Abstract
Objectives: As professional medical caregivers, nurses have extensive medical knowledge and information than general population. However, they may use their professional knowledge and networks to seek prompt health services. In this study, we aimed to determine susceptibility of nurses with diabetes to developing end-stage renal disease requiring dialysis compared to diabetes patients in the general population.
Methods: This retrospective longitudinal study extracted data of nurses with newly diagnosed diabetes and general patients with diabetes from the National Health Insurance Database between 1998 and 2006 and follow-up to December 2009, satisfied the participant inclusion criteria was 518,058. Nurses and general population were matched with propensity score method in a 1:10 ratio. Basic characteristics and health status were similar between groups. Cox proportional hazards model was used to compare relative risks and dialysis factors between groups.
Results: Nurses were younger than general population with diabetes (42.01 years vs. 59.29 years) and had lower risk of dialysis (adjusted hazard ratio = 0.36, 95% confidence interval 0.16-0.81). Nurses with Diabetes Complications Severity Index (DCSI)≧3 had dialysis risk up to 83.53 times higher than that of the reference group (DCSI < 3). DCSI was the only variable determined to be a related factor affecting dialysis risk in nurses with diabetes.
Conclusions: Nurses with diabetes have lower risk of dialysis. This suggests that nurses may have more knowledge regarding chronic disease control and change their lifestyles than general diabetes patients. Results of this study may serve as a reference for developing health education.
Keywords: Nurse with Diabetes, Dialysis, National Health Insurance, KAP, Cohort Study
1. Introduction
The data from the United States Renal Data System (USRDS) in 2013 showed that Taiwan has both a high prevalence and incidence of end-stage renal disease (ESRD).[1] Molitch et al.[2] reported that the major cause of ESRD was diabetes and that the percentage increased from 25.4% in 1990 to 39.5% in 2004. The effect of diabetes on ESRD has increased 1.6 times over 15 years, which is attributable to the high prevalence of type 2 diabetes mellitus (T2DM).
T2DM is a major chronic disease worldwide, with approximately 382 million diabetes patients aged between 20 and 79 years in 2013.[3] The International Diabetes Federation (IDF) reported that 3.8 million people die of diabetes-related diseases annually around the world.[4] Therefore, early diagnosis of diabetes and provision of comprehensive and professional health education may enhance the self-care ability and personal responsibility of patients as well as to reduce related complications and mortality rate.
There are numerous studies related to illness behaviors and health seeking, the majority of which focus on specific types of patients. The health belief model,[5] the Andersen Behavioral Model of Health Services Use,[6] the Theory of Planned Behavior,[7] and the general theory of help-seeking [8] describe the basic foundation for the determinants of various diseases. However, a limited number of studies have examined the behavior of disease-affected health providers to determine whether they are influenced by their medical knowledge.
Self-care ability is a factor in patient behavior. Patient knowledge regarding their health status affects their attitude and practice. The interaction of these three aspects – knowledge, attitude and practice – has been described as the knowledge, attitude and practice theory (KAP)[9]. This theory postulates that if people have accurate knowledge of a disease and develop an active and positive attitude, they will acquire functional self-care ability, which can directly or indirectly affect their prognosis.
As professional medical caregivers, nurses have extensive medical knowledge and different health-seeking behavior and information compared to the general population.[10] Research has investigated nurses, with regard to job satisfaction,[11] stress,[12] daytime sleepiness and risk of disease,[13] and they have more sources of assistance than the general population. However, few studies have examined the relation between professional knowledge and chronic disease outcome with nurses as patients. Whether the advantage of health knowledge regarding their own diabetes ultimately reduces the risk of dialysis in nurses is unknown.
This study primarily investigated relative risk and factors related to the development of ESRD that required dialysis between nurses with newly diagnosed diabetes and patients with newly diagnosed diabetes in the general population. The results of this study could possibly serve as a reference for medical providers and related units in planning health promotion activities. Results of this study may serve as a reference for developing health education regarding chronic diseases.
2. Materials and Methods
2.1. Data source
This is a retrospective longitudinal study. The secondary data in the analysis was retrieved from the National Health Insurance Research Database (NHIRD) and used a specific diabetes mellitus (DM) database that included all nationwide DM patients. This database is an extensive source of health data that currently represents the majority of the population of Taiwan. The National Health Insurance (NHI) commenced in March 1995 as a mandatory public health insurance providing comprehensive coverage of medical services. Since 2012, the NHI covers up to 99.85% of the population in Taiwan.[14] The insurance coverage includes medications prescribed in outpatient, inpatient and emergency departments. The database includes all medical data of insured patients, including chronic disease coverage of diabetes and ESRD[15], which makes it an ideal source of data for the present study. Before the study analyses, all individual identification information was deleted, and personal privacy was protected. This study was approved by the Institutional Review Board (IRB) of China Medical University and Hospital (IRB Number: CMUH 20130326C).
2.2. Study population and sample
Study subjects were Taiwanese nurses with newly diagnosed diabetes and general patients with newly diagnosed diabetes who were diagnosed and treated between 1998 and 2006. We included people who were already nurses at the time of diagnosis with diabetes. Each patient had been observed from the time of their diagnosis until December 31, 2009. Because the majority of nurses in Taiwan are female (98.92%),[16] study subjects included only female nurses and female general patients with newly diagnosed diabetes. Finally, satisfied the participant inclusion criteria was 518,058 (Table 1).
