Abstract
Background
Cognitive decline in the elderly is strongly associated with cerebral hypoperfusion, a condition that can be reversed with exercise. Adhering to a traditional exercise regimen, however, is challenging for this population.
Objective
In a pilot clinical study, we evaluated the ability of a “passive” exercise regimen (noninvasive calf muscle pump stimulation) to normalize blood pressure in a chronically hypotensive elderly population and enhance cognitive function.
Participants and methods
Ten elderly (82.5±7.5 years) men and women volunteers, residing in a senior living facility in upstate New York, were divided into control (N=5) and intervention (N=5) groups based on initial diastolic blood pressure (DBP); participants with initial DBP <65 mmHg became intervention participants, and those with initial DBP >65 mmHg enrolled in the control group. Body mass, blood pressure, and executive function (using incongruent Stroop and Trailmaking B test) were evaluated weekly for 4 months.
Results
At initiation of the study, time to complete the executive function tests in the hypotensive group was almost twice that of the control group. Daily calf muscle pump stimulation (passive exercise) for 1 hour/day, or less, was found to be sufficient to normalize DBP and significantly improve performance on the executive function tests.
Keywords: cognitive impairment, chronic hypotension, soleus stimulation, executive function
Plain language summary
Age-related cognitive impairment is a challenging clinical situation as there are still no effective pharmaceutical treatments. However, exercise, of essentially any form, seems to be effective in slowing the progression of age-related cognitive decline. This raises the possibility that exercise is effective through its ability to increase blood pressure and enhance blood flow to the brain. Here, we investigate a passive form of exercise, micromechanical stimulation of the plantar surface, a technology which activates the calf muscle pump in the lower legs, thereby enhancing cardiac return, normalizing blood pressure, and improving cerebral blood flow. Men and women residing in a senior living center were segregated into normal blood pressure (control) group and low blood pressure (intervention) group. The intervention group undertook passive exercise for 1 hour/day. While at the start of the study the intervention group’s performance was significantly worse in executive function tests compared to the control group, by the 14th week of the study, those in the intervention group had improved to the point of matching the performance of the control group.
Introduction
Age-related cognitive impairment continues to be a growing concern in both developed and developing countries. Currently, over five million older adults in the US suffer from dementia or cognitive impairment.1 Prevalence is strongly age dependent, with 14% of individuals over 70 having some form of dementia, while by the age of 80 years, one in three will have developed Alzheimer’s disease.2 Worldwide, mild cognitive impairment, a condition intermediate between normal cognitive aging and dementia, has also been reported to have prevalence rates in the 3%–5% range.3 Because pharmaceutical approaches to treating dementia are not currently available, and even symptomatic therapies have modest benefit, the consensus of the clinical community is that prevention must remain a primary focus.4
Foremost among the preventative therapies is exercise. A recent meta-analysis of randomized controlled exercise studies has shown that essentially all forms of exercise improve cognitive function in the elderly.5 The mechanism by which exercise improves cognition in older individuals remains unknown; however, one proposed mechanism is that exercise enhances cerebral blood flow (CBF).6 Between the ages of 30 and 70 years, CBF declines 30%–50%,7 but even mild exercise can significantly enhance CBF.8 Specifically, exercises which raise mean arterial blood pressure by just 5%–15% can increase CBF by 25%–30% in the older (62±7 years) population.9
The predominant challenge to implementing an exercise program as a means of maintaining CBF and slowing the progression of dementia in the elderly is adherence. Two-thirds of adults over 75 do not engage in any physical activity beyond that involved in activities of daily living, and among those who are physically active, only 30% of men and 15% of women participate in that activity regularly.10 Among those who are motivated to initiate a new exercise program, >50% drop out before realizing any health benefits with the greatest attrition occurring in the first 6 months.11 The explanations for the low adherence rates in the elderly are numerous: physical activity takes more time and effort than other preventative health measures; learning proper technique to ensure safety and effectiveness is too involved; guidance by their physician is vague regarding the specific physical activity to be undertaken; physical activity is often accompanied by discomfort (sweating, muscle soreness, etc); and as well, their living environment does not support easy access to the resources necessary to maintain a daily exercise schedule.12
An effective exercise approach for the elderly would therefore seem to require a modality which significantly increases CBF and has a sound theoretical foundation which will convince the clinical community of its effectiveness, requires minimal training, and introduces minimal inconvenience to daily life. Adequate CBF requires a normal cardiac output so as to maintain normal blood pressure. Cardiac output, in turn, is dependent on adequate venous return to the heart, a condition which does not typically exist among sedentary elderly. As a result, orthostatic hypotension is remarkably common in the elderly population, exceeding 30% in women over 75 years, and 25% in men over 75 years of age.13
Recent work has shown that cardiac return can be significantly increased through soleus muscle activation. As soleus muscle stimulation can be achieved noninvasively using micromechanical stimulation of the frontal plantar surface, this approach can be viewed as a type of “passive” exercise.14 The stimulation activates mechanoreceptors (Meissner’s corpuscles) in the dermis, triggering a postural reflex arc which results in contraction of the soleus muscles in the calves. The soleus muscles serve as the primary muscle pumps for ensuring adequate venous and lymphatic return from the lower extremities to the heart during orthostasis.15 In this age-matched, controlled, pilot clinical study, we investigated the potential of daily calf muscle pump stimulation (passive exercise) to normalize blood pressure and improve cognitive performance in an elderly population residing in a senior living center.
