Abstract
Isolated abdominal aortic dissection (IAAD) is a rare form of aortic dissection involving usually the infrarenal part of the abdominal aorta. A 45-year-old male presented with lumbar pain and claudication. Computed tomography angiography (CTA) revealed an infrarenal IAAD extending to the left external iliac artery (EIA), causing ≥90% narrowing of the lumen. An endovascular approach was decided, with deployment of an aortic stent-graft and two balloon expandable stents in both common iliac arteries (IAs), applying the kissing stents technique. Post-surgical course was uneventful; 12 month follow-up showed excellent vessel patency. Endovascular therapy seems to be a feasible treatment option with promising long-term follow-up results.
Keywords: isolated abdominal aortic dissection, kissing stents
Introduction
Isolated abdominal aortic dissection (IAAD) is a rare clinical entity, requiring a high index of clinical suspicion for an accurate and prompt diagnosis, due to its innocuous presentation and possible fatal complications.1) There is an assortment of radiologic modalities, used both for diagnosis and pre-operative planning, while initial treatment approach depends on patient’s clinical condition and the complexity of the dissection. This paper aims to inform clinicians of this medical condition, and provide insight regarding an endovascular treatment approach.
Case Report
A 45-year-old Caucasian male was referred to our vascular surgery department, after progressive pain in the lumbar region for the past three days, along with ‘rest pain’ of his left lower extremity. The onset of symptoms was reported to be after strenuous exercise four days ago. Patient had visited an orthopedist, who prescribed anti-inflammatory drugs regarding a possible musculoskeletal lumbar strain. Despite medication, the pain worsened, with progressive development of left thigh discomfort and claudication, leading to rest pain for the past 24 hours. His medical history was free, reporting no hypertension, chronic medication or previous surgery; still he reported tobacco abuse.
Physical examination revealed a cold, pale, lower left extremity with diminished femoral pulse. Dorsalis pedis and posterior tibial pulse was non-palpable with monophasic signal at Doppler scan. Ankle branchial index (ABI) of his extremity was 0.36. Abdominal examination was unremarkable with no palpable mass or tenderness. Blood pressure was 142/89 mmHg, heart rate 72 beats/min and body temperature was 36.8°C. Laboratory, biochemistry and urine exams were within normal limits.
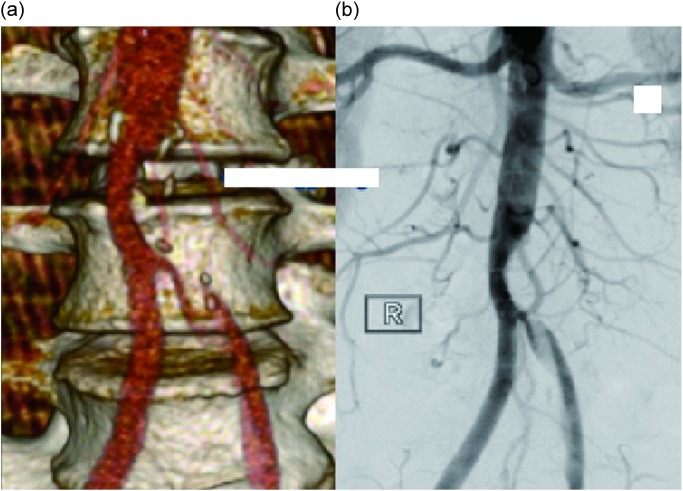
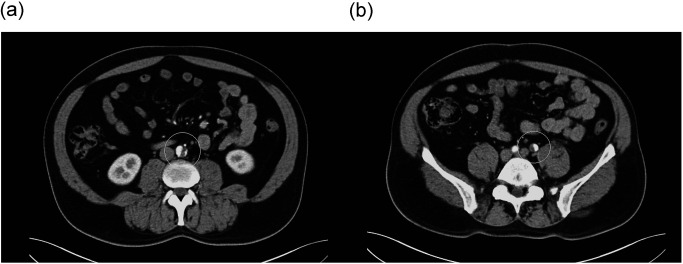
Patient was suspected of lower extremity occlusive disease, thus a digital subtraction angiography (DSA) was performed. Surprisingly, findings revealed an infrarenal stenosis of the abdominal aorta, progressing down to the left external iliac artery (EIA) (Fig. 1b). A Computed Tomography (CT) angiogram was further carried out, uncovering an isolated infrarenal aortic dissection, with its entry point commencing at the level of the inferior mesenteric artery (IMA). The dissection was extending up to the iliac bifurcation of the left common iliac artery (CIA) depicting no re-entry point. Its total length was 9.6 cm, causing an 80% stenosis of the aorta and a ≥90% stenosis of the left CIA. Maximum diameter of the thrombosed false lumen was 7 mm, located between IMA and aortoiliac bifurcation (Figs. 1a, 2a, and 2b).
Fig. 1 DSA (a) and 3D CTA (b) reconstruction of infrarenal IAAD, extending to the left CIA.