Table 1.
- Patient demographics before and after propensity score (PS) matching.
| Variables | Before PS Matching | After PS Matching (10:1) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | General patients | Nurse | P-value | Total | General patients | Nurse | P-value | |||||||
| N | % | N | % | N | % | N | % | N | % | N | % | |||
| Total patients | 518058 | 100.00 | 516100 | 99.62 | 1958 | 0.38 | 18601 | 100.00 | 16910 | 90.91 | 1691 | 9.09 | ||
| Age | <0.001 | 0.928 | ||||||||||||
| <25 | 3092 | 0.60 | 2913 | 0.56 | 179 | 9.14 | 1194 | 6.42 | 1083 | 6.40 | 111 | 6.56 | ||
| 25-34 | 15361 | 2.97 | 14951 | 2.90 | 410 | 20.94 | 3214 | 17.28 | 2933 | 17.34 | 281 | 16.62 | ||
| 35-44 | 53986 | 10.42 | 53436 | 10.35 | 550 | 28.09 | 5568 | 29.93 | 5069 | 29.98 | 499 | 29.51 | ||
| 45-54 | 127935 | 24.70 | 127351 | 24.68 | 584 | 29.83 | 6059 | 32.57 | 5494 | 32.49 | 565 | 33.41 | ||
| 55-64 | 136540 | 26.36 | 136363 | 26.42 | 177 | 9.04 | 1894 | 10.18 | 1717 | 10.15 | 177 | 10.47 | ||
| ≥65 | 181144 | 34.97 | 181086 | 35.09 | 58 | 2.96 | 672 | 3.61 | 614 | 3.63 | 58 | 3.43 | ||
| Average age (Mean, Std) | 59.22 | 13.15 | 59.29 | 13.11 | 42.01 | 12.03 | 44.14 | 11.86 | 44.19 | 11.87 | 43.60 | 11.78 | ||
| Insured salary (NT$) | <0.001 | 0.659 | ||||||||||||
| Low-income household | 5010 | 0.97 | 5009 | 0.97 | 1 | 0.05 | 3 | 0.02 | 2 | 0.01 | 1 | 0.06 | ||
| ≤17280 | 35033 | 6.77 | 34873 | 6.77 | 160 | 8.17 | 1826 | 9.82 | 1670 | 9.88 | 156 | 9.23 | ||
| 17281~22800 | 295781 | 57.20 | 295390 | 57.34 | 391 | 19.97 | 4312 | 23.18 | 3922 | 23.19 | 390 | 23.06 | ||
| 22801~28800 | 77247 | 14.94 | 77044 | 14.96 | 203 | 10.37 | 2011 | 10.81 | 1819 | 10.76 | 192 | 11.35 | ||
| 28801~36300 | 30974 | 5.99 | 30745 | 5.97 | 229 | 11.70 | 2015 | 10.83 | 1829 | 10.82 | 186 | 11.00 | ||
| 36301~45800 | 33977 | 6.57 | 33470 | 6.50 | 507 | 25.89 | 4128 | 22.19 | 3739 | 22.11 | 389 | 23.00 | ||
| 45801~57800 | 19896 | 3.85 | 19584 | 3.80 | 312 | 15.93 | 2540 | 13.66 | 2311 | 13.67 | 229 | 13.54 | ||
| ≥57801 | 19206 | 3.71 | 19051 | 3.70 | 155 | 7.92 | 1766 | 9.49 | 1618 | 9.57 | 148 | 8.75 | ||
| Missing data | 934 | 934 | ||||||||||||
| Urbanization of residence | <0.001 | 0.181 | ||||||||||||
| Level 1 | 141455 | 27.35 | 140779 | 27.33 | 676 | 34.53 | 6593 | 35.44 | 5998 | 35.47 | 595 | 35.19 | ||
| Level 2 & 3 | 231299 | 44.73 | 230365 | 44.72 | 934 | 47.70 | 9149 | 49.19 | 8334 | 49.28 | 815 | 48.20 | ||
| Level 4 & 5 | 94836 | 18.34 | 94589 | 18.36 | 247 | 12.61 | 2145 | 11.53 | 1944 | 11.50 | 201 | 11.89 | ||
| Level 6 & 7 | 49533 | 9.58 | 49432 | 9.60 | 101 | 5.16 | 714 | 3.84 | 634 | 3.75 | 80 | 4.73 | ||
| Missing data | 935 | 935 | ||||||||||||
| Other catastrophic illnesses | 0.318 | 0.158 | ||||||||||||
| No | 503285 | 97.15 | 501375 | 97.15 | 1910 | 97.55 | 18200 | 97.84 | 16554 | 97.89 | 1646 | 97.34 | ||
| Yes | 14773 | 2.85 | 14725 | 2.85 | 48 | 2.45 | 401 | 2.16 | 356 | 2.11 | 45 | 2.66 | ||
| Moderate to severe kidney disease | 0.218 | 0.085 | ||||||||||||
| No | 440556 | 85.04 | 438871 | 85.04 | 1685 | 86.06 | 16425 | 88.30 | 14954 | 88.43 | 1471 | 86.99 | ||
| Yes | 77502 | 14.96 | 77229 | 14.96 | 273 | 13.94 | 2176 | 11.70 | 1956 | 11.57 | 220 | 13.01 | ||
| CCI | <0.001 | 0.247 | ||||||||||||
| 0 | 8776 | 1.69 | 8751 | 1.70 | 25 | 1.28 | 233 | 1.25 | 212 | 1.25 | 21 | 1.24 | ||
| 1~3 | 129044 | 24.91 | 128410 | 24.88 | 634 | 32.38 | 6438 | 34.61 | 5881 | 34.78 | 557 | 32.94 | ||
| 4~6 | 148079 | 28.58 | 147421 | 28.56 | 658 | 33.61 | 6130 | 32.96 | 5581 | 33.00 | 549 | 32.47 | ||
| 7~9 | 125612 | 24.25 | 125197 | 24.26 | 415 | 21.20 | 3858 | 20.74 | 3493 | 20.66 | 365 | 21.58 | ||
| ≥10 | 106547 | 20.57 | 106321 | 20.60 | 226 | 11.54 | 1942 | 10.44 | 1743 | 10.31 | 199 | 11.77 | ||
| Average CCI (Mean, Std) | 6.33 | 3.78 | 6.33 | 3.78 | 5.41 | 3.39 | 5.18 | 3.29 | 5.15 | 3.28 | 5.43 | 3.42 | ||
| DCSI | <0.001 | 0.438 | ||||||||||||
| 0 | 359786 | 69.45 | 358301 | 69.42 | 1485 | 75.84 | 14358 | 77.19 | 13075 | 77.32 | 1283 | 75.87 | ||
| 1 | 79434 | 15.33 | 79144 | 15.34 | 290 | 14.81 | 2737 | 14.71 | 2480 | 14.67 | 257 | 15.20 | ||
| 2 | 52368 | 10.11 | 52232 | 10.12 | 136 | 6.95 | 1118 | 6.01 | 1009 | 5.97 | 109 | 6.45 | ||
