Abstract
Background
Identifying risk factors for youth e-cigarette use is critical, given high rates of e-cigarette use and unknown health effects of long-term use. The current study examined whether an early age of onset of e-cigarette use mediates the association between impulsivity and e-cigarette frequency.
Methods
Cross-sectional survey data of e-cigarette users (n=927) were collected from 8 high schools in southeastern Connecticut. The sample was 44.7% female (mean age 16.2 [SD=1.2], mean age of e-cigarette onset 14.7 [SD=1.6]). Two domains of self-reported, trait impulsivity were assessed using the abbreviated Barratt Impulsiveness Scale: impaired self-regulation (e.g., problems with concentration or self-control) and behavioral impulsivity (e.g., doing things without thinking). Mediation was tested with Mplus, and the model included school as a cluster variable and controlled for covariates related to e-cigarette use (i.e., sex, age, race, peer use, and other tobacco products ever tried).
Results
The hypothesized mediation was supported for both domains of impulsivity (impaired self-regulation a1b=.09, SE=.02, 95%CI [.03–.14], p=.002; behavioral impulsivity a2b=.07, SE=.03, 95 CI [.01–.14], p=.03). Specifically, impaired self-regulation (B=−.33, SE=.06, p<.001) and behavioral impulsivity (B=−.26, SE=.11, p=.02) predicted trying e-cigarettes at an earlier age, and earlier initiation was associated with more days of e-cigarette use in the past month (B=−.28, SE=.08, p<.001).
Conclusions
Adolescents who endorse aspects of impulsivity, such as acting without thinking, are at greater risk for more frequent e-cigarette use through an early age of e-cigarette initiation. Further research is needed to evaluate these relationships longitudinally and to develop targeted e-cigarette interventions for impulsive youth.
Keywords: youth, e-cigarette, tobacco, impulsivity, initiation
1 Introduction
National data estimate 3 million youth currently use e-cigarettes, and e-cigarettes are now the most commonly used tobacco product among middle and high school students (Singh et al., 2016). Although limited evidence exists regarding the long-term effects of e-cigarette use, e-liquids contain chemicals that are toxic when heated and inhaled (Farsalinos et al., 2015; Kosmider et al., 2014; Kosmider et al., 2016) leading to concerns that e-cigarette use among youth could pose significant health consequences. Understanding risk factors for e-cigarette use during adolescence is critical for developing prevention and intervention efforts and is an important research priority according to the recent U.S. Surgeon General report (USDHHS, 2016).
1.1 Impulsivity and e-Cigarette Use
Prior research has identified impulsivity, or a predisposition toward rapid, unplanned action without regard for negative consequences (Barratt et al., 1975; Moeller et al., 2001), as a key risk factor for adolescent substance use (Fernie et al., 2013; Quinn and Harden, 2013; Stautz and Cooper, 2013), including heavier and more persistent tobacco use (Balevich et al., 2013; Chase and Hogarth, 2011; Fields et al., 2009; Primack et al., 2015; Reynolds et al., 2007) and poorer substance use treatment outcomes (Stevens et al., 2014). Although much of this research has examined conventional cigarette use, initial evidence indicates that impulsivity is also associated with e-cigarette use. For example, self-reported impulsivity is higher among youth who use e-cigarettes versus those who do not use e-cigarettes (Leventhal et al., 2015; Wills et al., 2015), and results from a recent, longitudinal cohort study indicate that impulsivity is associated with ever use of e-cigarettes two years later (Hanewinkel and Isensee, 2015). Although emerging evidence indicates a positive association between impulsivity and e-cigarette use, the potential reasons for this association remain unexplored. Identifying potential mediators of the relationship between impulsivity and e-cigarette use among youth could inform the development of targeted e-cigarette prevention and intervention efforts.
1.2 Impulsivity and Early Age of Onset
Age of onset may be one factor that mediates the association between impulsivity and e-cigarette use. Evidence indicates impulsivity is associated with an earlier age of onset of a variety of substances, including combustible tobacco products (Dom et al., 2006; Elkins et al., 2007; Tarter et al., 2003; Verdejo-García et al., 2008), yet it is currently unknown whether a similar relationship exists between impulsivity and early age of onset of e-cigarette use. It is possible that e-cigarettes are especially attractive to impulsive adolescents due to novel product designs such as the ability to customize the device (Brown and Cheng, 2014) and the wide variety of unique e-liquid flavors (Zhu et al., 2014), or due to other factors such as targeted marketing (USDHHS, 2016), or social influences such as peer use (Barrington-Trimis et al., 2015; Wills et al., 2015).
1.3 Age of Onset and E-Cigarette Use
The relationship between age of onset and future use has also not been examined for e-cigarettes, yet there is substantial evidence that youth who first try conventional cigarette smoking at an earlier age are at increased risk for heavier long-term use, greater nicotine dependence, and greater difficulty quitting smoking (Behrendt et al., 2009; Buchmann et al., 2013; Kendler et al., 2013; Lanza and Vasilenko, 2015; Nelson et al., 2015). The association between age of onset and future substance use is further supported by longitudinal evidence indicating that early adolescent substance use interventions that delay the age of onset of substance use are effective at reducing the frequency of future use and associated problems across a range of substances (e.g., alcohol, cigarettes, illicit drug use) (Spoth et al., 2009). It is possible that these findings of a significant association between early age of onset and future substance use would also extend to e-cigarette use. Younger adolescents report that e-cigarettes are the first tobacco product that they tried (Krishnan-Sarin et al., 2015), and e-cigarette use is now more prevalent than conventional cigarette use among youth (Singh et al., 2016), suggesting that e-cigarettes may be an adolescent’s first exposure to nicotine. Consequently, youth who try e-cigarettes at an earlier age may then be more vulnerable to heavier or more problematic future use given the sensitivity of the developing brain to the reinforcing properties of nicotine (Counotte et al., 2011; Dwyer et al., 2009; Yuan et al., 2015).
