical features and surrounding ecology of each property was obtained. Thirteen of 46 presumptive predictor variables were found to be significantly associated with Orthopoxvirus serostatus by univariate logistic regression methods. Use of teat sanitizer and having felids on the property were independently associated with virus exposure by multivariable analysis. Rodents have long been suspected of serving as maintenance reservoirs for vaccinia-like viruses in Brazil. Therefore, domestic felids are not only effective predators of small rodent pests, but also their urine can serve as a deterrent to rodent habitation in buildings such as stables and barns. These results corroborate previous evidence of the high significance of rodents in the Vaccinia virus transmission cycle, and they also raise questions regarding the common use of teat sanitizers in dairy production areas.
Keywords: Bovid, bovine vaccinia, cowpox, dairy, epidemiology, Orthopoxvirus, risk factor, vaccinia
Introduction
Vaccinia virus (VACV) has been described in wild environments in Brazil since 1965 [1], [2]; reports of VACV isolation from wild rodents [1] and from sentinel mice exposed to wild environments [1], [2] suggest that VACV circulates naturally in the country. Reports of zoonotic outbreaks of bovine vaccinia (BV), however, date from the year 2000. Damaso et al. [3] described BV outbreaks from 1999 in Rio de Janeiro state. Since then, VACV outbreaks have been recurrent in agricultural areas throughout Brazil [4]. Minas Gerais state accounts for nearly all of the outbreaks reported annually [4]. It is the largest dairy-producing state in Brazil, having undergone a substantial expansion in production (25%, or ∼1400 tons, of milk produced) during the 8-year period from 1998 to 2006 (Embrapa Dairy Cattle, http://www.cnpgl.embrapa.br/).
A genetically diverse set of vaccinia isolates has been recovered during these outbreaks and from related biological surveys aimed at virus discovery [5], [6], [7], [8], [9], [10], [11], [12], [13], [14], [15], [16]. Some strains have been observed to persist in different regions across years and even decades [17], suggesting that environmental conditions which favor the circulation and maintenance of these viruses exist across broad swaths of the country. Prior studies have demonstrated the presence of vaccinia-like viruses and/or genus Orthopoxvirus (OPV)-neutralizing antibodies in different species of small mammals (rodent, marsupial, procyonid, nonhuman primates) and some domestic animals (felid, canid, equid) sampled near farms or in regions affected by BV [18], [19].
Speculation about the origin and emergence of VACV strains has pointed towards either the escape of so-called feral smallpox vaccine strains [3], [20] or the emergence of resident ancestral strains [6], [7], [14], [21], [22]. Neither hypothesis has been wholly successful at explaining the range of lineages observed, some with genetic similarities to historic smallpox vaccine strains and others without these similarities. However, the circumstances of contemporary BV outbreaks have been similar in that they occur mainly on small-size (<30 milk cows) to midsize (30–100 milk cows) dairy farms, which have typically used traditional hand-milking practices [4].
During outbreaks, infections are commonly noted on the teats and udders of milk cows, the hands and forearms of farm workers (milkers) and occasionally on the muzzles of suckling calves [4]. In bovids, infections range in severity from relatively benign to serious; morbidity can be extensive in very young animals [9], [10], [23]. A similar range of severity has been seen in humans, with the most significant infections leading to hospitalization [9], [10]. In humans, infectious virus can be transmitted from one person to another, and transmission to contacts is a concern in household and healthcare settings [4], [16], [24].
Studies have shown a decrease in 90% of milk production in BV-affected cows [4]. Affected milkers are frequently unable to work because of the pain and malaise caused by VACV infection; a minimum of 7 consecutive days are taken to recover, assuming that secondary infections and/or second sites of VACV multiplication (produced by self-infection) are avoided [4]. BV is also among the differential diagnoses of mouth-and-foot disease, which itself represents economic, social and political issues throughout Brazil [4].
BV outbreaks in Brazil usually occur during the winter dry period (May to August). This observation suggests that specific seasonal features of the environment or ecology may influence the manner in which vaccinia viruses are introduced on farms [4]. Seasonal variation in the population sizes and behaviours of potential reservoir species (including peridomestic and wild animal species) could influence contact patterns between these species and domestic bovids [18]. Alternatively, seasonal variations in grazing, type of supplemental feed or animal housing could affect the timing and frequency of bovid exposure to circulating VACV [18], [25]. However, a comprehensive survey of property characteristics and farming practices related to risk for BV has not been conducted.
To date, VACV is the only OPV proven to circulate naturally in Brazil [4]. Despite the antigenic cross-reactivity among OPV species, which precludes virus species–specific serologic testing [26], VACV has been the single OPV isolated or detected by molecular approaches in the country. National studies from which samples were collected during the acute phase of OPV infections and are positive for OPV antibodies are frequently positive for VACV isolation and/or detection of DNA fragments [3], [6], [27]. Virus isolation or molecular identification of VACV in samples collected from animals which no longer exhibit clinical signs is only rarely possible [4]. Positive serology—e.g. plaque-reduction neutralization test (PRNT)—plus consistent epidemiologic and clinical information are strongly suggestive of previous contact with VACV. The most appropriate term for serology-restricted diagnosis is, however, as we found, a contact with vaccinia-like viruses.