| ≥3 | 26470 | 5.11 | 26423 | 5.12 | 47 | 2.40 | 388 | 2.09 | 346 | 2.05 | 42 | 2.48 | ||
| Average DCSI (Mean, Std) | 0.54 | 0.98 | 0.54 | 0.98 | 0.37 | 0.76 | 0.34 | 0.73 | 0.34 | 0.73 | 0.36 | 0.75 | ||
CCI, Charlson Comorbidity Index; DCSI, Diabetes Complications Severity Index; PS, propensity score. It’s 32 New Taiwan Dollar (NT$) per US dollar. Urbanization level of residence area (overall 7 levels; Level 1 was the most urbanized). The boldface indicated that p values less than 0.05 are considered statistically significant.
The number of nurses with newly diagnosed diabetes was less than the number of general patients with diabetes; this study used propensity score matching (PSM) with a 1:10 ratio (nurses: general patients) for objective analysis of the risks of dialysis. For comparison, the PSM is applied widely in the health care field,[17] to account for selection bias and obtain better participation effects on outcome compliance.
This result was calculated by logistic regression using the 7 covariates listed in Table 1. The majority of the variables were significantly different between the two groups. After propensity score matching, no significant differences were found in any variable between the two groups (P > 0.05, Table 1). Finally, the data of 18,601 study subjects were analyzed (nurses, n = 1691; general patients, n = 16,910).
2.3. Study design
This study defined diabetes as having diagnosis of diabetes (ICD-9-CM: 250 or A-code: A181) with three or more outpatient visits or one hospital admission within the past 365 days.[18] Patients with type 1 diabetes, gestational diabetes, neonatal diabetes and impaired glucose tolerance (ICD-9-CM: 6488, 7751, 7902, 6480) were excluded. Patients requiring dialysis within 90 days of their diabetes diagnosis were excluded. Patients younger than 20 years and older than 90 years were excluded. Dialysis was defined as follows: patients began dialysis treatments for more than three consecutive months after a new diagnosis of diabetes between 1998 and 2006.
Nurses were part of the registry for medical personnel from the NHI from 1998 to December 31, 2009. Patients who received nursing licenses after their diagnosis of diabetes were excluded. A general patient was defined as a patient who had not registered as a licensed medical professional, such as physicians, dentists, physical therapists, and nutritionists, before December 31, 2009.
The presence of other catastrophic illnesses were defined by the National Health Insurance Administration in Taiwan, including 30 categories of major illnesses (e.g., stroke, hemophilia, cancer, autoimmune diseases, chronic mental illness, congenital factor disorder, congenital hypothyroidism, etc.).[19] In this study, the presence of other catastrophic illnesses was classified as yes or no. According to Deyo et al.,[20] the Charlson comorbidity index (CCI) involves 17 comorbidities weighted based on severity. Additionally, the definition of diabetes complication severity index (DCSI) developed by Young et al.[21] was used, and complications observed upon diagnosis or prior to the last day of observation were identified.
2.4. Statistical analysis
This study used descriptive statistics to analyze the demographic characteristics, including age, insured salary, urbanization level of residence area (overall 7 levels; Level 1 was the most urbanized),[22] nurse status, comorbidity factors, CCI, and DCSI of the study population. To reduce the bias between the two groups, this study used the propensity score matching method with a ratio of 1:10 to generate matched study subjects before analyses. The chi-square test was used to compare the differences in ESRD requiring dialysis between the two groups of study subjects. A Cox proportional hazards model (Hazard ratio, HR) was used to compare relative risk and factors affecting dialysis. The Cox proportional hazards model was used to further analyze the related factors of nurses with newly diagnosed diabetes requiring dialysis. All the analyses were conducted using SAS 9.3 software (SAS Institute, NC, USA). In this study, the P values less than 0.05 were considered significant.
