Abstract
Background
The response to therapeutics varies widely in patients with depression and anxiety, making selection of an optimal treatment choice challenging. IDgenetix®, a novel pharmacogenomic test, has been shown to improve outcomes by predicting the likelihood of response to different psychotherapeutic medications.
Objective
The objective of this study was to estimate the cost effectiveness of implementing a novel pharmacogenomic test (IDgenetix®) to guide treatment choices in patients with depression and/or anxiety compared with treatment as usual from the US societal perspective.
Methods
We developed a discrete event simulation to compare clinical events, quality-adjusted life-years, and costs of the two treatment strategies. Target patients had a Hamilton Rating Scale for Depression Score ≥ 20 and/or a Hamilton Rating Scale for Anxiety score ≥ 18 at baseline. Remission, response, and no response were simulated based on the observed rates in the IDgenetix® randomized controlled trial. Quality-adjusted life-years and direct and indirect costs attributable to depression and anxiety were estimated and compared over a 3-year time horizon. We conducted extensive deterministic and probabilistic sensitivity analyses to assess the robustness of the results.
Results
The model predicted cumulative remission rates of 78 and 66% in IDgenetix® and treatment as usual groups, respectively. Estimated discounted quality-adjusted life-years were 2.09 and 1.94 per patient for IDgenetix® and treatment as usual, respectively, which resulted in 0.15 incremental quality-adjusted life-years (95% credible interval 0.04–0.28). The total costs after accounting for a US$2000 test cost were US$14,124 for IDgenetix® compared with US$14,659 for treatment as usual, suggesting a US$535 (95% credible interval − 2902 to 1692) cost saving per patient in the IDgenetix® group. Incremental quality-adjusted life-year gain (0.49) and cost savings (US$6800) were substantially larger in patients with severe depression (Hamilton Rating Scale for Depression score ≥ 25).
Conclusion
Using the IDgenetix® test to guide the treatment of patients with depression and anxiety may be a dominant strategy, as it improves quality-adjusted life-years and decreases overall costs over a 3-year time horizon.
Electronic supplementary material
The online version of this article (10.1007/s40273-017-0587-0) contains supplementary material, which is available to authorized users.
Key Points
| The response to therapeutics varies widely in patients with depression and anxiety and there is a great need for personalized approaches to guide the choice of treatments. |
| In a randomized trial, IDgenetix®-guided treatment resulted in higher rates of response and remission compared with treatment as usual in patients with moderate and severe depression and/or anxiety, but the economic value of the test is unknown. |
| Our cost-effectiveness analysis suggested that using the IDgenetix® test to guide the treatment of patients with moderate-to-severe depression and/or anxiety may improve quality-adjusted life-years and decrease overall costs over a 3-year time horizon. |
Background
Pharmacotherapy is the cornerstone of treatment of patients with moderate-to-severe depression and anxiety [1–3]. Efficacy and toxicity of pharmacotherapy, however, vary widely across patients. The results of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study demonstrated that only one third of patients achieved remission after receiving the initial treatment level [4, 5]. Patients often need to undergo an odyssey of treatments that may last months or years to find the medication that results in adequate response or remission. This trial-and-error approach is associated with continued debilitating symptoms for patients, increased health resource utilization, and reduced functionality and work productivity. The likelihood of remission also decreases when patients do not respond and are required to receive higher treatment levels for extended periods [5]. As such, there is a great need for precision approaches that can be used to guide the choice of initial treatment options for individual patients.
Recent genome-wide association studies have suggested that a substantial proportion of heterogeneity in treatment outcomes can be explained by genetic variations across patients [6]. Several pharmacogenomic tests have been recently developed to guide the choice of pharmacotherapy medications [7, 8]. Until now, evidence on the efficacy of these pharmacogenomic-guided treatments was generally limited to the data from a few small randomized controlled trials (RCTs) [9, 10] or observational studies [11]. A recent double-blinded (patients, raters) RCT was the first large RCT to compare the efficacy of pharmacogenomic-guided treatment (IDgenetix® test) with treatment as usual (TAU) in patients with depression and/or anxiety. The RCT enrolled a total of 685 subjects with mild, moderate, or severe depression and/or anxiety. As per the trial protocol, the efficacy analysis was conducted on subjects with a disease severity of moderate or severe (n = 485) [12]. The IDgenetix® test uses a genetic variant panel of ten genes to provide information about gene–drug and drug–drug interactions for over 40 medications typically used in the treatment of depression and anxiety. The IDgenetix® RCT was conducted in 20 clinical sites across USA specializing in psychiatry, internal medicine, family medicine, neurology, and obstetrics and gynecology. The trial found statistically significant improvements in response rates and large increases in remission rates in patients with a baseline Hamilton Rating Scale for Depression (HAM-D) score ≥ 20 and/or a baseline Hamilton Rating Scale for Anxiety (HAM-A) score ≥ 18 who received IDgenetix®-guided treatment.
In this study, we aimed to assess the cost effectiveness of using IDgenetix®-guided treatment compared with TAU in patients with moderate or severe depression and/or anxiety, based on the results of the published RCT and other published observational studies. The secondary aim of this study was to evaluate the cost-effectiveness results in different patient subgroups and under different assumptions about model parameters.
Methods
Simulation Model
We developed a discrete-event simulation model using Arena Version 15.00 (2016 Rockwell Automation Technologies, Inc., Milwaukee, WI, USA) to simulate clinical outcomes, resource utilization, and the cost of two alternative strategies for the treatment of patients with depression and/or anxiety (Fig. 1). For this purpose, we created a hypothetical cohort of 10,000 individuals with baseline characteristics (age, sex, baseline HAM score, diagnosis of depression with/without anxiety or anxiety only) that mimicked the actual distribution of patients included in the final evaluation of outcomes in the IDgenetix® RCT (Table 1). Individual patients were treated for their depression and/or anxiety and were then tracked every 3 months over the model time horizon. Health trajectories in the model were defined based on the possible treatment outcomes, including likelihood of remission, response, and no response. We assumed that patients who responded to treatment or achieved remission could relapse, requiring a new round of treatment. We also modeled suicide attempts among patients who did not achieve remission and the proportion of successful suicides. All patients were assumed to be exposed to the risk of adverse drug events (ADEs) when on treatment. Patients exited the simulation if the end of the model time horizon was reached or if they died because of suicide or background mortality. As patients experienced different health states in the model, their quality-adjusted life years (QALYs) and costs were calculated and recorded. Incremental effectiveness and incremental cost were estimated by calculating the difference in QALYs gained and total costs accrued between the two treatment strategies. The analysis was performed from the US societal perspective.
Fig. 1.
