Abstract
Introduction
In contrast to urban populations, little is known about polysubstance use among rural people who inject drugs (PWID), particularly in Puerto Rico where injection drug use and related health consequences are prevalent. The aim of the study is to compare injection and non-injection substance use profiles among separate urban and rural samples of Puerto Rican PWID.
Material and Methods
Data for the urban sample come from 455 PWID who participated in the CDC's National HIV Behavioral Surveillance survey of injection drug use in San Juan. The data for the rural sample come from 315 PWID residing in four rural cities approximately 40-miles from San Juan. Latent class analysis was used to derive separate urban and rural profiles of weekly injection and non-injection substance use. Injection behaviors were examined as possible correlates of latent class membership.
Results
Five latent classes were identified in the urban sample, and three latent classes were identified in the rural sample. Classes were similar across samples; however, key differences emerged. Both samples had classes of primary heroin injectors, primary speedball injectors, and cocaine-heroin injectors. The urban sample had one high polysubstance class. Polysubstance use profiles that shared similar characteristics between samples also shared similar injection patterns, with some variation.
Discussion
Variations in substance patterns and associated health risks are likely shaped by social and geographic boundaries.
Conclusions
Understanding variations in substance use patterns across rural and urban locales may improve surveillance efforts and tailor desistance and harm reduction efforts at the state and local levels.
Keywords: Polysubstance use, rural, injection drugs, Hispanic, latent class analysis
1. Introduction
Patterns of substance use and related health risks differ considerably across substances and geographic locations (Colon et al., 2001; Deren et al., 2003). This is particularly evident among Puerto Ricans, who despite lower overall rates of lifetime illicit substance use (Canino, 2007), display higher rates of substance use-related health consequences such as HIV and hepatitis C (HCV; Mino et al., 2011). Comparative research in the San Juan metropolitan area and New York City shows that people who inject drugs (PWID) in San Juan use injection drugs more often and engage in riskier injection behaviors compared to Puerto Ricans on the mainland (Colon et al., 2001). Within Puerto Rico, internal differences in use patterns, overdose risk, and service need—especially urban/rural differences—are not well known, while the growth in injection opioid use in rural communities elsewhere in the U.S. suggests a need for research in rural areas (Dombrowski et al., 2016). This study uses latent class analysis (LCA) to examine weekly injection and non-injection polysubstance use profiles across comparable rural and urban samples of active PWID in Puerto Rico to determine how and when rural and urban substance use and injection risk differ.
Polysubstance use is understood as the consumption of two or more substances during a specified time period, including simultaneous use of multiple substances in a single occasion or concurrent use of multiple substances on separate occasions within a short period of time (Ives and Ghelani, 2006). In general, polysubstance use among PWID has been associated with distinct physical and mental health comorbidities (Betts et al., 2016; Patra et al., 2009), increased injection and sexual risk behaviors (Harrell et al., 2012; Meacham et al., 2015), and poorer treatment outcomes (Dutra et al., 2008). These factors may explain higher risks of overdose and HIV and HCV infection among polysubstance using PWID when compared to PWID who use a limited range of substances (Harrell et al., 2012; Keen et al., 2014).
Simultaneous use of heroin and cocaine (i.e., speedball) is highly prevalent among Puerto Rican PWID (Colon et al., 2001). Compared to U.S. born Hispanics, Puerto Rican born Hispanics are more likely to use injection heroin and speedball and less likely to inject amphetamines (Freeman et al., 1999). Compared to Puerto Rican PWID in New York City, those in San Juan are more likely to use injection heroin, cocaine, and speedball and less likely to use non-injection substances such marijuana, alcohol, and non-injectable heroin and cocaine (Colon et al., 2001). Despite these findings, surprisingly little is known about concurrent polysubstance use profiles among Puerto Rican PWID. Qualitative research in urban Puerto Rico suggests that marijuana, alcohol, and benzodiazepines are often used simultaneously with injection heroin and/or cocaine to enhance or attenuate the effects (Finlinson et al., 2006; Porter, 1999), but rigorous statistical treatments are few.
Understanding distinct classes of polysubstance use has important implications for those situations where select patterns of substance use and routes of administration are associated with distinct health consequences (Harrell et al., 2012). Polysubstance use among Puerto Rican PWID has been associated with increased injection risk behavior compared to use of primarily one injection substance (Hautala et al., 2017). Others suggest that the use of alcohol with injection drugs also increases injection risk behavior (Matos et al., 2004; Welch-Lazoritz et al., 2017). Despite suspected risks, the association between various substance use combinations and injection risk behaviors among PWID is not well understood, particularly in Puerto Rico, and particularly for rural users. Prior research among rural non-Hispanic populations in the U.S. suggests important differences in types of substances used (Gfroerer et al., 2007), patterns and emergence of substance use disorders (Brooks et al., 2017), and routes of administration (Young et al., 2010). Because rural communities in Puerto Rico have limited access to safe injection resources compared to their counterparts in urban San Juan (Des Jarlais et al., 2013; Welch-Lazoritz et al., 2017), the association between substance use patterns and injection-related behavior may vary considerably across rural and urban distinctions, with important implications for tailoring treatment and harm reduction services.
To address these gaps in the literature, the first aim of this study is to use LCA to compare weekly polysubstance use profiles within and between separate rural and urban samples of active PWID in Puerto Rico. LCA is a statistical method which aims to identify latent subgroups of individuals who share similar profiles on a set of observed variables (Collins and Lanza, 2013), and has recently been used to characterize polysubstance use among PWID outside of Puerto Rico (Betts et al., 2016; Hopfer et al., 2014; Meacham et al., 2015; Roth et al., 2015). LCA, however, has not been used previously to compare urban and rural PWID. Thus, the second aim of this study is to examine injection related outcomes associated with polysubstance use within and between comparable urban and rural samples. Understanding these differences may help improve surveillance efforts and tailor cost-effective interventions.