3. Results
3.1. Patient demographics
This study recruited nurses and general patients diagnosed with diabetes between 1998 and 2006. All subjects were observed for the relative risks of dialysis and were followed until the end of 2009. The mean follow-up time was 6.71 ± 2.61 years (nurses vs. general patients = 6.80 ± 2.60 vs. 6.70 ± 2.61).
In the recruitment period (Table 1), 518,058 female patients who were newly diagnosed with diabetes were included, among which 1,958 (0.38%) were nurses and 516,100 (99.62%) were general patients. In the two study populations, significant differences were found between age, insured salary, urbanization of residence, CCI and DCSI (P < 0.001).
The mean age of the nurses was younger than the age of the general patients (42.01 ± 12.03 years vs. 59.29 ± 13.11 years). Regarding the CCI and DCSI, the average CCI (5.41 ± 3.39) and DCSI (0.37 ± 0.76) of the nurses were lower than those of the general patients, indicating that compared with the general public diagnosed with diabetes, the nurses were healthier when newly diagnosed with diabetes (Table 1).
3.2. The relative risks of nurses with diabetes and general patients with diabetes requiring dialysis
Bivariate analysis after matching the two groups requiring dialysis suggested that the dialysis rate of nurses was lower than that of the general patients (0.35% vs. 1.11%) (Table 2) and the difference reached statistical significance (P < 0.05). After controlling for other factors, Cox proportional hazards models were used to identify the mortality rate for the nurses and general patients. The results in Table 3 and Fig. 1 show that nurses had a lower risk of dialysis than the general public (reference group) [adjusted hazard ratio(AHR)= 0.36, 95% confidence interval (CI) 0.16-0.81]. As shown in Table 3, patients with a higher CCI had a higher risk of dialysis compared to that of the reference group (CCI ≤ 3); when the CCI increased to ≥ 5, the risk of dialysis increased up to 5.64 times (95% CI 1.79-17.75). The DCSI demonstrated similar results; patients with a higher DCSI had a higher risk of dialysis compared to that of the reference group (DCSI = 0); when the DCSI increased to ≥ 3, the risk of dialysis increased up to 400.55 times (95% CI 55.72-2879.64).
Table 2.
- Bivariate analysis of nurses with diabetes and general patients with diabetes requiring dialysis.
| Variables | Total | Without Dialysis | With Dialysis | P-value | |||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Total patients | 18601 | 100.00 | 18408 | 98.96 | 193 | 1.04 | |
| Nurses or general patients | 0.005 | ||||||
| General | 16910 | 90.91 | 16723 | 98.89 | 187 | 1.11 | |
| Nurses | 1691 | 9.09 | 1685 | 99.65 | 6 | 0.35 | |
| Age | 0.247 | ||||||
| <25 | 1194 | 6.42 | 1185 | 99.25 | 9 | 0.75 | |
| 25-34 | 3214 | 17.28 | 3191 | 99.28 | 23 | 0.72 | |
| 35-44 | 5568 | 29.93 | 5503 | 98.83 | 65 | 1.17 | |
| 45-54 | 6059 | 32.57 | 5996 | 98.96 | 63 | 1.04 | |
| 55-64 | 1894 | 10.18 | 1870 | 98.73 | 24 | 1.27 | |
| ≥65 | 672 | 3.61 | 663 | 98.66 | 9 | 1.34 | |
| Average age (Mean, Std) | 44.14 | 11.86 | 44.12 | 11.86 | 46.05 | 11.81 | |
| Insured salary(NT$) | <0.001 | ||||||
| ≤17280 | 1829 | 9.83 | 1810 | 98.96 | 19 | 1.04 | |
| 17281~22800 | 4312 | 23.18 | 4258 | 98.75 | 54 | 1.25 | |
| 22801~28800 | 2011 | 10.81 | 1971 | 98.01 | 40 | 1.99 | |
| 28801~36300 | 2015 | 10.83 | 1997 | 99.11 | 18 | 0.89 | |
| 36301~45800 | 4128 | 22.19 | 4088 | 99.03 | 40 | 0.97 | |
| 45801~57800 | 2540 | 13.66 | 2527 | 99.49 | 13 | 0.51 | |
| ≥57801 | 1766 | 9.49 | 1757 | 99.49 | 9 | 0.51 | |
| Urbanization of residence | 0.135 | ||||||
| Level 1 | 6593 | 35.44 | 6537 | 99.15 | 56 | 0.85 | |
| Level 2 & 3 | 9149 | 49.19 | 9043 | 98.84 | 106 | 1.16 | |
| Level 4 & 5 | 2145 | 11.53 | 2125 | 99.07 | 20 | 0.93 | |
| Level 6 & 7 | 714 | 3.84 | 703 | 98.46 | 11 | 1.54 | |
| Other catastrophic illnesses | 0.937 | ||||||
| No | 17708 | 95.20 | 17525 | 98.97 | 183 | 1.03 | |
| Yes | 893 | 4.80 | 883 | 98.88 | 10 | 1.12 | |
| Moderate to severe kidney disease | <0.001 | ||||||
| No | 15240 | 81.93 | 15233 | 99.95 | 7 | 0.05 | |
| Yes | 3361 | 18.07 | 3175 | 94.47 | 186 | 5.53 | |
| CCI | <0.001 | ||||||
| ≤3 | 4100 | 22.04 | 4097 | 99.93 | 3 | 0.07 | |
| 4 | 1928 | 10.37 | 1919 | 99.53 | 9 | 0.47 | |
| ≥5 | 12573 | 67.59 | 12392 | 98.56 | 181 | 1.44 | |
| Average CCI (Mean, Std) | 6.53 | 3.59 | 6.51 | 3.58 | 8.71 | 3.23 | |
| DCSI | <0.001 | ||||||
| 0 | 8687 | 46.70 | 8686 | 99.99 | 1 | 0.01 | |
| 1 | 4966 | 26.70 | 4964 | 99.96 | 2 | 0.04 | |
| 2 | 2730 | 14.68 | 2688 | 98.46 | 42 | 1.54 | |
| ≥3 | 2218 | 11.92 | 2070 | 93.33 | 148 | 6.67 | |
| Average DCSI (Mean, Std) | 1.01 | 1.29 | 0.98 | 1.25 | 3.97 | 1.65 | |
CCI, Charlson Comorbidity Index; DCSI, Diabetes Complications Severity Index.