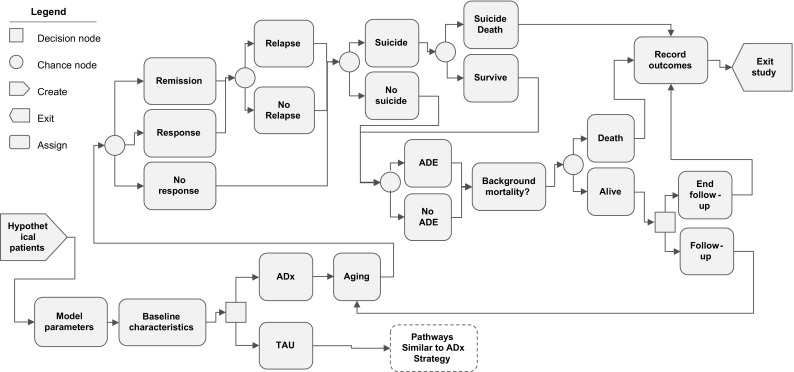
Model structure of one of the treatment arms (IDgenetix®-guided treatment). The treatment as usual (TAU) arm has the identical structure but with different values for model parameters. The model assigns baseline characteristics (age, sex, Hamilton Rating Scale for Depression score, Hamilton Rating Scale for Anxiety score, initial diagnosis, treatment level) to a hypothetical cohort of patients with depression and/or anxiety. Patients are assigned to a treatment strategy and follow different health trajectories depending on their treatment outcome (remission, response, non-response), incidence of suicide, adverse drug event (ADE), background mortality, and relapse. These probabilities are a function of patient characteristics and/or treatment at a given time. If a patient survives in each treatment period, the quality-adjusted life-year and total cost accrued in that year will be recorded and patient age, Hamilton Rating Scale score, history of remission or response, and other characteristics will be updated for the next simulation cycle. All patients are followed over 3 years in the base-case analysis. ADx IDgenetix® pharmacogenomic test
Table 1.
Model input parameters and assumptions
| IDgenetix®-guided treatment | TAU | Distribution used to model uncertainty | Data source | |
|---|---|---|---|---|
| Cohort characteristics | ||||
| Age, years, mean (SD) | 48 (14.5) | 48 (14.5) | Normal (48, 14.5) | Bradley et al. [32] |
| Male sex (%) | 27 | 27 | Binomial (0.27) | Bradley et al. [32] |
| Patients with depression with or without anxiety (%) | 65 | 65 | Binomial (0.65) | Bradley et al. [32] |
| Proportion with 20 ≤ HAM-D < 25 | 64 | 64 | Binomial (0.64) | Bradley et al. [32] |
| Proportion with HAM-D ≥ 25 | 36 | 36 | Binomial (0.36) | Bradley et al. [32] |
| Patients with anxiety only (%) | 45 | 45 | Binomial (0.45) | Bradley et al. [32] |
| Proportion with 18 ≤ HAM-A < 25 | 55 | 55 | Binomial (0.55) | Bradley et al. [32] |
| Proportion with HAM-A ≥ 25 | 45 | 45 | Binomial (0.45) | Bradley et al. [32] |
| Efficacy | ||||
| Remission rate in patients with depression with or without anxiety at week 12 (mean %, 95% CIa) | Bradley et al. [32] | |||
| 20 ≤ HAM-D < 25 | 41 (33–49) | 43 (34–53) | Beta (62, 89); Beta (46, 61) | |
| HAM-D ≥ 25 | 35 (21–52) | 13 (5–25) | Beta (13, 24); Beta (6, 38) | |
| Remission rate in patients with anxiety only (at week 12) | Bradley et al. [32] | |||
| 18 ≤ HAM-A < 25 | 44 (33–55) | 36 (26–47) | Beta (35, 45); Beta (30, 53) | |
| HAM-A ≥ 25 | 27 (17–40) | 25 (14–37) | Beta (16, 43); Beta (14, 42) | |
| Response rate in patients with depression with or without anxiety (at week 12)a | Bradley et al. [32] | |||
| 20 ≤ HAM-D < 25 | 57 (48–65) | 57 (47–66) | Beta (77, 58); Beta (61, 46) | |
| HAM-D ≥ 25 | 73 (56–85) | 36 (23–50) | Beta (27, 10); Beta (18, 32) | |
| Response rate in patients with anxiety only (at week 12) | Bradley et al. [32] | |||
| 18 ≤ HAM-A < 25 | 63 (51–73) | 52 (41–62) | Beta (37, 22); Beta (47, 43) | |
| HAM-A ≥ 25 | 63 (50–75) | 51 (38–64) | Beta (48, 28); Beta (30, 28) | |
| Decline in remission rate (relative risk) by treatment levelb | Rush et al. [5] | |||
| Level 1 | 1 | |||
| Level 2 | 0.83 | |||
| Level 3 | 0.37 | |||
| Level 4 | 0.35 | |||
| Decline in response rate (relative risk) by treatment level | ||||
| Level 1 | 1 | |||
| Level 2 | 0.59 | |||
| Level 3 | 0.34 | |||
| Level 4 | 0.34 | |||
| ADEs | Rush et al. [5] | |||
| ADE rate in patients with depression with or without anxiety (at week 12) | 599 out of 3671 (16.3%) | Beta (599. 3072) | ||
| ADE rate in patients with anxiety only (at week 12) | 599 out of 3671 (16.3%) | Beta (599, 3072) | ||
| Increase in ADE rate (relative risk) by treatment level | ||||
| Level 1 | 1 | |||
| Level 2 | 1.20 | |||
| Level 3 | 1.57 | |||
| Level 4 | 1.84 | |||
| Suicide rates in patients with depression and anxiety | Simon et al. [18] | |||
| Suicide attempt rate among patients with depression (%, within 6 months)c | ||||
| <18 years of age | 0.314 | |||
| 18–30 years of age | 0.145 | |||
| 31–50 years of age | 0.780 | |||
| >50 years of age | 0.045 | |||
| Proportion of suicides that are successful (%) | 43 | Beta (40, 53) | ||
| Relative risk of suicide attempt among those who respond to treatment | 0.49 | Beta (67, 70) | Olin et al. [19] | |
| Relapse rates | ||||
| Relapse rates among patients with remission depending on latest treatment level (%, within 3 months) | Rush et al. [5] | |||
| Level 1 | 33.5 | |||
| Level 2 | 47.4 | |||
| Level 3 | 42.9 | |||
| Level 4 | 50.0 | |||
| Relapse rates among patients with response depending on latest treatment level (%, within 3 months) | Rush et al. [5] | |||
| Level 1 | 58.6 | |||
| Level 2 | 68.0 | |||
| Level 3 | 76.0 | |||
| Level 4 | 83.3 | |||
| Decline in relapse rates by duration of remission | 1/Exp(7 × time on remission) | Assumption (calibration parameter) | ||
| Utilities and costs (mean, SD) | ||||
| Baseline QOL weights (EQ-5D)d | Age dependent | Sullivan et al. [21] | ||
| QOL weights for remission | 0.826 (0.065) | Normal (0.826, 0.065) | Mrazek et al. [22] | |
| QOL weight for response | 0.673 (0.031) | Normal (0.673, 0.031) | Mrazek et al. [22] | |
| QOL weight for no response | 0.417 (0.126) | Normal (0.417, 0.126) | Mrazek et al. [22] | |
| ADE impact on QOL | − 0.055 (0.028) | Normal (− 0.055, 0.028) | Mrazek et al. [22] | |
| IDgenetix® test cost (US$) | 2000 | Assumption | ||
| Direct costs attributable to depression and anxiety, per patient per yeare (US$) | 6407 (1600) | Normal (6407, 1600) | Greenberg et al. [23] | |
| Indirect costs attributable to depression and anxiety, per patient per yearf (US$) | 2922 (730) | Normal (2922, 730) | Greenberg et al. [23] | |
| Discount rate (%) | 3 (0–5) | Assumption | ||
ADEs adverse drug events, CI confidence interval, HAM-A Hamilton Rating Scale for Anxiety, HAM-D 17-item Hamilton Rating Scale for Depression, IDgenetix ® AltheaDx IDgenetix® test, SD standard deviation, QOL quality of life, STAR*D Sequenced Treatment Alternatives to Relieve Depression, TAU treatment as usual
aResponse defined as a ≥ 50% reduction in HAM scores. Remission defined as HAM scores ≤ 7
bFour treatment levels were defined per STAR*D trial
c93 serious suicide attempts per 100,000 patients, of which 40 were successful
dEstimated using the age-specific EQ-5D values reported by Sullivan et al. [21]
eUnit costs were inflated to 2017 US$ using the changes in the consumer price index between 2012 and 2017
fIndirect costs only include costs of disability and absenteeism. Cost of presenteeism has been excluded
Patient Characteristics