1.4 Hypothesized Mediation
Based on these findings, it stands to reason that impulsivity may be associated with an earlier age of onset of e-cigarette use, which is subsequently related to a greater frequency of e-cigarette use. However, no studies to date have tested this potential mediation. The current investigation aims to fill important gaps in the literature on e-cigarette use by examining associations among impulsivity, age of onset, and e-cigarette use frequency in a sample of high-school youth. We examined whether the relationship between impulsivity and frequency of e-cigarette use was mediated by an earlier age of onset of e-cigarette use, after controlling for covariates that have been shown to relate to e-cigarette use (i.e., sex, age, race, ever use of other tobacco products, and e-cigarette use with peers) (Barrington-Trimis et al., 2015; Krishnan-Sarin et al., 2015; Wills et al., 2015). Given prior substance use research, we expected that greater impulsivity would be associated with an earlier age of onset, and that an earlier age of onset would predict more frequent e-cigarette use (more days of use in the past month). If impulsive adolescents are especially vulnerable to early e-cigarette initiation, and an early age of onset leads to heavier or more problematic e-cigarette use, then e-cigarette prevention efforts targeted to younger, impulsive youth may be imperatively needed.
2 Method
2.1 Survey Procedures
Youth from 8 Southeastern Connecticut (CT) high schools were surveyed in Spring 2015 (N=7045). To obtain a socio-demographically diverse sample, these schools were drawn from 7 of 9 district reference groups, which are groupings of schools based on family income levels, parental education and occupation levels, and use of non-English language in the home (Connecticut State Department of Education, 2006).
Study procedures were approved by the Yale University Institutional Review Board and school administrators. Parents were contacted in advance of the study and could indicate if they did not want their child to participate. Students were informed that their participation was voluntary and data were anonymous. Individual paper-and-pencil surveys were distributed school-wide (grades 9–12) during homeroom periods. The response rate based on attendance on the day of the survey administration was high (83.8%).
2.2 Sample
Two survey versions were randomly distributed throughout the 8 high schools. Current analyses focus on a subsample of youth (n=3474) who received the survey version containing impulsivity items (measures described in detail below). Individuals receiving the impulsivity items did not differ from those receiving the other survey version in terms of sex, age, race, age of e-cigarette onset, ever use of e-cigarettes, or e-cigarette frequency in the past 30 days (p-values > 0.10).
2.3 Measures
2.3.1 Demographics
Participants reported demographic characteristics including age, sex (male/female), and race/ethnicity (select all that apply: White/Caucasian, Black/African American, Hispanic/Latino, Asian, American Indian or Alaskan Native, Native Hawaiian or other Pacific Islander, Middle Eastern, Other).
2.3.2 Impulsivity
Impulsivity was assessed with 8 items from the adolescent version of the Barratt Impulsiveness Scale-11 (Fossati et al., 2002; Patton et al., 1995). Prior research validated the psychometric properties of an abbreviated 8-item version (Morean et al., 2014) and confirms that impulsivity assessed with this 8-item scale is related to tobacco use outcomes in adolescents (Morean et al., 2015). Item responses include 1 “rarely/never”, 2 “occasionally”, 3 “often”, 4 “almost always/always” and were averaged to create two, 4-item subscale scores representing: Impaired Self-Regulation (i.e., reverse-scored items: “I plan what I have to do”, “I am self-controlled”, “I concentrate easily”, and “I like to think carefully about things”) and Behavioral Impulsivity (i.e., “I do things without thinking”, “I do not pay attention”, “I say things without thinking”, and “I act on the spur of the moment”) (Morean et al., 2014; Morean et al., 2015). The two-factor latent structure from previous research was confirmed with the current scale in this sample based on indices of good fit to the data (model fit indices: CFI=0.97, RMSEA=.06, SRMR=0.04). The subscales also had good internal consistency (Cronbach’s α=.80 for both subscales).
2.3.3 E-Cigarette Use
E-cigarette use was assessed by asking “Have you ever tried e-cigarettes (yes/no)?”. Open-ended responses characterized age of onset of e-cigarette use (i.e., “How old were you when you first tried an e-cigarette?”) and frequency of e-cigarette use (i.e., “How many days out of the past 30 did you use e-cigarettes?”).
2.3.4 E-Cigarette Use with Peers
E-cigarette use with peers was assessed by asking “When you use an e-cigarette, who do you use it with?”. Youth could select all that apply from response options including “I do not use e-cigarettes” or alone, with friends, sibling/cousin, or parents. Use of e-cigarettes with either friends or sibling/cousin is characterized subsequently as use with peers.
2.3.5 Other Tobacco Use
Ever use of other tobacco products (i.e., cigarettes, cigars, cigarillos, smokeless tobacco, blunts, hookah) was assessed by asking students if they had ever tried each product (yes/no). Affirmative responses were added to create the total number of other tobacco products ever tried.
