To the Editor: Dural arteriovenous fistula (dAVF) is a rare disease accounting for fewer than 10% of all cerebral vascular malformations.[1] Intracranial dAVF with perimedullary venous drainage is very rare and prone to misdiagnosis because of its indistinct clinical and radiological manifestation. Here, we present such a case that was initially misdiagnosed as brainstem neoplasm.
A 67-year-old woman who manifested headache and progressive confusion for one month was admitted to our hospital. On admission, she was in a state of somnolence; her Glasgow coma score was 12. Her muscle strength was graded 3/5 on the left side and 4/5 on the right side, and bilateral Babinski signs were positive. Tumor-like lesions were found in the right cerebellar hemisphere and pons on magnetic resonance imaging (MRI) [Figure 1a–1d]. Neither dilated vessel nor flow voids were detected around the brainstem. Routine blood investigations and cerebrospinal fluid tests were unremarkable. Aquaporin-4 and myelin-oligodendrocyte glycoprotein antibodies were all negative. Brainstem tumor was initially suspected, and brain biopsy was scheduled. However, the hypodensity observed in the subsequent susceptibility weighted imaging (SWI) raised the possibility of a vascular problem [Figure 1e]. Cerebral angiography was performed, and an intracranial dAVF was found in the superior petrosal sinus with perimedullary drainage [Figure 1f and 1g]. Endovascular embolization of the fistula was performed using the transarterial approach. Several weeks later, the patient's consciousness was improved, and repeated MRI showed marked alleviation [Figure 1h].
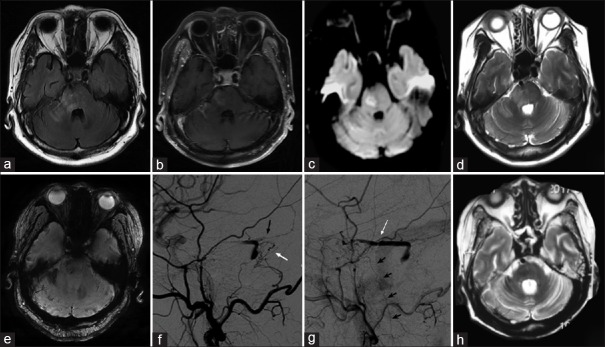
Figure 1.
Representative images of the patient. (a and d) Axial FLAIR magnetic resonance imaging and T2W showed multiple hyperintense lesions in the right cerebellum and pons. (b) This was partially enhanced by contrast. (c) DWI showed some hyperintense signals. (e) SWI showed multiple microbleeds. (f and g) Cerebral angiography showed a dAVF supplied by a distal dural branch of the occipital artery (white arrow), and (f) the petrosal branch of the middle meningeal artery (black arrow), draining into the right superior petrosal sinus (white arrow) and (g) refluxed into the perimedullary vein (small black arrows). (h) T2W showed the lesions vanished several weeks after treatment. FLAIR: Fluid attenuated inversion recovery; dAVF: Dural arteriovenous fistula; T2W: T2-weighted images; DWI: Diffusion weighted imaging; SWI: Susceptibility weighted imaging.
Intracranial dAVF with perimedullary venous drainage is a rare disease that was first described in 1982. Only a small number of cases have been reported in the literature.[2] The majority of reported cases have been located on the dura mater of the posterior fossa, and very few of them were found in the cavernous sinus. Clinical manifestation of intracranial dAVF is extremely heterogeneous, ranging from nondisabling tinnitus to intracranial hemorrhage, seizure, and venous hypertension encephalopathy. The precise manifestation is mainly determined by anatomical location and venous drainage pattern.[3] On MRI, dilated vessels and flow voids can be found in the subarachnoid space at the spinal cord or brainstem. In the present rare case, the dAVF was located in the superior petrosal sinus and drained into the perimedullary vein. According to the Cognard classification, it was classified as a Type V fistula, which is characterized by perimedullary venous drainage associated with progressive myelopathy and brainstem dysfunction.
Venous congestion leading to brainstem masses like lesions seem to be related to the involvement of the right superior petrosal vein, which is connected to the superior petrosal sinus superiorly and to the anterior spinal vein inferiorly. The superior petrosal vein mainly collects venous blood from cerebellar hemisphere and lateral pons. Venous congestion of superior petrosal vein may cause lesions in these areas. The clinical diagnosis of dAVF was very challenging. Brainstem abnormal signal with contrast enhancement may raise the possibility of brainstem tumors. However, careful investigations looking for evidence of inflammatory, infectious or vascular etiology were also necessary for differential diagnosis.[4] Although neither dilated vessel nor flow voids were detected, a hypointense signal was found on SWI, indicating the possibility of a vascular problem. If this is the case, cerebral angiography should be performed for confirming the diagnosis and establishing an intervention strategy. If the diagnosis is delayed too much, the patient may suffer permanent neurologic deficits.[5]
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Footnotes
Edited by: Yi Cui
REFERENCES
- 1.Hacein-Bey L, Konstas AA, Pile-Spellman J. Natural history, current concepts, classification, factors impacting endovascular therapy, and pathophysiology of cerebral and spinal dural arteriovenous fistulas. Clin Neurol Neurosurg. 2014;121:64–75. doi: 10.1016/j.clineuro.2014.01.018. doi: 10.1016/j.clineuro.2014.01.018. [DOI] [PubMed] [Google Scholar]
- 2.Renner C, Helm J, Roth H, Meixensberger J. Intracranial dural arteriovenous fistula associated with progressive cervical myelopathy and normal venous drainage of the thoracolumbar cord: Case report and review of the literature. Surg Neurol. 2006;65:506–10. doi: 10.1016/j.surneu.2005.06.022. doi: 10.1016/j.surneu.2005.06.022. [DOI] [PubMed] [Google Scholar]
- 3.Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995;82:166–79. doi: 10.3171/jns.1995.82.2.0166. doi: 10.3171/jns.1995.82.2.0166. [DOI] [PubMed] [Google Scholar]
- 4.Le Guennec L, Leclercq D, Szatmary Z, Idbaih A, Reyes-Botero G, Delattre JY, et al. Dural arteriovenous fistula mimicking a brainstem glioma. J Neuroimaging. 2015;25:1053–5. doi: 10.1111/jon.12220. doi: 10.1111/jon.12220. [DOI] [PubMed] [Google Scholar]
- 5.Gandhi D, Chen J, Pearl M, Huang J, Gemmete JJ, Kathuria S. Intracranial dural arteriovenous fistulas: Classification, imaging findings, and treatment. AJNR Am J Neuroradiol. 2012;33:1007–13. doi: 10.3174/ajnr.A2798. doi: 10.3174/ajnr.A2798. [DOI] [PMC free article] [PubMed] [Google Scholar]