Most model parameters including remission, response, relapse, ADEs, suicide, and background mortality were a function of individual patient characteristics such as baseline HAM score, diagnosis (depression and/or anxiety), treatment level, age, and sex. Therefore, patient characteristics directly influenced the individual and overall clinical and cost outcomes in our simulation. The target population in our analysis was similar to the RCT population and consisted of patients with moderate or severe depression (HAM-D ≥ 20) and/or anxiety (HAM-A ≥ 18). Patients with HAM-D ≥ 25 and/or HAM-A ≥ 25 scores were considered severe cases. The mean age of the cohort was 48 years (standard deviation = 14.5) and 27% were male. Baseline characteristics of the simulated cohorts in both treatment strategies were assumed to be identical to control for variability in outcomes caused by differences in patient populations (Table 1). We assumed that all patients received treatment level 1, as defined in the STAR*D study, at model entry. In the STAR*D study, treatment level 1 was defined as patients receiving citalopram or an equivalent medication. Treatment escalated to higher levels (levels 2–4) for non-responders and included options such as bupropion, cognitive therapy, sertraline, extended-release venlafaxine, tranylcypromine, or extended-release venlafaxine plus mirtazapine [5].
Analytical Perspective and Time Horizon
We assumed a 3-year time horizon for the base-case analysis. The results assuming shorter and longer time horizons (12 weeks, 1, 2, 10 years, and lifetime) were also provided to supplement the findings of the base-case analysis. The analysis was done from the US societal perspective, accounting for direct and indirect costs as a result of disability and absenteeism. Both costs and QALYs were discounted at a 3% per year rate in accordance with US Public Health Service guidelines for cost-effectiveness analyses [12] and sensitivity analyses were conducted with 0% and 5% discount rates. Incremental cost-effectiveness ratios (ICERs) were estimated by dividing incremental costs by incremental QALYs. We also calculated the net monetary benefit (NMB) assuming a US$50,000 per QALY threshold for willingness to pay (WTP) [12, 13]. The NMB () estimates the monetary value of additional benefit of a treatment after subtracting additional costs [14]; therefore, resulting in a positive value if the strategy is cost effective at a given WTP threshold.
Treatment Strategies
We considered two alternative strategies for the treatment of patients with depression and/or anxiety: (1) using IDgenetix® test results to individualize pharmacotherapy based on information about drug–drug and drug–gene interactions; and (2) TAU, where physicians use their best judgment to select treatment by considering patient characteristics and clinical history using a trial-and-error process. The IDgenetix® test is a one-time test that can be performed prior to or at the initial visit. The IDgenetix® report provides the likelihood of response to approximately 40 medications given a patient’s genomic profile, potential interactions with concurrent medications that a patient may use, and environmental/lifestyle factors that may contribute to patient response (i.e., smoking). The test results provide charts indicating which medications should be used as directed and which medications should be used with caution or increased monitoring. Physicians can then use this information to choose medications that are more likely to be a safe and effective option for the patient. We assumed that the information provided by the initial IDgenetix® test could be used to inform subsequent treatment decisions at no additional cost over a patient’s lifetime.
Data on Clinical Utility of the Test and Disease Progression
We used the overall clinical utility of IDgenetix®-guided treatment compared with TAU as reported in the IDgenetix® RCT (12) to model clinical outcomes and costs under two strategies. We assumed that the overall clinical utility measured in terms of remission and response rates has captured the impact of all test-related factors including analytical validity, clinical validity, and test turnaround time. Remission was defined as a HAM-D or HAM-A score of 7 or less and response was defined as a 50% decline in HAM-D or HAM-A scores. We used the remission and response rates for each diagnosis and disease severity to inform our model inputs. We assumed that remission and response rates are functions of individual-level covariates (Table 1) including baseline disease severity (defined based on HAM-D and HAM-A scores), primary diagnosis (depression and/or anxiety), and latest antidepressant treatment level per STAR*D definitions [5]. Patients were assumed to stop receiving treatment if they achieved remission and remained in that state for two consecutive periods (i.e., 6 months) [15, 16]; otherwise, treatment escalated to the next level and continued over the next period. We also assumed that the likelihood of remission and response declined and the likelihood of ADEs increased at higher treatment levels, as observed in the STAR*D study (Table 1).
We used the observed rates in the STAR*D study to model the rate of relapse in patients who responded to treatment or achieved remission in either treatment strategy (Table 1). In line with the STAR*D study [5], we assumed that the relapse rates were higher in patients who only responded to treatment (i.e., did not achieve remission) and in those who required higher treatment levels (Table 1). Furthermore, we assumed that relapse rates declined exponentially the longer a patient stayed in remission. This was a calibration parameter in the model to ensure that the cumulative number of depression and/or anxiety episodes over a patient’s lifetime in our simulation matched the observed frequencies based on empirical studies [17].
We used age-dependent rates of suicide attempts and suicide success rates as reported by Simon et al. [18] to model rates of suicide among patients who did not respond to treatment. We assumed that the relative risk of suicide attempts decreased by 0.49 if the patient responded to treatment [19] and assigned a rate of zero for those who achieved remission (Table 1).
Background mortality rates stratified by sex were derived from the US life tables published as part of the National Vital Statistics Reports [20]. Exponential functions were fitted to each population stratum and the resulting values were incorporated into our model to predict the probability of background mortality for each patient at different time points of the simulation. We used a test cost of US$2000 for the base-case analysis and varied this value in the sensitivity analyses to assess the impact of the test cost on the cost-effectiveness results.
Quality-of-Life Weights
We assumed that the quality of life (QOL) for a patient in the remission state was identical to that of the general population for that specific age category [21]. Quality of life for other health states, including response and no response, were obtained from Mrazek et al. [22]. As patients moved through different health states in the simulation, QALYs were calculated by multiplying the health-related QOL weight of each health state with the time spent in that health state. We assumed that the occurrence of an ADE negatively affected a patient’s QOL [22] and we therefore penalized the QOL over that treatment period. The QOL in patients with attempted suicides dropped to zero for one treatment period (3 months) and then bounced back to its value prior to the suicide event. We assigned a zero QOL to patients who died because of suicide or background mortality.