2.4 Statistical Analysis
Descriptive statistics were used to characterize predictors of interest. Analyses were run with Mplus (version 6.12) using maximum likelihood estimation with robust standard errors. All models included school as a cluster variable. First, unadjusted regression models examined the direct associations between 1) both impulsivity factors (independent variables) and age of e-cigarette onset (mediator variable), and 2) age of onset (mediator variable) and number of days of e-cigarette use in the past month (dependent variable). Frequency of e-cigarette use was a count variable (range 0–30 days, with 38.0% reporting no use in the past month), so models specified a negative binomial distribution with log-link function for this outcome. Then, a mediation model tested whether impulsivity was indirectly associated with e-cigarette frequency through an early age of onset. Age of onset was regressed on both factors of impulsivity and covariates related to e-cigarette use (i.e., sex, race, use of e-cigarettes with peers, and total number of other tobacco products ever used). E-cigarette frequency was regressed on both factors of impulsivity, age of onset of e-cigarette use, current age at the time of the survey, and other covariates (sex, race, use of e-cigarettes with peers, and total number of other tobacco products ever used). The mediated effect is estimated as the product of the path between impulsivity and age of onset (a paths) and the path between age of onset and e-cigarette frequency (b path) (Hayes, 2013). Standard errors and confidence intervals around the indirect effects (ab) were calculated to determine statistical significance of the mediation. The model simultaneously included both impulsivity factors to estimate the unique variance accounted for by each factor after considering the variance accounted for by the other.
3 Results
3.1 Sample
Among the subsample of n=3,474 high school students surveyed, 930 reported ever trying an e-cigarette (26.8%). Three youth were dropped from analyses due to invalid data (i.e., reporting an older age of e-cigarette onset than current age at the time of the survey), leaving n=927 for the analyses. Consistent with prior research (e.g., (Leventhal et al., 2015; Wills et al., 2015), average impulsivity scores were higher among youth who had ever tried e-cigarettes compared to non-users (Impaired Self-Regulation: users M=2.20, SD=0.73; non-users M=2.01, SD=0.77; Behavioral Impulsivity: users M=2.14, SD=0.68; non-users M=1.90, SD=0.64, p-values <.001).
Extreme age of onset values were set to the lower limit (3 standard deviations from the mean) to reduce the influence of outliers (n=10). Complete cases on all predictors and covariates were available for n=663 participants (71.5%). Survey item non-response may be due in part to unexpected time constraints during survey administration which did not provide enough time for all students to complete the survey. To assess for potential bias from missing data, analyses were run first with complete cases and then where missing data were imputed using multiple imputation methods (n=100 imputations) (Rubin, 2004; Schafer, 1997). Results were consistent in both analyses, so complete case analyses for the mediation results are presented below.
3.2 Participants
The total sample of ever e-cigarette users (n=927) was 44.7% female. Participants selected all that applied for their race/ethnicity. The majority selected White (70.8%) so race/ethnicity was categorized as White vs. other for analyses. Other responses included Black/African American (10.9%), Hispanic/Latino (22.1%), Asian (3.0%), American Indian or Alaskan Native (2.4%), Native Hawaiian or other Pacific Islander (<1%), Middle Eastern (<2%), Other (2%). The sample included youth from grades 9–12 and was approximately evenly distributed across grades (21.3%–27.5% from each grade). On average, youth were 14.7 (SD=1.6, range 9–19) years old when they first tried an e-cigarette, and the average age at the time of the survey was 16.2 (SD=1.2, range 14–19). Over half of the sample reported using e-cigarettes with their peers (56.9%), and the average number of other tobacco products ever tried was 2.5 (SD=1.8).
3.3 Impulsivity and Early Age of Onset
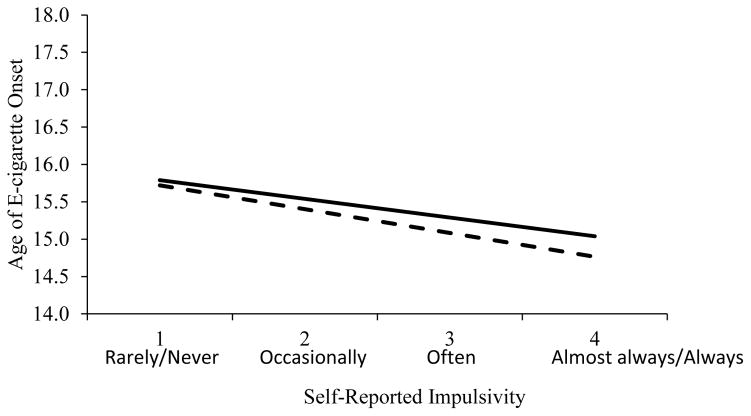
Results from unadjusted regression models indicated both impaired self-regulation (B=−.32, SE=.06, p<.001) and behavioral impulsivity (B=−.25, SE=.10, p=.02) were associated with an earlier age of onset. Figure 1 displays the predicted age of onset based on the average impulsivity scores. Results indicate high trait impulsivity reported as impaired self-regulation or behavioral impulsivity “almost always/always” is associated with first trying e-cigarettes almost one year earlier than low trait impulsivity reported “rarely/never”.
Figure 1.
Predicted age of e-cigarette onset based on average impaired self-regulation and behavioral impulsivity. Note: Impulsivity values represent average scores across the four-item scales, demonstrating that the estimated age of onset of e-cigarette use decreases as average impulsivity scores increase. Dashed line: impaired self-regulation; Solid line: behavioral impulsivity.