Methods
The study protocol was reviewed and approved by the Institutional Review Board at Hearth Management, LLC (Syracuse, NY, USA) and executed at the Castle Gardens Senior Living Center (Vestal, NY, USA), an assisted living care facility. Residents of the center (age range of 65–95 years) were recruited for the study through an orientation session open to all residents. The study was designed to assess temporal changes in executive function in a group of hypotensive individuals undertaking a passive exercise intervention, in comparison to a population of normotensive individuals. While an “untreated” group of hypotensive individuals could have alternatively been selected as the control group, we felt the latter approach would have made it more difficult to determine the clinical relevance of any observed changes in cognitive performance in the intervention group.
Interested individuals were screened to determine whether they met the inclusion/exclusion criteria and to obtain written informed consent. Inclusion criteria included fluency in the English language, being cognitively aware (cognizant of the current date, their location, President of the country), and willingness to use the intervention on a daily basis for a 4-month period of time. Exclusion criteria included having experienced a deep vein thrombosis or pulmonary embolism in the last 6 months, treatment for hypertension, difficulty or discomfort using the intervention device. The study was performed from January into May, 2016 (17 weeks).
Each week for the duration of the study, the study coordinator met with each enrolled participant and obtained the individual’s body mass, systolic blood pressure (SBP), and diastolic blood pressure (DBP), and had the participants complete three executive function tests which included the congruent Stroop, the incongruent Stroop, and the Trailmaking B tests. The congruent Stroop test is primarily a measure of basic reading rate where the color of a word (red) matches the word itself (“red”). Conversely, in the incongruent Stroop test, the color of a word and the word are discordant, that is, the name of a color is printed in a color that does not match the word (eg, “blue” or “green” is printed in red ink). For both tests, the words were printed in highlighted, 24-point font on gloss paper to enhance contrast and readability. Participants were asked to “read” the color of the word; this test is considered to be a measure of both mental flexibility and the ability to deal with interference.16 The Trailmaking B test evaluates visual attention and task switching in which the participant is instructed to connect a set of 24 alternate numbers and letters as quickly as possible while maintaining accuracy. All tests were explained to the participant with an opportunity given to complete a short practice run. The test was then issued on a letter size (216mm × 279mm) paper and timing was initiated, if the participant made a mistake, the investigator notified the participant, who then needed to correct the mistake before continuing with the timed test. All test results are reported in the number of seconds required to complete the task.
A 3-week learning period preceded the start of the study, giving the participants time to become familiar with both the physiologic testing and the executive function testing protocols.
Based on our previous research demonstrating the strong influence of blood pressure on cognitive function,13 recruited participants were divided into control and intervention groups based on their resting DBP; those with an average resting DBP >65 mmHg during assessments obtained in 3 weeks of the learning period were assigned to the control group, while those with a resting DBP <65 mmHg were assigned to the intervention group.
After the 3-week learning period, the intervention was introduced. Five calf muscle pump stimulation devices (HeartPartner; Sonostics, Inc, Endicott, NY, USA) were placed in a readily accessible common area at the center. This device activates the calf muscle pumps (soleus muscles) through stimulation of a postural reflex arc, resulting in the reduction of retained fluids in the lower body,17,18 as well as enhanced cardiac output leading to normalization of blood pressure under orthostatic conditions.19 The intervention permits participants to wear their shoes or socks/stockings during the exercise. The intervention participants were asked to use the passive exercise device for at least 1 hour/day for the duration of the study. In addition, a registry was positioned in the common area and the participants were asked to record their “exercise” duration upon completion of their daily routine. Control participants were asked not to use the devices at any time. Usage patterns were subsequently reviewed with each participant during the weekly study coordinator visit.