2. Material and Methods
2.1 Sample
The urban sample consists of the 455 PWID residing in the San Juan metropolitan area who participated in the CDC's National HIV Behavioral Surveillance (NHBS) survey of injection drug use (IDU) Round 3 in 2012 (Centers for Disease Control and Prevention, 2012). The rural sample consists of 315 PWID residing in four rural towns in central Puerto Rico, about 40-miles from San Juan. Interviews were completed between April-June 2015. The sampling technique and questionnaire for the rural sample were adapted from the CDC NHBS IDU 3 study to generate a comparison to the urban data. Persons were eligible if they injected drugs in the past 12 months and were age 18 years or older, able to complete the survey in either English or Spanish, and able to provide informed consent. Drug injection in the past 12 months was confirmed by observing physical evidence of recent injection (e.g., track marks) and by assessing knowledge of injection practices.
Recruitment for both samples was managed using respondent driven sampling (RDS; (Heckathorn, 1997; 2002). An initial set of respondents, referred to as “seeds” (13 seeds in urban sample; 8 seeds in rural sample—two in each town), were recruited and given three referral coupons that they could give to other PWID who had not previously participated in the study. Eligible participants referred by the seeds comprise the first wave of the sample, and are given three referral coupons to recruit the next wave, and so on. In both studies, participants were compensated with $25 for the interview and $10 for each referral. Written, informed consent was obtained by all study participants in both samples. The study received IRB approval through the [removed for blind review] and [removed for blind review].
2.2 Measures
2.2.1 Substance Use
In trained interviewer administered questionnaires, respondents were asked about frequency of use on a wide array of injection and non-injection substances. Consistent with prior research (Harrell et al., 2012; Monga et al., 2007), we restricted the selection of both injection and non-injection drugs to those in which at least 20% of the sample reported using in the past month. Both samples resulted in the selection of the same seven substances. For injection drug use, heroin, cocaine, and speedball use were included. For non-injection drug use, binge drinking (five or more drinks on a single occasion for men and four or more drinks on a single occasion for women), marijuana, benzodiazepine, and crack cocaine use were included. Respondents were asked how often they used each substance in the past 12 months. Response options ranged from (0) never to (9) four or more times per day. To differentiate between habitual use rather than episodic use (Roth et al., 2015), we dichotomized each item into (0) less than weekly use and (1) weekly or more use.
2.2.2 Injection Behavior
Four injection-related variables were examined as potential correlates of latent class membership. Respondents were asked how many people they used a needle with after someone already injected with it in the past 12 months; how many people they used the same cooker, cotton, or water with after someone had already used it in the past 12 months; and, how many people they used drugs with that had been divided with a syringe that has already been used in the past 12 months (i.e., backloading). Because of heavy skew, response options for these three questions were dichotomized into (0) zero partners and (1) one or more partners. Respondents were also asked whether they had received new sterile needles for free, not including those given to them by a friend, relative, or sex partners in the past 12 months (e.g., from a needle exchange program). Response options were (0) no and (1) yes.
2.3 Analytic Strategy
LCA was used to examine profiles of polysubstance use for the urban and rural samples separately in Mplus version 7.4 (Muthen and Muthen, 1998-2016). Full-information maximum likelihood was used to account for missing data on the substance use indicators. LCA aims to uncover unobserved heterogeneity in the data which represents subgroups of individuals who share similar profiles on a set of observed characteristics. Because class enumeration must be inferred from the data, three information criteria measures (Akaike information criteria – AIC, Akaike, 1987; Bayesian information criteria—BIC, Schwarz, 1978; and the sample-adjusted BIC—A-BIC) and two likelihood ratio tests (Lo-Mendall-Rubin likelihood ratio test—LMR-LRT, Lo et al., 2001; and bootstrap likelihood ratio test—BLRT, McLachlan and Peel, 2000) were compared across successive models. Lower values on the information criteria suggest better model fit, and significant values on the likelihood ratio tests suggests that a k-class model fits the data better than a k-1 class model. Multiple random start values were examined to ensure proper model identification, and the tenability of the local independence assumption was assessed by examining the standardized bivariate residuals (Magidson and Vermunt, 2011). Injection related behaviors were examined as possible outcomes of latent class membership using the auxiliary (DCAT) command in Mplus to examine probabilities of the four injection behavior variables across latent class groups. This approach takes into account latent class assignment uncertainty, and simulation studies suggest that this model-based approach produces less bias than the classify-and-analyze and pseudo-class draw methods (Lanza et al., 2013).
3. Results
3.1 Descriptive Statistics
Table 1 presents sample demographics, substance use prevalence, and injection-related behaviors. Both samples were comprised of similar demographic and injection profiles (e.g., mostly male, average age of early 40s, low educational attainment, mostly single), with the exception of past year homelessness, which was nearly twice as prevalent in the urban sample. Prevalence of non-injection substance use was similar across both samples for binge drinking; however, the rural sample had a slightly higher percentage of people who regularly used marijuana and benzodiazepines, and the urban sample had a slightly higher percentage of people who regularly use crack cocaine. Prevalence of weekly or greater injection drug use was similar across both samples for cocaine, heroin, and speedball. Additional demographic, substance use, injection risk, and RDS descriptive comparisons can be found in Thrash et al. (2017).