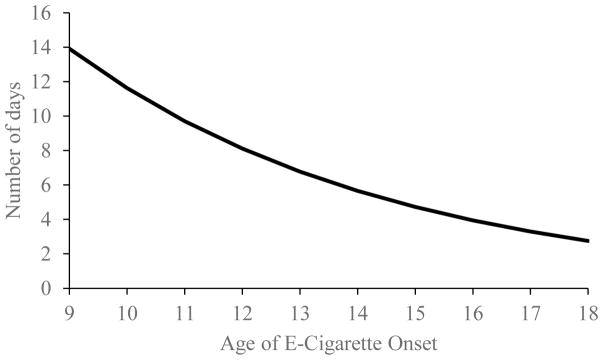
3.4 Early Age of Onset and Frequency of E-Cigarette Use
Additionally, age of onset was negatively related to the frequency of e-cigarette use in unadjusted regression models, such that an earlier age of onset was associated with more days of e-cigarette use in the past month (B=−.18, SE=.04, p<.001). Figure 2 displays the predicted past month e-cigarette frequency based on age of onset. E-cigarette frequency decreases in a nonlinear pattern with increasing age of onset. For example, the estimated past 30-day frequency of e-cigarette use is 10 times greater for youth reporting first trying e-cigarettes at age 9 compared to age 18.
Figure 2.
Predicted past 30-day e-cigarette frequency based on age of e-cigarette onset. Note: E-cigarette frequency is measured as the number of days of use in the past month, indicating that the estimated frequency of past-month e-cigarette use decreases as age of onset decreases.
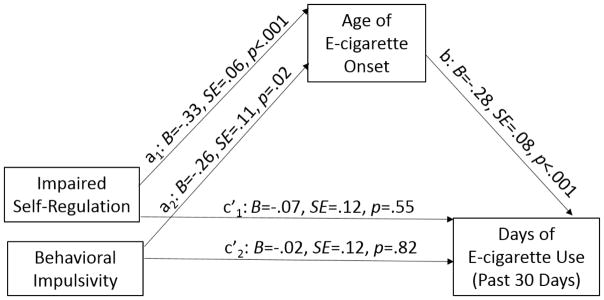
3.5 Early Age of Onset Mediates Relations Between Impulsivity and Frequency of E-Cigarette Use
The hypothesized mediation was supported (Figure 3). When controlling for other covariates related to e-cigarette use (i.e., sex, race, e-cigarette use with peers, the number of other tobacco products tried), both facets of impulsivity were associated with an earlier age of onset of e-cigarette use (a paths) (Table 1). Additionally, an earlier age of onset predicted more days of e-cigarette use in the past month while controlling for impulsivity (b path), even when accounting for current age at the time of the survey and other covariates related to e-cigarette use (Table 2). Both indirect paths were statistically significant (impaired self-regulation a1b=.09, SE=.02, 95% CI=.03–.14, p=.002; behavioral impulsivity a2b=.07, SE=.03, 95% CI=.01–.14, p=.03), indicating that adolescents who endorsed aspects of impulsivity (such as difficulty with self-regulation or acting without thinking) were using e-cigarettes more frequently due to the risk conferred by initiating e-cigarette use at an earlier age.
Figure 3.
Early age of onset mediates the association between impulsivity and frequency of e-cigarette use. Note: The model includes school as a cluster variable. Estimates are adjusted for all predictors in the model and other covariates related to e-cigarette use (sex, age, race, e-cigarette use with peers, and total number of other tobacco products ever tried).
Table 1.
Regression results predicting age of e-cigarette onset
| Variable | B | SE | Beta | t | p |
|---|---|---|---|---|---|
| Impaired Self-Regulation | −0.33 | 0.06 | −0.15 | −5.42 | <.001 |
| Behavioral Impulsivity | −0.26 | 0.11 | −0.12 | −2.30 | 0.02 |
| Male (vs. Female) | 0.08 | 0.12 | 0.06 | 0.70 | 0.48 |
| White (vs. Other) | 0.12 | 0.10 | 0.08 | 1.24 | 0.21 |
| E-cigarette use with peers: Yes (vs. No) | −0.24 | 0.08 | −0.16 | −3.10 | 0.002 |
| Number of other tobacco products used | −0.08 | 0.03 | −0.09 | −2.33 | 0.02 |
Note: Impulsivity factors (impaired self-regulation and behavioral impulsivity) predicted age of e-cigarette onset (mediator variable). Impulsivity factors were computed as average scores from two four-item subscales adapted from the adolescent version of the Barratt Impulsiveness Scale-11 (Fossati et al., 2002; Morean et al., 2014). The number of other tobacco products used includes ever-use of cigarettes, cigars, cigarillos, smokeless tobacco, blunts, or hookah.
Table 2.
