Abstract
Objectives
The purpose of this article is to describe a community-based participatory research pilot project conducted to investigate the knowledge, attitudes, and beliefs that Pacific Islanders (PIs) hold toward biospecimen collection, use, and banking, all of which will help drive higher PI participation rates in both medical and behavioral research studies.
Method
Academic and community partners worked side by side to develop a conceptual model, study measures, and study protocols. PI community partners screened, recruited, and conducted data collection, which consisted of a paper-and-pencil survey and a 1-hour semistructured interview administered by trained community workers.
Results
A total of 60 PI adults representing various PI ethnic groups completed the surveys and interviews. Results showed a general support for biospecimen studies that would benefit the community, and many are willing to provide their biospecimen samples if asked.
Conclusion
Due to the established level of trust, community partners were able to successfully recruit and collect data for the study. Many of those interviewed also called for more outreach and education about the importance of biospecimen research in their communities.
Keywords: cancer prevention and control, cultural competence, health disparities, ethics, community-based participatory research, health research, Native Hawaiian, minority health, Pacific Islander
BACKGROUND
Approximately 1.2 million U.S. residents identify themselves as Pacific Islander (PI; i.e., people of Polynesian, Melanesian, and Micronesian descent) either in combination with other races or alone (U.S. Census Bureau, 2012). Known as Pacific Island Americans or Oceanian Americans, they make up less than 1% of the total U.S. population but have one of the largest health disparities among minority groups. Compared to other ethnic groups, PIs have higher rates of smoking, alcohol consumption, and obesity (Office of Minority Health [OMH], 2012). Cancer, heart disease, unintentional injuries, stroke, and diabetes are the leading causes of death among PIs. In 2002, the infant mortality rate for Native Hawaiians was 9.6 deaths per 1,000 live births as compared to the rates for all ethnic groups of 7.0. In 2010, the rate of tuberculosis in Native Hawaiian/PIs was 8 times higher than that in their Caucasian counterparts (OMH, 2012). These rates are disturbing and are especially alarming in a population that has limited access to health care and health education (Families USA, 2002; OMH, 2012).
Advancement in genetic research is crucial to addressing these health disparities. Study participation among minorities has not been proportionate to the burden of disease among these populations (Murthy, Krumholz, & Gross, 2004), and thus participation in research through donation of biospecimen samples from diverse populations is vital. These biospecimen samples help researchers draw a link between genetics, disease, and health disparities, such as that related to heart disease, diabetes, and cancer. Studies conducted in Hawaii among both native and nonnative samples have found marked differences in enzyme-encoding genes involved with folate and nicotine metabolism and estrogen biosynthesis (Dachs, Currie, & McKenzie, 2008). Studies like this are limited, and thus more genetic research is needed to explore variation in disease incidence and prognosis among diverse groups.
Unfortunately, minorities are often underrepresented in clinical trials (Hoel et al., 2009; Hussain-Gambles, Atkin, & Leese, 2004), and a majority of the genetic samples currently being studied are from non-Hispanic Whites (Hilton et al., 2010; Wang, Fridinger, Sheedy, & Khoury, 2001). Participation rates for PIs are even much lower than for their Hispanic or African American counterparts. Why are minorities like PIs underrepresented in research studies? What is preventing PIs from participating? In this study, we attempt to understand the barriers and facilitators to study participation among PIs, which can assist researchers and public health professionals in conducting effective biospecimen-related studies. To our knowledge, this pilot study is the first of its kind to assess the knowledge, attitudes, and beliefs that may either hinder or support PIs’ participation in research involving biospecimen samples on the U.S. mainland. This article provides a general overview of the study and its main results plus reports on the use of a community-based participatory research (CBPR) approach involving PI community partners.