The purpose of this study was to identify environmental features of dairy farms or farming practices that are associated with the risk of dairy cows' exposure to vaccinia-like viruses. To accomplish this, we performed a cross-sectional serosurvey among dairy cows in areas with a history of outbreaks, sampling animals from farms of different sizes, with different environments and/or work practices.
Material and Methods
Description of study location and clinical specimens
The investigation was performed in rural communities of Minas Gerais state, southern Brazil. Most farms are relatively small (average of 57 ha) with natural or cultivated pastures over most of the terrain, and with minor stands of sugarcane, elephant grass, maize or sorghum silage and native vegetation covering the remaining area; this last corresponds to at least 20% of each farm's territory.
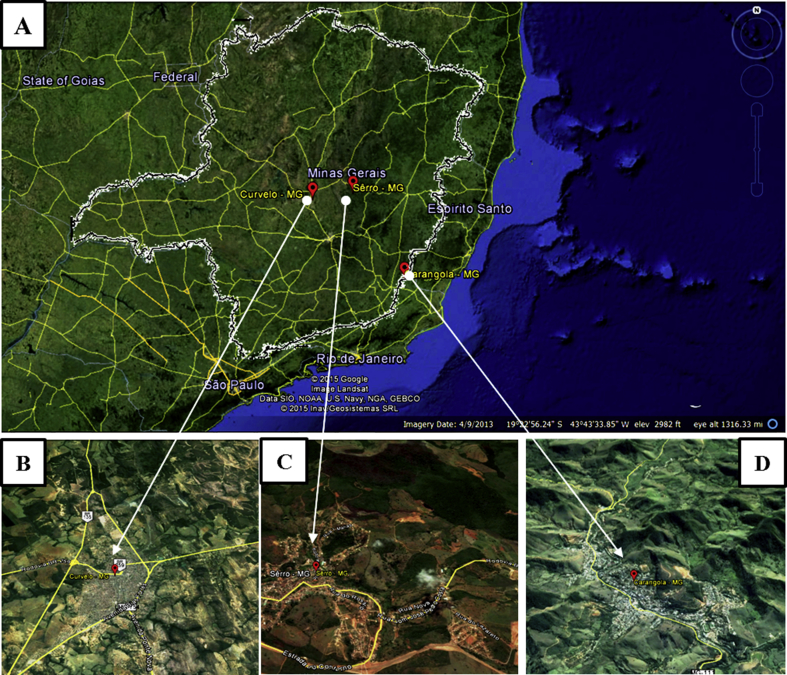
Over the course of eight field visits which took place from June 2010 to February 2012, 18 dairy farms within the Minas Gerais municipalities of Serro (ten farms), Curvelo (seven farms), and Carangola (one farm) were visited by investigators (Fig. 1). One property in Carangola [16] and two in Serro [13] had recently—approximately 1 month before our visit—experienced a documented zoonotic outbreak of BV, but all farms were located in areas with a history of BV outbreaks [4].
Fig. 1.
Overview of Minas Gerais state, Brazil. (A) Extended view of locations of properties surveyed during course of this investigation (red markers indicate vicinity). (B), (C) and (D) are closer landscapes and demonstrate, respectively, municipalities of Curvelo, Serro and Carangola. (Google Earth, 2015).
Farms were selected by convenience sampling among properties that had reliable phone service and which were willing to participate. For three farms, the confirmed occurrence of a prior BV outbreak instigated their inclusion into the study. None of these three farms or the other 15 farmers had animals with clinical evidence of OPV acute infection during sampling.
Written consent was obtained from farm owners or responsible employees to obtain biological specimens from cows maintained on the farm. Sera were collected from a minimum of 10% of the dairy herd (http://www.bibliotecadigital.ufmg.br/dspace/bitstream/handle/1843/BUOS-8FGG7X/tese_de_doutorado_de_marieta_cristina_madureira.pdf?sequence=1)—i.e. productive dairy cows. Cows were selected to be sampled only on the basis of their active milk production; once a cow was being milked, it was susceptible to being randomly chosen. They were all sampled during milking to facilitate our approach and to reduce stress on the animal. Collected sera were tested for the presence of neutralizing anti-OPV antibodies.
Collection of environmental data and husbandry information
A standardized data-collection questionnaire was used to record information from each property detailing the animal husbandry and dairy production practices used by the farm (e.g. breeds of cattle kept, cattle feed, utilization of mechanized vs. manual milking, forms of lactation stimulation), the physical features of the property (e.g. type of corral, pasture characteristics, presence of other domestic animals) and the general features of the surrounding ecology (e.g. water sources, nondomestic animals seen on property). Observable physical features were recorded by an investigator. The property owner or farm manager was asked to answer questions about husbandry and production practices and to supply information about sightings of peridomestic or wild animals on the property. Observations and responses were entered into a database as 243 binary or multiple-selection categorical variables.
Laboratory testing
As a result of the absence of outbreaks during sampling, PRNT (rather than PCR or culture) was selected as the method to assess vaccinia-like virus exposure among the dairy cows. PRNT-positive results were considered related to prior vaccinia-like virus exposure.