Costs
We used the total per-patient economic burden of major depressive disorder (MDD) published by Greenberg et al. in 2015 [23], as it provides a comprehensive overall cost of depression and details the breakdown of factors included in each cost category. The total economic burden of an individual with MDD according to Greenberg et al. is the sum of the direct healthcare costs associated with MDD (such as costs of medical services and prescriptions), the costs associated with depression other than MDD (costs of non-depression mental health), the costs of non-mental health medical services and prescription, and the costs of missed productivity (absenteeism and disability). Data were collected from a private insurance database with 16 million beneficiaries from 69 large self-insured US companies. Patients with a minimum of two International Classification of Diseases, Ninth Revision claims for MDD and with continuous healthcare eligibility, and propensity-matched controls without MDD were compared in the analysis.
We estimated direct and indirect costs attributable to depression and anxiety as simulated patients moved throughout the model’s different pathways. We assumed that patients taking treatment for depression and/or anxiety accrued costs. Patients that maintained remission for two consecutive periods (i.e., 6 months) were not assigned additional costs. Direct and indirect costs attributable to depression and anxiety were based on the differences between estimated values for patients with MDD and the control group as reported by Greenberg et al. [23]. Patients aged 65 years or younger accrued indirect costs related to disability and absenteeism; for older patients, the absenteeism component was dropped and they only accrued indirect costs owing to disability. We also excluded indirect costs as a result of presenteeism and suicide to ensure conservative estimates for the benefits of IDgenetix®. All 2015 unit cost estimates from Greenberg et al. were converted to 2017 values using changes in the consumer price index [24]. A one-time test cost was applied to the patients who were assigned to the IDgenetix® strategy.
Deterministic and Probabilistic Sensitivity Analysis
To examine the impact of each input parameter on the results, we changed each parameter one at a time across their possible ranges and examined the impact on the ICER and NMB. To assess the uncertainty in the estimated base-case results caused by uncertainty in the input parameters, we conducted probabilistic sensitivity analyses [25]. For this purpose, we sampled 1000 independent sets of input parameters from their probability distributions (Table 1) and modeled a cohort of 1000 hypothetical patients per treatment strategy using a Monte Carlo simulation [26, 27]. The results of these probabilistic sensitivity analyses are reported using incremental cost-effectiveness planes and incremental cost-effectiveness acceptability curves.
Model Validation
We first ran the model for one treatment period (3 months) and compared the remission rates and response rates with the observed rates in the IDgenetix® RCT. As expected, remission and response rates in the simulation were almost identical to those in the RCT. Next, we compared the simulated cumulative remission rate in the TAU arm at year 3 (66%) with empirical rates reported in the STAR*D prospective study (67% after trying all treatment levels) [5]. Finally, we ran the model over a patient’s lifetime and compared the simulated distribution of the number of depressive episodes in the TAU group with corresponding empirical rates reported by Marcotte et al. [17] [Table 1 of the Electronic Supplementary Material (ESM)]. The distributions of simulated episodes were comparable to corresponding observed distributions in our final model. This validated the disease progression and relapse rates over a patient’s lifetime in our model.
Results
Base-Case Analysis
The mean baseline age in the simulated cohorts was 48 years and 27% were male. Approximately 65% of patients had depression with/without anxiety and 35% had anxiety only. At the end of the simulation, the mean treatment level was 2.3 [95% credible interval (CrI) 1–4] for the IDgenetix® group and 2.7 (95% CrI 1– 4) for the TAU group. By the end of year 3, the mean HAM-D score was 7.9 (0.7–28.4) for the IDgenetix® group and 9.8 (0.7–31.2) for the TAU group. Similarly, the HAM-A score was 8.4 (0.8–33.1) for the IDgenetix® group and 10.6 (0.8–34.9) for the TAU group. Remission was achieved in 78% (73–82) of patients in the IDgenetix® group compared with 66% (60–72) of patients in the TAU group. Suicide attempts (0.13 vs. 0.18%) and suicide death (0.06 vs. 0.08%) were also lower in the IDgenetix® group compared with the TAU group.
Estimated discounted QALYs were 2.09 (95% CrI 1.88–2.28) and 1.94 (95% CrI 1.66–2.21) in the IDgenetix® and TAU groups, respectively, resulting in an incremental QALY of 0.15 (0.04–0.28) (Table 2). The total cost per IDgenetix® patient was US$14,124 (95% CrI 10,703–17,630) compared with US$14,659 (95% CrI 10,384–19,275) per TAU patient, leading to an incremental cost of − US$535 (95% CrI − 2902 to − 1692) per patient (Table 2). These estimates suggest that IDgenetix® is a dominant treatment strategy as it results in a positive QALY gained and more than US$530 cost savings per patient over a 3-year time horizon, after accounting for the test cost.
Table 2.
Base-case results, 3-year time horizon
| IDgenetix®-guided treatment | TAU | |
|---|---|---|
| Clinical outcomes (mean, 95% CrI)a | ||
| Last treatment level | 2.3 (1–4) | 2.7 (1–4) |
| Number of relapses per patient | 0.97 (0–4) | 0.82 (0–4) |
| HAM-D score at the end of simulation | 7.9 (0.7–28.4) | 9.8 (0.7–31.2) |
| HAM-A score at the end of simulation | 8.4 (0.8–33.1) | 10.6 (0.8–34.9) |
| Patients achieved remission (%) | 78 (73–82) | 66 (60–72) |
| Suicides (%) | 0.13 (0.00–0.40) | 0.18 (0.00–0.50) |
| Suicide death (%) | 0.06 (0.00–0.20) | 0.08 (0.00–0.30) |
| QALYs and costs (mean, 95% CrI) | ||
| QALYs gained per patient | 2.09 (1.88–2.28) | 1.94 (1.66–2.21) |
| Direct costs (US$) | 10,530 (7487–13,600) | 10,323 (6568–14,433) |
| Total cost per patient (US$) | 14,124 (10,703–17,630) | 14,659 (10,384–19,275) |
| Incremental QALYs | 0.15 (0.04–0.28) | Reference |
| Incremental direct costs (US$) | 207 (− 1671 to 2022) | Reference |
| Incremental total costs (US$) | − 535 (− 2902 to 1692) | Reference |
| Incremental cost-effectiveness ratio (US$ per QALY) based on incremental direct costs | 1394 | Reference |
| Incremental cost-effectiveness ratio (US$ per QALY) based on incremental total costs | Dominant (cost saving) | Reference |
| Net monetary benefit (US$, assuming a WTP threshold of US$50,000 per QALY) | 7955 (793–16,098) | Reference |
CrI credible interval, HAM-A Hamilton Rating Scale for Anxiety, HAM-D Hamilton Rating Scale for Depression, QALYs quality-adjusted life-years, TAU treatment as usual, WTP willingness to pay
a95% Crl reflects the results of a probabilistic sensitivity analysis using a Monte Carlo simulation
Our subgroup analysis showed that patients with depression with or without comorbid anxiety had a slightly larger QALY gain (0.17 vs. 0.12) and cost savings (− US$972 vs. US$4) compared with patients with anxiety only (Table 3). Furthermore, the subgroup analysis suggested that QALY gain (0.49) and cost savings (− US$6871) were substantially larger in patients with severe depression with or without comorbid anxiety (HAM-D ≥ 25). This relationship was not seen with patients with severe anxiety only (Table 4).