To date, there is no conclusive evidence to suggest reasons for the large health disparities among this population. Research studying cancer risk factors have had limited access to PI genetic data due to lack of participation (Chlebowski et al., 2005; Murthy et al., 2004). Even as a combined group, Asian American/PIs account for less than 10% of the sample in most studies (Chlebowski et al., 2005; Murthy et al., 2004). An extensive review of the barriers to recruiting underrepresented populations to cancer clinical trials by the Johns Hopkins School of Public Health showed low participation rates to be related to awareness, language, cultural beliefs, and trust in researchers (Ford et al., 2008). Although the review looked at a total of 65 articles with a total sample of over 600,000 participants, there was not enough information from PIs, and thus we still do not understand why PIs are under-represented.
To gain entry into the PI community and better understand the reasons that drive low participation rates, we used the existing networks of PI community leaders who have a strong relationship with their communities. This is a pilot research project built on the successes of the community network program— WINCART: Weaving an Islander Network for Cancer Awareness, Research and Training—which aims to reduce chronic disease mortality and morbidity through lifestyle change among PIs using community-based approaches (Tanjasiri et al., 2007; Tanjasiri & Tran, 2008). The main goal of this pilot study was to investigate the knowledge, attitudes, and beliefs of PIs concerning biospecimen research in the hope of understanding the reasons that hinder their participation, and to identify factors that may support their involvement in biospecimen research. Among our objectives was to learn about the willingness of PIs to participate in research, to investigate the barriers that might prevent PIs from joining studies, and to gain a general overview of the experiences PIs have had with providing their biospecimen samples in a clinical setting while using a CBPR approach that actively engages PI community leaders.
THE CBPR APPROACH
Based on the works of researchers and educators like Kurt Lewin, Orlando Fals Borda, and Paulo Freire, CBPR focuses on research that is equally shared by community members and traditionally trained professionals (Minkler & Wallerstein, 2008). We involved the PI community partners in all phases of the study because they know their study populations best. Community partner involvement ranged from development of a conceptual model that was used to guide study measures to refinement of surveys and questionnaires to recruitment, data collection, and interpretation of results.
WINCART’s CBPR community partners consists of five community-based organizations located in Southern California that provide services to PIs living in Los Angeles, Orange, Riverside, San Bernardino, and San Diego counties. These five community partners consist of (a) The Guam Communications Network— GCN 501(c)(3), a community-based multiservice agency serving Chamorros in Los Angeles, Orange, Riverside, and San Bernardino counties and a recipient of numerous government and private foundation funding awards; (b) Pacific Islander Health Partnership—PIHP 501(c)(3), which serves all PIs living mainly in the Orange County area; (c) the Union of Pan Asian Communities—UPAC 501(c)(3), an organization based in San Diego County that addresses the social, psychological, physical, and economic needs of San Diego’s Asian PI populations; (d) the Tongan Community Service Center—TCSC 501(c)(3), a Los Angeles–based organization that specializes in working in conjunction with diverse ethnic minority and disenfranchised community groups to develop models for social service delivery and community self-sufficiency; and (e) the Samoan National Nurses Association—SNNA 501(c) (3), an organization in Carson, California, that aims to improve the Samoan community through service, outreach, education, advocacy, organizing, and research.
WINCART’s community partners were involved in every phase of the pilot project. Partners helped develop the conceptual model (Months 1–3), study design, and measures (Months 3–6); helped in recruitment and screening materials (Months 6–7); recruited potential participants (Months 6–9); collected data (Months 10–18); transcribed interviews (Months 10–18); assisted with interpretation of the results (Months 18–20); and assisted with dissemination (Months 21–24). We did not move to the next steps until the group approved and agreed on the issues at hand. For example, before printing the recruitment and screening materials, we revised the screening questionnaire several times because some partners felt that the wording did not make sense to them. Study materials were typically developed by the academic partners, who later shared them with the community partners at monthly meetings to obtain input and suggestions. Suggestions from community partners were then integrated into revised versions and were shared again at the next monthly meeting. These back and forth processes took several months, but what resulted are products that reflect the needs of the academic team in terms of scientific rigor as well as of the community partners in terms of cultural appropriateness and relevancy. In addition to development, community partners worked alongside the academic team to implement the study. Partners recruited potential participants at local festivals, workshops, and community events. They scheduled interviews and conducted the data collection at their agencies. Once data collection was complete, the community and academic team worked together to interpret the results with community partners taking active role in providing meaningful interpretation of the results. Together the entire team reviewed frequencies and percentages of the demographic data and other study variables plus carefully assessed the major themes that were obtained from the qualitative portion of the study. A few months after study completion, community partners held an event where the results of the pilot study were presented to the general PI community. Some community partners also took a lead role and presented a poster of the data at a national conference.