Missing data points were imputed using linear interpolation. Averages are reported as ± standard error unless otherwise noted. As device usage compliance fell well below the requested target range after 14 weeks, trends were analyzed by linear regression analysis over the first 14 weeks of the intervention period based on mean values (Origin 2017; OriginLab, Northampton, MA, USA), though all data throughout 17 weeks are reported. Trends with p<0.05 were considered significant.
Results
Twenty-three participants expressed interest in participating in the study; 13 of these met all the inclusion criteria, none of the exclusion criteria, and completed the initial 3-week training period. Ten of these participants completed the 17-week study, 6 men and 4 women, with three men and two women in both the control and intervention groups. Explanations for dropping out included inconvenience, not liking the executive function testing, insufficient time, and other interfering health complications. Among those completing the study, ages ranged from 72 to 94 years, with the average age in the control group being 82.4±6.7 years, and 82.6±8.1 years in the intervention group.
Self-reported compliance with device usage was largely consistent with that requested of the participants, at least for the first 14 weeks of the study (Figure 1). Usage time among the five intervention participants averaged 0.88±0.35 (standard deviation) hours/day during this time. As the weather turned warm in spring, the center staff encouraged the residents to go outside during their free time and daily device usage time dropped substantially, averaging only 0.25±0.16 hours/day for the last 3 weeks of the study.
Figure 1.
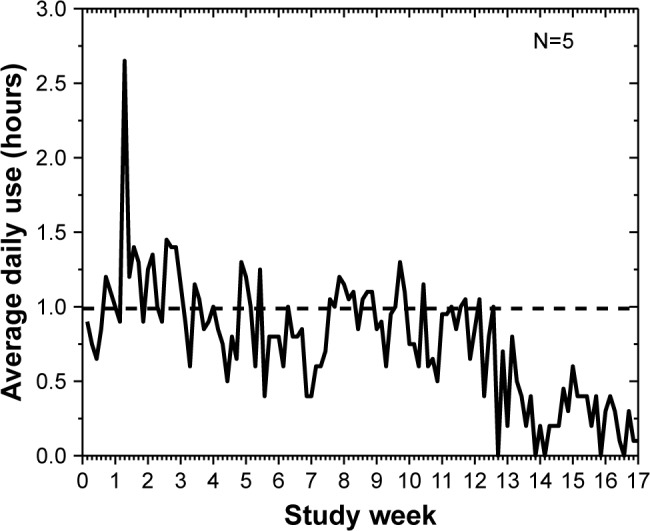
Compliance with device use during the study period. Participants were asked to use the device for at least 1 hour/day during their free time. Self-reported usage averaged 0.88 hours/day for the first 14 weeks, but fell to an average of just 15 minutes/day after warm weather set in.
Average body mass in the control and intervention groups was not significantly different at the start of the study period, with the control group averaging 80.1±7.7 kg while the intervention group averaged 80.8±7.5 kg. While average body mass of the control group did not change significantly over the course of the study, average body mass in the intervention group decreased by ~0.1 Kg/week over the 14 weeks of the analyzed intervention period, resulting in a final average body mass of 79.3 kg, representing a significant (p<0.0001) decline (Figure 2).
Figure 2.
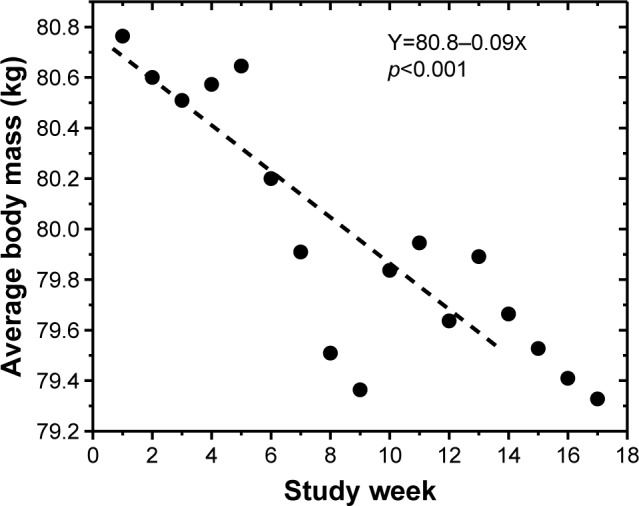
Change in body mass of participants in the intervention group over the course of the study. Body mass declined at a rate of ~0.1 kg/week (p<0.001) over the first 14 weeks of the study, consistent with calf muscle pump stimulation leading to clearance of fluid pooled in the lower body.