PRNT was executed according to Newman et al. [28]. Briefly, six-well plates with BSC-40 cell monolayers (CRL-2761; American Type Culture Collection (ATCC), Manassas, VA, USA) were inoculated with a 2.5% (or 1:40) serum solution plus 150 plaque-forming units (PFU) of VACV strain Western Reserve (WR) per well. Before infection, sera/WR solutions were incubated overnight at 37°C. To maintain the viability of the virus control, fetal bovine serum (FBS) was added to this solution at the same concentration (2.5%). Cell-only control also contained 2.5% of FBS. After infection, 1 hour of adsorption was followed by the addition of 2 mL of 1% FBS media per well, with incubation at 37°C and an atmosphere of 5% CO2 for approximately 48 hours. After typical VACV-WR cytopathic effects were clearly observed, all monolayers were fixed with 3.7% formaldehyde and stained with 1% crystal violet.
All samples were tested in triplicate, and the number of PFUs in each well was enumerated. Positive sera (positive for neutralizing OPV antibodies) were defined as those samples that had PFU below 50% PFU of the viral control.
Data analysis
Characteristics of the bovine herd, milking procedures, nutrition, breeding, silage and farm ecology were examined for univariable association with serum-neutralization capacity; odds ratios (ORs) and 95% confidence intervals (CIs) were calculated by modelling the number of seropositive dairy cows tested per farm by using logistic regression and generalized estimation equation methodology to account for farm-level seropositivity correlations [29], [30], [31]. Characteristics significantly associated with dairy cow seropositivity in a univariate analysis (p <0.10) were considered in a multivariable logistic regression model. Backwards elimination was used, and predictor variables remained significant in the model at p <0.05; variables were tested for multicollinearity using statistical clustering before selected for final inclusion in a multivariate model. All analyses were performed by SAS 9.3 software (SAS Institute, Cary, NC, USA).
Results
Questionnaires were administered and bovine serosurveys were performed at 18 properties across three municipalities. Two-thirds (n = 12) of the properties produced only dairy and were not engaged in meat production, and most (n = 11) were relatively small operations with fewer than 50 milk cows. The median number of dairy cows per property was 38 (mean 41), with the number per farm ranging from as few as eight to as many as 100.
No association was observed between the number of milk cows on the property and the use of manual or mechanized systems for milk extraction. One property with eight milk cows used a mechanized system for milk collection, whereas two other properties with 77 and 50 milk cows relied on traditional manual methods. Methods used to stimulate milk ejection were also not directly correlated with the process used for milking (manual vs. mechanical) or the size of the operation. Four operations that used mechanized milking procedures, including one operation with >50 milk cows, reported the use of traditional means of inducing milk ejection (restricted suckling, conditioning) rather than injected oxytocin.
Some form of sanitization to clean teats before and/or after milking was observed both in mechanical and manual milking operations; independent of the operation practiced, however, not all farms used sanitization. The most used method consisted of an inverted cone-shaped dipping device containing iodine or chlorine solutions of 0.5% and 0.6%, respectively, which were reused from one animal to the next.
Most properties that we queried (n = 15) used one or multiple forms of rodent control (poison, cat and/or trap), either intermittently (n = 8) or permanently (n = 7). Despite the 100% negative response for the item “Presence of small rodents at the corral,” mice faeces and other indicators of their presence were recorded by the investigators during the samplings.
The total number of dairy cows on the 18 properties was 745. Sera were collected from 103 (13.8%) of the animals. Sera were analysed for the presence of OPV-neutralizing antibodies by PRNT. In all, 78 (75.7%) were PRNT-positive cows. All properties but one had at least one PRNT-positive cow. The percentage and absolute number of PRNT-positive cows per property (among those tested) ranged from 20% (n = 1) to 100% (n = 10). All eight animals with a laboratory-confirmed (PCR) history of BV (in prior years) were PRNT positive; an additional 70 animals with no history of BV were also PRNT positive.
Of the 46 presumptive predictor variables assessed, ten were found to be associated (either positively or negatively) with PRNT-positive status (p ≤ 0.050). These variables were the presence of domestic equids (e.g. horses) or domestic felids (e.g. cats); the observation of small rodents around domestic areas, in pastures, in crops or some combination of these; the existence of local dams and springs; the milking type practiced (mechanical vs. manual); the use of udder sanitizer and artificial insemination; BV history confirmed by laboratory analysis; and the use of cattle manure as fertilizer when planting corn (Table 1). An additional two variables—the presence of deer and feeding cattle with sugarcane—were weakly associated with serostatus (p≤0.10) (Table 1).
Table 1.