CONCEPTUAL MODEL
Under the CBPR approach, community and academic partners together developed a conceptual model that takes into consideration potential moderators (ethnicity, acculturation, education, etc.) and mediators (health locus of control, perceived threats/benefits, trust in medical and research personnel, personal experiences, knowledge, etc.) that affect participation in biospecimen research. In this model, we wanted to demonstrate the factors that lead to PI knowledge, attitudes, and beliefs, which then fuels future actions and future decision making about research study participation (see Figure 1). We conceptualized that demographic characteristics such as age, gender, and socioeconomic status and personal characteristics such as health status and acculturation form the foundation from which experience, health locus of control, perceived benefits or threats, and individual preferences are formed. Together these factors form the basis of individual knowledge, attitudes, and beliefs.
FIGURE 1.
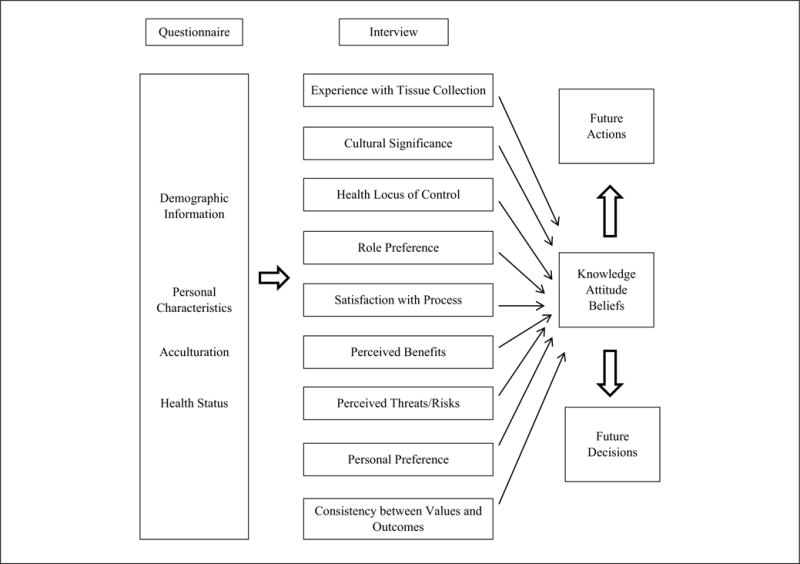
Conceptual Model
This conceptual model began with review of existing literature on participation and involvement in biospecimen-related studies among both Caucasians and minorities. We reviewed works of the Tuskegee Legacy Project (Katz et al., 2006) and works done in urban indigenous populations of Australia (E. H. Cunningham et al., 2007; J. Cunningham & Dunbar, 2007), in Native Americans (Jacobs et al., 2010), and in Native Hawaiians (Fong, Braun, & Chang, 2004), in addition to studies on the general population and their attitudes toward studies involving biospecimen samples (Beskow & Dean, 2008; Meslin & Quaid, 2004; Porteri & Borry, 2008). We borrowed constructs from a study looking at informed decision making (Mullen et al., 2006) and developed our own construct that best fit our study population. Mullen et al. (2006) conducted a review of 36 studies involving decision making for cancer screening. They identified the most frequent constructs across the studies, such as knowledge, perceived risk and severity, benefits and barriers to screening, plus discussion of screening with health care providers. We adapted these constructs for our model by changing it from cancer screening to biospecimen donation. However, through discussion with our community partners we realized that we lacked questions regarding the importance of culture on biospecimen donation. We learned that certain PI cultures believe that blood, hair, and other parts of the body belonged to the land. If samples are taken from the body, they should be returned to the land, and thus we included a construct on cultural significance.
