Abstract
Introduction
Tuberculosis outbreaks emerge occasionally in long-term care facilities and various educational establishments. This study was designed to determine the five year overall prevalence and trend of tuberculosis and associated factors among students at Adama Science and Technology University and Addis Ababa University Sidist Kilo campus.
Methods
A five-year retrospective study was conducted on students medical records of tuberculosis Directly Observed Treatment Short Course clinics from September 2009 – July 2014. The overall prevalence and the trend of smear positive, smear negative and extra pulmonary tuberculosis cases was determined. Odds ratio with 95 percent confidence interval was calculated for categorical variables using a multivariate logistic regression model to assess the strength of association.
Results
A total of 112 and 263 tuberculos cases were recorded in Addis Ababa University Sidist Kilo campus and Adama Science and Technology University, respectively. The mean proportion of tuberculosis cases of all types among the total number of students enrolled at Adama Science and Technology University and Addis Ababa University Sidist Kilo campus was 1098.1 and 511.7 cases per 100,000 population, respectively. There was a statistically significant difference in prevalence of tuberculosis among students in Adama Science and Technology University compared to that in Addis Ababa University Sidist Kilo campus [adjusted odds ration: 2.881, 95% CI (1.76–4.71)]. The trend of tuberculosis prevalence showed a steady decline from the first to the last year of the study period.
Conclusion
The number of tuberculosis cases observed among university students in this study was high. Governmental and nongovernmental agencies involved in tuberculosis control must consider higher education institutions as focal points for prevention and elimination of tuberculosis in Ethiopia.
Keywords: Prevalence, Trend, University-students, daily observed therapy Short course-Clinic, Universities
INTRODUCTION
Mycobacterium tuberculosis (MTB) may be regarded as the most successful intracellular bacterium worldwide, in view of its global prevalence and distribution. Globally, MTB ranks as the second leading cause of death from a single infectious agent, after the human immunodeficiency virus (HIV) (1). Despite availability of anti-tuberculous drugs for the last 50 years, MTB is responsible for 1.5 million deaths every year with about one third of the world population having been in contact and latently infected (2). Today, tuberculosis (TB) incidence is 100 times higher than the elimination target for 2050. The long term goal has been established to eliminate TB as a public health problem by 2050 by reducing the incidence to less than one case per one million population (3).
Tuberculosis has the potential to affect all people regardless of sex and age; different groups of people have a variable chance to contract the infection and to develop the disease. It predominantly occurs among young adults; where approximately 75% of all tuberculosis cases arise coinciding with people s most productive years, between the ages of 15 and 54 years. As a result, tuberculosis is a major economic stress for poor families worldwide (4).
Historically, schools have been the settings for numerous outbreaks of TB (5). College students are usually 18–23 years old, characterized by rapid physical development and endocrine instability, and reports have revealed that the incidence of pulmonary TB (PTB) starts to rise greatly during this period (6).
TB outbreaks emerge occasionally in long-term care facilities and various educational establishments. Boarding schools are sites where adolescents are concentrated in conditions of relative overcrowding predisposing to TB outbreaks (7). The crowded situation both in classrooms and dormitories increases the risk of exposure to TB infections. A person with active but untreated TB can infect 10–15 people per year (8). Thus such kinds of congregated settings should be a target to implement TB infection control measures.
In Ethiopia, tuberculosis is the leading cause of morbidity, and the third highest cause of hospital admission and the second highest cause of death after malaria (9). The expansion of Higher Education Institutions from less than 5 federal universities to 32 in the last decades has significantly increased the number of undergraduate students joining public Universities, but the infrastructure of the universities has not kept pace with the expansion (10). This in turn forces students to spend their 3–6 years of University life in a crowded living environment, where there are more than 20 students per dormitory; 100–200 students per class room; and 2000–5000 students in a single dining hall who congregate for meals three times a day (8).
Thus, the living conditions in dormitories of Ethiopian Universities could be favorable for TB transmission. However, there is no compiled report on the magnitude and trend of tuberculosis in the higher education institutions of Ethiopia. Therefore, the study was designed to determine the five year overall prevalence and trend of tuberculosis and to identify factors associated with the occurrence of tuberculosis among students at Adama Science and Technology University and Addis Ababa University, Sidist Kilo campus, from September 2009 to July 2014. Since the implementation of quality laboratory diagnostic system would influence the actual number of infectious or non-infectious disease cases identified in any of the study population, the AFB sputum smear examination practices of the respective university laboratories were assessed using the WHO standard checklist.