Univariate analysis results of characteristics significantly associated with bovine seropositivity
| Serology of dairy cows, n (%) |
||||||
|---|---|---|---|---|---|---|
| No. | Variable | Occurrence | PRNT positive | PRNT negative | 95% CI | p |
| 1 | Presence of bats | Yes | 59 (72%) | 23 (28%) | 0.27 (0.06–1.31) | 0.1044 |
| No | 19 (90%) | 2 (9.5%) | ||||
| 2 | Presence of capybaras | Yes | 46 (81%) | 11 (19%) | 1.83 (0.56–5.98) | 0.3176 |
| No | 32 (70%) | 14 (30%) | ||||
| 3 | Presence of deera | Yes | 20 (61%) | 13 (39%) | 0.32 (0.09–1.17) | 0.0855 |
| No | 58 (83%) | 12 (17%) | ||||
| 4 | Presence of hares | Yes | 57 (74%) | 20 (26%) | 0.68 (0.24–1.90) | 0.4598 |
| No | 21 (81%) | 5 (19%) | ||||
| 5 | Presence of possums | Yes | 59 (73%) | 22 (27%) | 0.42 (0.09–2.10) | 0.2934 |
| No | 19 (86%) | 3 (14%) | ||||
| 6 | Presence of small nonhuman primates | Yes | 45 (73%) | 17 (27%) | 0.64 (0.16–2.50) | 0.5227 |
| No | 33 (80%) | 8 (20%) | ||||
| 7 | Presence of wild canids | Yes | 64 (74%) | 23 (26%) | 0.40 (0.12–1.30) | 0.1282 |
| No | 14 (88%) | 2 (13%) | ||||
| 8 | Presence of wild felids | Yes | 43 (75%) | 14 (25%) | 0.97 (0.30–3.15) | 0.9533 |
| No | 35 (76%) | 11 (24%) | ||||
| 9 | Presence of domestic equidsb | Yes | 69 (78%) | 19 (22%) | 2.42 (1.20–4.87) | 0.0131 |
| No | 9 (60%) | 6 (40%) | ||||
| 10 | Presence of domestic small ruminants | Yes | 4 (50%) | 4 (50%) | 0.28 (0.06–1.32) | 0.1085 |
| No | 74 (78%) | 21 (22%) | ||||
| 11 | Presence of poultry | Yes | 60 (77%) | 18 (23%) | 1.30 (0.26–6.58) | 0.7542 |
| No | 18 (72%) | 7 (28%) | ||||
| 12 | Presence of swine | Yes | 28 (74%) | 10 (26%) | 0.84 (0.25–2.81) | 0.7775 |
| No | 50 (77%) | 15 (23%) | ||||
| 13 | Presence of domestic felidsb | Yes | 40 (63%) | 24 (38%) | 0.04 (0.01–0.37) | 0.0039 |
| No | 38 (97%) | 1 (2.6%) | ||||
| 14 | Presence of small rodents at domestic areasb | Yes | 75 (78%) | 21 (22%) | 4.76 (2.34–9.70) | < .0001 |
| No | 3 (43%) | 4 (57%) | ||||
| 15 | Presence of small rodents at pastures and/or cropsb | Yes | 21 (95%) | 1 (4.5%) | 8.84 (1.13–69.39) | 0.0381 |
| No | 57 (70%) | 24 (30%) | ||||
| 16 | Presence of small-rodent poison control | Yes | 52 (73%) | 19 (27%) | 0.63 (0.23–1.75) | 0.3777 |
| No | 26 (81%) | 6 (19%) | ||||
| 17 | Existence of dams (min. 1)b | Yes | 61 (85%) | 11 (15%) | 4.57 (1.35–15.49) | 0.0148 |
| No | 17 (55%) | 14 (45%) | ||||
| 18 | Existence of rivers (min. 1) | Yes | 20 (67%) | 10 (33%) | 0.52 (0.13–2.00) | 0.3401 |
| No | 58 (79%) | 15 (21%) | ||||
| 19 | Existence of springs (min. 1)b | Yes | 64 (80%) | 16 (20%) | 2.57 (1.01–6.55) | 0.0476 |
| No | 14 (61%) | 9 (39%) | ||||
| 20 | Existence of streams (min. 1) | Yes | 55 (80%) | 14 (20%) | 1.88 (0.61–5.81) | 0.2733 |
| No | 23 (68%) | 11 (32%) | ||||
| 21 | Type of corral floor | Dirt | 7 (64%) | 4 (36%) | 0.52 (0.09–2.86) | 0.4497 |
| Concrete | 71 (77%) | 21 (23%) | ||||
| 22 | Corral cleaning | Weekly | 8 (57%) | 6 (43%) | 0.36 (0.10–1.29) | 0.1161 |
| Daily | 70 (79%) | 19 (21%) | ||||
| 23 | Sanitizer use for corral cleaning | Yes | 12 (63%) | 7 (37%) | 0.47 (0.06–3.80) | 0.4769 |
| No | 66 (79%) | 18 (21%) | ||||
| 24 | Cattle type | Milk and meat | 20 (69%) | 9 (31%) | 0.61 (0.18–2.07) | 0.4315 |
| Milk | 58 (78%) | 16 (22%) | ||||
| 25 | Milking typeb | Mechanical | 67 (82%) | 15 (18%) | 4.06 (1.14–14.50) | 0.0309 |
| Manual | 11 (52%) | 10 (48%) | ||||
| 26 | Milking device semestral maintenance | Yes | 55 (80%) | 14 (20%) | 0.33 (0.03–3.30) | 0.3434 |
| No | 12 (92%) | 1 (7.7%) | ||||
| 27 | Hand sanitizers for milking | Yes | 46 (81%) | 11 (19%) | 1.83 (0.53–6.37) | 0.3423 |
| No | 32 (70%) | 14 (30%) | ||||
| 28 | Milking line based on pathologies | Yes | 68 (76%) | 22 (24%) | 0.93 (0.12–7.16) | 0.9423 |
| No | 10 (77%) | 3 (23%) | ||||
| 29 | Udder sanitizerb | Yes | 66 (83%) | 14 (18%) | 4.32 (1.27–14.66) | 0.0189 |
| No | 12 (52%) | 11 (48%) | ||||
| 30 | Artificial oxytocin | Yes | 51 (84%) | 10 (16%) | 2.83 (0.81–9.92) | 0.1034 |
| No | 27 (64%) | 15 (36%) | ||||