Table 1. Descriptive Statistics across Rural and Urban Samples.
| Rural (N = 315) | Urban (N = 455) | |
|---|---|---|
|
| ||
| % or Mean | % or Mean | |
| Demographics: | ||
| Age (Mean) | 41.8 | 40.7 |
| Male | 90.8% | 82.5% |
| Past Year Homelessness | 38.5% | 78.2% |
| Marital Status | ||
| Single | 47.0% | 61.8% |
| Married/Cohabiting | 22.2% | 17.4% |
| Divorced/Separated/Widowed | 30.8% | 20.9% |
| ≥ High School Diploma | 47.6% | 45.5% |
| Years injecting drugs (Mean) | 19.9 | 20.1 |
| Substance Use (Weekly vs. Less Than Weekly Use): | ||
| Non-Injection: | ||
| Binge Drinking | 21.6% | 24.6% |
| Marijuana | 32.2% | 19.8% |
| Benzodiazepine | 23.2% | 16.5% |
| Crack Cocaine | 11.5% | 16.3% |
| Injection: | ||
| Cocaine | 29.3% | 26.4% |
| Heroin | 35.6% | 39.1% |
| Speedball | 85.0% | 90.3% |
| Injection Characteristics: | ||
| Shared used syringe in past year | 33.7% | 37.2% |
| Shared used cooker, cotton, or water in past year | 60.0% | 60.6% |
| Backloading in past year | 34.2% | 50.0% |
| Obtained sterile needle from service agency in past year | 58.7% | 71.4% |
3.2 LCA Model Selection and Within Sample Description
For the rural sample, up to six classes were examined (see Table 2). The AIC and A-BIC values favored a four-class model. One of the classes, however, contained only five individuals and was not considered. When two- and three-class solutions were considered, the AIC and A-BIC values were lowest in the three-class model, and the BLRT further suggested that a three-class model fits the data better than the two-class model. As a result, a three-class model was selected for the rural sample with high class separation and classification accuracy (entropy = .73; average posterior probability range = .77 - .90).
Table 2. Latent Class Analysis Model Selection.
| AIC | BIC | SA-BIC | LMR-LRT | BLRT | Entropy | LL | |
|---|---|---|---|---|---|---|---|
| Rural Sample | |||||||
| 1 | 2347.93 | 2374.20 | 2352.00 | -1166.97 | |||
| 2 | 2291.77 | 2348.06 | 2300.48 | 70.63* | 72.17* | 0.82 | -1130.89 |
| 3 | 2285.37 | 2371.68 | 2298.73 | 21.92 | 22.40* | 0.73 | -1119.69 |
| 4 | 2278.97 | 2395.30 | 2296.98 | 21.92* | 22.39* | 0.79 | -1108.49 |
| 5 | 2278.80 | 2425.15 | 2301.45 | 15.83 | 16.17 | 0.78 | -1100.40 |
| 6 | unidentified | ||||||
| Urban Sample | |||||||
| 1 | 3205.10 | 3233.94 | 3211.72 | -1595.55 | |||
| 2 | 3077.11 | 3138.92 | 3091.31 | 141.10* | 143.99* | 0.65 | -1523.56 |
| 3 | 2994.02 | 3088.78 | 3015.79 | 97.11* | 99.09* | 0.75 | -1474.01 |
| 4 | 2974.17 | 3101.90 | 3003.52 | 35.13* | 35.85* | 0.79 | -1456.09 |
| 5 | 2962.33 | 3123.02 | 2999.25 | 27.29 | 27.84* | 0.78 | -1442.16 |
| 6 | 2963.36 | 3157.02 | 3007.85 | 14.67 | 14.97 | 0.87 | -1434.68 |
p < .05
Note: AIC – Akaike Information Criteria; BIC – Bayesian Information Criteria; SA-BIC – Sample Adjusted BIC; LMR-LRT – Lo-Mendell-Rubin Likelihood Ratio Test; BLRT – Bootstrap Likelihood Ratio Test; LL – Log Likelihood
Table 3 presents the unconditional and conditional class probabilities for each substance. The first class (Rural Class 1: 7%) had high probabilities of weekly heroin injection and moderate probabilities of binge drinking, marijuana, and benzodiazepine use. Probabilities on all other substances were low. The second class (Rural Class 2: 26%) had high probabilities of weekly cocaine, heroin, and speedball injection, and moderate probabilities of weekly marijuana and benzodiazepine use. Probabilities on all other substances were low. The third group (Rural Class 3: 67%) had high probabilities of weekly speedball injection, and low probabilities of using all other substances.
Table 3. Latent Class Analysis Probabilities across Rural and Urban Samples.
| Rural (N = 315) | Urban (N = 455) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Rural Class 1 | Rural Class 2 | Rural Class 3 | Urban Class 1 | Urban Class 2 | Urban Class 3 | Urban Class 4 | Urban Class 5 | |
| Proportion: | .07 | .26 | .67 | .06 | .10 | .42 | .21 | .21 |
| Non-Injection: | ||||||||
| Binge Drinking | .26 | .17 | .23 | .45 | .49 | .09 | .38 | .20 |
| Marijuana | .51 | .63 | .18 | .81 | .75 | .00 | .10 | .16 |
| Benzodiazepine | .32 | .46 | .14 | .52 | .50 | .05 | .11 | .13 |
| Crack Cocaine | .13 | .21 | .08 | .88 | .30 | .07 | .11 | .09 |
| Injection: | ||||||||
| Cocaine | .00 | .77 | .14 | .87 | .09 | .02 | .88 | .00 |
| Heroin | .80 | .68 | .19 | .81 | .10 | .05 | .69 | .97 |
| Speedball | .00 | 1.00 | .88 | 1.00 | 1.00 | .99 | .93 | .20 |
For the urban sample, up to six classes were examined (see Table 2). The AIC and A-BIC values were lowest in the five-class model. The BLRT further provided support that a five-class solution fits the data better than a four-class solution. The five-class solution had high class separation and classification accuracy (entropy = .78; average posterior probability range = .77 - .94).
Table 3 presents the unconditional and conditional class probabilities for use of each substance in the urban sample. The first class (Urban Class 1: 6%) had high probabilities of weekly use on all seven substances examined. The second class (Urban Class 2: 10%) had high probabilities of weekly speedball injection and marijuana use, and moderate probabilities of weekly binge drinking and benzodiazepine use. The third class (Urban Class 3: 42%) had high probabilities of weekly speedball use and low probabilities on all other substances. The fourth class (Urban Class 4: 21%) had high probabilities of weekly cocaine, heroin, and speedball injection, and moderate probabilities of weekly binge drinking. Probabilities of all other substances were low. The fifth class (Urban Class 5: 21%) had high probabilities of weekly heroin use and low probabilities of other substance use.