Assignment to control and intervention groups was based on average DBP recorded during the learning period, using a cutoff point of 65 mmHg; however, this division did not translate to significant differences in SBP for the two groups. SBP for the control group averaged 139.5±1.4 mmHg, and 138.3±1.2 mmHg for the intervention group, with no evidence of any changes over the study period. Average DBPs were significantly lower in the intervention group at the start of the study as compared to the control group. Control DBP averaged 76.5±5.6 over the 3-week screening period; while DBP for the intervention group averaged 59.5±2.0 over this same time period. During the study, the control group experienced a slow, but significant (p<0.01) decline in DBP (Figure 3), whereas the intervention group experienced a significant increase in DBP at a rate of 0.77 mmHg/week (p<0.02), such that by 14 weeks of intervention DBP had reached a level similar to that of the control group. Interestingly, the temporal DBP pattern in the intervention group was remarkably similar to the group’s compliance with the “exercise” regimen. Compliance and DBP increased for the first 4 weeks, declined over the next 4 weeks, then rose again over the following 4 weeks, before declining abruptly in the last few weeks of the study.
Figure 3.
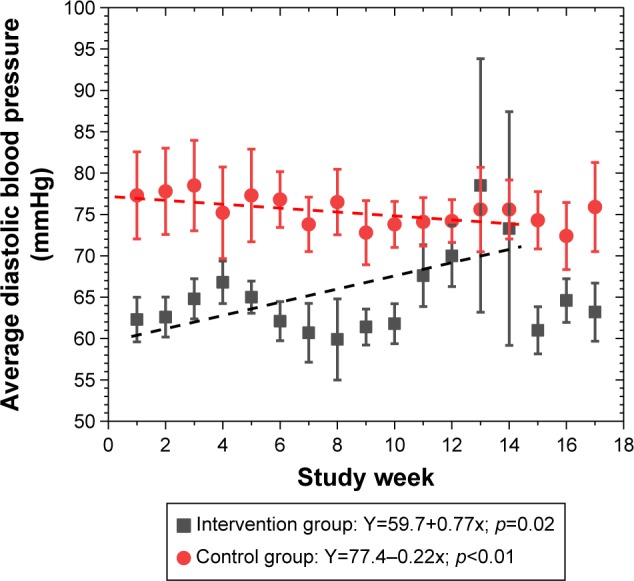
DBP was ~15 mmHg lower in the intervention group as compared to the control group at the start of the study. DBP fell slowly, but significantly, in the control group over the study period while DBP in the intervention group rose significantly, such that by week 14 DBP in both groups was statistically equal. Interestingly, the variation in DBP in the intervention group appears to mimic the variation in compliance with the intervention.
Abbreviation: DBP, diastolic blood pressure.
The Trailmaking B test evaluates visual attention and task switching. At the beginning of the study, the intervention group required twice the time (179±39 seconds), on average, to complete this test as compared to the control group (91±14 seconds; Figure 4). The control group demonstrated significant improvement in test times over the course of the study period, reducing test times by about 2.3 seconds/week (p<0.001). However, over the first 14 weeks of the study period, the intervention group improved their test times at almost twice the rate of the control group (4.4 seconds/week; p<0.001). In conjunction with the drop in compliance, the test times in the intervention group plateaued after 14 weeks.
Figure 4.