Table 3.
Results for all patients diagnosed with depression with/without anxiety [Hamilton Rating Scale for Depression (HAM-D) score ≥ 20] and for all patients diagnosed with anxiety only [Hamilton Rating Scale for Anxiety (HAM-A) score ≥ 18], assuming a 3-year time horizon
| IDgenetix®-guided treatment | TAU | |
|---|---|---|
| Patients with depression with/without anxiety (anxiety only excluded) and HAM-D score ≥ 20 | ||
| Patients achieved remission (%) | 79 (77–82) | 65 (62–68) |
| QALYs gained per patient | 2.10 (2.07–2.13) | 1.93 (1.90–1.96) |
| Total cost per patient ($US) | 14,005 (13,387–14,570) | 14,977 (14,347–15,636) |
| Incremental QALYs | 0.17 | Reference |
| Incremental total costs (US$) | − 972 | Reference |
| Incremental cost-effectiveness ratio (US$ per QALY) based on incremental total costs | Dominant (cost saving) | Reference |
| Patients with anxiety only and HAM-A score ≥ 18 | ||
| Patients achieved remission (%) | 77 (74–80) | 68 (65–71) |
| QALYs gained per patient | 2.08 (2.05–2.11) | 1.96 (1.93–1.99) |
| Total cost per patient (US$) | 14,602 (13,978–15,210) | 14,579 (13,976–15,237) |
| Incremental QALYs | 0.12 | Reference |
| Incremental total costs (US$) | 4 | Reference |
| Incremental cost-effectiveness ratio (US$ per QALY) based on incremental total costs | 35 | Reference |
QALYs quality-adjusted life-years, TAU treatment as usual
Table 4.
Results for the subgroup of patients with severe depression and/or severe anxiety [Hamilton Rating Scale for Depression (HAM-D) score ≥ 25 and/or Hamilton Rating Scale for Anxiety (HAM-A) score ≥ 25], assuming a 3-year time horizon
| IDgenetix®-guided treatment | TAU | |
|---|---|---|
| Patients with severe depression with/without anxiety (anxiety only excluded, HAM-D score ≥ 25) | ||
| Patients achieved remission (%) | 82 (79–84) | 40 (37–43) |
| QALYs gained per patient | 2.15 (2.13–2.18) | 1.66 (1.63–1.69) |
| Total cost per patient (US$) | 13,591 (13,047–14,129) | 20,463 (19,913–21,019) |
| Incremental QALYs | 0.49 | Reference |
| Incremental total costs (US$) | − 6871 | Reference |
| Incremental cost-effectiveness ratio (US$ per QALY) based on incremental total costs | Dominant (cost saving) | Reference |
| Patients with severe anxiety only (HAM-A score ≥ 25) | ||
| Patients achieved remission (%) | 71 (69–74) | 63 (60–66) |
| QALYs gained per patient | 2.02 (1.99–2.05) | 1.91 (1.88–1.94) |
| Total cost per patient (US$) | 16,264 (15,599–16,874) | 15,875 (15,233–16,482) |
| Incremental QALYs | 0.11 | Reference |
| Incremental total costs (US$) | 389 | Reference |
| Incremental cost-effectiveness ratio (US$ per QALY) based on incremental total costs | 3396 | Reference |
| Patients with severe depression and/or anxiety (HAM-D score ≥ 25 and/or HAM-A score ≥ 25) | ||
| Patients achieved remission (%) | 78 (76–81) | 48 (45–51) |
| QALYs gained per patient | 2.11 (2.08–2.14) | 1.75 (1.71–1.78) |
| Total cost per patient (US$) | 14,522 (13,491–15,085) | 18,896 (18,282–19,516) |
| Incremental QALYs | 0.36 | Reference |
| Incremental total costs (US$) | − 4373 | Reference |
| Incremental cost-effectiveness ratio (US$ per QALY) based on incremental total costs | Dominant (cost saving) | Reference |
QALYs quality-adjusted life-years, TAU treatment as usual
Deterministic Sensitivity Analyses
Estimated ICERs and NMBs were sensitive to our assumptions about the efficacy of IDgenetix®-guided treatment (Figs. 3 and 4 of the ESM). We assumed 25% higher response rates would result in US$2300 cost savings while 25% lower response rates would result in a cost-effectiveness ratio of approximately US$17,000 per QALY. Additionally, a 25% increase or decrease in remission rates varied the cost-effectiveness estimates from US$2100 cost savings to US$12,000 per QALY. Direct and indirect costs of depression and anxiety and QOL weight for non-responders also had a moderate impact on the estimated outcomes. Our base-case results did not meaningfully change when we varied other input parameters of the model such as suicide rates or discount rate.
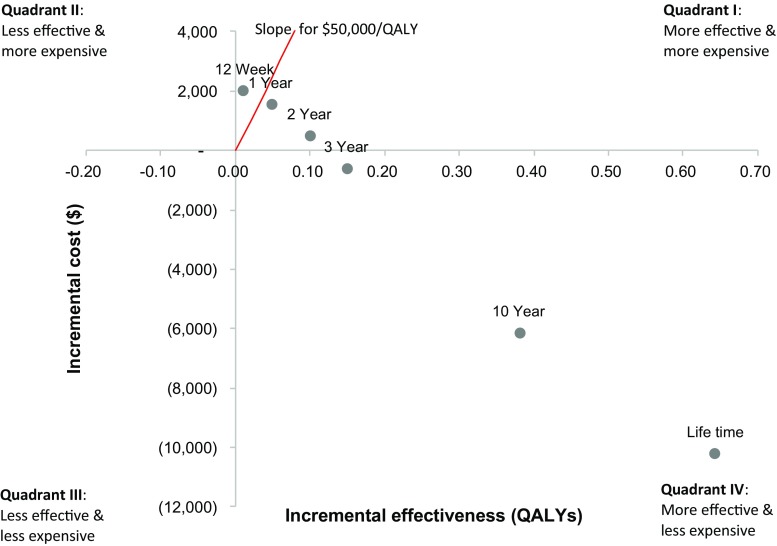
Extending the model time horizon had a substantial impact on the estimated outcomes. The estimated results suggested that the ICER dropped below US$50,000 per QALY for any time horizon that was longer than 1 year, indicating that the IDgenetix® strategy is cost effective by most measures. IDgenetix® becomes a cost-saving strategy when the model time horizon was set to 3 years or longer. Our model shows that using IDgenetix® would result in more than US$6000 cost savings over 10 years and more than US$10,000 cost savings over the lifetime of patients (Fig. 2).
Fig. 2.
Incremental cost-effectiveness results by model time horizon. QALYs quality-adjusted life-years
In a one-way sensitivity analysis, we assessed the impact of the test cost on the estimated ICERs (Fig. 1 of the ESM). The IDgenetix® became a cost-saving strategy when the test cost was US$2500 or less. The ICER remained below the commonly acceptable WTP threshold of US$50,000 per QALY when we varied the IDgenetix® test cost between US$2500 and US$3500. That is, even at a price of US$3500, the test would remain cost effective.