3.3 Between Sample Comparisons of Polysubstance Use Profiles
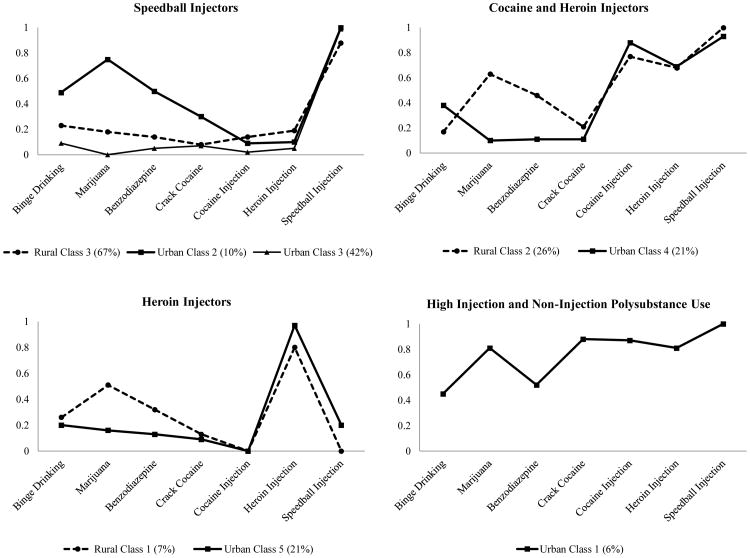
Plots of conditional probabilities were grouped together based on key similarities across both samples to provide between-sample polysubstance use comparisons (see Figure 1). In both samples, each class was primarily characterized by the type of injection drug. The largest classes in both samples (Rural Class 3 and Urban Class 3) were characterized by regular speedball injection and low probabilities on all other substances examined. A somewhat similar group in the urban sample (Urban Class 2) was distinguished by moderate probabilities of weekly binge drinking and benzodiazepine use, and a high probability of weekly marijuana use (similar to Rural Class 1). In addition to the primary speedball injector classes, both samples revealed classes of respondents who were primarily heroin injectors (Rural Class 1 and Urban Class 5; see bottom left portion of Figure 1). The rural class, however, was smaller in proportion and had moderate probabilities of weekly marijuana and benzodiazepine use compared to the urban class. Both samples also had at least one group that had high probabilities of weekly cocaine, heroin, and speedball injection (Rural Class 2 and Urban Class 4). The urban sample revealed one unique class (Urban Class 1) comprised of respondents with relatively high probabilities of weekly use on all substances examined. This class shared similar injection patterns with Rural Class 2 and Urban Class 4, and shared similar non-injection patterns with Urban Class 2. However, this is the only class across either sample with high probabilities of weekly crack cocaine use.
Figure 1.
Latent class analysis profiles of weekly non-injection (i.e., binge drinking, marijuana, benzodiazepine, and crack cocaine) and injection (i.e., cocaine, heroin, and speedball) substances grouped by similarities across rural (dashed lines) and urban (solid lines) samples. The Y-axis represents the probability of weekly or greater use of a particular substance within each class.
3.4 Within Sample Injection Profiles across LCA Subgroups
Table 4 displays the injection risk profiles within the LCA subgroups. For the rural sample, probabilities for shared syringe use and shared cooking equipment were significantly lower in the Rural Class 1 (heroin injectors) compared to the other two rural classes. Conversely, Rural Class 1 (heroin injectors) was significantly less likely to obtain sterile needles from a service agency than rural class 2 (cocaine and heroin injectors), but not Rural Class 3 (speedball injectors). Backloading was not a significant correlate of polysubstance use patterns in the rural sample.
Table 4. Within-Sample Injection Behavior Probabilities across Latent Classes.
| Rural (N = 315) | Urban (N = 455) | |||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Rural Class 1 | Rural Class 2 | Rural Class 3 | Urban Class 1 | Urban Class 2 | Urban Class 3 | Urban Class 4 | Urban Class 5 | |
| Shared syringe+ | .08a | .37b | .35b | .74a | .27bc | .31b | .47c | .22b |
| Shared cooking equipment+ | .33a | .70b | .59b | 1.00a | .75b | .52cd | .69bc | .36d |
| Backloading# | .11a | .62a | .28a | .95a | .53bc | .40bd | .65c | .24d |
| Obtained Sterile Needles* | .36a | .68b | .58ab | .78a | .67a | .69a | .70a | .87a |
significant in rural sample only
significant in urban sample only
significant in both samples
Note: Probabilities or means within each sample that do not share a subscript are significantly different from one another (p < .05)
In the urban sample, Urban Class 1 (high injection and non-injection polysubstance use) had significantly higher probabilities of shared syringe use, shared cooking equipment, and backloading than the other urban polysubstance use classes. For shared syringe use, Urban Class 4 (cocaine and heroin injectors) had significantly higher probabilities than Urban Classes 3 (speedball injectors) and 5 (heroin injectors). No other contrasts were significant. For shared cooking equipment, Urban Class 2 (speedball injectors) had higher probabilities than Urban Classes 3 (speedball injectors) and 5 (heroin injectors), but not Urban Class 4 (cocaine and heroin injectors). Urban Class 5 (heroin injectors) had significantly lower probability than Urban Class 4 (cocaine and heroin injectors). No other contrasts were significant. For backloading, Urban Classes 2 (speedball injectors) and 4 (cocaine and heroin injectors) had higher probabilities than UrbanClass 5 (heroin injectors). In addition, Urban Class 4 (cocaine and heroin injectors) had higher probabilities of backloading than Urban Class 3 (speedball injectors). No other contrasts were significant. There were no significant differences for obtaining sterile needles from a service agency such as a needle exchange program.