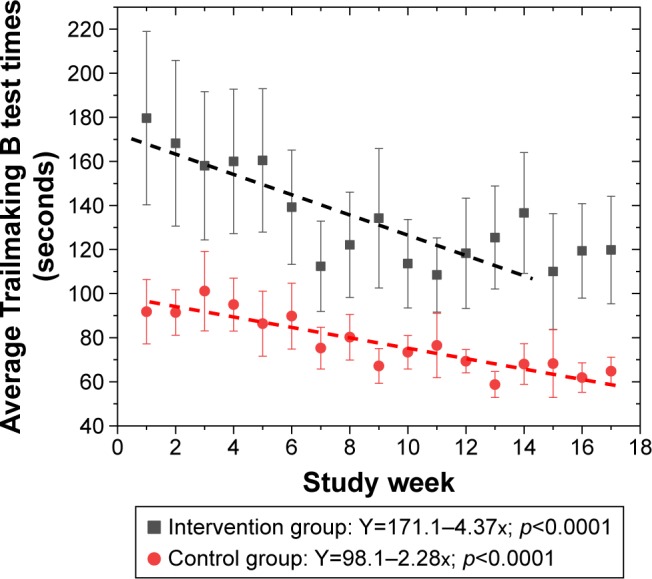
Time to complete the Trailmaking B test was almost twice as long for the intervention (hypotensive) group as compared to the control group. Test times improved over the study period in both control and intervention groups, with the intervention group improving their test times by almost twice the rate of the control group. However, even if these trends persisted it would take 18 months for the intervention group to match the performance of the control group.
The congruent Stroop test is primarily a measure of basic reading rate, and serves as a reference point for incongruent Stroop test results. Similar to the Trailmaking B results, the intervention group required significantly greater time (12.7±1.5 seconds), on average, to complete the test as compared to the control group which required on average 8.7±0.4 seconds (Figure 5). The control group improved their test times slightly, but significantly (0.05 seconds/week; p=0.006) over the course of the study. The intervention group demonstrated no significant improvement in their test times over the course of the study, though similar to the temporal DBP pattern, congruent Stroop scores mimicked the pattern of the group’s temporal “exercise” compliance levels.
Figure 5.
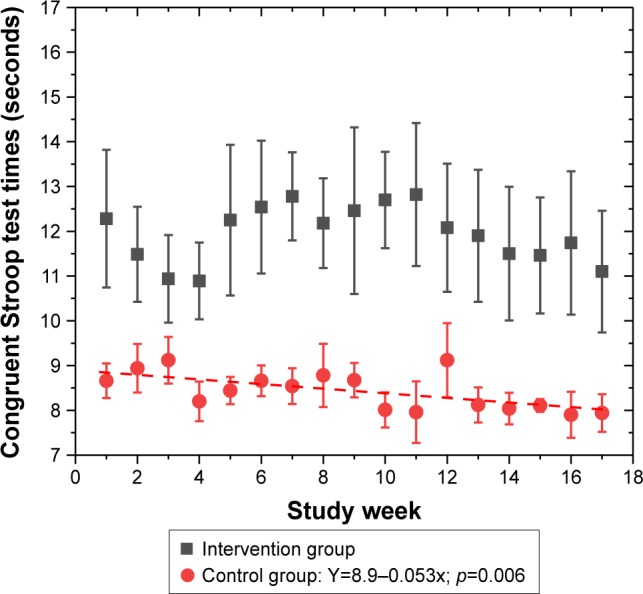
Congruent Stroop test times were ~1/3 greater in the intervention group as compared to the control group at the start of the study. While the control group improved their test times slightly over the study period, no significant, sustained improvement was observed in the intervention group. Similar to the DBP results, the temporal pattern of test times obtained from the intervention group mimicked the “exercise” compliance levels.
Abbreviation: DBP, diastolic blood pressure.
The incongruent Stroop test is considered a measure of both mental flexibility and the ability to deal with interference. Similar to Trailmaking B and congruent Stroop, the intervention group initially required substantially more time (47.6±9.1 seconds) to complete the test in comparison to the control group (32.9±6.2 seconds; Figure 6). While the control group demonstrated no improvement in test times over the course of the study, the intervention group improved their times, on average, by 1.5 seconds/week (p<0.0001) such that by the 14-week time point, the two groups had similar test times.
Figure 6.