MATERIALS AND METHODS
The study was conducted at Addis Ababa University (AAU) Sidist Kilo campus and at Adama Science and Technology University (ASTU) in Oromia region, central Ethiopia. Addis Ababa University is located in Addis Ababa, the capital city of Ethiopia, and the Sidist Kilo campus is the main campus of the University, while Adama Science and Technology University is located in Adama/Nazreth 100km to the east of Addis Ababa. The data collection was conducted from April to June/2015. These Universities were selected for the study due to ease of access and convenience.
A retrospective record review was conducted at the AAU Sidist Kilo campus and ASTU Directly Observed Treatment Short Course (DOTS) TB clinics from September 2009 – July 2014, this time frame roughly corresponds to the start and end of the regular academic calendar year for Ethiopian Universities. All student patients who visited the student health service facility of the higher education institution in the specified period were the source population of this study, from which all tuberculosis cases were used as a study population. Prevalence was calculated from the total number of student population who were by then registered in the respective study University registrar office. Furthermore, the proportion of TB cases among the total number of students who visited the university clinics for various kinds of ill-health was determined.
Individuals with complete data in the DOTS register including age, sex, and type of pulmonary TB were included whereas, individuals with incomplete information for the data required were excluded from the analysis. Data were collected by trained nurses under intensive supervision by the principal investigator of the study. The data collectors were given training on how to extract data from students medical history using the data collection format. Pre-testing of data collection tools were conducted before the actual data collection took place. The data were checked for correctness and completeness on site. Verified data were transferred into SPSS version 22 statistical package and analyzed. P<0.05 was considered to be statistically significant.
Laboratory assessment
In order to assess whether a standard laboratory diagnostic system for tuberculosis case detection was in place or not, an in-depth interview using the World Health Organization's (WHO) TB lab assessment tool was conducted with the heads of the respective University Clinic labs.
Ethical considerations
Ethical approval was obtained from the Institutional Review Board of AAU, College of Natural Sciences. Research and support letters were obtained from the respective Universities . Full confidentiality was maintained during the study and analysis was done without inclusion of names.
RESULTS
A combined total of 375 TB cases was recorded in the five year period at both AAU Sidist Kilo campus and ASTU clinics. The majority (89.9%) of the cases were male with a mean age of 21.3 (SD+ 1.91) years and range of 18–27 years. More TB cases were detected in ASTU (263 or 70% of all) than in AAU Sidist Kilo campus (29%). The difference was statistically significant [adjusted odds ratio (AOR): 2.88, 95% CI (1.76–4.71)]. TB was also significantly more prevalent in the academic year, 2011/12; AOR of 3.08 [95% CI (1.49–6.36)]. No significant difference was observed with other variables studied (Table 1).
Table 1.
Distribution of tuberculosis cases among university students by age, sex and academic year at Addis Ababa University Sidist Kilo campus and Adama Science & technology University, 2009 – 2014.
| Characteristics | Total No. of TB cases | Smear Positive cases no. (%)¥ | AOR (95% CI) |
|---|---|---|---|
| Sex | |||
| Male | 337 | 99 (29.4) | 1 |
| Female | 38 | 14 (36.8) | 0.492 (0.233–1.041) |
| Age group (years) | |||
| 18–20 | 165 | 53 (32.1) | 1 |
| 21–23 | 156 | 43 (27.6) | 1.283 (0.770–2.136) |
| >24 | 54 | 17 (31.5) | 1.148 (0.571–2.311) |
| Study University | |||
| Addis Ababa 6 Kilo campus | 112 | 50 (44.6) | 1 |
| Adama Science and Technology | 263 | 63 (23.9) | 2.881(1.763–4.707)** |
| Academic Year | |||
| 2009/10 | 122 | 43 (35.2) | 1 |
| 2010/11 | 83 | 28 (33.7) | 1.022 (0.557–1.874) |
| 2011/12 | 82 | 13 (15.9) | 3.077 (1.488–6.363)* |
| 2012/13 | 49 | 17 (34.7) | 0.860 (0.416–1.778) |
| 2013/14 | 39 | 12 (30.7) | 1.156 (0.514–2.601) |
AOD: adjusted Odds Ratio; CI: Confidence Interval
p<0.001;
p<0.05
The percentage is calculated from the total examined for the respective characteristic.