Fig. 2 Preoperative CTA showing infrarenal IAAD commencing at the level of the IMA and extending to the left CIA.
Patient started therapy on beta blockers, vasodilators and anticoagulants. An endovascular treatment approach was decided, and after written consent, he was taken to the operating room.
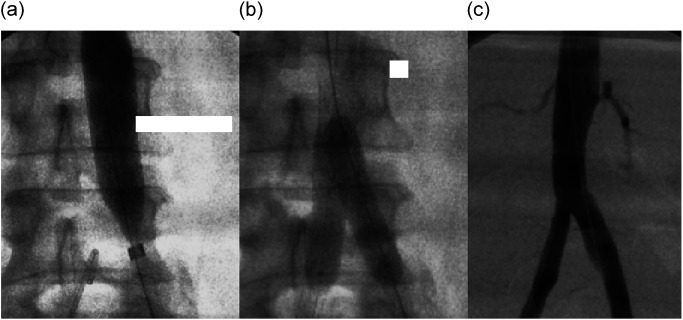
As patient’s preference, general anesthesia was implemented, during which percutaneous access of both common femoral arteries (CFAs) was achieved, with the introduction of an 11 Fr sheath on the left, and an 8 Fr sheath on the right CFA. After an angiogram through a pigtail catheter from the right site, predilatation of the left CIA was performed. A 16×41 mm PTFE balloon expandable stent-graft (Advanta V12, Atrium Europe, Mijdrecht, the Netherlands) was advanced and deployed in the aorta through the left CFA, in order to seal off the entry point. After full deployment of the stent-graft, two 10×40 mm balloon expandable cobalt chromium stents (Litus Xi Stent, Tsunamed, Winsen, Germany) were introduced in both CIAs with their proximal end extending inside the aortic stent graft. They were successfully deployed with the application of the kissing stents technique, in order to avoid a future re-stenosis of the left CIA. Final intraoperative angiography showed complete exclusion of the dissection with excellent patency of the aorta and both CIAs (Figs. 3a–3c).
Fig. 3 Intraoperative angiography depicting (a) deployment of the aortic stent graft, (b) deployment of two iliac balloon expandable stents with the application of the kissing stents technique, (c) final angiography showing excellent patency of all involved vessels.
Post-surgical recovery of the patient was uneventful with no further lumbar pain or claudication. He was discharged on the 2nd postoperative day, receiving antiplatelet medication daily (clopidogrel 75 mg). At 6th and 12th month follow-up, patient was symptom free, with color duplex scan showing excellent vessel patency with no re-stenosis of the left CIA.
Discussion
Aortic dissection is described as a tear in the intimal layer of the aorta, which allows blood flow between intima and media layer. A false lumen is created, thus forming a dual lumen aorta. It is a medical emergency requiring urgent therapy due to its possible fatal complications (heart failure, organ malperfusion, aortic rupture). Aortic dissection shows a preference in patients above the age of 60, with a men to women ratio of 4 : 1.1) Patients’ main complaint is usually sudden onset of pain (up to 90% of cases), the location of which depends on the level of the dissection.1) Hypertension is identified as a major predisposing factor for the appearance of aortic dissection, presenting in up to 70% of patients, while pregnancy, trauma, biscupid valve and Marfan’s syndrome are also associated with its development.1,2)
IAAD comprises a subgroup of aortic dissections. It is defined as the acute dissection of the abdominal aorta, with the patient seeking medical assistance in less than 2 weeks from symptoms onset. It is a fairly rare medical condition, accounting for less than 1.5% of all acute aortic dissections.1) Etiology can be spontaneous, iatrogenic or traumatic.3) Presentation can be ambiguous, with sharp abdominal or lumbar pain in 80% of cases.1,2) Pain is characterized as a ‘tear,’ moving downwards as the dissection of the abdominal aorta further progresses. IAAD usually commences below the level of the renal arteries, thus renal function remains unaffected. Lower extremity involvement is reported in up to 33% of cases, while it is also highly associated with the synchronous presence of abdominal aortic aneurysm.1,4,5)
Color duplex scan and CT angiography play a major role in identification and management of this medical condition. Ultrasonography of the abdomen can reveal the intimal flap in case of an IAAD, with a sensitivity and specificity of up to 80% and 100% respectively.6) CT angiography is excellent for assessment and preoperative management of IAADs. It can identify the location of the intimal tear, extension of the dissection, and branch vessel involvement. Other imaging modalities include angiography, which provides insight in evaluation of limb perfusion.7)
Therapeutic management and decision making regarding IAADs has seen much controversy, due to the small number of cases and the different approaches on each center. Therapy for IAADs can be either medical, open surgery, or endovascular. Medical therapy along with surveillance is recommended as initial therapy, in asymptomatic patients or non-complicated dissections.1) Indications for surgical therapy include the synchronous presence of abdominal aneurysm, critical limb ischemia, refractory pain, renal function compromise and hypertension resistant to medical therapy.1,2,5) Patient’s comorbidities also affect decision making regarding an open surgery or endovascular approach.