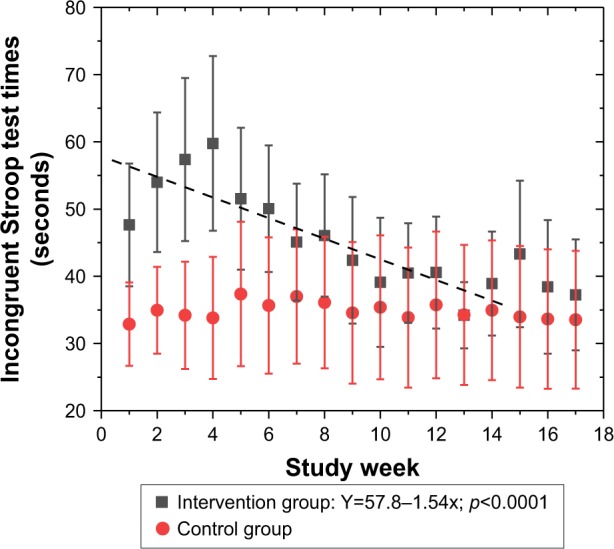
Incongruent Stroop test times for the intervention (hypotensive) group were ~2/3 greater than those obtained for the control group. While control group test times demonstrated no improvement over the course of the study, the intervention group demonstrated a significant 1.5 seconds/week improvement, such that by 14 weeks the two groups had similar test times.
Discussion
Numerous, large, prospective trials have shown chronic hypotension, in particular chronic diastolic hypotension, to be a prognostic factor in the development of dementia.20–23
Chronic postural hypotension is a particular concern for the elderly as, following age 65, blood pressure tends to decline, with the greatest impact on diastolic pressure.24 While some portion of blood pressure decline in the elderly is likely due to polypharmacy and the corresponding occurrences of drug interactions,25 in large part this decline appears to be simply associated with aging. As exercise has consistently been shown to slow or reverse cognitive impairment, and most exercises serve to increase blood pressure, the hypothesis that much of the observed age-related cognitive decline is related to reduced cerebral perfusion has gained substantial support. The challenge, however, has been identifying exercise regimens which meet the needs of the elderly population, whether community dwelling or residing in senior living centers, so that adherence to the regimen remains high.
Consistent with previous reports of an association between hypotension and cognitive impairment, we observed that our hypotensive group (initial DBP <65 mmHg) was initially much slower in completing the three executive function tests than the control group. Surprisingly, this extended to the congruent Stroop test which is essentially just a reading test of basic vocabulary words. Not only were the test times significantly longer, they were remarkably greater, approaching a factor of 2× for the Trailmaking B test. Given that all of our participants resided in the same assisted living center, and were of similar age, the difference in initial DBP, which is directly related to CBF, would seem to account for much of this difference. While the initial average DBP for the control group (during the 3-week training period) was over 76 mmHg, the intervention group had an average DBP of <60 mmHg. Based on reported work showing that just a 5%–10% increase in blood pressure can increase CBF by 25%,9 this difference of >25% between the two study groups could reflect a difference in CBF of >50%.
Compliance with device usage largely met the protocol requirements, at least for the first 14 weeks of the study. Placing the devices in a common area was initially viewed as beneficial for the residents as they would have other people to socialize with during the “exercise” sessions. However, numerous participants expressed concerns that getting to where the devices were located was problematic. A common comment from the participants was that if the devices were placed in their personal rooms it would be much more convenient as they could watch television, talk on the phone, or work on their computers during their “exercise” sessions. The significant drop in compliance which occurred in spring, while unexpected, did permit observation of the effects of stopping the exercise regimen.
The physiological influence of daily calf muscle pump stimulation was observed in two assessments. First, the intervention group participants lost, on average 1.5 kg of body mass, while no significant change in body mass was observed in the control group. This is consistent with the expectation of fluid clearance from the lower limbs as a result of this fluid being returned to the cardiovascular system. In addition, DBP was normalized in the intervention group during the first 14 weeks of the study, while DBP in the control group declined significantly. Importantly, when compliance fell off after the 14-week time point, DBP also fell significantly, providing additional confirmation that the intervention was the cause of the normalization of DBP.
Consistent with the hypothesis that any exercise which serves to increase blood pressure in hypotensive individuals will have a positive impact on cognitive function, daily use of calf muscle stimulation (passive exercise) had robust effects on both of the measures we utilized to evaluate cognitive function. At the start of the study, time to complete the Trailmaking B test in the intervention group was almost twice that of the control group, but these times improved by over 4 seconds/week over the following 14 weeks. While encouraging, given that the control group test times were improving as well it would have taken close to 18 months before the intervention scores matched those of the controls. While not an extraordinarily long time frame, this observation does lead to the suggestion that a more extended exercise regimen of 2–3 hours/day may help to normalize test times much more quickly. Given the convenience of noninvasive calf muscle pump stimulation, such daily usage times are probably not impractical as the typical adult in the US sits for over 12 hours/day.26
The incongruent Stroop test results demonstrated a much more rapid response. Starting out at test times more than 2/3 greater than the control group, the intervention group saw an improvement of over 1.5 seconds/week such that after 14 weeks, the test times were similar for both groups. As with the Trailmaking B results, test times plateaued when compliance dropped after 14 weeks, but regression analysis would seem to suggest that with continuation of the “exercise” regimen, test times would have continued to improve.