Like other components of the study, the conceptual model went through several revisions before it was finalized. Our original models had over 20 constructs (e.g., religion and spirituality, acculturation and stress, safeguards from group harm, and responsibilities to the community). Community partners took active roles in reviewing each revised model and provided input on ways the model can be improved. As a group, we decided to trim down the conceptual model, collapsing constructs together whenever possible, and ended up with a final model consisting of 9 constructs. Like other CBPR studies on biospecimen collection, our final model includes constructs like attitudes and experience.
METHOD
To better understand the factors that hinder and support PI participation in biospecimen research, we conducted a brief paper-and-pencil survey plus a 45- to 60-minute one-on-one, semistructured interview among 60 PIs. Cancer survivors were recruited to participate in this study because of the high incidence of cancer among the PI community and because of their unique experiences with biospecimen collection, use, and storage. After reviewing previous studies of similar scope and discussion with community partners, the sample size was set at 60 (12 per community agency) because we wanted a realistic number that each partner could attain. It is also important to note that we conducted a community sampling process rather than a random sampling process because community partners know and understand their communities best. These partners serve as gatekeepers, advocates, and health educators to their communities. They are a trusted source of information and are able to identify pockets of individuals for the study that traditional recruitment cannot.
Screening and Recruitment
A recruitment flyer was developed specifically for each partner and contained contact information for a staff member at each community partner organization. Recruitment was conducted at various PI festivals in the Southern California region, health fairs, community partner–sponsored activities (e.g., PIHP’s Aloha Seniors), through word of mouth and personal contact. Eligible participants were males and females 21 years of age or older who self-identified as being a PI and living in the Southern California region.
Interview Training
Since many of our community partners were not trained to conduct formal interviews for qualitative studies, we developed a two-component interview training guide. This guide consisted of an educational module and a video demonstration module where an academic partner and a community partner acted out mock interviews under various scenarios (i.e., over-responder, underresponder, emotional responder, etc.). Both modules were shared with each partner and made available online as reference. Community partners also participated in a 1-day interview training session.
Instruments
Guided by the conceptual model, the study instrument consisted of a 46-item paper-and-pencil questionnaire and a semistructured, one-on-one interview. The paper-and-pencil survey consisted of demographic items in addition to questions on acculturation, health status, and cancer history. Whenever applicable, standardized scales such as the health locus of control scale (Wallston, 1978) and the acculturation scale (Acculturation, Habits, and Interests Multicultural Scale for Adolescents; Unger et al., 2002) were adapted and used in the questionnaire. The interview questions consisted of six different sections as outlined in Table 1. Due to the very specific and tailored research questions, certain measures were developed exclusively for the study.
TABLE 1.
Components of the Semistructured Interview
| Sections | Sample Questions |
|---|---|
| Experience With Tissue Collection: Satisfaction With the Process | How do you feel in general about providing tissue samples (blood, skin, hair, nails, or urine) to help in diagnosing illness and treating people who need medical care? |
| Perceptions Regarding Genetic Research | How would you feel about your tissue sample being used for genetic research that might someday benefit other people, in particular, other Pacific Islanders? |
| Cultural Significance | Can you describe whether in your culture, tissue samples belong to the individual, family, or community? |
| Consistency Between Values and Outcomes | What might researchers or doctors do to gain trust in the Pacific Islander community? |
| Perceived Benefits | In your opinion, how might tissue sample research benefit your community? |
| Perceived Threats/Risks | In your opinion, how might tissue sample research harm your community? |
Data Collection
Each component of the data collection packet was color coded to minimize mistakes during data collection. Community partner data collectors were provided with specific instructions on the data collection process and were given audio recorders. Once the interviews were completed, recordings were downloaded onto the computer and community partners at each organization transcribed and, whenever necessary, translated the interviews into Word documents. All transcripts were then imported into Atlast.ti and coded by the project leader, who read through each transcript and coded each participant’s responses into a variety of themes such as “understand the benefits of biospecimen research,” “knows little about informed consent,” and “has reservations about providing biospecimen samples.” Each time a participant provided a response, it was coded under the appropriate theme. However, a participant may have expressed a particular theme more than once during the interview, and this is reflected in the number of coded responses (i.e., a participant may express that he or she “has reservations about providing biospecimen samples” more than once during the interview).
