Abstract
Congenital absence of the left circumflex artery is a rare coronary anomaly with few reported cases in the literature. These patients are usually diagnosed incidentally when they undergo coronary angiography or coronary CT to rule out underlying coronary artery disease. In this article, we report a case of a 46-year-old man who was incidentally found to have a congenitally absent left circumflex artery with a superdominant right coronary artery after a workup was initiated for frequent premature ventricular contractions and regional wall motion on echocardiogram. A review of the clinical presentation, symptoms, and diagnostic modalities used to diagnose this entity is presented.
1. Introduction
Congenital absence of the left circumflex (LCX) artery is a rare coronary anomaly with an incidence of 10 in 1495 (0.0067%) patients [1, 2]. Due to its uncommon nature, diagnosis can be challenging, especially among patients who present with acute cardiac symptoms. It may initially be misdiagnosed as complete occlusion of the left circumflex artery [3]. A better understanding of the natural history and clinical implications of this condition may allow us to diagnose and manage this condition with an algorithmic approach. We present a case of congenitally absent left circumflex artery with a superdominant right coronary artery (RCA) detected by coronary angiography and confirmed by coronary CT. Also, a review of previously published cases in literature and their clinical outcomes is presented.
2. Methods
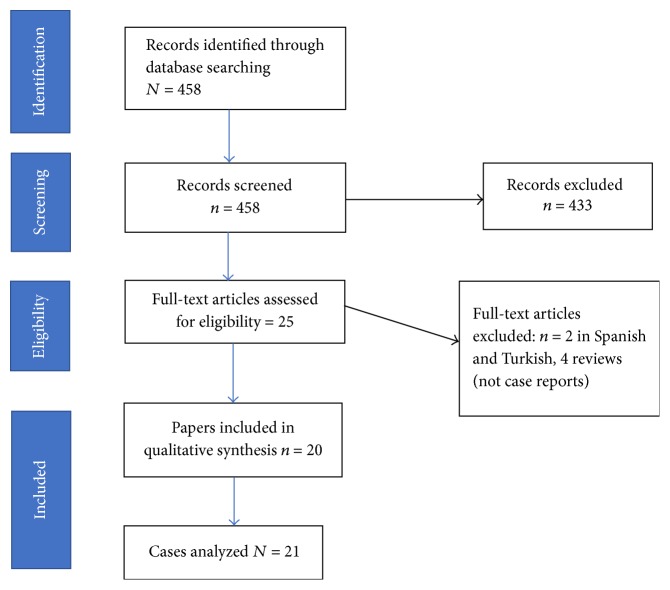
In addition to the present case, a systematic review of case reports/short cases in OVID looking at patients who presented with congenitally absent left circumflex artery was performed. The review only considered papers published in the English language. An electronic search strategy with the keywords Left circumflex AND Absent OR Absence AND Congenital was used. Duration of published papers was defined between and 1946 and October 2016. Definitions used for case-inclusion were (a) age greater than 18 years and (b) diagnosis of left circumflex artery abnormality either by CT/MRI or coronary angiography (Figure 1).
Figure 1.
PRISMA flowchart: data collection and selection of cases.
3. Case Presentation
A 46-year-old man with no significant medical history presented to the emergency department with an episode of transient loss of consciousness after a mechanical fall. He had no preceding chest pain or palpitations. There was no history of syncope, presyncope, loss of consciousness, diabetes, hypertension, or seizure disorder. On admission, vital signs showed heart rate of 88 bpm, BP of 115/83 mmhg, oxygen saturation of 95% on room air, and respiratory rate of 18 cpm. Physical examination was within normal limits including no neurological deficits. Computed tomography of the brain showed normal findings with no evidence of intracerebral hemorrhage. Labs were all within normal limits including a negative troponin.