The value of the IDgenetix® test slightly varied based on patient age (Fig. 2 of the ESM). Everything else equal, younger patients were estimated to have a larger QALY gain and cost savings from using the IDgenetix® test, resulting in larger NMBs. Using IDgenetix® in patients aged 65 years or younger resulted in a 0.147 QALY gain and US$668 cost savings. In contrast, incremental QALY and incremental costs of using the IDgenetix® test in patients aged older than 65 years were 0.112 and US$113, respectively, resulting in an ICER of US$1003 per QALY gained. This suggests that IDgenetix® is still a cost-effective strategy in patients aged older than 65 years. The NMB remained positive for all age groups (Fig. 2 of the ESM). The impact of baseline age on NMB was larger when we used a lifetime model as compared with a 3-year model in the base-case analysis.
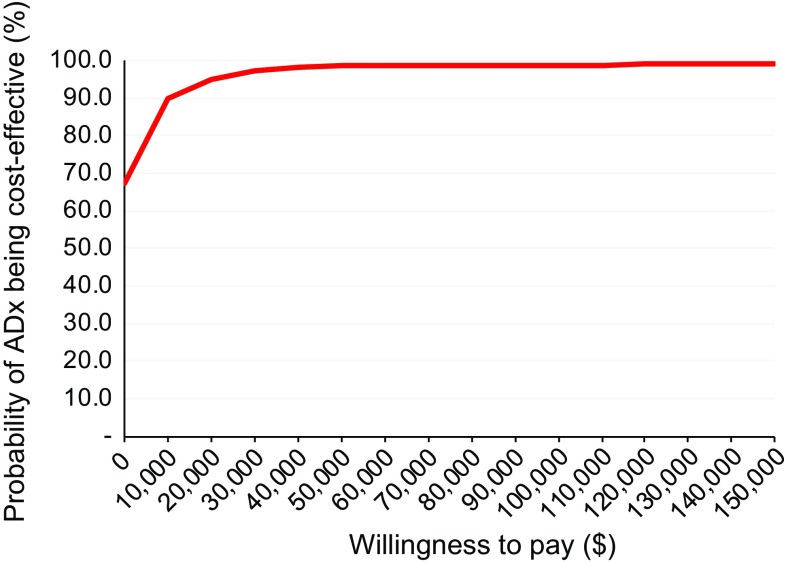
Probabilistic Sensitivity Analyses
The results of probabilistic analysis are presented in Fig. 3 using cost-effectiveness acceptability curves. Cost-effectiveness acceptability curves present the probability of IDgenetix® being the cost-effective strategy at different WTP thresholds. For example, cost-effectiveness acceptability curves suggest that the probability of IDgenetix® being the cost-effective strategy is approximately 90% at US$10,000 per QALY WTP threshold. This probability was more than 98% at the commonly used WTP threshold of US$50,000 per QALY. Figure 5 of the ESM also presents the results of the Monte Carlo simulation using the incremental cost-effectiveness plane. The distribution of results suggests that IDgenetix® is a cost-effective strategy in more than 98% of the simulations, and is a dominant strategy (positive QALY gain with cost savings) in more than 67% of the simulations.
Fig. 3.
Cost-effectiveness acceptability curve, probabilistic sensitivity analysis comparing IDgenetix®-guided treatment with treatment as usual. ADx IDgenetix® pharmacogenomic test
Discussion
Our findings suggest that using the IDgenetix® test to guide treatment of patients with moderate or severe depression (HAM-D ≥ 20) and/or anxiety (HAM-A ≥ 18) is a dominant strategy. Compared with TAU, IDgenetix®-guided treatment is expected to result in additional QALYs gained and reduced total costs over a 3-year time horizon after accounting for a one-time test cost of US$2000. The benefits of the IDgenetix® test accumulate over time and are estimated to be considerably larger over a 10-year or longer time horizon.
The economic value of the IDgenetix® test is particularly substantial in patients with severe depression (HAM-D ≥ 25). These patients are often hard to treat and require longer trial-and-error periods, causing high clinical and economic burden. The significant improvements in remission and response rates in this patient subgroup, as has been demonstrated in the IDgenetix® RCT, directly translated to a high economic value in our evaluation. We found that cost savings from implementing IDgenetix® could be as large as US$6800 over 3 years in patients with severe depression. In patients with anxiety, however, the benefits of the IDgenetix® test did not vary based on disease severity. Nevertheless, we found that using IDgenetix® in patients with anxiety is still cost effective because of significant improvements in response rates.
The sensitivity analysis showed that our results were generally robust to the changes in model input parameters. As expected, estimated cost-effectiveness results were most sensitive to our assumptions about remission and response rates of alternative treatment strategies. Although the test cost had direct impact on the results, the IDgenetix® strategy remained cost saving for test costs less than US$2500 and stayed cost effective at even higher test costs. This was because a one-time test cost could be quickly recovered by improving remission and response rates and the subsequent reduction in the direct and indirect costs of depression and anxiety. Our probabilistic sensitivity analyses, furthermore, showed that using IDgenetix® is cost effective, even at very low WTP thresholds. These results intuitively make sense because the impact of the IDgenetix® test on the efficacy of guided treatment exceeds that of many expensive medications or other interventions that need to be used for extended periods [2].
An important advantage of our analysis is that the efficacy parameters in our model were directly informed based on the estimates obtained from a double-blinded RCT comparing IDgenetix® guided treatment with TAU [12]. This was the first large-scale RCT directly assessing the efficacy of using a pharmacogenomic test compared with TAU. Randomization and blinding of patients and raters ensured unbiased estimates of efficacy, an advantage often hard to achieve in open-label observational studies because of unmeasured confounding.
The RCT included patients enrolled in psychiatric and non-psychiatric clinics, suggesting that IDgenetix®-guided treatment can be successfully implemented in psychiatry, internal medicine, family medicine, neurology, and obstetrics and gynecology. This is of particular importance because 70–80% of prescriptions for psychiatric medications are now written by family medicine practitioners, primary care physicians, internal medicine practitioners, and obstetrician/gynecologists [28]. Additionally, the RCT included patients with concurrent depression and anxiety, adding to the generalizability of the results to real-world patient populations.
The patient population included in the final analysis of the IDgenetix® RCT was similar to the patient population in the STAR*D trial in terms of depression severity: the mean HAM-D score was 20 in the IDgenetix® trial and 19.9 at study entry for the STAR*D trial. However, STAR*D patients were younger on average (mean age was 48 years and 40 years in the IDgenetix® trial and STAR*D study, respectively). In the absence of large randomized trials, previous cost-effectiveness studies of pharmacogenomic tests for depression mainly relied on the results of published observational cohort studies or small randomized trials to inform their model assumptions. A study conducted by Hornberger et al. compared the cost effectiveness of the GeneSight® test compared with TAU using a simulation analysis [29]. They combined the evidence from a published RCT (n = 51) [10] and two open-label non-randomized studies [30] to estimate the efficacy rates of the GeneSight® test-guided treatment. Their results suggested that pharmacogenomics-guided treatment was a dominant strategy, as it increased QALY gains and reduced the costs [29]. Because data on remission rates were not available, efficacy was modeled only based on treatment response rates. Several randomized trials are currently underway to assess the efficacy of the GeneSight® test-guided treatment [7] and might provide additional evidence of its efficacy and value. Other notable differences between the current analysis and Hornberger et al.’s model were the choice of model time horizon (3 years vs lifetime), and the assumptions about direct and indirect cost of depression.