The mean prevalence rate of TB cases of all types for ASTU was 1.12% (1098.1 cases per 100,000 population), ranging from 0.5% to 1.8% (521.6 to 1814.1 cases per 100,000 population); whereas the mean prevalence rate of TB cases of all types for AAU Sidist Kilo campus was 0.54% (511.7 cases per 100,000 population), ranging from 0.4% to 0.7% (348.4 to 619.2 cases per 100,000 population). As shown in Table 2, the number of TB cases per 100,000 population in the respective University was higher than the national prevalence rate for the corresponding years. ASTU had three times higher than the respective national TB prevalence rate in 2009/10 calendar year (Table 2). The proportion of TB cases of all types from the total number of students who visited and obtained health services for various types of illnesses ranged from 1.3% to 4.4% for ASTU, and from 0.7% to 2.3% for AAU Sidist Kilo campus (Table-3).There was a difference in the proportion of different forms of tuberculosis between the two universities. The most prevalent type of tuberculosis cases observed at AAU Sidist Kilo campus was smear positive TB (Table 4). By contrast, the most prevalent form of TB at ASTU was extra pulmonary TB.
Table 2.
Prevalence of TB among university students at AAU Sidist Kilo campus and ASTU by academic year, 2009 – 2014.
| Year | ASTU | AAU Sidist Kilo campus | ||||
|---|---|---|---|---|---|---|
| Total No. of students enrolled | No. of TB Cases | TB Prevalence in percent (per 100,000 population) | Total No. of students enrolled | No. of TB Cases | TB Prevalence in percent (per 100,000 population) | |
| 2009/10 | 4465 | 81 | 1.8 (1814.1) | 6868 | 41 | 0.6 (596.9) |
| 2010/11 | 4967 | 58 | 1.2 (1167.7) | 4764 | 25 | 0.5 (524.8) |
| 2011/12 | 4647 | 58 | 1.3 (1248.1) | 3876 | 24 | 0.7 (619.2) |
| 2012/13 | 5278 | 39 | 0.8 (738.9) | 2870 | 10 | 0.4 (348.4) |
| 2013/14 | 5176 | 27 | 0.5 (521.6) | 2558 | 12 | 0.5 (469) |
Table 3.
Proportion of TB cases among students who visited the university clinics at AAU Sidist Kilo campus and ASTU for various illnesses, 2009 – 2014.
| Year | ASTU | AAU Sidist Kilo campus | ||||
|---|---|---|---|---|---|---|
| No. of students who visited the clinic | No. of TB Cases | Proportion of clinic students with TB | No. of students who visited the clinic | No. of TB Cases | Proportion of clinic students with TB | |
| 2009/10 | 1856 | 81 | 4.4% | 1812 | 41 | 2.3% |
| 2010/11 | 2312 | 58 | 2.5% | 1499 | 25 | 1.7% |
| 2011/12 | 1978 | 58 | 2.9% | 1803 | 24 | 1.3% |
| 2012/13 | 2343 | 39 | 1.7% | 1426 | 10 | 0.7% |
| 2013/14 | 2102 | 27 | 1.3% | 1343 | 12 | 0.9% |
Table 4.
Types of TB cases among University students atAAU Sidist Kilo campus and ASTU, 2009 – 2014.
| Type of TB | University | Total No. (%) | |
|---|---|---|---|
| AAU Sidist Kilo Campus No. (%) | ASTU No. (%) | ||
| Smear positive TB case | 50 (44.6) | 63 (24) | 113 (30.1) |
| Smear negative TB case | 27 (24.1) | 93 (35.4) | 120 (32) |
| Extra Pulmonary TB case | 35 (31.3) | 107 (40.6) | 142 (37.9) |
|
| |||
| Total | 112 | 263 | 375 (100) |
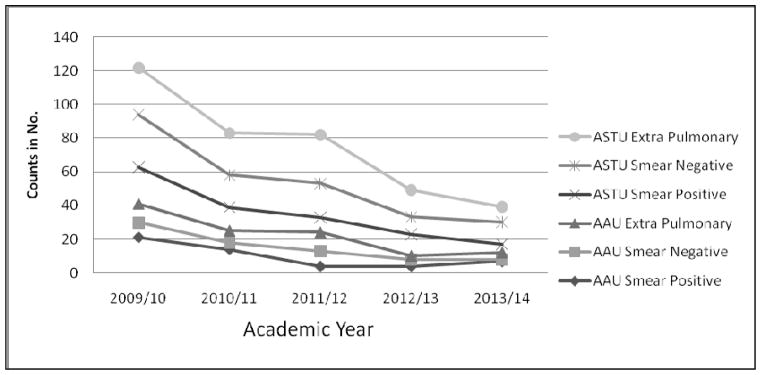
Extra pulmonary TB was predominant among all cases of TB detected, 142 (37.9%), followed by smear negative and smear positive TB cases each accounting for 120 (32.0%) and 113 (30.1%) of cases, respectively (Table 4). The number and type of TB cases showed a steady decrease from the first to the last year of the study period at both Universities (Figure and Table 4).