| 31 | Artificial inseminationb | Yes | 48 (87%) | 7 (13%) | 4.11 (1.40–12.07) | 0.0100 |
| No | 30 (63%) | 18 (38%) | ||||
| 32 | >10 L of milk per cow per day | Yes | 48 (80%) | 12 (20%) | 1.73 (0.49–6.07) | 0.3898 |
| No | 30 (70%) | 13 (30%) | ||||
| 33 | Lesion on calf muzzle | Yes | 7 (70%) | 3 (30%) | 1.33 (0.11–15.97) | 0.8203 |
| No | 7 (64%) | 4 (36%) | ||||
| 34 | Respondent knows about BV | Yes | 63 (78%) | 18 (22%) | 1.63 (0.54–4.95) | 0.3857 |
| No | 15 (68%) | 7 (32%) | ||||
| 35 | Lab-confirmed BV historyb | Yes | 8 (100%) | 0 (0.0%) | 0.13 (0.04–0.39) | 0.0003 |
| No | 70 (74%) | 25 (26%) | ||||
| 36 | Cattle fed after milking | Yes | 26 (84%) | 5 (16%) | 1.16 (0.26–5.22) | 0.8459 |
| Dry season | 20 (74%) | 7 (26%) | ||||
| No | 32 (71%) | 13 (29%) | ||||
| 37 | Cattle manure use for pastures | Yes | 44 (79%) | 12 (21%) | 1.40 (0.43–4.59) | 0.5765 |
| No | 34 (72%) | 13 (28%) | ||||
| 38 | Cattle manure use for grass | Yes | 67 (75%) | 22 (25%) | 0.83 (0.09–7.71) | 0.8703 |
| No | 11 (79%) | 3 (21%) | ||||
| 39 | Cattle manure use for planting cornb | Yes | 7 (39%) | 11 (61%) | 0.13 (0.04–0.39) | 0.0003 |
| No | 71 (84%) | 14 (16%) | ||||
| 40 | Cattle fed with grass | Yes | 44 (71%) | 18 (29%) | 0.50 (0.14–1.85) | 0.3015 |
| No | 34 (83%) | 7 (17%) | ||||
| 41 | Cattle fed with sugarcanea | Yes | 43 (68%) | 20 (32%) | 0.31 (0.09–1.11) | 0.0708 |
| No | 35 (88%) | 5 (13%) | ||||
| 42 | Cattle fed with silage | Yes | 48 (80%) | 12 (20%) | 1.73 (0.55–5.48) | 0.3491 |
| No | 30 (70%) | 13 (30%) | ||||
| 43 | Grain used for silage | Yes | 32 (82%) | 7 (18%) | 1.43 (0.36–5.67) | 0.6121 |
| No | 16 (76%) | 5 (24%) | ||||
| 44 | Grass used for silage | Yes | 45 (80%) | 11 (20%) | 1.36 (0.56–3.31) | 0.4930 |
| No | 3 (75%) | 1 (25%) | ||||
| 45 | Cattle fed with ration | Yes | 72 (77%) | 22 (23%) | 1.64 (0.29–9.20) | 0.5762 |
| No | 6 (67%) | 3 (33%) | ||||
| 46 | Adult cattle fed with its own milk or whey | Yes | 29 (78%) | 8 (22%) | 1.26 (0.35–4.54) | 0.7263 |
| No | 49 (74%) | 17 (26%) | ||||
CI, confidence interval; min, minimum; OPV, genus Orthopoxvirus; PRNT, plaque-reduction neutralization test.
Variables not among the top ten most correlated variables with OPV seropositivity but still considered strongly correlated (p <0.1).
Ten most correlated variables with OPV seropositivity (p <0.05).
Multivariable logistic regression analysis using the 12 significantly associated (p <0.10) variables resulted in identification of two property practices or features which were independently associated with serostatus (Table 2). Taking other factors into account, the presence of domestic felids on a property was significantly associated with diminished odds of a cow having OPV-neutralizing antibody (OR, 0.03; 95% CI, 0.005–0.18). Cows on properties that used udder sanitizers had greater odds of having OPV-neutralizing antibody (OR, 7.45; 95% CI, 3.71–15.01) (Table 2).
Table 2.
Univariate analysis results of characteristics independently associated with bovine seropositivity
| Characteristic | Odds ratio (95% confidence interval) | p |
|---|---|---|
| Domestic felids (cats) | 0.03 (0.005–0.18) | 0.0002 |
| Teat sanitizer use | 7.45 (3.71–15.01) | < 0.0001 |
Discussion and Conclusion
With this study, we sought to gain insight both into how the viruses that cause BV enter farm environments and how they then spread between cows and people. Our approach was to assess production practices and property characteristics across a variety of property types, then to relate that information to an individual animal's risk for exposure to BV (using the presence of OPV-neutralizing antibodies as a proxy for exposure). The properties surveyed during this study varied in size and relative sophistication; they generally represented the range of farm types found in Minas Gerais state, Brazil [4]. One property characteristic in particular, the presence of domestic cats, was noted to be independently associated with a diminished probability of BV exposure, while the use of teat sanitization (‘dipping’) was shown to be independently associated with elevated risk.