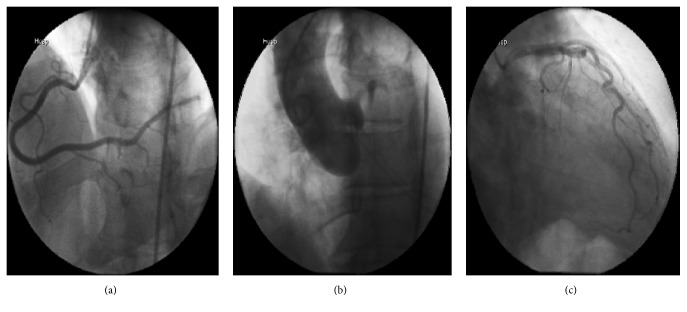
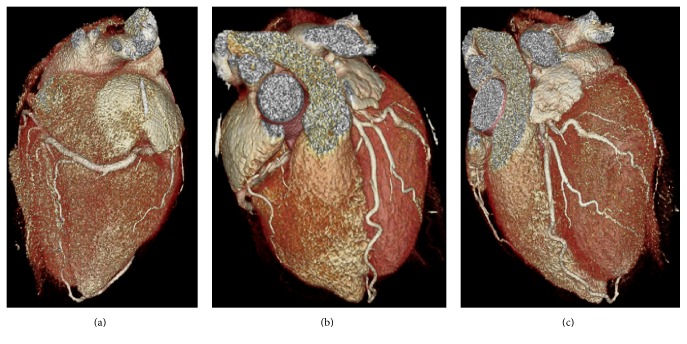
While the patient was being monitored in the emergency department he was noted to be in sinus rhythm with frequent premature ventricular contractions (PVCs). An EKG showed sinus rhythm with T wave inversions in the inferior leads and frequent PVCs. A transthoracic echocardiogram (TTE) revealed a left ventricular ejection fraction (LVEF) of 40–45%, with akinesis of the basal-mid inferior segments. These findings led to a coronary angiogram that showed a very large sized, dominant RCA supplying the entire lateral wall; normal left main and left anterior descending (LAD) arteries; and a congenitally absent left circumflex artery (Figure 2). A subsequent cardiac 64 multislice CT scan confirmed the absence of the LCX and showed an RCA with a large posterolateral artery that supplied the entire lateral wall. The LAD was normal (Figure 3). Given the unexplained regional wall motion abnormality, a cardiac MRI was performed which revealed viable myocardium with no areas of late gadolinium enhancement. The calculated LVEF was 40% on the cardiac MRI; the patient was initiated on metoprolol for his frequent PVCs, appropriate therapy for his systolic dysfunction, and discharged home with primary care and cardiology follow-up. On a subsequent Holter monitor, he continued to have occasional PVCs but no ventricular arrhythmias were detected.
Figure 2.
Coronary angiogram: (a) LAO-CAU view of superdominant RCA, (b) aortic root shot to rule out anomalous origin of the LCX, and (c) RAO caudal view showing absent left circumflex in the AV groove.
Figure 3.
Coronary CT views: (a) left ventricle being supplied by branches of the RCA, (b) LAD in the interventricular groove, and (c) absent left circumflex artery.
4. Literature Review
To the best of our knowledge, 20 cases of absent left circumflex artery have been described in the literature that met our inclusion criteria. Our case is the first to be diagnosed due to workup of occasional PVCs but shared some similarities with previously published reports.
Table 1 summarizes the baseline demographics, comorbidities, presentation findings, and diagnostic modalities for all patients. There were 15 male and 8 female patients with a mean ± SD age of 53 ± 10 years. One out of every three patients did not have any cardiovascular comorbidities, whereas the others had known cardiovascular comorbidities. Of these, the most prevalent were systemic hypertension and a history of tobacco use.
Table 1.
Cases of patients presenting with congenitally absent left circumflex artery.