While the results from this pilot clinical study are encouraging, there are a number of limitations to this study. First is the small size of the study; with N=5 in both control and intervention groups there was no opportunity to break the study population down into subgroups to identify if any specific subpopulation preferentially benefitted from the passive exercise intervention. In addition, the study duration was relatively short; the 3–4 month study duration occurring in spring may, for example, only reflect a seasonal effect. A year long study with monthly assessment would help to identify if any seasonal effects existed, and whether the effects of intervention continue to accumulate over time. Also, monthly assessments would perhaps be seen as less onerous by the study participants and might reduce the learning effects associated with weekly repeated measures which were observed in the control group. Further, we relied on self-reported device usage. An internal monitor in the devices would allow more accurate recording of usage, and as well, could provide information on the specific days and times when the devices were used. Finally, as with many exercise studies, we saw a significant fall off in compliance at the end of the study. We believe this was due to the transition to warmer weather such that the participants were more likely to spend their free time outdoors, but it may also be a reflection of the commonly reported development of boredom with exercise interventions.
In summary, we have observed that a relatively simple, and convenient, noninvasive “passive” exercise regimen, involving micromechanical stimulation of the calf muscle pump (soleus muscles), is sufficient to normalize DBP in a hypotensive elderly population over a 4-month period of time, resulting in significantly improved cognitive performance on executive function tests. Longer term testing will be required to evaluate both the persistence of these effects and the extent to which these effects can be enhanced with sustained intervention.
Acknowledgments
The authors would like to acknowledge the assistance of Hearth Management, LLC, Ms Pamela Stento, Executive Director of the Castle Gardens Senior Living Center, as well as the residents and staff of the Castle Gardens senior living facility.
Footnotes
Disclosure
Dr McLeod holds an equity position in Sonostics, Inc and so could potentially benefit financially from the publication of this article. The other author reports no conflicts of interest in this work.
References
- 1.Satizabal CL, Beiser AS, Chouraki V, Chêne G, Dufouil C, Seshadri S. Incidence of dementia over three decades in the Framingham heart study. N Engl J Med. 2016;374:523–532. doi: 10.1056/NEJMoa1504327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Savica R, Petersen RC. Prevention of dementia. Psychiatr Clin North Am. 2011;24:127–145. doi: 10.1016/j.psc.2010.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sosa AL, Albanese E, Stephan BCM, et al. Prevalence, distribution and impact of mild cognitive impairment in Latin America, China, and India. PLoS Med. 2012;9(2):e1001170. doi: 10.1371/journal.pmed.1001170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wilcock GK. Primary prevention of dementia. Psychiatry. 2004;3:35–36. [Google Scholar]
- 5.Cai H, Li G, Hua S, Liu Y, Chen L. Effect of exercise on cognitive function in chronic disease patients: a meta-analysis and systematic review of randomized controlled trials. Clin Interv Aging. 2017;12:773–783. doi: 10.2147/CIA.S135700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Colcombe SJ, Kramer AF, Erickson KI, et al. Cardiovascular fitness, cortical plasticity, and aging. Proc Natl Acad Sci U S A. 2004;101:3316–3321. doi: 10.1073/pnas.0400266101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Scheel P, Ruge C, Petruch UR, Schoning M. Color duplex measurement of cerebral blood flow volume in healthy adults. Stroke. 2000;31:147–150. doi: 10.1161/01.str.31.1.147. [DOI] [PubMed] [Google Scholar]