OVERALL STUDY RESULTS
A total of 60 PIs were interviewed for the study, 35% of whom were males (N = 21) with an average age of 61 years. Close to half were born outside the United States in Samoa, American Samoa, Guam, and Palau. The largest PI ethnic group in the sample was Native Hawaiians (35%), followed by Samoans (22%) and Chamorros (20%), with 1 Paluan and 1 Maori representative. English was the primary language for 75% of the sample, and over half had completed high school or more. The average household income was between $35,000 and $45,000 per year with an average household size of four people (see Table 2).
TABLE 2.
Demographic Data
| Frequency (%) | |
|---|---|
| Total sample size | 60 |
| Cancer survivors | 35 (58) |
| Males | 21 (35) |
| Average age, years | 61 |
| Ethnicity | |
| Native Hawaiian | 21 (35) |
| Samoan | 13 (22) |
| Chamorro | 12 (20) |
| Tongan | 9 (15) |
| Marshallese | 3 (5) |
| Paluan | 1 (2) |
| New Zealand Maori | 1 (2) |
| English as a primary language | 45 (75) |
| Born outside the United States | 29 (48) |
| Education | |
| Less than high school | 3 (5) |
| High school/GED | 22 (37) |
| Post–high school | 27 (45) |
| College graduate | 8 (13) |
| Average household income, $ | 35,000–45,000 |
| Average household size | 4 |
Qualitative analysis of the 60 interview transcripts in Atlas.ti resulted in six main themes and approximately 1600 coded responses. “Understands the benefits of research,” “had a positive clinical experience,” “willing to provide biospecimen samples for beneficial research,” and “has trust in medical doctors and researchers” were some of the major themes obtained from the interviews. The most common theme among the PI participants in this project was “understands the benefits of research,” meaning that participants understand that biospecimen research is beneficial to them and their community, which was cited by 92% of the participants (see Table 3).
TABLE 3.
Common Themes (Number of Coded Response = 1,601)
| Themes | % Coded response | % Participants |
|---|---|---|
| Understands the benefits of research | 8 | 92 |
| Had a positive clinical experience | 5 | 80 |
| Were provided with detailed information about treatment from providers | 5 | 82 |
| Willing to provide biospecimen samples for beneficial research | 12 | 98 |
| Willing to provide biospecimen samples for medical diagnosis | 5 | 80 |
| Has trust in medical doctors and researchers | 5 | 83 |
DISCUSSION
Community partner involvement was crucial to the success of this pilot study. Due to the lack of existing literature on this topic, we had no previous information on which to draw. The community partners served as field experts in PI culture, lifestyles, and beliefs and thus provided valuable input that shaped and refined the conceptual model. Their input helped guide the study measures and brought community relevancy to the project. Their existing connections in the community made recruitment effective and efficient. More importantly, we would not have been able to conduct interviews had we not employed community partners as data collectors and interviewers. Some participants indicated during the interviews that they would have never agreed to participating in the study had they not been recruited by someone they know and trust.
Results of the interview among PIs showed general support for biospecimen research. Many indicate that they support research that will benefit others in their community and that they were willing to provide biospecimen samples for that specific purpose: “If I can help someone get cured or help someone in a study that will help our native people, then I’m all for it” (male, Native Hawaiian). Many call for more education about biospecimen research in their community and suggest that researchers would garner more enthusiasm about participating in similar research if they educated the community about its intent and significance: “If doctors educate people properly they would probably have more people willing to participate” (male, Chamorro). These findings are consistent with research conducted among Asians (Wong, Chia, Yam, Teodoro, & Lau, 2004), Hispanics (Zimmerman, 1997), and African Americans (Smith et al., 2007).