| Ref | Age | sex | Comorbidities | Chest pain | Diagnostic procedure | MI | Echo/nuclear | Associated anomalies of other vessels |
|---|---|---|---|---|---|---|---|---|
| Ali et al. [4] | 40 | M | DM, HTN, smoking | Exertional pain CP | CATH | Yes | Reduced LV function, with inferior and posterior segments were akinetic, anterior, lateral, and septal segments hypokinesis | Large RCA (70% stenosis) and complete occlusion of LAD → CABG, super dominant RCA |
|
| ||||||||
| Ali et al. [4] | 39 | M | None | Exertional pain CP | CATH | No | NA | Superdominant RCA |
|
| ||||||||
| Varela et al. [3] | 55 | F | None | Nonexertional CP | CATH | No | NA | Superdominant RCA |
|
| ||||||||
| Oliveira et al. [5] | 70 | M | Aortic stenosis | Exertional chest pain, syncope | CATH | No | HFPEF 58%, severe AS area < 0.7 | Superdominant RCA, anomalous origin of left coronary artery from right coronary sinus |
|
| ||||||||
| Duan et al. [6] | 66 | M | Constrictive pericarditis | None | CATH (Pre-op evaluation | No | NA | Superdominant RCA and enlarged LAD branches |
|
| ||||||||
| Guo and Xu [7] | 52 | M | HTN, smoking | Nonexertional CP | CATH + CT | Yes | Echo showed severe hypokinesis of the lateral wall, inferior left ventricular wall thinning and akinesis | Superdominant RCA + RCA thrombus, mid portion of LAD stenosis |
|
| ||||||||
| Quijada-Fumero et al. [8] | 51 | M | DM, HTN, obesity | None (T wave inversions in V3-v6) | CATH | No | Normal LV, no RWMA | Normal LAD, absent LCX, superdominant RCA |
|
| ||||||||
| Lin et al. [9] | 44 | F | None | Exertional CP | CATH | No | Thallium perfusion showed perfusion defects in the septal and inferior walls which normalized in the delayed imaging | Superdominant RCA coronary angiogram |
|
| ||||||||
| Teunissen et al. [10] | 46 | M | None | Exertional CP | CATH | No | Normal LV, no RWMA | Mid segment of LAD was atretic originating from left sinus Valsalva, superdominant right coronary artery |
|
| ||||||||
| Vijayvergiya and Jaswal [11] | 40 | M | None | Nonexertional CP | CATH | No | Normal LV, no RWMA | Superdominant RCA, LAD originated from the right coronary cusps |
|
| ||||||||
| Hongsakul and Suwannanon [12] | 52 | M | HTN, smoking | Exertional CP | CT | Stress test, inconclusive | Superdominant RCA | |
|
| ||||||||
| Majid et al. [13] | 55 | F | HTN | Nonexertional CP | CT | No | NA | Superdominant RCA |
|
| ||||||||
| Hong et al. [14] | 68 | M | HLD | Nonexertional CP | CATH then CT | Yes | NA | Superdominant RCA, with acute thrombosis of RCA |
|
| ||||||||
| Bildirici et al. [15] | 67 | F | HTN | Exertional CP | CATH, Confirmed with aortography | No | Normal EF (NRWMA) | Dual LAD, superdominant RCA |
|
| ||||||||
| Yoon et al. [16] | 48 | M | HTN, chronic alcoholism | Nonexertional CP | CATH | No | LVH with no other abnormality | Superdominant RCA |
|
| ||||||||
| Baskurt et al. [17] | 55 | F | None | Nonexertional CP | CATH, Confirmed with aortography and MDCT (multidetector row Computed tomography) | No | Normal LV, no RWMA | Superdominant RCA |
|
| ||||||||
| Sato et al. [18] | 62 | M | CAD | Exertional CP | Coronary CT/CATH | No | NA | Superdominant RCA |
|
| ||||||||
| Harada et al. [19] | 65 | F | Aortic stenosis | None | CT coronary (Pre-op) | No | NA | Absence of left circumflex and left subclavian |
|
| ||||||||
| Doven et al. [20] | 67 | M | HTN, HLD, smoking | Exertional CP | CATH | No | Normal EF, no RWMA | Superdominant RCA |
|
| ||||||||
| Harada et al. [19] | 49 | M | HTN, HLD | Exertional CP | CATH | Yes | NA | Complete Left main occlusion, absent LCX → treated with PCI |
|
| ||||||||
| Our case | 46 | M | None | None (frequent PVCs and abnormal Echo findings) | CATH | No | Echo-EF of 40–45%, with mild diffuse hypokinesis with RWMA and akinesis in the basal-mid inferior walls | Superdominant RCA |
CATH: coronary angiogram, EF: left ventricular ejection fraction, F: female, HTN: hypertension, LAD: left anterior descending artery, LCX: left circumflex artery, HTN: hypertension, M: male, NA: not available, RCA, right coronary artery, RWMA, regional wall motion abnormalities, STEMI: ST segment elevation MI, and CP: chest pain.
The most common presenting symptom that led to the diagnosis of congenitally absent circumflex artery was chest pain. Chest pain on exertion was documented in 59% of the cases; however, these patients did not have any angiographic evidence of coronary artery disease. The etiology of chest pain in these patients is not clearly understood. One of the explanations offered in literature is a steal phenomenon during exertion, where there may be transient ischemia in territories fed by the RCA and LAD due to the diversion of blood flow to anatomical regions usually fed by the left circumflex artery [3].