An unanticipated finding from this investigation was the high proportion (75.7%) of animals that were found to have antibody capable of neutralizing VACV when diluted 1:40 (PRNT-positive cows considered to have had prior vaccinia-like exposure). Only eight of the 78 cows that tested positive had a confirmed history of BV illness. In a 2011 study performed in an area of neighbouring Sao Paulo state that had experienced outbreaks of BV, a much smaller proportion of animals (38.8%) had vaccine-neutralizing antibodies [12]. In that study, however, only 12 (25%) of 48 of the properties surveyed used mechanized milking practices, whereas in our study, the number of properties using mechanized milking was substantially higher (11/17, 61%). In our study, the practice of mechanized milking was strongly collinear with that of the use of teat sanitizer, the latter of which was independently associated with BV exposure. From an analytic perspective, the two practices were integrally related, and in practice both or either could inadvertently perpetuate the risk of virus exposure among bovids. For example, dipping devices, which are typically filled with iodine or chlorine, may be only partially effective in deactivating VACV and may therefore be inadequate at ensuring sanitization of teats from one cow to the next [32]. Alternatively, the lack of adherence to proper cleaning of mechanical milk extractors from one cow to the next could perpetuate virus transmission. Abnormal vacuum pressure or vacuum/massage ratio within these mechanical extractors may also cause lesions at the teats, compromising the elasticity of their sphincters and therefore facilitating further infections.
Another practice becoming increasingly common as dairy operations increase in sophistication is the use of injected hormone (oxytocin) to stimulate milk ejection. Needle reuse between animals is commonplace, which introduces repeated opportunities for contamination of multidose hormone vials and exposure of vaccinia-like viruses to animals. The use of injectable hormone was associated with BV exposure (OR, 2.83; 95% CI, 0.81–9.92), and it is tempting to hypothesize that the sort of broad-scale, low-level exposure to vaccinia-like viruses that could be engendered by reuse of a syringe between animals could also in part account for the high seroprevalence observed, particularly in the absence of overt disease. Effectively, animals may be being immunized against parenteral infection, thus providing them with some protection against severe disease. This hypothesis bears further scrutiny.
The presence of domestic cats on properties in this study was independently associated with significantly diminished odds of a cow having OPV-neutralizing antibodies (OR, 0.03; 95% CI, 0.005–0.18). Rodents have long been suspected of serving as maintenance reservoirs for vaccinia-like viruses in Brazil [1], [2], [18]. Domestic felids are not only effective predators of small rodent pests, but also their urine can serve as a deterrent to rodent habitation of buildings such as stables and barns [33]. It therefore makes intuitive sense that the presence of cats on a property mitigates against virus introduction onto a farm via a rodent host.
It is worth noting that Brazil has no reports of felids with clinical signs of OPV infection, in contrast to what has been observed for Cowpox virus (OPV species) in Europe [34], where domestic cats play a prominent role in the transmission of Cowpox virus to humans. OPV PRNT-positive felids, on the other hand, have been reported [35]; the importance of this finding needs to be further investigated, as does the presence of small rodents in farms with profiles similar to the farms we investigated here. The presence of small rodents at domestic areas was indeed associated with a higher number of cows positive for OPV-neutralizing antibodies (OR, 4.76%; 95% CI, 2.34–9.70); however, evidence suggesting the presence of mice or other small rodents was frequently observed on corrals evaluated during this study when their presence was verbally denied by the farm owner. With all that in mind, ecology studies are underway on a limited number of properties where the attempt to capture small rodents has been authorized.
As dairy production becomes increasingly standardized throughout Brazil with the introduction of mechanized milking practices, previously predictable patterns of BV occurrence will almost certainly change. Whether changing practices will result in the interruption of BV exposure and less frequent outbreaks, or whether something entirely unanticipated may come into play (e.g. increased prevalence of animal exposure due to inadequate sanitary precautions during milking and injections) remains to be seen. Until then, the impact of this zoonosis on animal and human health will continue to be a concern for producers, dairy workers and consumers of dairy products in Brazil. The introduction of domestic cats onto properties to reduce the exposure of bovids to vaccinia-like viruses, as well as further investigation of sanitizers and sanitization devices currently in use are therefore interesting actions to take to minimize this impact. These conclusions are limited by the relatively small number of farms under observations. We recommend further studies of larger scope to refine our understanding of on-farm risks for BV.
Acknowledgements
We thank Capes, CNPq, FAPEMIG, MAPA and CDC for financial support. We thank IMA for greatly facilitating our fieldwork. We also thank all owners and managers who voluntarily joined our study, providing us with their precious time, information, animals and pleasant cups of coffee to warm our mornings or to prepare us for an afternoon journey. EGK, GST and JSA are CNPq fellowship recipients.
Conflict of Interest
None declared. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the funding agencies.