- 8.Ogoh S, Ainslie PN. Cerebral blood flow during exercise: mechanisms of regulation. J Appl Physiol. 2009;107:1370–1380. doi: 10.1152/japplphysiol.00573.2009. [DOI] [PubMed] [Google Scholar]
- 9.Smirl JD, Haykowsky MJ, Nelson MD, Altaimirano-Diaz LA, Ainslie PN. Resting and exercise cerebral blood flow in long-term heart transplant recipients. J Heart Lung Transplant. 2012;31:906–908. doi: 10.1016/j.healun.2012.04.003. [DOI] [PubMed] [Google Scholar]
- 10.Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med. 2004;39:1056–1061. doi: 10.1016/j.ypmed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 11.Dishman RK. Motivating older adults to exercise. South Med J. 1994;87:S79–S82. [PubMed] [Google Scholar]
- 12.Chao D, Foy CF, Farmer D. Exercise adherence among older adults: challenges and strategies. Control Clin Trials. 2000;21:212S–217S. doi: 10.1016/s0197-2456(00)00081-7. [DOI] [PubMed] [Google Scholar]
- 13.McLeod KJ, Jain T. Postural hypotension and cognitive function in older adults. Gerontol Geriatr Med. 2017;3:1–8. doi: 10.1177/2333721417733216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wolters FJ, Mattrace-Raso FUS, Koudstaat PJ, Hofman A, Ikram MA. Orthostatic hypotension and the long term risk of dementia. PLoS Med. 2016;13(10):e1002143. doi: 10.1371/journal.pmed.1002143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Padberg F. The physiology and hemodynamics of the normal venous circulation. In: Gloviczki P, Yao JST, editors. Handbook of Venous Disorders. 2nd ed. Vol. 3. London: Hodder Arnold; 2001. pp. 25–35. [Google Scholar]
- 16.Wecker NS, Kramer JH, Wisniewski A, Delis DC, Kaplan E. Age effects on executive ability. Neuropsychology. 2000;14:409–414. doi: 10.1037//0894-4105.14.3.409. [DOI] [PubMed] [Google Scholar]
- 17.Goddard AA, Pierce CS, McLeod KJ. Reversal of lower limb edema by calf muscle pump stimulation. J Cardiopulm Rehabil Prev. 2008;28:174–179. doi: 10.1097/01.HCR.0000320067.58599.ac. [DOI] [PubMed] [Google Scholar]
- 18.Pierce C, McLeod KJ. Feasibility of treatment of lower limb edema with calf muscle pump stimulation in chronic heart failure. Eur J Cardiovasc Nurs. 2009;8:345–348. doi: 10.1016/j.ejcnurse.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 19.Madhavan G, Steward JM, McLeod KJ. Effect of plantar micromechanical stimulation on cardiovascular responses to immobility. Am J Phys Med Rehabil. 2004;84:338–345. doi: 10.1097/01.phm.0000159970.81072.8b. [DOI] [PubMed] [Google Scholar]
- 20.Guo A, Viitanen M, Fratiglioni L, Winblad B. Low blood pressure and dementia in elderly people: the Kungsholmen project. BMJ. 1996;312:805–808. doi: 10.1136/bmj.312.7034.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Verghese J, Lipton RB, Hall DB, Kuslansky G, Katz MJ. Low blood pressure and the risk of dementia in very old individuals. Neurology. 2003;61:1667–1672. doi: 10.1212/01.wnl.0000098934.18300.be. [DOI] [PubMed] [Google Scholar]
- 22.Ruitenberg A, den Heijer T, Bakkar SLM, van Swieten JC, Koudstaal PJ, Hofman A. Cerebral hypoperfusion and clinical onset of dementia: the Rotterdam study. Ann Neurol. 2016;57:789–794. doi: 10.1002/ana.20493. [DOI] [PubMed] [Google Scholar]
- 23.Waldstein SR, Giggery PP, Thayer JF, Zonderman AB. Nonlinear relations of blood pressure to cognitive function: the Baltimore longitudinal study of aging. Hypertension. 2005;45:374–379. doi: 10.1161/01.HYP.0000156744.44218.74. [DOI] [PubMed] [Google Scholar]
- 24.Cheng S, Xanthakis V, Sullivan LM, Vasan RS. Blood pressure tracking over the adult life course. Hypertension. 2012;60:1393–1399. doi: 10.1161/HYPERTENSIONAHA.112.201780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cohen I, Rogers P, Burke V, Beilin LJ. Predictors of medication use, compliance and symptoms of hypotension in a community-based sample of elderly men and women. J Clin Pharm Ther. 1998;23:423–432. doi: 10.1046/j.1365-2710.1998.00183.x. [DOI] [PubMed] [Google Scholar]
- 26.Diaz KM, Howard VJ, Hutto B, et al. Patterns of sedentary behavior and mortality in U.S. Middle-aged and older adults: a national cohort study. Ann Intern Med. 2017;167(7):465–475. doi: 10.7326/M17-0212. [DOI] [PMC free article] [PubMed] [Google Scholar]