Although a majority of participants did show support for biospecimen research, there were a few participants with reservations that may help provide an explanation as to why PIs are underrepresented in research studies. A small percentage of the participants did not trust medical providers and researchers because they felt that these individuals do not understand the PI culture. Some participants suggested the fear of pain or fear of learning that something is wrong discouraged PIs from donating their biospecimen samples. A few participants feared that their biospecimen samples may be sold overseas for profit or used in unethical ways. The fears and hesitations expressed by PI participants of this pilot study are not unique. Research studies conducted among African Americans and Hispanics have found similar issues with distrust and fear of pain (Corbie-Smith, Thomas, Williams, & Moody-Ayers, 1999; Giuliano et al., 2000; Shavers-Hornadaya, Lynch, Burmeister, & Torner, 1997). A focus group study conducted among African American adults found that trust issues were an important barrier to participation in clinical studies. Participants indicated that they did not fully understand the process of informed consent and felt exploited (Corbie-Smith et al., 1999).
Several limitations do exist in this study that need to be noted. First, because this is a pilot study the sample was very small. We did not employ random sampling and thus our findings might not reflect the knowledge, attitudes, and beliefs of PIs living in other parts of the United States or around the world. The majority of our participants were born in the United States, and thus there is a sufficient level of acculturation among our sample, which might not be the case in other regions. Second, close to two thirds of our sample were female and over half were cancer survivors. The clinical experiences of cancer survivors are different from that of the general population. It may be positive or negative like the general population, but it is definitely more extensive. Last, over 50% of our sample are older than 65 years and come from a generation whom may distrust genetic research.
In this article, we described the process of using CBPR to develop and implement a pilot study among PIs with equal partnership between community leaders and academic research staff. The success of using CBPR has been reported in many studies (Andrews et al., 2012; Barbee et al., 2010; DeHaven et al., 2011; Pazoki, Nabipour, Seyednezami, & Imami, 2007), and our pilot project is no different. With the assistance and dedication of community partners, we were able to successfully recruit and interview the intended study sample without any problems. The success of this project provides additional support for involving the community as research partners in studies of minorities and health disparities. Future studies in this field should look to the community partners not only as gatekeepers and a source of information but as researchers who can assist with study design, refinement of measures, and data interpretation and dissemination. Studies of minorities and health disparities that fail to involve community partners may face a lower chance of success.
Acknowledgments
This research was supported by the National Cancer Institute’s Center to Reduce Cancer Health Disparities (grant number U54CA153458-02). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Andrews JO, Tingen MS, Jarriel SC, Caleb M, Simmons A, Brunson J, Hurman C. Application of a CBPR framework to inform a multi-level tobacco cessation intervention in public housing neighborhoods. American Journal of Community Psychology. 2012;50:129–140. doi: 10.1007/s10464-011-9482-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barbee L, Kobetz E, Menard J, Cook N, Blanco J, Barton B, McKenzie N. Assessing the acceptability of self-sampling for HPV among Haitian immigrant women: CBPR in action. Cancer Causes & Control. 2010;21:421–431. doi: 10.1007/s10552-009-9474-0. [DOI] [PubMed] [Google Scholar]
- Beskow L, Dean E. Informed consent for biorepositories: assessing prospective participants’ understanding and opinions. Cancer Epidemiology, Biomarkers & Prevention. 2008;17:1440–1451. [Google Scholar]
- Chlebowski R, Chen Z, Anderson G, Rohan T, Aragaki A, Lane D, Prentice R. Ethnicity and breast cancer: Factors influencing differences in incidence and outcome. Journal of the National Cancer Institute. 2005;97:439–448. doi: 10.1093/jnci/dji064. [DOI] [PubMed] [Google Scholar]
- Corbie-Smith G, Thomas SB, Williams MV, Moody-Ayers S. Attitudes and beliefs of African Americans toward participation in medical research. Journal of General Internal Medicine. 1999;14:537–546. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cunningham EH, Cameron V, Evans J, Irvine V, Pitama S, Robertson P. The development of guidelines for handling samples and specimens collected for research involving Maori. New Zealand Medical Journal. 2007;120:U2785. [PubMed] [Google Scholar]