Figure 1.
Trend of tuberculosis among university students at Addis Ababa University Sidist Kilo campus and Adama Science Technology University, 2009 – 2014.
The highest prevalence of smear positive TB cases was recorded in the academic calendar year 2009/10. However, the highest prevalence of smear negative and extra pulmonary TB cases was observed in the years 2011/12 and 2012/13, respectively (Table 5).
Table 5.
Proportion of forms of TB among university students at AAU Sidist Kilo campus and Adama Science Technology University by academic calendar years, 2009 – 2014.
| Types of TB cases | ||||
|---|---|---|---|---|
| Academic Calendar Year | Smear positive N (%) | Smear negative N (%) | Extra pulmonary N (%) | Total |
| 2009/10 | 43(35.2) | 40 (32.8) | 39 (31.9) | 122 (100) |
| 2010/11 | 28 (33.7) | 23 (27.7) | 32 (38.6) | 83 (100) |
| 2011/12 | 13 (15.9) | 29 (35.4) | 40 (48.8) | 82 (100) |
| 2012/13 | 17 (34.7) | 14 (28.5) | 18 (36.7) | 49 (100) |
| 2013/14 | 12 (30.7) | 14 (35.8) | 13 (33.3) | 39 (100) |
|
| ||||
| Total | 113 (30.1) | 120 (32) | 142 (37.9) | 375 (100) |
The TB laboratory assessment indicated that the University TB laboratories were structurally separated from the national tuberculosis program as there were no quality assurance lab services undertaken by any responsible agency. As a result, the answers from heads of the respective laboratories for almost all quality measure questions indicated in WHO s Tuberculosis Laboratory Assessment tool (3rd draft, 2002) were no (data not shown). Both laboratory heads in the study University clinics reported that university TB laboratory technicians have not received basic in-service training on either sputum smear microscopy or on safe laboratory practices. These are courses which are frequently provided for their colleague lab professionals in other government health centers and hospitals.
DISCUSSION
A high prevalence of TB of all types among students at two universities in Ethiopia was revealed in this study. The study provides the first report on TB prevalence among university students in central Ethiopia. The findings showed a high TB prevalence ranging from 348.4 to 1814.1 cases per 100,000 population in both universities. It should be noted that occurrence of even a single case of contagious tuberculosis in a college campus is reason for anxiety and concern for students, parents, and Faculty (11). It should be noted that the prevalence rates indicated in this study might actually underestimate the actual burden of the disease in the universities studied. This is because a considerable number of cases might have been diagnosed elsewhere and obtained the DOTS service in private health facilities and/or in other health institutions of preference to students to avoid stigma. Another reason is that incomplete documentation was excluded from analysis here but retained in the number of total student population and those visiting the university clinic for other reasons. An important limitation of this study is again that prevalence is calculated against a total student population that has not been actively screened. The study assumes that those who did not seek health care were free from illness. This could underestimate the true prevalence of TB.
TB prevalence at these two higher education institutions was considerably higher than the national TB prevalence for the corresponding years, although there are limitations when making such comparisons (12). The national TB prevalence data were also not age-matched for the group of interest in this study. Even so, what the data here show is that there is an unacceptably high TB prevalence among university students. Like other congregate settings, higher education institutions can facilitate the transmission of TB as well as other air-borne infections. Several studies indicate that students at higher education institutions tend to be exposed to TB due to congested settings in both dormitories and classrooms (5). It is also possible that TB acquired outside the university campus may get reactivated in students under stress.