It’s 32 New Taiwan Dollar (NT$) per US dollar.
Urbanization level of residence area (overall 7 levels; Level 1 was the most urbanized).
The boldface indicated that p values less than 0.05 are considered statistically significant.
Table 3.
- The relative risks of nurses with diabetes and general patients with diabetes requiring dialysis.
| Variables | Unadj. HR | P-value | Adj. HR | 95% CI | P-value | |
|---|---|---|---|---|---|---|
| Nurses or general patients | ||||||
| General (reference) | ||||||
| Nurses | 0.31 | 0.005 | 0.36 | 0.16 | 0.81 | 0.013 |
| Age | ||||||
| < 25 (reference) | ||||||
| 25-34 | 0.99 | 0.982 | 0.63 | 0.29 | 1.37 | 0.240 |
| 35-44 | 1.50 | 0.256 | 0.75 | 0.37 | 1.54 | 0.436 |
| 45-54 | 1.50 | 0.253 | 0.58 | 0.28 | 1.18 | 0.134 |
| 55-64 | 1.93 | 0.094 | 0.50 | 0.23 | 1.10 | 0.087 |
| ≥65 | 2.30 | 0.077 | 0.37 | 0.14 | 0.94 | 0.037 |
| Insured salary (NT$) | ||||||
| ≤17280 (reference) | ||||||
| 17281~22800 | 1.51 | 0.121 | 1.44 | 0.84 | 2.45 | 0.182 |
| 22801~28800 | 1.52 | 0.132 | 1.24 | 0.71 | 2.15 | 0.447 |
| 28801~36300 | 0.78 | 0.445 | 0.66 | 0.35 | 1.27 | 0.213 |
| 36301~45800 | 0.83 | 0.496 | 0.77 | 0.44 | 1.33 | 0.350 |
| 45801~57800 | 0.44 | 0.023 | 0.45 | 0.22 | 0.91 | 0.026 |
| ≥57801 | 0.52 | 0.107 | 0.57 | 0.25 | 1.26 | 0.164 |
| Urbanization of residence | ||||||
| Level 1 (reference) | ||||||
| Level 2 & 3 | 1.35 | 0.069 | 1.09 | 0.79 | 1.51 | 0.605 |
| Level 4 & 5 | 1.01 | 0.979 | 0.76 | 0.45 | 1.28 | 0.297 |
| Level 6 & 7 | 1.70 | 0.109 | 1.01 | 0.52 | 1.95 | 0.987 |
| Other catastrophic illnesses | ||||||
| No (reference) | ||||||
| Yes | 1.03 | 0.920 | 0.71 | 0.37 | 1.34 | 0.287 |
| CCI | ||||||
| (reference) | ||||||
| 4 | 5.77 | 0.009 | 3.83 | 1.04 | 14.18 | 0.044 |
| ≥5 | 16.45 | <0.001 | 5.64 | 1.79 | 17.75 | 0.003 |
| DCSI | ||||||
| 0 (reference) | ||||||
| 1 | 3.26 | 0.334 | 2.94 | 0.27 | 32.42 | 0.380 |
| 2 | 117.76 | <0.001 | 103.01 | 14.14 | 750.60 | <0.001 |
| ≥3 | 475.45 | <0.001 | 400.55 | 55.72 | 2879.64 | <0.001 |
CCI, Charlson Comorbidity Index; DCSI, Diabetes Complications Severity Index;
HR, hazard ratio; CI, confidence interval.
It’s 32 New Taiwan Dollar (NT$) per US dollar.
Urbanization level of residence area (overall 7 levels; Level 1 was the most urbanized).
The boldface indicated that p values less than 0.05 are considered statistically significant.
Fig. 1.
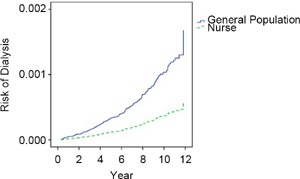
- The relative risk of requiring dialysis between nurses with diabetes and general patients with diabetes (Cox proportional hazards model was used to control for age, monthly salary, urbanization of residence, other catastrophic illnesses, CCI and DCSI.)