References
- 1.Lopes O.S., Lacerda J.P., Fonseca I.E., Castro D.P., Forattini O.P., Rabello E.X. Cotia virus: a new agent isolated from sentinel mice in Sao Paulo, Brazil. Am J Trop Med Hyg. 1965;14:156–157. doi: 10.4269/ajtmh.1965.14.156. [DOI] [PubMed] [Google Scholar]
- 2.da Fonseca F.G., Trindade G.S., Silva R.L., Bonjardim C.A., Ferreira P.C., Kroon E.G. Characterization of a vaccinia-like virus isolated in a Brazilian forest. J Gen Virol. 2002;83:223–228. doi: 10.1099/0022-1317-83-1-223. [DOI] [PubMed] [Google Scholar]
- 3.Damaso C.R., Esposito J.J., Condit R.C., Moussatche N. An emergent poxvirus from humans and cattle in Rio de Janeiro State: Cantagalo virus may derive from Brazilian smallpox vaccine. Virology. 2000;277:439–449. doi: 10.1006/viro.2000.0603. [DOI] [PubMed] [Google Scholar]
- 4.Kroon E.G., Mota B.E., Abrahão J.S., da Fonseca F.G., de Souza Trindade G. Zoonotic Brazilian Vaccinia virus: from field to therapy. Antiviral Res. 2011;92:150–163. doi: 10.1016/j.antiviral.2011.08.018. [DOI] [PubMed] [Google Scholar]
- 5.Nagasse-Sugahara T.K., Kisielius J.J., Ueda-Ito M., Curti S.P., Figueiredo C.A., Cruz A.S. Human vaccinia-like virus outbreaks in São Paulo and Goiás States, Brazil: virus detection, isolation and identification. Rev Inst Med Trop. 2004;46:315–322. doi: 10.1590/s0036-46652004000600004. [DOI] [PubMed] [Google Scholar]
- 6.Trindade G.S., Lobato Z.I.P., Drumond B.P., Leite J.A., Trigueiro R.C., Guedes M.I. Short report: isolation of two Vaccinia virus strains from a single bovine vaccinia outbreak in rural area from Brazil: implications on the emergence of zoonotic orthopoxviruses. Am J Trop Med Hyg. 2006;75:486–490. [PubMed] [Google Scholar]
- 7.Trindade G.S., Emerson G.L., Carroll D.S., Kroon E.G., Damon I.K. Brazilian vaccinia viruses and their origins. Emerg Infect. 2007;13:965–972. doi: 10.3201/eid1307.061404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Megid J., Appolinario C.M., Langoni H., Pituco E.M., Okuda L.H. Vaccinia virus in humans and cattle in southwest region of Sao Paulo state, Brazil. Am J Trop Med Hyg. 2008;79:647–651. [PubMed] [Google Scholar]
- 9.Abrahao J.S., Silva-Fernandes A.T., Assis F.L., Guedes M.I., Drumond B.P., Leite J.A. Human Vaccinia virus and pseudocowpox virus co-infection: clinical description and phylogenetic characterization. J Clin Virol. 2010;48:69–72. doi: 10.1016/j.jcv.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 10.Silva D.C., Moreira-Silva E.A., Gomes J.A., Fonseca F.G., Correa-Oliveira R. Signs, diagnosis, and case reports of Vaccinia virus infections. J Infect Dis. 2010;14:129–134. doi: 10.1590/s1413-86702010000200003. [DOI] [PubMed] [Google Scholar]
- 11.Schatzmayr H.G., Costa R.V., Goncalves M.C., D'Andrea P.S., Barth O.M. Human and animal infections by vaccinia-like viruses in the state of Rio de Janeiro: a novel expanding zoonosis. Vaccine. 2011;29:D65–D69. doi: 10.1016/j.vaccine.2011.09.105. [DOI] [PubMed] [Google Scholar]
- 12.Megid J., Borges I.A., Abrahao J.S., Trindade G.S., Appolinario C.M., Ribeiro M.G. Vaccinia virus zoonotic infection, São Paulo State, Brazil. Emerg Infect Dis. 2012;18:189–191. doi: 10.3201/eid1801.110692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Assis F.L., Borges I.A., Ferreira P.C., Bonjardim C.A., Trindade G.S., Lobato Z.I.P. Group 2 Vaccinia virus, Brazil. Emerg Infect Dis. 2012;18:2035–2038. doi: 10.3201/eid1812.120145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Assis F.L., Almeida G.M., Oliveira D.B., Franco-Luiz A.P., Campos R.K., Guedes M.I. Characterization of a new Vaccinia virus isolate reveals the C23L gene as a putative genetic marker for autochthonous group 1 Brazilian Vaccinia virus. PLoS One. 2012;7:e50413. doi: 10.1371/journal.pone.0050413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oliveira D.B., Assis F.L., Ferreira P.C., Bonjardim C.A., de Souza T.G., Kroon E.G. Group 1 Vaccinia virus zoonotic outbreak in Maranhao State, Brazil. Am J Trop Med Hyg. 2013;89:1142–1145. doi: 10.4269/ajtmh.13-0369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.de Assis F.L., Borges I.A., Mesquita V.S., Ferreira P.C., Trindade G.S., Kroon E.G. Vaccinia virus in household environment during bovine vaccinia outbreak, Brazil. Emerg Infect Dis. 2013;19:2045–2047. doi: 10.3201/eid1912.120937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de Assis F.L., Vinhote W.M., Barbosa J.D., de Oliveira C.H., de Oliveira C.M., Campos K.F. Reemergence of Vaccinia virus during zoonotic outbreak, Pará State, Brazil. Emerg Infect Dis. 2013;19:2017–2020. doi: 10.3201/eid1912.130589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Abrahao J.S., Guedes M.I., Trindade G.S., Fonseca F.G., Campos R.K., Mota B.F. One more piece in the VACV ecological puzzle: could peridomestic rodents be the link between wildlife and bovine vaccinia outbreaks in Brazil? PLoS One. 2009;4:e7428. doi: 10.1371/journal.pone.0007428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peres M.G., Bacchiega T.S., Appolinario C.M., Vicente A.F., Allendorf S.D., Antunes J.M. Serological study of Vaccinia virus reservoirs in areas with and without official reports of outbreaks in cattle and humans in São Paulo, Brazil. Arch Virol. 