In our model, we focused on disease-specific costs using the observed difference between patients with and without depression as reported by Greenberg et al. [23]. The unit costs in Hornberger et al., however, were obtained from a different study [22] and reflected the costs in treatment-responsive and treatment-resistant patients with depression. The cost-effectiveness study conducted by Perlis and colleagues [31] evaluated a pharmacogenetic test and found that using the test to identify and treat those at a higher risk of non-response with bupropion rather than initially treating all patients with selective serotonin reuptake inhibitors resulted in US$95,000 per QALY. However, the pharmacogenomic test was specifically focused on a single nucleotide polymorphism associated with response to citalopram. Therefore, their results were not comparable to ours because IDgenetix® is a combinatorial test that provides treatment guidance on a comprehensive panel of 40 medications and related gene–gene and drug–gene interactions and appears to provide a higher improvement in response and remission rates.
Our results mainly apply to the specific patient populations described in this analysis. The target population in our study was identical to participants in the IDgenetix® RCT; patients with moderate or severe depression (HAM-D ≥ 20) and/or anxiety (HAM-A ≥ 18). Therefore, the results do not apply to patients with mild depression and/or anxiety. The results of the National Comorbidity Survey Replication suggested that the 12-month prevalence of MDD was 6.6% (more than 13 million adults in USA) where approximately 90% of those were considered moderate-to-severe cases. Considering the heterogeneity of clinical benefits and costs in different patient subgroups, the estimated outcomes can vary by patient characteristic and cohort composition. It should also be noted that several comorbidities were considered exclusionary criteria in the IDgenetix® RCT, including concurrent diagnosis of bipolar disorder, schizophrenia, personality disorder, traumatic physical injury, significant risk for suicide, and hospitalization. Therefore, our economic evaluation may not directly apply to patients excluded from the trial. In addition, data on the long-term progression of depression and anxiety and the pattern and frequency of relapse are limited.
Our model extrapolated relapse events based on the rates observed in the STAR*D study. However, the data reported by Marcotte et al. [17] was the only data source that could be used to validate accuracy of our extrapolation over longer time periods. Overestimation or underestimation of relapse rates may influence the estimated cost and clinical benefits. However, we expect a minimal impact on the base-case results that only reported the outcomes within a 3-year time frame. Using the results from the STAR*D study to inform some of our model inputs was justified considering the overall similarities between patient populations in the STAR*D study and the IDgenetix® trial. The patient population in the STAR*D study was similar to IDgenetix® trial participants in terms of severity of depression, a higher proportion of female patients, and racial distribution. However, patients enrolled in the IDgenetix® trial on average were older (mean age was 48 years in the IDgenetix® trial and 40 years in the STAR*D study, respectively).
We assumed that the remission and response rates observed at the end of the RCT (3 months) apply to future episodes, albeit after adjusting for a reduction in efficacy for higher treatment levels. We believe that this is a realistic assumption in the absence of long-term trial data. We used QOL weights from Mrazek et al. to inform model inputs for our base-case analysis. Mrazek et al. combined QOL weights from four different studies measured using Standard Gamble and EQ-5D to provide average estimates for patients with different treatment outcomes (i.e., remission, response, no response). Despite important limitations of their approach for combining QOL weights measured using different methods, we used those values in our base-case analysis because they resulted in conservative estimates for cost benefits of the IDgenetix® test.
The annual costs attributable to depression and anxiety in our model are based on the study by Greenberg et al. This study included patients with MDD with 27% having anxiety disorder. Therefore, generalizability of those unit costs to our study population is unclear, considering that 45% of the patient population in our study had anxiety only. Furthermore, in the absence of cost data for different severity levels, we used the same unit costs for all severity levels, which is a limitation our analysis. Finally, we did not include the costs associated with presenteeism and wage loss related to suicide in the calculation of indirect costs. Considering that the cost of presenteeism is estimated to be greater than three-fold larger than the cost of absenteeism [23], the inclusion of presenteeism would have resulted in a substantial change in the results in favor of IDgenetix®.
Conclusion
In summary, we found that implementing IDgenetix®-guided treatment of patients with moderate-to-severe depression and/or anxiety is likely to result in cost savings and improved QOL, compared with TAU. Our model was informed by the results of a relatively large randomized clinical trial and the cost-effectiveness results were robust to the changes in model parameters. The impact of the IDgenetix® test on treatment efficacy is larger or, at minimum, comparable to what one might expect from a novel and effective therapeutic option. Overall, several features of the IDgenetix® test, such as the efficacy of a guided treatment strategy, one-time test cost, and the prospect of using test results for guiding future episodes of depression or anxiety, make it a potentially dominant strategy compared with usual care.
Data Availability Statement
The statistical code is available in the Electronic Supplementary Material (ESM). All data and input parameters and sources are provided in the text and ESM. Any question or request about the statistical code, data sources, or methods can be forwarded to Dr. Maciel (AMaciel@altheadx.com).
Electronic supplementary material
Below is the link to the electronic supplementary material.
Author Contributions
Concept and design: MN, AM; acquisition of data: MN, AM, JG; statistical model and analysis: MN; interpretation of results: MN, AM, JG; drafting of the manuscript: MN; critical revision of the manuscript: MN, AM, JG.
Compliance with Ethical Standards
Funding
No sources of funding were received for the conduct of this study.
Conflict of interest
Dr. Najafzadeh was a consultant to AltheaDx for the conduct of this study. Drs. Garces and A. Maciel are employees of AltheaDx.
Footnotes
Electronic supplementary material
The online version of this article (10.1007/s40273-017-0587-0) contains supplementary material, which is available to authorized users.
