Abstract
We describe the case of a 73-year-old man who experienced dry cough and exertional dyspnea after dabigatran administration. Chest radiographs revealed the development of bilateral consolidative and ground glass opacity, and transbronchial lung biopsy showed organized materials in the alveolar spaces with moderate inflammatory infiltrate and focal fibrosis. Lung opacity gradually disappeared after discontinuing dabigatran. To date, there has been only one report regarding dabigatran-induced lung injury, except for alveolar hemorrhage and eosinophilic pneumonia. Therefore, we should consider that any drug can cause various types of lung injuries.
Keywords: Dabigatran, Interstitial pneumonia, Drug-induced lung injury
Abbreviations: OP, organizing pneumonia; HRCT, high-resolution computed tomography; NSIP, nonspecific interstitial pneumonia; BALF, Bronchoalveolar lavage fluid
1. Introduction
With the ever-increasing number of therapeutic drugs, the list of drugs responsible for severe pulmonary diseases also increases. Drug-induced lung injury is defined as a lung injury that results from the specific use of a drug associated with various types of lung complication, including organizing pneumonia (OP). Here we describe a case of bilateral consolidation and ground glass opacity observed on chest radiograph after administering dabigatran, a novel anticoagulant.
2. Case report
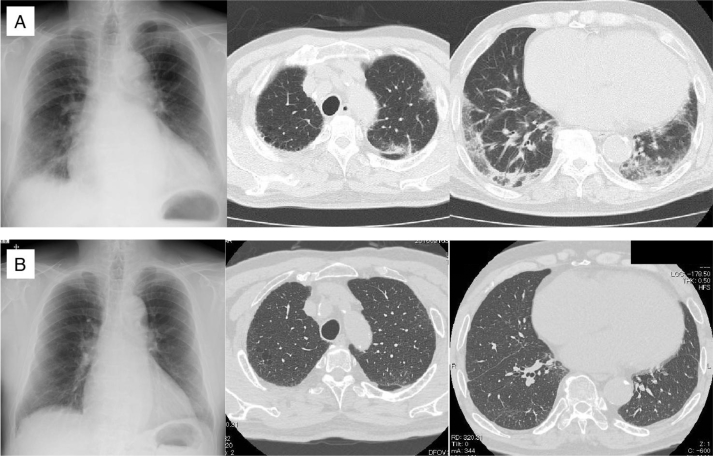
A 73-year-old man with a history of chronic heart failure, paroxysmal atrial fibrillation, and a 24-month treatment regime of dabigatran was referred to our department because of his dry cough and exertional dyspnea (modified MRC grade 2). Examination of the patient's respiratory system revealed fine crackles at the lower back. Chest X-ray showed bilateral infiltration in the lower field, and chest high-resolution computed tomography (HRCT) showed nonsegmental subpleural consolidation and ground glass opacity, indicating nonspecific interstitial pneumonia (NSIP) with OP pattern (Fig. 1). Blood tests revealed elevated KL-6 levels (1302 U/mL) and slightly elevated eosinophil percentage with no anemia. No autoantibodies were observed (Table 1).
Fig. 1.
Chest radiograph of the patient. (A) Chest X-ray revealed bilateral infiltration predominantly in the lower fields. HRCT of the chest demonstrated nonsegmental subpleural consolidation and ground glass opacity mainly in the lower lung. (B) Follow-up chest X-ray and HRCT findings obtained after 2 months showed improvement of the previously existing opacities.
Table 1.
Laboratory findings of the patient with interstitial pneumonia caused by dabigatran.