3.5 Between Sample Comparisons of Injection Risk Profiles
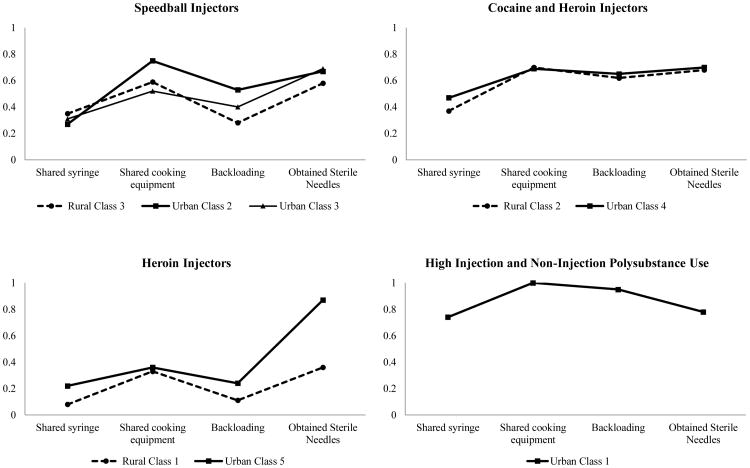
Because they share common metrics, probabilities of shared syringe use, cooker use, backloading, and obtaining sterile needles from a service agency were plotted across latent classes that share similar polysubstance use profiles to allow cross-class comparisons of associated risk behaviors (see Figure 2). Here we see that similar polysubstance use latent classes across the rural/urban samples also share similar injection risk patterns. For the three classes of primarily speedball injectors (Rural Class 3, Urban Class 2, and Urban Class 3), risk patterns look relatively similar, with the slight exception of the class characterized by moderate non-injection polysubstance use (Urban Class 2) which had higher probabilities of shared cooker equipment use and backloading. For the heroin injector classes (Rural Class 1 and Urban Class 5), probabilities were also quite similar except for obtaining sterile needles, which was higher in the urban sample. For the cocaine and heroin injector classes (Rural Class 2 and Urban Class 4), risk behavior probabilities were again nearly identical. Lastly, for the high injection and non-injection polysubstance use class (Urban Class 1), the probabilities of all four outcomes are among the highest compared to all the other classes.
Figure 2.
Predicted probabilities of past year injection behavior grouped by similarities in latent substance use profiles across rural (dashed lines) and urban (solid lines) samples. The Y-axis represents the predicted probability of endorsing each item in the past 12 months.
4. Discussion
The first aim of the study was to compare weekly polysubstance use profiles within and between separate rural and urban samples of PWID in Puerto Rico. A three-class solution was identified in the rural sample, and a five-class solution was identified in the urban sample, patterns similar to those found in prior LCA research with PWID (Betts et al., 2016; Harrell et al., 2012; Kuramoto et al., 2011; Meacham et al., 2015; Monga et al., 2007; Roy et al., 2013; Trenz et al., 2013). These patterns across diverse populations of PWID suggests that polysubstance use is normative (rather than restricted to a small subset) within the PWID population—and may reflect a common liability for polysubstance use among heavy substance users everywhere (Vanyukov et al., 2003). However, economic, political, and geographic structures are also known to generate differences in use patterns and related injection risks across locales (Singer, 1999).
Our results show important similarities and differences in polysubstance use between distinct urban and rural areas—supporting both normative and spatial-cultural arguments. We feel this is true despite the fact that the rural sample was comprised of PWID residing 40 miles outside of San Juan. The mountainous terrain and low mobility of rural users produced considerable geographic isolation, implying that similarities in polysubstance use profiles may not be reduced to a function of close proximity or overlapping drug markets. The urban sample had a more diverse array of polysubstance use profiles, whereas nearly all of the rural sample fit into two classes. Potential sources for this difference include greater demographic and cultural homogeneity in rural communities (Brooks et al., 2017), and rural social networks that tend to be more dense, family-centered, and interdependent compared to urban communities (Dew et al., 2007).
The second aim of this study was to examine injection related outcomes associated with polysubstance use profiles. Importantly, we found widespread evidence that similar polysubstance use classes across the samples shared similar injection risk profiles. Within samples, however, we found that latent classes with a higher number of substance use combinations have higher probabilities of risky injection behavior than classes characterized by fewer substances. The rural and urban classes characterized by primarily heroin injectors had the lowest probability of risky injection behavior, echoing results from PWID in Baltimore (Kuramoto et al., 2011) and San Diego (Roth et al., 2015). Conversely, the urban class that was characterized by high injection and non-injection polysubstance use had the highest probabilities of risky injection behavior, findings supportive of research among various samples of PWID (Harrell et al., 2012). The other latent classes with evidence of polysubstance use (cocaine and heroin injectors, speedball injectors) had moderate probabilities of risky injection behavior, higher than heroin injectors but lower than the class containing high polysubstance use. The association between moderate and high polysubstance use with risky behaviors is likely related to frequent injection speedball use, which has been associated with increased injection frequency (Colon et al., 2001b) and joint drug purchasing in Puerto Rico (Colón et al., 2001a). Ethnographic reports from Puerto Rico suggest that PWID who pool money to purchase heroin and cocaine to prepare speedballs are likely to use a single needle to divide the mixture into smaller quantities (e.g., backloading; Abadie et al., 2016).
Understanding differences between urban and rural use patterns and associated injection behaviors is important when seeking to counter overdose risk. Despite similarities in polysubstance use and injection risk profiles across the rural and urban samples, small to moderate differences in polysubstance use patterns can have important implications for overdose prevention. Where injection use of heroin (alone or in combination with cocaine) is common, the risk for opioid overdose increases with co-use of other substances, especially central nervous system depressants such as alcohol and benzodiazepines (Darke, 2014). Based on our results, approximately one third of respondents in both samples are at high risk for overdose because of regular use of some form of injection heroin along with moderate alcohol and/or benzodiazepine use (Rural Classes 1 and 2, and Urban Classes 1, 2, and 4).