Uniquely our patient had T wave inversions in the inferior leads and occasional PVCs which led to an ECHO that showed reduced ejection fraction and distinct regional wall motion abnormalities in the territory supplied by the LCX or RCA. This led to the angiogram and the diagnosis of an absent LCX artery. Echocardiograms were reported in 11/21 (52.4%) patients in the review. Apart from our patient, the other 2 patients who had reduced ejection fraction with regional wall motion abnormalities were those with underlying coronary artery disease. The exact etiology of our patients reduced ejection fraction, which was confirmed on the cardiac MRI, was unclear given that he had viable myocardium and no underlying coronary artery disease. Premature ventricular contractions (PVCs) have not been reported as an associated finding in patients with left circumflex anomaly; however, our patient continues to have them despite beta blocker therapy. It is unclear if the PVCs are related to his underlying coronary anomaly.
Percutaneous coronary angiography and computed tomography (CT) of the coronary arteries were the two main diagnostic modalities reported. Like the present case, 12 other patients were diagnosed with a coronary angiography, 3 with cardiac CT and 5 using a combination of coronary angiography and an aortogram. Coronary angiography is the preferred imaging technique for coronary artery evaluation; however, multislice 3D coronary CT has proven to be equally beneficial given its noninvasive nature and three-dimensional view. A combination of both imaging methods obviously gives a more robust assessment of coronary arteries and their neighboring structures [13].
Patients with a congenitally absent LCX usually have a superdominant RCA as an anatomical compensation for blood supply to areas of the heart usually supplied by the LCX. This was evident in our case and was reported in 90.4% of the entire cohort. In addition to the absent LCX, other concomitant congenital abnormalities described so far are (i) atretic mid LAD originating from the sinus of Valsalva, (ii) dual LAD, (iii) LAD originating from the right coronary cusps, and (iv) nonexisting left subclavian artery [10, 15, 19].
The absence of a LCX is usually regarded as a benign condition that does not require lesion specific intervention [12]. Rather, management per guideline directed medical therapy is recommended. None of the 21 cases reviewed reported any negative outcome associated with the absent LCX. Of the entire cohort, 4 (19%) patients were diagnosed with acute myocardial infarction (AMI) with clinically significant stenotic lesions in the remaining blood vessels on angiogram. These patients, however, had significant comorbidities that predisposed them to atherosclerotic coronary artery disease.
5. Conclusion
Congenital absence of the left circumflex coronary artery is a rare, relatively benign condition that does not require lesion specific treatment. It presents most commonly with chest pain and may be associated with EKG abnormalities. Definitive diagnosis is usually made by cardiac CTA or coronary angiogram.
Conflicts of Interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or nonfinancial interest in the subject matter or materials discussed in this manuscript.
References
- 1.Namgung J., Kim J. A. The prevalence of coronary anomalies in a single center of Korea: origination, course, and termination anomalies of aberrant coronary arteries detected by ECG-gated cardiac MDCT. BMC Cardiovascular Disorders. 2014;14(1, article 1) doi: 10.1186/1471-2261-14-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yamanaka O., Hobbs R. E. Coronary artery anomalies in 126,595 patients undergoing coronary arteriography. Catheterization and Cardiovascular Diagnosis. 1990;21(1):28–40. doi: 10.1002/ccd.1810210110. [DOI] [PubMed] [Google Scholar]