- Cunningham J, Dunbar T. Consent for long-term storage of blood samples by Indigenous Australian research participants: The DRUID Study experience. Epidemiologic Perspectives & Innovation. 2007;4(7) doi: 10.1186/1742-5573-4-7. Retrieved from http://www.biomedcentral.com/1742-5573/4/7/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dachs G, Currie M, McKenzie F. Cancer disparities in indigenious Polynesian populations: Maori, Native Hawaiians, and Pacific people. Lancet Oncology. 2008;9:473–484. doi: 10.1016/S1470-2045(08)70127-X. [DOI] [PubMed] [Google Scholar]
- DeHaven MJ, Ramos-Roman MA, Gimpel N, Carson J, DeLemos J, Pickens S, Lee JJ. The GoodNEWS (Genes, Nutrition, Exercise, Wellness, and Spiritual Growth) Trial: A community-based participatory research (CBPR) trial with African-American church congregations for reducing cardiovascular disease risk factors–recruitment, measurement, and randomization. Contemporary Clinical Trials. 2011;32:630–640. doi: 10.1016/j.cct.2011.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Families USA. Health coverage in Asian American and Pacific Islander communities: What’s the problem and what can you do about it? 2002 Retrieved from http://familiesusa2.org/assets/pdfs/AsAm1044.pdf.
- Fong M, Braun K, Chang M. Native Hawaiian preferences for informed consent and disclosure of results from research using stored biological specimens. Pacific Health Dialog. 2004;11:154–159. [PubMed] [Google Scholar]
- Ford JG, Howerton MW, Lai GY, Gary TL, Bolen S, Gibbons MC, Bass EB. Barriers to recruiting underrepresented populations to cancer clinical trials: A systematic review. Cancer. 2008;112:228–242. doi: 10.1002/cncr.23157. [DOI] [PubMed] [Google Scholar]
- Giuliano AR, Mokuau N, Hughes C, Tortolero-Luna G, Risendal B, Ho RCS, McCaskill-Stevens WJ. Participation of minorities in cancer research: The influence of structural, cultural, and linguistic factors. Annals of Epidemiology. 2000;10(8 Suppl):S22–S34. doi: 10.1016/s1047-2797(00)00195-2. [DOI] [PubMed] [Google Scholar]
- Hilton C, Fitzgerald R, Jackson K, Maxim R, Bosworth C, Shattuck P, Constantino J. Brief report: Under-representation of African Americans in autism genetic research: A rationale for inclusion of subjects representing diverse family structures. Journal of Autism and Developmental Disorders. 2010;40:633–639. doi: 10.1007/s10803-009-0905-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoel AW, Kayssi A, Brahmanandam S, Belkin M, Conte MS, Nguyen LL. Under-representation of women and ethnic minorities in vascular surgery randomized controlled trials. Journal of Vascular Surgery. 2009;50:349–354. doi: 10.1016/j.jvs.2009.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussain-Gambles M, Atkin K, Leese B. Why ethnic minority groups are under-represented in clinical trials: A review of the literature. Health & Social Care in the Community. 2004;12:382–388. doi: 10.1111/j.1365-2524.. [DOI] [PubMed] [Google Scholar]
- Jacobs B, Roffenbender J, Collmann J, Cherry K, Bitsoi L, Bassett K, Evans C. Bridging the divide between genomic science and indigenous peoples. Journal of Law, Medicine & Ethics. 2010;38:684–697. doi: 10.1111/j.1748-720X.2010.00521.x. [DOI] [PubMed] [Google Scholar]
- Katz R, Russell S, Kressin N, Green B, Wang M, James S, Claudio C. The Tuskegee Legacy Project: Willingness of minorities to participate in biomedical research. Journal of Health Care for the Poor and Underserved. 2006;17:698–715. doi: 10.1353/hpu.2006.0126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meslin E, Quaid K. Ethical issues in the collection, storage and research use of human biological materials. Journal of Laboratory and Clinical Medicine. 2004;144:229–234. doi: 10.1016/j.lab.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Minkler M, Wallerstein N. Community-based participatory research for health: From process to outcomes. San Francisco, CA: Jossey-Bass; 2008. [Google Scholar]
- Mullen P, Allen J, Glanz K, Fernandez M, Bowen D, Pruitt S, Pignone M. Measures used in studies of informed decision making about cancer screening: A systematic review. Annals of Behavioral Medicine. 2006;32:188–201. doi: 10.1207/s15324796abm3203_4. [DOI] [PubMed] [Google Scholar]
- Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: Race-, sex-, and age-based disparities. Journal of the American Medical Association. 2004;291:2720–2726. doi: 10.1001/jama.291.22.2720. [DOI] [PubMed] [Google Scholar]
- Office of Minority Health. Native Hawaiian and Pacific Islander profile. 2012 Retrieved from http://minorityhealth.hhs.gov/templates/browse.aspx?lvl=2&lvlID=71.