Regression results predicting number of days of e-cigarette use in the past 30 days
| Variable | B | SE | Beta | t | p |
|---|---|---|---|---|---|
| Age of onset | −0.28 | 0.08 | −0.54 | −3.66 | <.001 |
| Impaired Self-Regulation | −0.07 | 0.12 | −0.06 | −0.60 | 0.55 |
| Behavioral Impulsivity | −0.02 | 0.12 | −0.02 | −0.22 | 0.82 |
| Current Age | 0.30 | 0.06 | 0.48 | 5.06 | <.001 |
| Male (vs. Female) | 0.40 | 0.19 | 0.52 | 2.06 | 0.04 |
| White (vs. Other) | −0.16 | 0.18 | 0.20 | −0.88 | 0.38 |
| E-cigarette use with peers: Yes (vs. No) | 0.73 | 0.16 | 0.95 | 4.56 | <.001 |
| Number of other tobacco products used | 0.08 | 0.07 | 0.20 | 1.22 | 0.22 |
Note: Age of onset (mediator variable) predicted e-cigarette frequency (number of days of reported use in the past month) while accounting for both impulsivity factors (impaired self-regulation and behavioral impulsivity). Impulsivity factors were computed as average scores from two four-item subscales adapted from the adolescent version of the Barratt Impulsiveness Scale-11 (Fossati et al., 2002; Morean et al., 2014). The number of other tobacco products used includes ever-use of cigarettes, cigars, cigarillos, smokeless tobacco, blunts, or hookah.
4 Discussion
The current study examined associations among impulsivity, age of onset, and frequency of e-cigarette use in a sample of high-school youth. Importantly, our results indicate that youth e-cigarette users who had greater impaired self-regulation and behavioral impulsivity were more likely to try e-cigarettes at an earlier age, and that earlier initiation was associated with using e-cigarettes on more days in the past month. In other words, impulsive adolescents were at a greater risk for more frequent e-cigarette use because they started to use e-cigarettes at an earlier age compared to their less impulsive peers.
The current findings extend previous research related to other tobacco product use (Buchmann et al., 2013; Elkins et al., 2007; Kendler et al., 2013; Lanza and Vasilenko, 2015) and indicate that impulsivity also is a significant risk factor for early e-cigarette initiation. Identifying risk factors for early e-cigarette use is critical for informing prevention efforts, given concerns about the possible negative health consequences of e-cigarette use (Farsalinos et al., 2015; Kosmider et al., 2014; USDHHS, 2016). Our results indicate the average age of first trying an e-cigarette was around 14 years old, although many youth reported trying e-cigarettes even earlier, so targeting younger adolescents may be critical for preventing initiation of e-cigarette use. Evidence suggests mass media campaigns (e.g., Real Cost, Truth) are effective at reaching both youth and young adults to prevent the initiation of conventional cigarette smoking and reduce progression to established smoking (Farrelly et al., 2017), so future efforts should consider extending these campaigns to address e-cigarette use as well. Additionally, it may be important to design interventions tailored to impulsive youth to prevent continued or heavier e-cigarette use among this high-risk group. Although impulsive adolescent smokers often have poor smoking cessation outcomes compared to youth who are less impulsive (Krishnan-Sarin et al., 2007), recent evidence suggests contingency management interventions may be effective at improving abstinence rates among impulsive adolescents who smoke cigarettes (Morean et al., 2015). Similarly, other strategies targeting impulsive youth through school-based prevention programs have been shown to be effective at reducing future substance use behavior, such as alcohol use (Conrod et al., 2013). Further work is needed to evaluate whether the types of prevention and intervention efforts that have been effective in reducing other substance use among impulsive youth can also be used to prevent e-cigarette initiation among never-users and promote cessation among e-cigarette using adolescents.
Additionally, it will be important to consider how the development and enforcement of new e-cigarette regulatory strategies influence the appeal and use of e-cigarettes among youth. Evidence suggests youth find many aspects of e-cigarettes appealing, including the wide variety of flavors and ability to use these products in unique ways such as for smoke tricks or ‘dripping’(Kong et al., 2015; Krishnan-Sarin et al., 2015; Krishnan-Sarin et al., 2017; Wagoner et al., 2016). E-cigarette devices themselves may also be appealing as they come in many different designs (e.g., tanks, cartridges) with elements that can be customized by the user (e.g., color, voltage, temperature, flavor) (Brown and Cheng, 2014). Importantly, the novelty of e-cigarette use may be especially appealing to highly impulsive youth, who tend to act without thinking and without regard for possible negative consequences. Given that the long-term effects of e-cigarette use among youth remain unknown (Grana et al., 2014; Pepper and Brewer, 2014; USDHHS, 2016), it will be important for future research to identify what aspects of e-cigarettes are especially appealing to impulsive youth and develop effective regulatory strategies and education programs to reduce the appeal of e-cigarettes to these high-risk youth.