In our case, the relatively young age of our patient ruled out aortic wall degeneration as a cause for the dissection. There was no medical or family history associated with connective tissue disorder. In fact our patient was a very physically fit athlete despite his age, describing onset of pain during excessive lumbar training.
Critical limb ischemia pointed us towards surgery, despite the initial medical therapy. Our patient was strongly against open surgery, and after preoperative planning using CT angiography, an endovascular approach was decided. There are various reports for endovascular repair of IAAD, with a 14 patient series published by Kouvelos et al., being the longest cohort of patients treated for IAAD using endovascular means.2,8–10) The role of endovascular therapy is to seal off the entry point of the dissection, using a stent-graft or endograft, and cause thrombosis of the false lumen. The small diameter of the aorta and common iliac arteries found in our patient limited our endovascular options, since the introduction of a bifurcated endograft in an aortic bifurcation of a diameter less than 21 mm can lead to graft limb occlusion.9) This left us with the decision of deploying an aortic stent-graft inside the aortic lumen with the additional introduction of balloon expandable stents in both CIAs using the kissing stents technique.
In a meta-analysis performed by Jonker et al.10) including 92 patients, 65 of them were treated for abdominal aortic dissections with either open surgery or endovascular therapy. His results demonstrated lower mortality and complication rates for the endovascular therapy (0% and 5% respectively) group compared to open surgery (2% and 13% respectively), rendering endovascular management of abdominal aortic dissections a safe and durable approach.
Conclusion
In conclusion, IAAD is a rare form of aortic dissection, for which clinicians must be highly suspicious in patients presenting with sudden onset abdominal or lumbar pain. Lower extremity involvement and a medical history of hypertension further raise suspicion. Initial medical therapy includes beta blockers, vasodilators and anticoagulants, while complicated dissections require either open surgical or endovascular management, depending on patient’s clinical condition and surgical experience.
Disclosure Statement
All authors declare that they have no conflict of interest.
Author Contributions
Writing: GS, GV
Data collection: GS, GV, KM, GP
Study conception: GS, GV
Supervision of the manuscript preparation process: GV, VT
Data analysis: all authors
Review and approval of the final version of the submitted manuscript: all authors
References
- 1).Trimarchi S, Tsai T, Eagle KA, et al.; International Registry of Acute Aortic Dissection (IRAD) investigators. Acute abdominal aortic dissection: insight from the International Registry of Acute Aortic Dissection (IRAD). J Vasc Surg 2007; 46: 913-9.e1. [DOI] [PubMed] [Google Scholar]
- 2).Kouvelos GN, Vourliotakis G, Arnaoutoglou E, et al. Endovascular treatment for isolated acute abdominal aortic dissection. J Vasc Surg 2013; 58: 1505-11. [DOI] [PubMed] [Google Scholar]
- 3).DeBakey ME, McCollum CH, Crawford ES, et al. Dissection and dissecting aneurysms of the aorta: twenty year follow-up of five hundred twenty seven patients treated surgically. Surgery 1982; 92: 1118-34. [PubMed] [Google Scholar]
- 4).Borioni R, Garofalo M, De Paulis R, et al. Abdominal aortic dissections: anatomic and clinical features and therapeutic options. Tex Heart Inst J 2005; 32: 70-3. [PMC free article] [PubMed] [Google Scholar]
- 5).Kalko Y, Kafa U, Basaran M, et al. Surgical experiences in acute spontaneous dissection of the infrarenal abdominal aorta. Anadolu Kadiyol Derg 2008; 8: 286-90. [PubMed] [Google Scholar]
- 6).Fojtik JP, Costantino TG, Dean AJ. The diagnosis of aortic dissection by emergency medicine ultrasound. J Emerg Med 2007; 32: 191-6. [DOI] [PubMed] [Google Scholar]
- 7).Mantelas M, Antonitsis P, Kaitzis D, et al. Spontaneous isolated dissection of the abdominal aorta: single-center experience. Interact Cardiovasc Thorac Surg 2009; 8: 398-401. [DOI] [PubMed] [Google Scholar]
- 8).Porcellini M, Mainenti P, Bracale U. Endograft repair of spontaneous infrarenal abdominal aortic dissection. J Vasc Surg 2005; 41: 155. [DOI] [PubMed] [Google Scholar]
- 9).Adam DJ, Roy-Choudhury S, Bradbury AW. Endovascular repair of spontaneous infrarenal aortic dissection presenting as severe lower extremity ischaemia. Eur J Vasc Endovasc Surg 2007; 34: 699-701. [DOI] [PubMed] [Google Scholar]
- 10).Jonker FH, Schlosser FJ, Moll FL, et al. Dissection of the abdominal aorta. Current evidence and implications for treatment strategies: a review and meta-analysis of 92 patients. J Endovasc Ther 2009; 16: 71-80. [DOI] [PubMed] [Google Scholar]