In both samples, the largest group was characterized by weekly use of injection speedball and low probabilities of other substance use (Rural Class 3 and Urban Class 3). This too represents unique overdose risks. Injection speedball use has been shown to moderately increase the odds of overdose death, perhaps because it is associated with increased injection quantity and frequency (Colon et al., 2001) and treatment noncompliance (Merraro et al., 2005), both of which are conducive to overdose risk (Darke, 2014). The only class across both samples with low potential overdose risk compared to other profiles is Urban Class 5, defined by high probabilities of weekly or greater injection heroin use and low probabilities on all other substances examined. Primarily heroin injector classes in both samples have the longest injection duration averages (results available upon request), and stable use patterns that likely increase tolerance which may provide a slight protective effect against overdose risk (Galea et al., 2006).
Although the risk for overdose is high in both samples, the lack of treatment and harm reduction services in rural Puerto Rico likely creates structural barriers that increase odds for overdose and other health risks in those areas (Des Jarlais et al., 2013). Indeed, a key difference to emerge across the rural and urban samples was obtaining sterile needles from a service agency. This was far more common in the urban sample, and not surprising, recent research shows that urban Puerto Rican PWID are more likely to access needle exchange programs than their rural counterparts (Welch-Lazoritz et al., 2017).
Addressing substantial unmet substance use and HIV treatment needs in Puerto Rico, with a particular focus on rural outreach, can reduce health risks conducive to mortality among Puerto Rican PWID. Different strategies may be required to address different drug use patterns, however. The results shown here argue for overdose prevention strategies that go beyond one-size-fits-all naloxone distribution. Use patterns and the specific challenges of service delivery in rural areas require specific attention. On the positive side, fewer distinct use classes found in rural areas may simplify outreach and allow for more concentrated prevention efforts.
4.1 Limitations
Several limitations may affect the interpretation of the findings. First, the data are cross-sectional and temporal ordering cannot be established between polysubstance use profiles and injection correlates. Longitudinal data and/or qualitative research may give better insight into the potential developmental processes underlying polysubstance use across rural and urban communities. Second, the two samples may not be generalizable to all of Puerto Rico. Given their hard-to-reach nature, generating a representative sample of active PWID is difficult. RDS is a common sampling technique with known qualities, which improves upon convenience sampling techniques to give more accurate population estimates. Despite the strengths of RDS, the samples may not be generalizable to all PWID within the two areas sampled, or Puerto Rican PWID residing outside of the expansive San Juan metropolitan area.
5. Conclusions
Injection drug use and its consequences are highly prevalent in Puerto Rico (Mino et al., 2011). This study extends research on Puerto Rican PWID by examining latent subgroups of injection and non-injection substance use patterns across rural and urban distinctions. Variations in substance use patterns across rural and urban communities suggests the need for more inclusive surveillance efforts, which can be used to understand various combinatorial patterns of substance use and related risks to adapt limited programming resources at the local, state, and national levels. The existence of unique polysubstance use classes and their distinct injection profiles support the general need for treatment modalities aimed at desistance and harm reduction to be tailored to particular patterns of substance use and population density.
Highlights.
Polysubstance use profiles vary across rural and urban communities in Puerto Rico
Some form of injection heroin was used by nearly all participants in both samples
Similar polysubstance use profiles also share similar injection behavior correlates
Acknowledgments
The authors would like to acknowledge Janet Burnett, Gabriela Paz-Bailey, and Melissa Cribbin from the Division of HIV/AIDS Prevention, Centers for Disease Control and Prevention, as well as Yadira Rolón Colón and Sandra Miranda De León from the Puerto Rico Department of Health, for collecting and sharing the NHBS San Juan IDU3 dataset with us.
Role of Funding Source: This work was supported by the National Institute on Drug Abuse of the National Institutes of Health [grant number R01DA037117] and by the Center for Drug Use and HIV Research [CDUHR-P30 DA011041]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Contributors: DH led the conception, analysis, and drafting of the manuscript. RA assisted with data collection and revisions to the manuscript. BK assisted with revisions to the manuscript. KD is the principle investigator of the rural component of the study and assisted with writing and revising the manuscript. All authors have approved the content of the manuscript and order of authorship.