While the current results provide new information and have potentially important implications, the following limitations and future directions should be considered. First, the results are based on cross-sectional data, so the temporal sequencing of the variables cannot be confirmed. However, the average age of e-cigarette onset was younger than the current age at the time of the survey when e-cigarette frequency was assessed, lending support to the chronological timing of the mediator and outcome. In terms of the association between the predictor and the mediator, it is possible that early e-cigarette use is driven by a pre-existing vulnerability of poor self-regulation or behavioral impulsivity. It also is possible that these associations are bidirectional such that e-cigarette use influences impulse control and reward processes that motivate continued use. Future longitudinal work will be needed to further explicate these potential pathways. Second, we surveyed a relatively diverse area in Connecticut including multiple schools; however, our results may not generalize to samples with different demographic characteristics or from other geographic locations. The current results suggest that national surveys of youth tobacco use should consider including impulsivity as a potential psychosocial risk factor to better understand how it relates to e-cigarette onset and use. We observed consistent results across two facets of impulsivity, impaired self-regulation (e.g., problems with concentration or self-control) and behavioral impulsivity (e.g., acting without thinking), and future studies may also want to consider the effects of other facets of impulsivity (e.g., sensation seeking) on e-cigarette use. Third, analyses relied on self-reported data and are subject to response bias (e.g., student willingness to complete the survey) and potential recall error (e.g., incorrectly recalling age of onset). Additionally, survey responses on predictors of interest were missing for a portion of the sample. However, results were consistent whether using complete cases or multiple imputation to correct for missing data, further strengthening confidence in the current findings. While our results indicate that an early age of e-cigarette onset helped explain the relationships between impulsivity and e-cigarette frequency above and beyond demographic factors (e.g., sex, race, current age) and other factors related to e-cigarette use (e.g., e-cigarette use with peers and use of other tobacco products), there may be other important factors that we did not assess that could influence e-cigarette use among adolescents. Additional research is needed on other individual or contextual factors that may also influence the observed mediation to help inform optimal intervention delivery. For example, evidence suggests both impulsivity and early age of onset of cigarette smoking are related to stronger smoking reinforcement (e.g., pleasurable effects) (Buchmann et al., 2013; Doran et al., 2007) which may contribute to smoking motivation and be a useful target for intervention. This relationship has been seen previously for conventional cigarette use, and it is possible that similar effects exist for e-cigarettes. Finally, our primary outcome focused on the frequency of e-cigarette use in the past month, and further research is needed to understand how impulsivity and age of onset influence other measures of e-cigarette use, including quantity of use and transitions to more long-term use or other substance use.
5.0 Conclusion
The current study is the first to examine associations among impulsivity, age of onset, and e-cigarette frequency in youth. The results suggest that an early age of onset is a possible pathway that can help explain the association between impulsivity and e-cigarette frequency among adolescents who use e-cigarettes. Given that youth who endorse aspects of impulsivity, such as acting without thinking, are at greater risk for early e-cigarette experimentation and more frequent e-cigarette use, there is a critical need for future research aimed at developing effective prevention and intervention programs for this vulnerable group.
Highlights.
School-wide surveys assessed e-cigarette use behaviors among high school students
Greater impulsivity was associated with trying e-cigarettes at an earlier age
Early age of onset was associated with more frequent e-cigarette use
Age of onset mediated the association between impulsivity and e-cigarette frequency
Acknowledgments
Funding Source
This work was supported by grants from National Institute on Drug Abuse and the FDA Center for Tobacco Products, Yale TCORS P50DA036151, P50DA009241, T32DA019426, and L40DA042454. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Footnotes
Contributors
All authors have participated in the concept and design; analysis and interpretation of data; drafting and revising the manuscript; and have approved the manuscript as submitted.
Conflicts of Interest
No conflict declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Balevich EC, Wein ND, Flory JD. Cigarette smoking and measures of impulsivity in a college sample. Subst Abuse. 2013;34:256–62. doi: 10.1080/08897077.2012.763082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barratt ES, Patton J, Stanford M. Barratt Impulsiveness Scale. Barratt-Psychiatry Medical Branch, University of Texas; 1975. [Google Scholar]
- Barrington-Trimis JL, Berhane K, Unger JB, Cruz TB, Huh J, Leventhal AM, Urman R, Wang K, Howland S, Gilreath TD. Psychosocial factors associated with adolescent electronic cigarette and cigarette use. Pediatrics. 2015;136:308–17. doi: 10.1542/peds.2015-0639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrendt S, Wittchen HU, Höfler M, Lieb R, Beesdo K. Transitions from first substance use to substance use disorders in adolescence: Is early onset associated with a rapid escalation? Drug Alcohol Depend. 2009;99:68–78. doi: 10.1016/j.drugalcdep.2008.06.014. [DOI] [PubMed] [Google Scholar]
- Brown CJ, Cheng JM. Electronic cigarettes: Product characterisation and design considerations. Tob Control. 2014;23:ii4–ii10. doi: 10.1136/tobaccocontrol-2013-051476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchmann AF, Blomeyer D, Jennen-Steinmetz C, Schmidt MH, Esser G, Banaschewski T, Laucht M. Early smoking onset may promise initial pleasurable sensations and later addiction. Addict Biol. 2013;18:947–54. doi: 10.1111/j.1369-1600.2011.00377.x. [DOI] [PubMed] [Google Scholar]
- Chase HW, Hogarth L. Impulsivity and symptoms of nicotine dependence in a young adult population. Nicotine Tob Res. 2011;13:1321–5. doi: 10.1093/ntr/ntr114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connecticut State Department of Education. [accessed on 1];District Reference Groups, 2006. 2006 http://sdeportal.ct.gov/Cedar/Files/Pdf/Reports/db_drg_06_2006.pdf.