3.3. Relative factors of nurses with diabetes requiring dialysis
As shown in Table 4, there were no significant differences between relative factors affecting nurses with diabetes requiring dialysis and those not requiring dialysis, including age, insured salary, urbanization of residence and CCI (P > 0.05); only the DCSI was significantly different (P < 0.05). If nurses had a DCSI ≥ 3, the risk of dialysis increased up to 83.53 times (95% CI 6.211123.59) that of the reference group (DCSI < 3).
Table 4.
- Relative factors of nurses with diabetes requiring dialysis.
| Variables | Unadj. HR | P-value | Adj. HR | 95% CI | P-value | |
|---|---|---|---|---|---|---|
| Age | ||||||
| <35 (reference) | ||||||
| 35-44 | 0.72 | 0.747 | 0.25 | 0.02 | 2.96 | 0.269 |
| ≥45 | 0.54 | 0.538 | 0.16 | 0.01 | 1.99 | 0.154 |
| Insured salary(NT$) | ||||||
| ≤17280 (reference) | ||||||
| 17281~22800 | 0.50 | 0.626 | 0.18 | 0.01 | 4.31 | 0.287 |
| 22801~28800 | 0.61 | 0.723 | 0.29 | 0.02 | 5.52 | 0.411 |
| 28801~36300 | 0.70 | 0.804 | 0.36 | 0.02 | 6.50 | 0.486 |
| ≥36301 | 0.36 | 0.403 | 0.18 | 0.01 | 2.34 | 0.188 |
| Urbanization of residence | ||||||
| Level 1 | ||||||
| Level 2 & 3 | 1.45 | 0.760 | 0.99 | 0.08 | 11.77 | 0.992 |
| Level 4 & 5 & 6 & 7 | 5.58 | 0.137 | 5.37 | 0.51 | 56.81 | 0.163 |
| CCI | ||||||
| < 5 (reference) | ||||||
| ≥5 | 1.72 | 0.621 | 0.45 | 0.03 | 6.11 | 0.549 |
| DCSI | ||||||
| < 3 (reference) | ||||||
| ≥3 | 35.38 | 0.001 | 83.53 | 6.21 | 1123.59 | <0.001 |
CCI, Charlson Comorbidity Index; DCSI, Diabetes Complications Severity Index;
HR, hazard ratio; CI, confidence interval.
It’s 32 New Taiwan Dollar (NT$) per US dollar.
Urbanization level of residence area (overall 7 levels; Level 1 was the most urbanized).
The boldface indicated that p values less than 0.05 are considered statistically significant.
5. Discussion
Because few studies have examined professional groups and their performance-related behavior, the majority of studies have used small samples or questionnaires. This is the first study using nationwide data to analyze whether the increased knowledge and resources available to nurses led to a difference in dialysis treatment between nurses and the general patients.
The results of the present study showed that the nurses were younger than the general patients (mean age 42.01 years vs. 59.29 years, respectively). The result was similar to that of previous studies.[23] The results suggesting that the shift work of nurses may contribute to developing diabetes at a younger age than the general public.[24] A correlation study of shift work and metabolic diseases conducted by Karlsson et al.[25] found that female shift workers had a higher risk of acquiring metabolic diseases than day-shift workers. However, this result may be due to screening bias; the nurses could have received the diagnosis prematurely and/or the others received it later because the awareness of the disease could be more pronounced among the nurses due to their medical knowledge. Additionally, the nurses could be more aware of the importance of preventive strategies once the disease was diagnosed, giving them a better prognosis compared to the general population. This result was similar to the conclusions in terms of their DCSI score (nursing vs. general patients = 0.37 ± 0.76 vs. 0.54 ± 0.98, Table 1).
The results in Tables 1 indicated that for the general population with newly diagnosed with diabetes aged ≧ 55 years are totally about 61.51%, but are only 12% in nurses with newly diagnosed with diabetes; this could be largely because nurses >55 year old has stopped working or stopped maintaining their licenses. This phenomenon is known as the healthy worker effect [26, 27]. Nurses must have excellent health to achieve effective performance; therefore, nurses are generally healthier than are the general population.
Because the database did not contain the related information of medication knowledge, we used propensity score matching. The nurse cohort and the general patient control group were similar in terms of demographics, health status, and their socioeconomic status (P > 0.05). The two groups may have differed in terms of their knowledge, attitude, and practice of health care. In the present study, the results of the bivariate analysis of nurses with diabetes and general patients with diabetes requiring dialysis found that nurses had a lower ratio of dialysis (0.35% vs. 1.11%) than that of patients in the general population. A Cox proportional hazards model was used to further analyze the data, and nurses had a lower risk of dialysis (AHR = 0.36) compared to general patients.
These results may be related to nurses having additional medical knowledge, as an individual’s perception of health or diseases and attitudes regarding medical care have been shown to affect health maintenance.[28] Many reports have described whether patients who received diabetes education and had self-management have significantly improved outcomes and reduced progression to dialysis.[29, 30] Nurses have a dual role of caregiver and care demander. They have additional medical care knowledge compared to the general patients, thus they may develop more positive and active disease care attitudes. They may be less sus ceptible to ESRD and have a lower risk of dialysis.