Conflict of Interest: No conflict declared
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Abadie R, Welch-Lazoritz M, Gelpi-Acosta C, Reyes JC, Dombrowski K. Understanding differences in HIV/HCV prevalence according to differentiated risk behaviors in a sample of PWID in rural Puerto Rico. Harm Reduct J. 2016;13 doi: 10.1186/s12954-016-0099-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akaike H. Factor analysis and AIC. Psychometrika. 1987;52:317–332. [Google Scholar]
- Betts KS, Chan G, McIlwraith F, Dietze P, Whittaker E, Burns L, Alati R. Differences in polysubstance use patterns and drug-related outcomes between people who inject drugs receiving and not receiving opioid substitution therapies. Addiction. 2016;111:1214–1223. doi: 10.1111/add.13339. [DOI] [PubMed] [Google Scholar]
- Brooks B, McBee M, Pack R, Alamian A. The effects of rurality on substance use disorder diagnosis: A multiple-groups latent class analysis. Addict Behav. 2017;68:24–29. doi: 10.1016/j.addbeh.2017.01.019. [DOI] [PubMed] [Google Scholar]
- Canino G. 25 years of child and adult psychiatric epidemiology studies in Puerto Rico. P R Health Sci J. 2007;26:385–394. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV Infection, Risk, Prevention, and Testing Behaviors among Persons Who Inject Drugs--National HIV Behavioral Surveillance: Injection Drug Use, 20 U S Cities, 2012. Centers for Disease Control and Prevention; Atlanta, GA: 2012. [Google Scholar]
- Collins LM, Lanza ST. Latent Class and Latent Transition Analysis: With Applications in the Social, Behavioral, and Health Sciences. John Wiley and Sons; Hoboken, NJ: 2013. [Google Scholar]
- Colon H, Robles R, Deren S, Hardeo S, Finlinson HA, Andi J, Cruz M, Kang SY, Oliver-Valex D. Between-city variation in frequency of injection among Puerto Rican injection drug users: East Harlem, New York, and Bayamon, Puerto Rico. JAIDS J Acquir Immune Defic Syndr. 2001a;27:405–413. doi: 10.1097/00126334-200108010-00012. [DOI] [PubMed] [Google Scholar]
- Colón HM, Finlinson HA, Robles RR, Deren S, Andía J, Kang SY, Oliver-Vélez D. Joint drug purchases and drug preparation risk behaviors among Puerto Rican injection drug users. AIDS Behav. 2001b;5:85–96. doi: 10.1023/A:1009515723223. [DOI] [Google Scholar]
- Darke S. Opioid overdose and the power of old myths: What we thought we knew, what we do know and why it matters. Drug Alcohol Rev. 2014;33:109–114. doi: 10.1111/dar.12108. [DOI] [PubMed] [Google Scholar]
- Deren S, Oliver-Velez D, Finlinson A, Robles R, Andia J, Colón HM, Kang SY, Shedlin M. Integrating qualitative and quantitative methods: Comparing HIV-related risk behaviors among Puerto Rican drug users in Puerto Rico and New York. Subst Use Misuse. 2003;38:1–24. doi: 10.1081/JA-120016563. [DOI] [PubMed] [Google Scholar]
- Des Jarlis D, Nugent A, Solberg A, Feelemyer J, Mermin J, Holtzman D. Syringe service programs for persons who inject drugs in urban, suburban, and rural areas — United States, 2013. MMWR Morb Moral Wkly Rep. 2013;64:1337–1341. doi: 10.15585/mmwr.mm6448a3. [DOI] [PubMed] [Google Scholar]
- Dew B, Elifson K, Dozier M. Social and environmental factors and their influence on drug use vulnerability and resiliency in rural populations. J Rural Health. 2007;23:16–21. doi: 10.1111/j.1748-0361.2007.00119.x. [DOI] [PubMed] [Google Scholar]
- Dombrowski K, Crawford D, Khan B, Tyler K. Current rural drug use in the US Midwest. J Drug Abuse. 2016;2 [PMC free article] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A Meta-analytic review of psychosocial interventions for substance use disorders. Am J Psychiatry. 2008;165:179–187. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- Finlinson HA, Colón HM, Robles RR, Soto-López M. An exploratory qualitative study of polydrug use histories among recently initiated injection drug users in San Juan, Puerto Rico. Subst Use Misuse. 2006;41:915–935. doi: 10.1080/10826080600669603. [DOI] [PubMed] [Google Scholar]
- Freeman R, Williams M, Saunders L. Drug use, AIDS knowledge, and HIV risk behaviors of Cuban-, Mexican-, and Puerto-Rican-born drug injectors who are recent entrants into the United States. Subst Use Misuse. 1999;34:1765–1793. doi: 10.3109/10826089909039426. [DOI] [PubMed] [Google Scholar]
- Galea S, Nandi A, Coffin P, Tracy M, Piper T, Ompad D. Heroin and cocaine dependence and the risk of accidental non-fatal drug overdose. J Addict Dis. 2006;25:79–87. doi: 10.1300/J069v25n03_10. [DOI] [PubMed] [Google Scholar]
- Gfroerer JC, Larson SL, Colliver JD. Drug use patterns and trends in rural communities. J Rural Health. 2007;23:10–15. doi: 10.1111/j.1748-0361.2007.00118.x. [DOI] [PubMed] [Google Scholar]
- Harrell PT, Mancha BE, Petras H, Trenz RC, Latimer WW. Latent classes of heroin and cocaine users predict unique HIV/HCV risk factors. Drug Alcohol Depend. 2012;122:220–227. doi: 10.1016/j.drugalcdep.2011.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hautala D, Abadie R, Thrash C, Reye JC, Dombrowski K. Latent risk subtypes based on injection and sexual behavior among people who inject drugs in rural Puerto Rico. J Rural Health. 2017 doi: 10.1111/jrh.12262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling: A new approach to the study of hidden populations. Soc Probl. 1997;44:174–199. doi: 10.2307/3096941. [DOI] [Google Scholar]
- Heckathorn DD. Respondent-driven sampling II: Deriving valid population estimates from chain-referral samples of hidden populations. Soc Probl. 2002;49:11–34. doi: 10.1525/sp.2002.49.1.11. [DOI] [Google Scholar]
- Hopfer S, Tan X, Wylie JL. A social network–informed latent class analysis of patterns of substance use, sexual behavior, and mental health: social network study III, Winnipeg, Manitoba, Canada. Am J Public Health. 2014;104:834–839. doi: 10.2105/AJPH.2013.301833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ives R, Ghelani P. Polydrug use (the use of drugs in combination): A brief review. Drugs Educ Prev Policy. 2006;13:225–232. doi: 10.1080/09687630600655596. [DOI] [Google Scholar]