- 3.Varela D., Teleb M., Said S., Fan J., Mukherjee D., Abbas A. Congenital absence of left circumflex presenting after an emotional stressor. Polish Journal of Radiology. 2015;80(1):529–531. doi: 10.12659/PJR.895872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ali F. A., Khan S. A., Tai J. M., Fatimi S. H., Dhakam S. H. Congenital absence of left circumflex artery with a dominant right coronary artery. BMJ Case Reports. 2009;2009 doi: 10.1136/bcr.08.2008.0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oliveira M. D. P., de Fazzio F. R., Mariani J., Jr., et al. Superdominant right coronary artery with absence of left circumflex and anomalous origin of the left anterior descending coronary from the right sinus: an unheard coronary anomaly circulation. Case Reports in Cardiology. 2015;2015:4. doi: 10.1155/2015/721536.721536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Duan Q.-J., Cheng H.-F., Jiang D.-M., Tao K.-Y. Congenital absence of left circumflex artery associated with constrictive pericarditis and thoracostomach. Acta Cardiologica. 2014;69(4):467–468. doi: 10.2143/AC.69.4.3036669. doi: 10.2143/AC.69.4.3036669. [DOI] [PubMed] [Google Scholar]
- 7.Guo J., Xu M. Congenital absence of the left circumflex artery associated with inferior myocardial infarction. Internal Medicine. 2012;51(1):71–74. doi: 10.2169/internalmedicine.51.6141. [DOI] [PubMed] [Google Scholar]
- 8.Quijada-Fumero A., Pimienta-González R., Rodriguez-Esteban M. Absence of left circumflex with superdominant right coronary artery. BMJ Case Reports. 2014 doi: 10.1136/bcr-2014-206782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lin T.-C., Lee W.-S., Kong C.-W., Chan W.-L. Congenital absence of the left circumflex coronary artery. Japanese Heart Journal. 2003;44(6):1015–1020. doi: 10.1536/jhj.44.1015. [DOI] [PubMed] [Google Scholar]
- 10.Teunissen P. F., Marcu C. B., Knaapen P., Van Royen N. A case of multiple coronary atresias: a rarity even within the family of coronary anomalies. European Heart Journal. 2015;36(29):p. 1936. doi: 10.1093/eurheartj/ehv146. [DOI] [PubMed] [Google Scholar]
- 11.Vijayvergiya R., Jaswal R. K. Anomalous left anterior descending, absent circumflex and unusual dominant course of right coronary artery: a case report-R1. International Journal of Cardiology. 2005;102(1):147–148. doi: 10.1016/j.ijcard.2004.03.075. [DOI] [PubMed] [Google Scholar]
- 12.Hongsakul K., Suwannanon R. Congenital absence of left circumflex artery detected by computed tomography coronary angiography: a case report. Case Reports in Vascular Medicine. 2012;2012:3. doi: 10.1155/2012/204657.204657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Majid Y., Warade M., Sinha J., Kalyanpur A., Gupta T. Superdominant right sdcoronary artery with absent left circumflex artery. Biomedical Imaging and Intervention Journal. 2011;7(1) doi: 10.2349/biij.7.1.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hong P. S., Lee Y. S., Lee J. B. Congenital absence of the left circumflex coronary artery in a patient with acute inferior myocardial infarction. Herz. 2014;39(8):957–959. doi: 10.1007/s00059-013-3893-0. [DOI] [PubMed] [Google Scholar]
- 15.Bildirici U., Kiliç T., Ura D., Bulut O., Ural E. Combined congenital coronary artery anomaly: dual left anterior descending coronary artery and absence of left circumflex artery. Anadolu Kardiyoloji Dergisi. 2011;11(2):180–181. doi: 10.5152/akd.2011.042. [DOI] [PubMed] [Google Scholar]
- 16.Yoon Y. K., Rha S.-W., Na J. O., et al. Congenital absence of left circumflex coronary artery presented with vasospastic angina and myocardial bridge in single left coronary artery. International Journal of Cardiology. 2009;131(3):e108–e111. doi: 10.1016/j.ijcard.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 17.Baskurt M., Okcun B., Caglar I. M., Ozkan A. A., Ersanli M., Gurmen T. Congenital absence of the left circumflex coronary artery and an unusually dominant course of the right coronary artery. Cardiovascular Journal of Africa. 2010;21(5):286–288. [PMC free article] [PubMed] [Google Scholar]
- 18.Sato Y., Matsumoto N., Ichikawa M., et al. MDCT detection of congenital absence of the left circumflex artery associated with atherosclerotic coronary artery disease. International Journal of Cardiology. 2006;113(3):408–409. doi: 10.1016/j.ijcard.2005.09.045. [DOI] [PubMed] [Google Scholar]
- 19.Harada R., Nakajima T., Kawaharda N. Absent left circumflex artery detected by computed tomography-angiography. Asian Cardiovascular and Thoracic Annals. 2016 doi: 10.1177/0218492316648582. [DOI] [PubMed] [Google Scholar]
- 20.Doven O., Yurtdas M., Çicek D., Ozcan I. T. Congenital absence of left circumflex coronary artery with superdominant right coronary artery. The Anatolian Journal of Cardiology. 2006;6:208–209. [PubMed] [Google Scholar]