Previous studies of disease care behaviors of medical personnel and the general public found that when medical personnel sought medical care, it was based on previous personal experience with cases and personal experience seeking an informal consultation or formal treatment recommendations from colleagues. [31] After extensively collecting related information, they would then perform self-care behavior. When nurses have chronic diseases, their medical knowledge can strengthen their self-care abilities and change their lifestyles, which may result in better outcomes[32] and delay disease progression.
In the analysis of relative risk of dialysis in nurses with diabetes, only DCSI was a related factor affecting whether nurses would ultimately require dialysis. The result was similar to that of previous studies[33], which showed that the DCSI was an important determining factor of dialysis. Nurses had similar and consistent knowledge and socioeconomic status, and the DCSI was a determining factor of nurses with diabetes requiring dialysis.
5.1. Limitations
This study has several limitations. First, the NHIRD used the ICD-9 to define diabetes; however, these data could not be validated because no clinical data could be obtained. This study used a strict diagnosis identification, and we defined diabetes as diagnosis of diabetes (ICD-9-CM: 250 or A-code: A181) in three outpatient visits or one inpatient visit in the past 365 days, as previously described.[18] The high standard was adopted to compensate for this limitation. Second, the NHIRD did not have the related information of “lifestyle of patient,” “health behavior” and “correlation of these interventions with glycemic control,” and therefore, none of these could be included in the variables. This lack of information affected the discussion and reasoning of disease variations. However, we clearly defined the DM population and used the propensity score method to match the nurses and general population to avoid selection bias. The propensity score adjustment is an important statistical technique to reduce the bias from confounding variables in observational studies and mimic the results of a randomized controlled trial.[17] Third, because each nurse’s number of years of service and shift lengths was unknown, the correlation between their shift work and diabetes or dialysis risk could not be determined.
6. Conclusion
Nurses with newly diagnosed diabetes were younger than the general people with diabetes but had a lower risk of dialysis. This finding suggests that nurses may receive a more complete medical education and have additional disease care knowledge than the general public, and they may be more able to change their lifestyles. Thus, they have a lower risk of dialysis than the general population with diabetes.
Diabetes is an incurable but manageable chronic disease. The pathogenesis is complex. Regardless of whether patients are medical personnel or the general public, when they are facing the treatment of chronic disease, their self-care ability and psychological adjustment must be considered in addition to medical perspectives. An integrated care model is necessary. The results of this study could serve as a reference for developing health education programs.
Conflicts of interest
The authors declare no conflicts of interest.
Acknowledgments
This study was supported by grants (CMU102-ASIA-12, DOH10541) from China Medical University and Asia University and Ministry of Health and Welfare. We are grateful for use of the National Health Insurance Research Database provided by the National Health Research Institutes. All interested researchers can obtain the databases published and managed by the NHRI. Before using the databases for research, all studies should get the IRB permission. The interpretations and conclusions contained herein do not represent those of the Ministry of Health and Welfare, Taiwan, R.O.C.
References
- 1.Foundation NK. Introduction to Volume One: 2013 USRDS Annual Data Report Atlas of Chronic Kidney Disease in the United States. Am J Kidney Dis (AJKD). 2013; 63: e1-e22. [Google Scholar]
- 2.Molitch M, DeFronzo R, Franz M, Keane W, Mogensen C, Parving H, et al. Nephropathy in diabetes. Diabetes care. 2004; 27: S79-83. [DOI] [PubMed] [Google Scholar]
- 3.Guariguata L, Whiting D, Hambleton I, Beagley J, Linnenkamp U, Shaw J. Global estimates of diabetes prevalence for 2013 and projections for 2035 for the IDF Diabetes Atlas. Diabetes Res Clin Pract. 2013. [DOI] [PubMed] [Google Scholar]
- 4.International Diabetes Federation (IDF). About diabetes. Risk factors. Available at http://www.idf.org. Accessed October 20, 2016. [Google Scholar]
- 5.Vazini H, Barati M. The Health Belief Model and Self-Care Behaviors among Type 2 Diabetic Patients. Iranian J Diabetes & Obesity (IJDO). 2014; 6. [Google Scholar]
- 6.Heider D, Matschinger H, Müller H, Saum K-U, Quinzler R, Haefeli WE, et al. Health care costs in the elderly in Germany: an analysis applying Andersen’s behavioral model of health care utilization. BMC health services research. 2014; 14: 71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kopelowicz A, Zarate R, Wallace CJ, Liberman RP, Lopez SR, Mintz J. Using the Theory of Planned Behavior to Improve Treatment Adherence in Mexican Americans With Schizophrenia. 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Vilhjalmsson R, Gudmundsdottir G. Psychological distress and professional help-seeking: a prospective national study. Scand J Caring Sci. 2014; 28: 273-80. [DOI] [PubMed] [Google Scholar]