- Pazoki R, Nabipour I, Seyednezami N, Imami S. Effects of a community-based healthy heart program on increasing healthy women’s physical activity: A randomized controlled trial guided by community-based participatory research (CBPR) BMC Public Health. 2007;7:216. doi: 10.1186/1471-2458-7-216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porteri C, Borry P. A proposal for a model of informed consent for the collection, storage and use of biological materials for research purposes. Patient Education and Counseling. 2008;71:136–142. doi: 10.1016/j.pec.2007.12.003. [DOI] [PubMed] [Google Scholar]
- Shavers-Hornadaya V, Lynch C, Burmeister LF, Torner J. Why are African Americans under-represented in medical research studies? Impediments to participation. Ethnicity & Health. 1997;2:31–45. doi: 10.1080/13557858.1997.9961813. [DOI] [PubMed] [Google Scholar]
- Smith Y, Johnson A, Newman L, Greene A, Johnson T, Rogers J. Perceptions of clinical research participation among African American women. Journal of Women’s Health. 2007;16:423–428. doi: 10.1089/jwh.2006.0124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanjasiri S, Tran J. Community capacity for cancer control collaboration: Weaving an Islander network for cancer awareness, research and training for Pacific Islanders in Southern California. Cancer Detection and Prevention. 2008;32(Suppl. 1):S37–S40. doi: 10.1016/j.cdp.2007.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanjasiri S, Tran J, Palmer P, Foo M, Hanneman M, Lee C, Sripattana A. Developing a community-based collaboration to reduce cancer health disparities among Pacific Islanders in California. Developing Human Resources in the Pacific. 2007;14:114–122. [PubMed] [Google Scholar]
- Unger J, Gallahen P, Shakib S, Ritt-Olson A, Palmer P, Johnson C. The AHIMSA Acculturation Scale: A new measure of acculturation for adolescents in a multicultural society. Journal of Early Adolescents. 2002;22:225–251. [Google Scholar]
- U.S. Census Bureau. The Native Hawaiian and other Pacific Islander population: 2010. 2012 Retrieved from http://www.census.gov/newsroom/releases/archives/facts_for_features_special_editions/cb12-ff09.html.
- Wallston KA. Health locus of control. Health Education Monographs. 1978;6:160–170. doi: 10.1177/109019817800600107. [DOI] [PubMed] [Google Scholar]
- Wang S, Fridinger F, Sheedy K, Khoury M. Public attitudes regarding the donation and storage of blood specimens for genetic research. Community Genetics. 2001;4:18–26. doi: 10.1159/000051152. [DOI] [PubMed] [Google Scholar]
- Wong M, Chia K, Yam W, Teodoro G, Lau K. Willingness to donate blood samples for genetic research: A survey from a community in Singapore. Clinical Genetics. 2004;65:45–51. doi: 10.1111/j..2004.00192.x. [DOI] [PubMed] [Google Scholar]
- Zimmerman S. Factors influencing Hispanic participation in prostate cancer screening. Oncology Nursing Forum. 1997;24:499–504. [PubMed] [Google Scholar]