- Conrod PJ, O’Leary-Barrett M, Newton N, Topper L, Castellanos-Ryan N, Mackie C, Girard A. Effectiveness of a selective, personality-targeted prevention program for adolescent alcohol use and misuse: A cluster randomized controlled trial. JAMA Psychiatry. 2013;70:334–342. doi: 10.1001/jamapsychiatry.2013.651. [DOI] [PubMed] [Google Scholar]
- Counotte DS, Smit AB, Pattij T, Spijker S. Development of the motivational system during adolescence, and its sensitivity to disruption by nicotine. Dev Cogn Neurosci. 2011;1:430–443. doi: 10.1016/j.dcn.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dom G, Hulstijn W, Sabbe B. Differences in impulsivity and sensation seeking between early-and late-onset alcoholics. Addict Behav. 2006;31:298–308. doi: 10.1016/j.addbeh.2005.05.009. [DOI] [PubMed] [Google Scholar]
- Doran N, McChargue D, Cohen L. Impulsivity and the reinforcing value of cigarette smoking. Addict Behav. 2007;32:90–8. doi: 10.1016/j.addbeh.2006.03.023. [DOI] [PubMed] [Google Scholar]
- Dwyer JB, McQuown SC, Leslie FM. The dynamic effects of nicotine on the developing brain. Pharmacol Ther. 2009;122:125–39. doi: 10.1016/j.pharmthera.2009.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkins IJ, McGue M, Iacono WG. Prospective effects of attention-deficit/hyperactivity disorder, conduct disorder, and sex on adolescent substance use and abuse. Arch Gen Psychiatry. 2007;64:1145–52. doi: 10.1001/archpsyc.64.10.1145. [DOI] [PubMed] [Google Scholar]
- Farrelly MC, Duke JC, Nonnemaker JM, MacMongele AJ, Alexander TN, Zhao X, Delahanty JC, Rao P, Allen J. Association between the real cost media campaign and smoking initiation among youths—United States, 2014–2016. MMWR Morbid Mortal Wkly Rep. 2017;66:47–50. doi: 10.15585/mmwr.mm6602a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farsalinos KE, Kistler KA, Gillman G, Voudris V. Evaluation of electronic cigarette liquids and aerosol for the presence of selected inhalation toxins. Nicotine Tob Res. 2015;17:168–74. doi: 10.1093/ntr/ntu176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernie G, Peeters M, Gullo MJ, Christiansen P, Cole JC, Sumnall H, Field M. Multiple behavioural impulsivity tasks predict prospective alcohol involvement in adolescents. Addiction. 2013;108:1916–23. doi: 10.1111/add.12283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fields S, Collins C, Leraas K, Reynolds B. Dimensions of impulsive behavior in adolescent smokers and nonsmokers. Exp Clin Psychopharmacol. 2009;17:302–11. doi: 10.1037/a0017185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fossati A, Barratt ES, Acquarini E, Di Ceglie A. Psychometric properties of an adolescent version of the Barratt Impulsiveness Scale-11 for a sample of Italian high school students. Percep Mot Skills. 2002;95:621–35. doi: 10.2466/pms.2002.95.2.621. [DOI] [PubMed] [Google Scholar]
- Grana RA, Benowitz N, Glantz SA. E-cigarettes: A scientific review. Circulation. 2014;129:1972–86. doi: 10.1161/CIRCULATIONAHA.114.007667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanewinkel R, Isensee B. Risk factors for e-cigarette, conventional cigarette, and dual use in German adolescents: a cohort study. Prev Med. 2015;74:59–62. doi: 10.1016/j.ypmed.2015.03.006. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Kendler KS, Myers J, Damaj MI, Chen X. Early smoking onset and risk forsubsequent nicotine dependence: A monozygotic co-twin control study. Am J Psychiatry. 2013;170:408–13. doi: 10.1176/appi.ajp.2012.12030321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kong G, Morean ME, Cavallo DA, Camenga DR, Krishnan-Sarin S. Reasons for electronic cigarette experimentation and discontinuation among adolescents and young adults. Nicotine Tob Res. 2015;17:847–54. doi: 10.1093/ntr/ntu257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosmider L, Sobczak A, Fik M, Knysak J, Zaciera M, Kurek J, Goniewicz ML. Carbonyl compounds in electronic cigarette vapors: effects of nicotine solvent and battery output voltage. Nicotine Tob Res. 2014;16:1319–26. doi: 10.1093/ntr/ntu078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosmider L, Sobczak A, Prokopowicz A, Kurek J, Zaciera M, Knysak J, Smith D, Goniewicz M. Cherry-flavoured electronic cigarettes exposure users to the inhalation irritant, benzaldehyde. Thorax. 2016;71:376–7. doi: 10.1136/thoraxjnl-2015-207895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Morean ME, Camenga DR, Cavallo DA, Kong G. E-cigarette use among high school and middle school adolescents in Connecticut. Nicotine Tob Res. 2015;17:810–8. doi: 10.1093/ntr/ntu243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Morean ME, Kong G, Bold KW, Camenga DR, Cavallo D, Wu R. “Dripping” among youth using e-cigarettes. Pediatrics. 2017;139:e20163224. doi: 10.1542/peds.2016-3224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krishnan-Sarin S, Reynolds B, Duhig AM, Smith A, Liss T, McFetridge A, Cavallo DA, Carroll KM, Potenza MN. Behavioral impulsivity predicts treatment outcome in a smoking cessation program for adolescent smokers. Drug Alcohol Depend. 2007;88:79–82. doi: 10.1016/j.drugalcdep.2006.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanza ST, Vasilenko SA. New methods shed light on age of onset as a risk factor for nicotine dependence. Addict Behav. 2015;50:161–4. doi: 10.1016/j.addbeh.2015.06.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leventhal AM, Strong DR, Kirkpatrick MG, Unger JB, Sussman S, Riggs NR, Stone MD, Khoddam R, Samet JM, Audrain-McGovern J. Association of electronic cigarette use with initiation of combustible tobacco product smoking in early adolescence. JAMA. 2015;314:700–7. doi: 10.1001/jama.2015.8950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moeller FG, Barratt ES, Dougherty DM, Schmitz JM, Swann AC. Psychiatric aspects of impulsivity. Am J Psychiatry. 2001;158:1783–93. doi: 10.1176/appi.ajp.158.11.1783. [DOI] [PubMed] [Google Scholar]