The TB prevalence in this study is higher than that reported for university students in Gondar, in northwest Ethiopia (8). As an example, the highest TB prevalence reported by the College of Health and Medical Sciences of Gondar University for the period 2009 to 2011 was 659.6/100,000 population. In this study TB prevalence was 1814.1/100,000 population for the academic year 2009/10. Such differences may arise from a variety of conditions that facilitate or impair TB transmission and are difficult to define precisely here. These include differing levels of awareness on TB prevention and transmission among students attending these universities, health seeking behaviors, knowledge and attitude towards TB, accessibility of health care services and strength of TB control services in the area. Infection and transmission within the universities could also differ based on early or late detection of infectious cases, crowding, and size of at risk population. For example, the number of students enrolled at both AAU Sidist Kilo campus and ASTU is higher than that of Gondar University.
The magnitude of TB was significantly higher at ASTU compared to AAU Sidist Kilo campus. Prevalence values which were higher by as much as 3 times in certain years were observed at ASTU. Students at ASTU had a three times higher risk for being positive for tuberculosis of any type compared to their counterparts at Addis Ababa University Sidist Kilo campus. This difference could again be explained by the variability in the awareness of students at higher education institutions. Another important consideration is possible difference in case detection rates between the two universities. Higher case detection rates can result from better laboratory and clinical services.
The proportion of tuberculosis of any type indicated in this study was higher in male students than in female ones. This is in agreement with different studies from Ethiopia (13) and other parts of the world (14). This could be explained by behavioral and immunological factors that contribute to increased risk of TB acquisition in men (15).
In this study the highest number of TB cases were extra pulmonary (37.9%). However, the prevalence of smear positive TB cases (30.1%) clearly showed that a considerable amount of TB was circulating among students attending higher education institutions, which implies that students could be the foci of infection not only to their peers but also to the community at large (7).
Analysis of the trend of tuberculosis of all types showed a decrease in the study period 2009–2014 in both universities studied. This was in agreement with different retrospective studies conducted in higher education institutions, or community studies from different corners of the country (8, 12).
In-depth interviews with the heads of the respective University Clinic laboratories clearly indicated lack of quality assurance measures for sputum smear microscopic examination for acid fast bacilli at both universities. The main measure for TB case detection used by WHO is the increment in new smear positive cases by improved laboratory service in the DOTS program (16). It is quite plausible that had the laboratories implemented quality assessment schemes, the possibility of the smear positive case detection rate could have been higher, which could then have led to earlier intervention to reduce the number of additional new TB infections. Although lack of quality measures could also lead to false positive diagnoses, high false negative rates appear to occur more commonly (17,18).
An absence of any visible linkage of the TB lab systems in the University clinics studied with responsible bodies such as the Ministry of Health (MOH) and/or the Ethiopian Public Health Institute (EPHI) was noted in this study. The lack of a formal communication link hampers the provision of key training agendas such as on sputum smear microscopy and safe lab practices (laboratory biosafety). As a result, quality assurance systems including external and internal quality assessment schemes were not in place in the study clinic labs. Active follow up and support from non-governmental organizations such as the International Center for AIDS Care and Treatment Program-Ethiopia (ICAP-E) has enhanced quality of AFB testing procedures and increased the rate of sputum smear positivity (14). However, the observed detachment of the university clinic laboratories from the national/regional TB and leprosy control program and other governmental and/or nongovernmental institutions could have hindered access to such services.
Conclusion
The number of tuberculosis cases observed in both University clinics was very high. Responsible governmental and/or non governmental agencies working on TB prevention and control should consider higher education institutions as targets for prevention and elimination of tuberculosis. Furthermore, we would like to recommend regular TB screening of students at Higher Education Institutions. The laboratories in the higher education institution clinics selected for the study require attention, and by extension all other higher education institution clinics in the country should be provided with the appropriate support to establish quality assurance schemes from the Ministry of Health including the Ethiopian Public Health Institute (EPHI) and other key stakeholders where these are similarly missing.
Acknowledgments
We would like to express our special appreciation and thanks to the Department of Microbial, Cellular and Molecular Biology, Addis Ababa University for its financial support. This work was supported in part by the NIH/Fogarty International Center Global Infectious Diseases Grant D43TW009127. We thank Addis Ababa University Sidist Kilo campus and Adama Science and Technology University students clinic staff for their unreserved support during data collection.