| Hematology | Biochemistry | ||
|---|---|---|---|
| WBC | 10040/μL | TP | 8.5 g/dL |
| Neut | 72.8% | Alb | 3.4 g/dL |
| Lymph | 15.3% | T.bil | 0.5 mg/dL |
| Mono | 5.1% | AST | 20 IU/L |
| Eos | 4.9% | ALT | 22 IU/L |
| Baso | 0.5% | LDH | 208 IU/L |
| RBC | 4.2 × 106/μL | BUN | 23 mg/dL |
| Hb | 13.2 g/dL | Cre | 1.0 mg/dL |
| Ht | 39.7% | Na | 135 mol/L |
| Plt | 34.3 × 104/μL | K | 4.6 mol/L |
| Cl | 99 mol/L | ||
| Serology | Glu | 105 mg/dL | |
| C-reactive protein | 1.98 mg/dL | Ferritin | 424.9 ng/dL |
| BNP | 71.3 pg/mL | ||
| KL-6 | 1302 U/mL | ||
| SP-D | 159 ng/mL | ||
| SP-A | 126.2 ng/mL | ||
| RF | 5 IU/mL | ||
| Anti-nuclear antibody | 40 Titer | ||
| MPO-ANCA | <3.5 IU/mL | ||
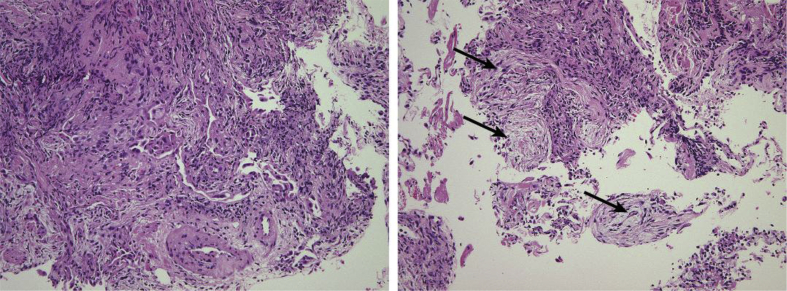
Bronchoscopy was performed to evaluate the patient's progress after discontinuing dabigatran. Bronchoalveolar lavage fluid (BALF) was not bloody, and cell fractionation revealed 71.5% macrophages, 8.0% neutrophils, 17.7% lymphocytes, and 2.8% eosinophils. The CD4/CD8 ratio of lymphocytes in BALF was 1.81. Microbiological examination results of BALF revealed no evidence of infection. Transbronchial lung biopsy specimen suggested OP (Fig. 2).
Fig. 2.
Histopathological findings from transbronchial lung biopsy. Bronchial and alveolar tissue with moderate chronic inflammatory infiltrate, focal fibrosis, and aggregates of macrophages and hyperplastic pneumocytes. Organized materials were focally evident in the alveolar spaces (arrows). Original magnification: ×10.
After bronchoscopy, we administered warfarin instead of dabigatran. Two months later, the patient's symptoms such as dry cough and dyspnea completely disappeared, and chest HRCT revealed that the lung infiltration had also disappeared (Fig. 1). Six months later, serum KL-6 levels reduced to normal levels. Therefore, the patient's interstitial pneumonia was diagnosed to be a drug-induced lung injury caused by dabigatran.
3. Discussion
Drug-induced lung injury is diagnosed on the basis of clinical examination and radiographic and histological findings [1]. Cases that develop subacutely, as in the present case, tend to be NSIP or OP. Although we have not conducted a drug-induced lymphocyte stimulation test for dabigatran, the patient's pathological findings and clinical course corresponded with the diagnosis of OP.
Dabigatran is a relatively new anticoagulant agent from the direct thrombin inhibitor class. Dabigatran is preferred to warfarin in many cases because it offers similar efficacy with a lower risk for bleeding and does not require frequent blood tests [2]. However, few cases of alveolar hemorrhage [3], [4], eosinophilic pneumonia [5], and OP [6] have been reported as adverse events. In the present case, the patient had no symptoms or findings of alveolar hemorrhage.
In 2011, the Ministry of Health, Labour and Welfare of Japan issued an alert that dabigatran administration might be associated with interstitial lung diseases, including death in cases with preexisting interstitial pneumonia. Thus, this is well recognized in Japan at least but only one case report of interstitial pneumonia has been published. Physicians should be aware of any potential adverse effects, including drug-induced lung injury, associated with novel drugs.
Conflict of interest
The authors declare no potential conflicts of interest.
References
- 1.Kubo K., Azuma A., Kanazawa M. Consensus statement for the diagnosis and treatment of drug-induced lung injuries. Respir. Investig. 2013;51(4):260–277. doi: 10.1016/j.resinv.2013.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Poller L., Jespersen J., Ibrahim S. Dabigatran versus warfarin in patients with atrial fibrillation. N. Engl. J. Med. 2009;361(27):2673–2674. [PubMed] [Google Scholar]
- 3.Yokoi K., Isoda K., Kimura T., Adachi T. Diffuse alveolar hemorrhage associated with dabigatran. Intern. Med. 2012;51(18):2667–2668. doi: 10.2169/internalmedicine.51.8345. [DOI] [PubMed] [Google Scholar]
- 4.Husari A., Beydoun A., Sheik Ammar A. The untold story of Dabigatran etexilate: alveolar hemorrhage in an elderly patient with interstitial pulmonary fibrosis. J. Thromb. Thrombolysis. 2012:1–2. doi: 10.1007/s11239-012-0784-9. [DOI] [PubMed] [Google Scholar]
- 5.Fujita A., Inami N.A.H. Dabigatran etexilate-induced eosinophilic pneumonia. Ann. Jpn. Respir. Soc. 2013;2:414–418. [Google Scholar]
- 6.Kono M., Hirota K., Yokoe A. Wandering pneumonia caused by dabigatran. Intern. Med. 2014;53(16):1825–1827. doi: 10.2169/internalmedicine.53.2307. [DOI] [PubMed] [Google Scholar]