References
- 1.Wiles N, Thomas L, Abel A, Ridgway N, Turner N, et al. Cognitive behavioural therapy as an adjunct to pharmacotherapy for primary care based patients with treatment resistant depression: results of the CoBalT randomised controlled trial. Lancet. 2013;381:375–384. doi: 10.1016/S0140-6736(12)61552-9. [DOI] [PubMed] [Google Scholar]
- 2.Khan A, Faucett J, Lichtenberg P, Kirsch I, Brown WA. A systematic review of comparative efficacy of treatments and controls for depression. PLoS One. 2012;7:e41778. doi: 10.1371/journal.pone.0041778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gelenberg AJ. A review of the current guidelines for depression treatment. J Clin Psychiatry. 2010;71:e15. doi: 10.4088/JCP.9078tx1c. [DOI] [PubMed] [Google Scholar]
- 4.Trivedi MH, Rush AJ, Wisniewski SR, Nierenberg AA, Warden D, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychiatry. 2006;163:28–40. doi: 10.1176/appi.ajp.163.1.28. [DOI] [PubMed] [Google Scholar]
- 5.Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- 6.Tansey KE, Guipponi M, Hu X, Domenici E, Lewis G, et al. Contribution of common genetic variants to antidepressant response. Biol Psychiatry. 2013;73:679–682. doi: 10.1016/j.biopsych.2012.10.030. [DOI] [PubMed] [Google Scholar]
- 7.Peterson K, Dieperink E, Anderson J, Boundy E, Ferguson L, et al. Rapid evidence review of the comparative effectiveness, harms, and cost-effectiveness of pharmacogenomics-guided antidepressant treatment versus usual care for major depressive disorder. Psychopharmacology (Berl). 2017;234(11):1649–1661. doi: 10.1007/s00213-017-4622-9. [DOI] [PubMed] [Google Scholar]
- 8.Rosenblat JD, Lee Y, McIntyre RS. Does pharmacogenomic testing improve clinical outcomes for major depressive disorder? A systematic review of clinical trials and cost-effectiveness studies. J Clin Psychiatry. 2017;78(6):720–729. doi: 10.4088/JCP.15r10583. [DOI] [PubMed] [Google Scholar]
- 9.Singh AB. Improved antidepressant remission in major depression via a pharmacokinetic pathway polygene pharmacogenetic report. Clin Psychopharmacol Neurosci. 2015;13:150. doi: 10.9758/cpn.2015.13.2.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Winner JG, Carhart JM, Altar CA, Allen JD, Dechairo BM. A prospective, randomized, double-blind study assessing the clinical impact of integrated pharmacogenomic testing for major depressive disorder. Discov Med. 2013;16:219–227. [PubMed] [Google Scholar]
- 11.Breitenstein B, Scheuer S, Pfister H, Uhr M, Lucae S, et al. The clinical application of ABCB1 genotyping in antidepressant treatment: a pilot study. CNS Spectr. 2014;19:165–175. doi: 10.1017/S1092852913000436. [DOI] [PubMed] [Google Scholar]
- 12.Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness in health and medicine. New York: Oxford University Press; 1996. [Google Scholar]
- 13.Neumann PJ, Cohen JT, Weinstein MC. Updating cost-effectiveness: the curious resilience of the $50,000-per-QALY threshold. N Engl J Med. 2014;371:796–797. doi: 10.1056/NEJMp1405158. [DOI] [PubMed] [Google Scholar]
- 14.O’Brien B, Briggs A. Analysis of uncertainty in health care cost-effectiveness studies: an introduction to statistical issues and methods. Stat Methods Med Res. 2002;11:455–468. doi: 10.1191/0962280202sm304ra. [DOI] [PubMed] [Google Scholar]
- 15.Davidson J. Major depressive disorder treatment guidelines in America and Europe. J Clin Psychiatry. 2010;71(Suppl. E1):e04. doi: 10.4088/JCP.9058se1c.04gry. [DOI] [PubMed] [Google Scholar]
- 16.Geddes JR, Carney SM, Davies C, Furukawa TA, Kupfer DJ, et al. Relapse prevention with antidepressant drug treatment in depressive disorders: a systematic review. Lancet. 2003;361:653–661. doi: 10.1016/S0140-6736(03)12599-8. [DOI] [PubMed] [Google Scholar]
- 17.Marcotte DE, Wilcox-Gok V, Redmon P. Prevalence and patterns of major depressive disorder in the United States labor force. J Ment Health Policy Econ. 1999;2:123–131. doi: 10.1002/(SICI)1099-176X(199909)2:3<123::AID-MHP55>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 18.Simon GE, Savarino J, Operskalski B, Wang PS. Suicide risk during antidepressant treatment. Am J Psychiatry. 2006;163:41–47. doi: 10.1176/appi.ajp.163.1.41. [DOI] [PubMed] [Google Scholar]
- 19.Olin B, Jayewardene AK, Bunker M, Moreno F. Mortality and suicide risk in treatment-resistant depression: an observational study of the long-term impact of intervention. PLoS One. 2012;7:e48002. doi: 10.1371/journal.pone.0048002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Arias E, Heron M, Tejada-Vera B. United States life tables eliminating certain causes of death, 1999–2001. Natl Vital Stat Rep. 2013;61(9):1–128. [PubMed]
- 21.Sullivan PW, Ghushchyan V. Preference-based EQ-5D index scores for chronic conditions in the United States. Med Decis Mak. 2006;26:410–420. doi: 10.1177/0272989X06290495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mrazek DA, Hornberger JC, Altar CA, Degtiar I. A review of the clinical, economic, and societal burden of treatment-resistant depression: 1996–2013. Psychiatr Serv. 2014;65:977–987. doi: 10.1176/appi.ps.201300059. [DOI] [PubMed] [Google Scholar]
- 23.Greenberg PE, Fournier A-A, Sisitsky T, Pike CT, Kessler RC. The economic burden of adults with major depressive disorder in the United States (2005 and 2010) J Clin Psychiatry. 2015;76:155–162. doi: 10.4088/JCP.14m09298. [DOI] [PubMed] [Google Scholar]
- 24.Statistics BoL. Consumer price inflation (CPI) calculator. US Bureau of Labor Statistics; 2017. https://www.bls.gov/data/inflation_calculator.htm. Accessed 20 Aug 2017.
- 25.Claxton K, Sculpher M, McCabe C, Briggs A, Akehurst R, et al. Probabilistic sensitivity analysis for NICE technology assessment: not an optional extra. Health Econ. 2005;14:339–347. doi: 10.1002/hec.985. [DOI] [PubMed] [Google Scholar]
- 26.Briggs AH. Handling uncertainty in cost-effectiveness models. Pharmacoeconomics. 2000;17:479–500. doi: 10.2165/00019053-200017050-00006. [DOI] [PubMed] [Google Scholar]
- 27.Spiegelhalter DJ, Best NG. Bayesian approaches to multiple sources of evidence and uncertainty in complex cost-effectiveness modelling. Stat Med. 2003;22:3687–3709. doi: 10.1002/sim.1586. [DOI] [PubMed] [Google Scholar]
- 28.Mark TL, Levit KR, Buck JA. Datapoints: psychotropic drug prescriptions by medical specialty. Psychiatr Serv. 2009;60:1167. doi: 10.1176/ps.2009.60.9.1167. [DOI] [PubMed] [Google Scholar]
- 29.Hornberger J, Li Q, Quinn B. Cost-effectiveness of combinatorial pharmacogenomic testing for treatment-resistant major depressive disorder patients. Am J Manag Care. 2015;21:e357–e365. [PubMed] [Google Scholar]
- 30.Hall-Flavin DK, Winner JG, Allen JD, Carhart JM, Proctor B, et al. Utility of integrated pharmacogenomic testing to support the treatment of major depressive disorder in a psychiatric outpatient setting. Pharmacogenet Genom. 2013;23:535–548. doi: 10.1097/FPC.0b013e3283649b9a. [DOI] [PubMed] [Google Scholar]
- 31.Perlis RH, Patrick A, Smoller JW, Wang PS. When is pharmacogenetic testing for antidepressant response ready for the clinic? A cost-effectiveness analysis based on data from the STAR*D study. Neuropsychopharmacology. 2009;34:2227–2236. doi: 10.1038/npp.2009.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bradley P, Shiekh M, Mehra V, Vrbicky K, Layle S, et al. Improved efficacy with targeted pharmacogenetic-guided treatment of patients with depression and anxiety: a randomized clinical trial demonstrating clinical utility. J Psychiatr Res. 2017;96:100–7. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The statistical code is available in the Electronic Supplementary Material (ESM). All data and input parameters and sources are provided in the text and ESM. Any question or request about the statistical code, data sources, or methods can be forwarded to Dr. Maciel (AMaciel@altheadx.com).