References
- 1.Federica B, Francesco M, Andrea D. Immunology of Tuberculosis. Mediterr J Hematol Infect Dis. 2014;6(1):e2014027. doi: 10.4084/MJHID.2014.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Global tuberculosis report 2012. Geneva, Switzerland: WHO; 2012. [Google Scholar]
- 3.Dye C, Williams B. Eliminating human tuberculosis in the twenty-first century. J R Soc Interface. 2008 Jun 6;5(23):653–62. doi: 10.1098/rsif.2007.1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dye C, Borgdorff M. Global Epidemiology and Control of Tuberculosis. In: Kaufmann S, Helden P, editors. Handbook of Tuberculosis: Clinics, Diagnostics, Therapy and Epidemiology. Weinheim: WILEY-VCH Verlag GmbH & Co. KGaA; 2008. [Google Scholar]
- 5.The Lodi Tuberculosis Working Group. A school-and community-based outbreak of Mycobacterium tuberculosis in northern Italy. Epidemiol Infect. 1994;113:83–93. [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang S, Hong Yan H, Zhang J, Zhang T, Li X, Zhang Y. The experience of college students with pulmonary tuberculosis in Shaanxi, China: a qualitative study. BMC Infect Dis. 2010;10:174. doi: 10.1186/1471-2334-10-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stein-Zamir C, Volovik I, Rishpon S, Atamna A, Lavy A, Weiler-Ravell D. Tuberculosis outbreak among students in a boarding school. Eur Respir J. 2006;28(5):986–91. doi: 10.1183/09031936.06.00002506. [DOI] [PubMed] [Google Scholar]
- 8.Moges B, Amare B, Yismaw G, et al. Prevalence of tuberculosis and treatment outcome among university students in Northwest Ethiopia: a retrospective study. BMC Public Health. 2015;15:15. doi: 10.1186/s12889-015-1378-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Manual of Tuberculosis and Leprosy and TB/HIV Prevention and Control FMOH. Addis Ababa: EthioTikur Printing Press; 2008. [Google Scholar]
- 10.Kate A, Philip R. The Purposes and Practices of Quality Assurance in Ethiopian Higher Education: Journey, Adaptation and Integration. International Journal of Business Anthropology. 2012;3(2):19–25. [Google Scholar]
- 11. [Last accessed Sept 27, 2016];Detection and treatment of latent tuberculosis infection in Massachusetts College and University students: Recommendation of the Medical Advisory Committee for the elimination of Tuberculosis (MACET) 2003 Aug; ( www.state.ma.us/dph/cdc/tb/index.htm)
- 12.Global Tuberculosis report, 2014. Key indicators for the WHO African region. [Last accessed Sept 27, 2016];Estimates of mortality, prevalence and incidence. ( www.who.int/tb/data/)
- 13.World Health Organization. Report by the Director General, 44th World Health Assembly (WHA/1991/REC/1); supplemented by 53rd World Health Assembly, Provisional Agenda Item 12.1, A53/5. Geneva, Swit-zerland: World Health Organization; 2000. [Google Scholar]
- 14.Yamasaki-Nakagawa K, Ozasa N, Yamada N, Osuga K, Shimouchi A, Ishikawa N, Bam DS, Mori T. Gender difference in delays to diagnosis and health care seeking behavior in a rural area of Nepal. Int J Tuberc Lung Dis. 2001;5:24–31. [PubMed] [Google Scholar]
- 15.Mekonnen A. Smear-positive pulmonary tuberculosis and AFB examination practices according to the standard checklist of WHO s tuberculosis laboratory assessment tool in three Governmental hospitals, Eastern Ethiopia. BMC Res Notes. 2014;7:295. doi: 10.1186/1756-0500-7-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.WHO. Global tuberculosis control: surveillance, planning, financing: WHO report 2008. 20 Avenue Appia 1211 Geneva 27, Switzerland: WHO/HTM/TB/2008.393, WHO Press, World Health Organization; 2008. [Google Scholar]
- 17.Nguyen TN, Wells CD, Binkin NJ, Becerra JE, Pham DL, Nguyen VC. Quality control of smear microscopy for acid-fast bacilli: the case for blinded re-reading. Int J Tuberc Lung Dis. 1999 Jan;3(1):55–61. [PubMed] [Google Scholar]
- 18.Ayana DA, Kidanemariam ZT, Tesfaye HM, Milashu FW. External quality assessment for acid fast bacilli smear microscopy in eastern part of Ethiopia. BMC Res Notes. 2015 Oct 5;8:537. doi: 10.1186/s13104-015-1478-0. [DOI] [PMC free article] [PubMed] [Google Scholar]