- Morean ME, DeMartini KS, Leeman RF, Pearlson GD, Anticevic A, Krishnan-Sarin S, Krystal JH, O’Malley SS. Psychometrically improved, abbreviated versions of three classic measures of impulsivity and self-control. Psychol Assess. 2014;26:1003–20. doi: 10.1037/pas0000003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morean ME, Kong G, Camenga DR, Cavallo DA, Carroll KM, Pittman B, Krishnan-Sarin S. Contingency management improves smoking cessation treatment outcomes among highly impulsive adolescent smokers relative to cognitive behavioral therapy. Addict Behav. 2015;42:86–90. doi: 10.1016/j.addbeh.2014.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson SE, Van Ryzin MJ, Dishion TJ. Alcohol, marijuana, and tobacco use trajectories from age 12 to 24 years: Demographic correlates and young adult substance use problems. Dev Psychopathol. 2015;27:253–277. doi: 10.1017/S0954579414000650. [DOI] [PubMed] [Google Scholar]
- Patton JH, Stanford MS, Barratt ES. Factor structure of the Barratt impulsiveness scale. J Clin Psychol. 1995;51:768–774. doi: 10.1002/1097-4679(199511)51:6<768::aid-jclp2270510607>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- Pepper JK, Brewer NT. Electronic nicotine delivery system (electronic cigarette) awareness, use, reactions and beliefs: A systematic review. Tob Control. 2014;23:375–384. doi: 10.1136/tobaccocontrol-2013-051122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Primack BA, Soneji S, Stoolmiller M, Fine MJ, Sargent JD. Progression to traditional cigarette smoking after electronic cigarette use among US adolescents and young adults. JAMA Pediatr. 2015;169:1018–1023. doi: 10.1001/jamapediatrics.2015.1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quinn PD, Harden KP. Differential changes in impulsivity and sensation seeking and the escalation of substance use from adolescence to early adulthood. Dev Psychopathol. 2013;25:223–239. doi: 10.1017/S0954579412000284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reynolds B, Patak M, Shroff P, Penfold RB, Melanko S, Duhig AM. Laboratory and self-report assessments of impulsive behavior in adolescent daily smokers and nonsmokers. Exp Clin Psychopharmacol. 2007;15:264. doi: 10.1037/1064-1297.15.3.264. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. John Wiley and Sons; 2004. [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. CRC press; 1997. [Google Scholar]
- Singh T, Arrazola RA, Corey CG, Husten CG, Neff LJ, Homa DM, King BA. Tobacco use among middle and high school students—United States, 2011–2015. MMWR Morbid Mortal Wkly Rep. 2016;65:361–7. doi: 10.15585/mmwr.mm6514a1. [DOI] [PubMed] [Google Scholar]
- Spoth R, Trudeau L, Guyll M, Shin C, Redmond C. Universal intervention effects on substance use among young adults mediated by delayed adolescent substance initiation. J Consult Clin Psychol. 2009;77:620. doi: 10.1037/a0016029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stautz K, Cooper A. Impulsivity-related personality traits and adolescent alcohol use: A meta-analytic review. Clin Psychol Rev. 2013;33:574–592. doi: 10.1016/j.cpr.2013.03.003. [DOI] [PubMed] [Google Scholar]
- Stevens L, Verdejo-García A, Goudriaan AE, Roeyers H, Dom G, Vanderplasschen W. Impulsivity as a vulnerability factor for poor addiction treatment outcomes: A review of neurocognitive findings among individuals with substance use disorders. J Subst Abuse Treat. 2014;47:58–72. doi: 10.1016/j.jsat.2014.01.008. [DOI] [PubMed] [Google Scholar]
- Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, Gardner W, Blackson T, Clark D. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am J Psychiatry. 2003;160:1078–1085. doi: 10.1176/appi.ajp.160.6.1078. [DOI] [PubMed] [Google Scholar]
- USDHHS; U.S. Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Chronic Disease Prevention and Health Promotion; Office on Smoking and Health, editor. A report of the Surgeon General. Atlanta, GA: 2016. E-cigarette use among youth and young adults. [Google Scholar]
- Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: Review of findings from high-risk research, problem gamblers and genetic association studies. Neurosci Biobehav Rev. 2008;32:777–810. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Wagoner KG, Cornacchione J, Wiseman KD, Teal R, Moracco KE, Sutfin E. E-cigarettes, hookah pens and vapes: Adolescent and young adult perceptions of electronic nicotine delivery systems. Nicotine Tob Res. 2016;18:2006–12. doi: 10.1093/ntr/ntw095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Knight R, Williams RJ, Pagano I, Sargent JD. Risk factors for exclusive e-cigarette use and dual e-cigarette use and tobacco use in adolescents. Pediatrics. 2015;135:e43–e51. doi: 10.1542/peds.2014-0760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan M, Cross SJ, Loughlin SE, Leslie FM. Nicotine and the adolescent brain. J Physiol. 2015;593:3397–3412. doi: 10.1113/JP270492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S-H, Sun JY, Bonnevie E, Cummins SE, Gamst A, Yin L, Lee M. Four hundred and sixty brands of e-cigarettes and counting: implications for product regulation. Tob Control. 2014;23:iii3–iii9. doi: 10.1136/tobaccocontrol-2014-051670. [DOI] [PMC free article] [PubMed] [Google Scholar]