- Keen L, Khan M, Clifford L, Harrell PT, Latimer WW. Injection and non-injection drug use and infectious disease in Baltimore City: Differences by race. Addict Behav. 2014;39:1325–1328. doi: 10.1016/j.addbeh.2014.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuramoto SJ, Bohnert ASB, Latkin CA. Understanding subtypes of inner-city drug users with a latent class approach. Drug Alcohol Depend. 2011;118:237–243. doi: 10.1016/j.drugalcdep.2011.03.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Tan X, Bray BC. Latent class analysis with distal outcomes: A flexible model-based approach. Struct Equ Model Multidiscip J. 2013;20:1–26. doi: 10.1080/10705511.2013.742377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–778. [Google Scholar]
- Magidson J, Vermunt J. The SAGE Handbook of Quantitative Methodology for the Social Sciences. SAGE Publications; Thousand Oaks, CA: Latent Class Models; pp. 176–199. 3011. [Google Scholar]
- Marrero CA, Robles R, Colon H, Reyes JC, Matos T, Sahai H, Calderon J, Shepard E. Factors associated with drug treatment dropout among injection drug users in Puerto Rico. Addict Behav. 2005;30:397–402. doi: 10.1016/j.addbeh.2004.05.024. [DOI] [PubMed] [Google Scholar]
- Matos T, Robles R, Sahai H, Colon H, Reyes JC, Marrero CA, Calderon J, Shepard E. HIV risk behaviors and alcohol intoxication among injection drug users in Puerto Rico. Drug Alcohol Depend. 2004;76:229–234. doi: 10.1016/j.drugalcdep.2004.05.007. [DOI] [PubMed] [Google Scholar]
- McLachlan G, Peel D. Finite Mixture Models. John Wiley and Sons; Hoboken, NJ: 2000. [Google Scholar]
- Meacham MC, Rudolph AE, Strathdee SA, Rusch ML, Brouwer KC, Patterson TL, Vera A, Rangel G, Roesch SC. Polydrug use and HIV risk among people who inject heroin in Tijuana, Mexico: A latent class analysis. Subst Use Misuse. 2015;50:1351–1359. doi: 10.3109/10826084.2015.1013132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milloy MJ, Kerr T, Tyndall M, Montaner J, Wood E. Estimated drug overdose deaths averted by North America's first medically-supervised safer injection facility. PLoS One. 2008;3:e3351. doi: 10.1371/journal.pone.0003351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mino M, Deren S, Colón HM. HIV and drug use in Puerto Rico: Findings from the ARIBBA study. J Int Assoc Physicians AIDS Care. 2011;10:248–259. doi: 10.1177/1545109710397768. [DOI] [PubMed] [Google Scholar]
- Monga N, Rehm J, Fischer B, Brissette S, Bruneau J, El-Guebaly N, Noël L, Tyndall M, Wild C, Leri F, Fallu JS, Bahl S. Using latent class analysis (LCA) to analyze patterns of drug use in a population of illegal opioid users. Drug Alcohol Depend. 2007;88:1–8. doi: 10.1016/j.drugalcdep.2006.08.029. [DOI] [PubMed] [Google Scholar]
- Muthen L, Muthen B. Mplus User's Guide. Muthen and Muthen; Los Angeles, CA: 1998. [Google Scholar]
- Patra J, Fischer B, Maksimowska S, Rehm J. Profiling polysubstance use typologies in a multi-site cohort of illicit opioid and other drug users in Canada–A latent class analysis. Addict Res Theory. 2009;17:168–185. doi: 10.1080/16066350802372827. [DOI] [Google Scholar]
- Porter J. The street/treatment barrier: Treatment experiences of Puerto Rican injection drug users. Subst Use Misuse. 1999;34:1951–1975. doi: 10.3109/10826089909039434. [DOI] [PubMed] [Google Scholar]
- Roth AM, Armenta RA, Wagner KD, Roesch SC, Bluthenthal RN, Cuevas-Mota J, Garfein RS. Patterns of drug use, risky behavior, and health status among persons who inject drugs living in San Diego, California: A latent class analysis. Subst Use Misuse. 2015;50:205–214. doi: 10.3109/10826084.2014.962661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy É, Richer I, Arruda N, Vandermeerschen J, Bruneau J. Patterns of cocaine and opioid co-use and polyroutes of administration among street-based cocaine users in Montréal, Canada. Int J Drug Policy. 2013;24:142–149. doi: 10.1016/j.drugpo.2012.10.004. [DOI] [PubMed] [Google Scholar]
- Schwarz G. Estimating the dimension of a model. Ann Stat. 1978;6:416–464. [Google Scholar]
- Singer M. Why do Puerto Rican injection drug users inject so often? Anthropol Med. 1999;6:31–58. doi: 10.1080/13648470.1999.9964573. [DOI] [Google Scholar]
- Thrash C, Welch-Lazoritz M, Gauthier G, Khan B, Abadie R, Dombrowski K. Rural and urban injection drug use in Puerto Rico: network implication for human immunodeficiency virus and hepatitis C virus infection. J Ethn Subst Abuse. 2017;30:1–24. doi: 10.1080/15332640.2017.1326864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trenz RC, Scherer M, Duncan A, Harrell PT, Moleko AG, Latimer WW. Latent class analysis of polysubstance use, sexual risk behaviors, and infectious disease among South African drug users. Drug Alcohol Depend. 2013;132:441–448. doi: 10.1016/j.drugalcdep.2013.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanyukov MM, Tarter RE, Kirisci L, Kirillova GP, Maher BS, Clark DB. Liability to substance use disorders: 1: Common mechanisms and manifestations. Neurosci Biobehav Rev. 2003;27:507–515. doi: 10.1016/j.neubiorev.2003.08.002. [DOI] [PubMed] [Google Scholar]
- Welch-Lazoritz M, Habecker P, Dombrowski K, Rivera Villegas A, Davila CA, Rolón Colón Y, Miranda De León S. Differential access to syringe exchange and other prevention activities among people who inject drugs in rural and urban areas of Puerto Rico. Int J Drug Policy. 2017;43:16–22. doi: 10.1016/j.drugpo.2016.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch-Lazoritz M, Hautala D, Habecker P, Dombrowski K. Association between alcohol consumption and injection and sexual risk behaviors among people who inject drugs in rural Puerto Rico. J Subst Abuse Treat. 2017;82:34–40. doi: 10.1016/j.jsat.2017.08.001. 10.1016/j.jsat.2017.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young AM, Havens JR, Leukefeld CG. Route of administration for illicit prescription opioids: A comparison of rural and urban drug users. Harm Reduct J. 2010;7:24. doi: 10.1186/1477-7517-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]