2013;158:2433–2441. doi: 10.1007/s00705-013-1740-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Medaglia M.L., Moussatché N., Nitsche A., Dabrowski P.W., Li Y., Damon I.K. Genomic analysis, phenotype, and virulence of the historical Brazilian smallpox vaccine strain IOC: implications for the origins and evolutionary relationships of Vaccinia virus. J Virol. 2015;89:11909–11925. doi: 10.1128/JVI.01833-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marques J.T., Trindade G.D., da Fonseca F.G., Bonjardim C.A., Ferreira P.C., Kroon E.G. Characterization of ATI, TK and IFN-alpha/betaR genes in the genome of the BeAn 58058 virus, a naturally attenuated wild Orthopoxvirus. Virus Genes. 2001;23:291–301. doi: 10.1023/a:1012521322845. [DOI] [PubMed] [Google Scholar]
- 22.Guedes M.I., Rehfeld I.S., de Oliveira T.M., Assis F.L., Matos A.C., Abrahao J.S. Detection of Vaccinia virus in blood and faeces of experimentally infected cows. Transbound Emerg Dis. 2013;60:552–555. doi: 10.1111/j.1865-1682.2012.01372.x. [DOI] [PubMed] [Google Scholar]
- 23.Rivetti A.V.J., Guedes M.I., Rehfeld I.S., Oliveira T.M., Matos A.C., Abrahao J.S. Bovine Vaccinia, a systemic infection: evidence of fecal shedding, viremia and detection in lymphoid organs. Vet Microbiol. 2013;162:103–111. doi: 10.1016/j.vetmic.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 24.Pereira G.O., Tavares Silva F.A., Lopes de A.F., Augusto A.P., Moreira Franco Luiz A.P., Barcelos F.L. Intrafamilial transmission of Vaccinia virus during a bovine vaccinia outbreak in Brazil: a new insight in viral transmission chain. Am J Trop Med Hyg. 2014;90:1021–1023. doi: 10.4269/ajtmh.13-0621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Assis F.L., Franco-Luiz A.P.M., Paim L.M., Oliveira G.P., Pereira A.F., de Alimeida G.M.F. Horizontal study of Vaccinia virus infections in an endemic area: epidemiologic, phylogenetic and economic aspects. Arch Virol. 2015;160:2703–2708. doi: 10.1007/s00705-015-2549-1. [DOI] [PubMed] [Google Scholar]
- 26.Fenner F., Wittek R., Dumbell K.R. Academic Press; San Diego, CA: 1989. The orthopoxviruses. [Google Scholar]
- 27.Leite J.A., Drummond B.P., Trindade G.S., Lobato Z.I.P., da Fonseca F.G., dos Santos J.R. Passatempo virus, a Vaccinia virus strain, Brazil. Emerg Infect Dis. 2005;11:1935–1941. doi: 10.3201/eid1112.050773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Newman F.K., Frey S.E., Blevins T.P., Mandava M., Bonifacio A.J., Yan L. Improved assay to detect neutralizing antibody following vaccination with diluted or undiluted Vaccinia (Dryvax) vaccine. J Clin Microbiol. 2003;41:3154–3157. doi: 10.1128/JCM.41.7.3154-3157.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Harrell F.E. Springer-Verlag; New York: 2001. Regression modeling strategies with applications to linear models, logistic regression and survival analysis. [Google Scholar]
- 30.Kleinbaum D.G., Klein M.C. 2nd ed. Springer-Verlag; New York: 2002. Logistic regression: a self-learning text. [Google Scholar]
- 31.Liang K.Y., Zeger S.L. Vol. 73. Oxford University Press on behalf of Biometrika Trust; Oxford: 1986. pp. 13–22. (Longitudinal data analysis using generalized linear models). [Google Scholar]
- 32.de Oliveira T.M., Rehfeld I.S., Guedes M.I.C., Ferreira J.M., Kroon E.G., Lobato Z.I.P. Susceptibility of Vaccinia virus to chemical disinfectants. Am J Trop Med Hyg. 2011;85:152–157. doi: 10.4269/ajtmh.2011.11-0144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Voznessenskaya V.V., Malanina T.V. Effect of chemical signals from a predator (Felis catus) on the reproduction of Mus musculus. Dokl Biol. 2013;453:362–364. doi: 10.1134/S0012496613060057. [DOI] [PubMed] [Google Scholar]
- 34.Coras B., Essbauer S., Pfeffer M., Meyer H., Schröder J., Stolz W. Cowpox and a cat. Lancet. 2005, 4;365(9457):446. doi: 10.1016/S0140-6736(05)17836-2. [DOI] [PubMed] [Google Scholar]
- 35.Peres G.P., Barros C.B., Appolinário C.M., Antunes J.M.A.P., Mioni M.S.R., Bacchiega T.S. Dogs and opossums positive for Vaccinia virus during outbreak affecting cattle and humans, São Paulo State, Brazil. Emerg Infect Dis. 2016;22:271–273. doi: 10.3201/eid2202.140747. [DOI] [PMC free article] [PubMed] [Google Scholar]