- 9.Bhargava A, Mishra B, Thakur A, Dogra V, Loomba P, Gupta S. Assessment of knowledge, attitude and practices among healthcare workers in a tertiary care hospital on needle stick injury. Int J Health Care Qual Assur. 2013; 26: 549-58. [DOI] [PubMed] [Google Scholar]
- 10.Sloan FA. Arrow’s concept of the health care consumer: a forty-year retrospective. J Health Polit Policy Law. 2001; 26: 899-911. [DOI] [PubMed] [Google Scholar]
- 11.Pineau Stam LM, Spence Laschinger HK, Regan S, Wong CA. The influence of personal and workplace resources on new graduate nurses' job satisfaction. J Nurs Manag. 2015; 23: 190-199. [DOI] [PubMed] [Google Scholar]
- 12.Mehta R, Singh I. Stress among nurses working in critical care areas at a tertiary care teaching hospital, Nepal. J Chitwan Med College. 2015; 4: 42-48. [Google Scholar]
- 13.Gangwisch JE, Rexrode K, Forman JP, Mukamal K, Malaspina D, Feskanich D. Daytime sleepiness and risk of coronary heart disease and stroke: results from the Nurses' Health Study II. Sleep medicine. 2014; 15: 782-788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bureau of Health promotion DoH, R.O.C.(Taiwan). Statistics & Surveys In: Insurance Coverage; 2013. National Health insurance Administration, Ministry of Health and Welfare. Statistics & Surveys Available at: http://www.nhi.gov.tw/English/webdata. Accessed November 25, 2016. [Google Scholar]
- 15.Cheng T-M. Taiwan’s new national health insurance program: genesis and experience so far. Health Affairs. 2003; 22: 61-76. [DOI] [PubMed] [Google Scholar]
- 16.Hsu Y-Y, Tang W-R, Chang Y-C, Maa S-H. A preliminary study of the work values of male nurses in Taiwan and related factors. Hu Li Za Zhi. 2013; 60: 50. [DOI] [PubMed] [Google Scholar]
- 17.Wilson FP, Yang W, Machado CA, Mariani LH, Borovskiy Y, Berns JS, et al. Dialysis versus nondialysis in patients with AKI: A propensity-matched cohort study. Clin J Am Soc Nephrol. 2014; 9: 673-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chang C, Shau W, Jiang Y, Li H, Chang T, H-H Sheu W, et al. Type 2 diabetes prevalence and incidence among adults in Taiwan during 1999-2004: a national health insurance data set study. Diabetic Medicine. 2010; 27: 636-43. [DOI] [PubMed] [Google Scholar]
- 19.National Health insurance Administration, Ministry of Health and Welfare. Reglations governing the exemption of the national heaelth insurance beneficiaries from co-payment. Available at: http://www. nhi.gov.tw. Accessed November 2, 2016. [Google Scholar]
- 20.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992; 45: 613-9. [DOI] [PubMed] [Google Scholar]
- 21.Young BA, Lin E, Von Korff M, Simon G, Ciechanowski P, Ludman EJ, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care. 2008; 14: 15. [PMC free article] [PubMed] [Google Scholar]
- 22.Liu C, Hung Y, Chuang Y, Chen Y, Weng W, Liu J, et al. Incorporating development stratification of Taiwan townships into sampling design of large scale health interview survey. J Health Manage. 2006; 4: 1-22. [Google Scholar]
- 23.Huang H-L, Pan C-C, Wang S-M, Kung P-T, Chou W-Y, Tsai W-C. The incidence risk of type 2 diabetes mellitus in female nurses: a nationwide matched cohort study. BMC public health. 2016, 16: 443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pan A, Schernhammer ES, Sun Q, Hu FB. Rotating night shift work and risk of type 2 diabetes: two prospective cohort studies in women. PLoS Med. 2011, 8: e1001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Karlsson B, Knutsson A, Lindahl B. Is there an association between shift work and having a metabolic syndrome? Results from a population based study of 27 485 people. Occup Environ Med. 2001, 58: 747-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naimi AI, Richardson DB, Cole SR. Causal Inference in Occupational Epidemiology: Accounting for the Healthy Worker Effect by Using Structural Nested Models. Am J Epidemiol. 2013: kwt215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Radon K, Goldberg M, Becklake M. Healthy worker effect in cohort studies on chronic bronchitis. Scand J Work Environ Health. 2002: 328-32. [DOI] [PubMed] [Google Scholar]
- 28.Andersen R, Newman JF. Societal and individual determinants of medical care utilization in the United States. The Milbank Memorial Fund Quarterly. Health and Society. 1973: 95-124. [PubMed] [Google Scholar]
- 29.Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-Management education for adults with type 2 Diabetes A metaanalysis of the effect on glycemic control. Diabetes Care. 2002, 25: 1159-71. [DOI] [PubMed] [Google Scholar]
- 30.McMurray SD, Johnson G, Davis S, McDougall K. Diabetes education and care management significantly improve patient outcomes in the dialysis unit. Am J Kidney Dis. 2002, 40: 566-75. [DOI] [PubMed] [Google Scholar]
- 31.Aasland OG, Hem E, Haldorsen T, Ekeberg Ø. Mortality among Norwegian doctors 1960-2000. BMC public health. 2011, 11: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jallinoja P, Absetz P, Kuronen R, Nissinen A, Talja M, Uutela A, et al. The dilemma of patient responsibility for lifestyle change: perceptions among primary care physicians and nurses. Scand J Prim Health Care. 2007, 25: 244-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yu H-C, Tsai W-C, Kung P-T. Does the pay-for-performance programme reduce the emergency department visits for hypoglycaemia in type 2 diabetic patients? Health policy and planning. 2014, 29: 732-41. [DOI] [PubMed] [Google Scholar]


