Abstract
Background
Over 10% of hospice patients experience at least one care transition 6-months prior to death. Transitions at the End-of-Life (EoL), particularly from hospice to hospital, result in burdensome and fragmented care for patients and families. Little is known about factors that predict hospitalization in this population.
Objectives
To develop and validate a model predictive of hospitalization after enrollment into home hospice using pre-hospice admission risk factors.
Design
Retrospective cohort study using Medicare fee-for-service claims.
Subjects
Patients enrolled into the Medicare Hospice Benefit >= 18 years old in 2012.
Outcome Measured
Hospitalization within 2 days from a hospice discharge.
Results
We developed a predictive model using 61,947 hospice enrollments, of which 3,347 (5.4%) underwent a hospitalization. Seven variables were associated with hospitalization: age 18–55 years old (adjusted odds ratio [95% confidence interval]; 2.94 [2.41–3.59]), Black race (2.13, [1.93–2.34]), East region (1.97, [1.73–2.24]), a non-cancer diagnosis (1.32, [1.21–1.45]), 4 or more chronic conditions (8.11, [7.19–9.14]), 2 or more prior hospice enrollments (1.75, [1.35–2.26]), and enrollment in a not-for-profit hospice (2.01, [1.86–2.18]). A risk scoring tool ranging from 0 to 29 was developed and a cutoff score of 18 identified hospitalized patients with a positive predictive value of 22%.
Conclusions
Reasons for hospitalization among home hospice patients are complex. Patients who are younger, belong to a minority group, and have a greater number of chronic conditions are at increased odds of hospitalization. Our newly developed predictive tool identifies patients at risk for hospitalization and can serve as a benchmark for future model development.
Keywords: Home hospice, hospitalization, End-of-life, predictive modeling
Introduction
Many terminally ill patients prefer to die at home.1,2 For these patients, home hospice care provides an opportunity to live the end of their lives among family and friends. Care is focused on reducing suffering, maximizing quality of life, and supporting patients and their caregivers. Since its creation in 1982, the Medicare Hospice Benefit has steadily grown, with over 1.5 million patient admissions in 2014.3 More than 45% of all U.S. deaths occur with hospice care.4,5
One of the goals of hospice as outlined in a 2014 Department of Health and Human Services report is to “make patients physically and emotionally comfortable with minimal disruption to normal activities, while remaining primarily in the home environment.”6 Despite efforts to maintain care for patients at home, there is a growing concern regarding care transitions into and out of hospice (e.g. hospice to hospital, hospice to nursing home) at the End-of-Life (EoL). Over 10% of hospice patients experience at least one care transition within the 6 months prior to death.7 The Institute of Medicine (IOM) recognizes this problem and has called for ways to reduce fragmentation in EoL care.8
Of all hospice care transitions, the transition from home hospice to an acute care hospital is arguably most burdensome and can lead to unwanted, aggressive treatments inconsistent with patients’ goals.9,10 Reasons surrounding hospitalization can be complex and influenced by patient, caregiver, and/or hospice related factors.11,12 The Medicare Hospice Payment Reform Report has labeled these events as “burdensome” transitions. Since 2000, the rate of these burdensome transitions has almost doubled.13
Given the impact hospitalization can have on patient care, reducing it is an important part of delivering high quality EoL care. However, little is known about which patients are at risk.12,14,15 The objective of this study is to analyze pre-hospice admission risk factors associated with hospitalization in order to develop and validate a predictive tool aimed at identifying home hospice patients at risk for hospitalization. Based on literature in other patient populations, we hypothesized that patients’ age, race, and number of chronic conditions would be significant determinants of hospitalization risk.7,16
Methods
Study Design
We conducted a retrospective cohort study using Medicare fee-for-service claims from the Centers for Medicare and Medicaid Services (CMS). The study was approved by the institutional review board of Weill Cornell Medical College.
Data Sources
We merged 2012 data from three CMS data files: (1) Hospice Research Identifiable File (RIF), (2) Chronic Conditions Summary file, and (3) the Medical Provider Analysis and Review (MedPAR) RIF. The Hospice RIF contains patient demographic data and claims submitted by hospice providers. The Chronic Conditions Summary file flags 26 predefined chronic conditions for each beneficiary. The MedPAR RIF contains acute care hospital claims data, which we used to confirm a hospitalization after a hospice discharge.
Study sample
The unit of analysis was the enrollment of a patient into hospice. Our initial study cohort included a random sample of 1 million Medicare fee-for-service beneficiaries enrolled in hospice in 2012. To be included in the study, patients had to be enrolled in a home hospice agency between April 1, 2012 through June 30, 2012. We selected this timeframe in order to: (1) examine whether previous hospital utilization (e.g., number of acute care hospital admissions) 3 months prior to enrollment influenced risk of hospitalization and; (2) have at least a 6 month window from the time of enrollment to examine whether a hospitalization occurred. The choice of a 6 month window was based on the presumption that hospice patients have a life expectancy of 6 months or less. We excluded any enrollments that documented more than one hospice diagnosis because we were not able to clearly distinguish the patient’s terminal diagnosis. We also excluded enrollments that were not flagged as having care delivered at home and enrollments with missing data in any of these fields: age, gender, race/ethnicity, patient’s state of residence, hospice diagnosis, hospice profit status.
Furthermore, we excluded enrollments that had incongruent reasons for discharge (e.g. a patient discharged from hospice and flagged as both having revoked care and dying on hospice) or were flagged as having “revoked care” and not hospitalized. Revocation of hospice care is a right of the patient and reasons for revoking care (e.g. pursuing more aggressive care) are varied. As a result, the final sample compared patients who were hospitalized to patients who died prior to or were still alive on hospice as of December 31, 2012.
Outcome variable
The outcome of interest was a hospice discharge that resulted in a subsequent hospitalization within 2 days, which has been used as an outcome in a previous study.17 We identified this outcome by cross-referencing the date of hospice discharge from the Hospice RIF with the date of hospitalization from the MedPAR RIF. Patients who transitioned from home hospice to an inpatient hospice setting were not included since we considered this particular care transition to be a continuation of hospice care.
Definition of Predictor Variables
The selection of candidate pre-hospice predictor variables for hospitalization was based on a literature search and clinical experience.16,18 Given that our objective was to develop a tool that could be used by hospices at the time of enrollment, we only examined pre-hospice variables. Candidate variables were extracted from all three datasets and included: age, gender, race, region, hospice profit status, hospice terminal diagnoses (dichotomized as cancer vs. non-cancer), number of hospitalizations 3 months prior to the date of enrollment, number of previous hospice enrollments, and number of chronic conditions. Three geriatric/palliative trained physicians (RDA, VP, MCR) reviewed the 26 predefined diseases listed in the Chronic Conditions summary file and divided the conditions into three groups. The first group included 14 chronic conditions (i.e., hypertension, hyperlipidemia, congestive heart failure, myocardial infarction, atrial fibrillation, chronic obstructive pulmonary disease, asthma, chronic kidney disease, dementia, Alzheimer’s disease, stroke/TIA, diabetes, history of hip fracture, depression) with high clinical relevance to hospitalization.19–23 We re-categorized these into 8 groups (heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, history of hip fracture, depression) and included them as covariates in our regression analysis. The second group included 7 conditions (i.e., osteoporosis, rheumatoid arthritis/osteoarthritis, anemia, cataract, glaucoma, hypothyroid, benign prostatic hyperplasia), which were excluded from our regression analysis because we did not find any robust literature associating these conditions with hospitalization. The third group included conditions (i.e., breast cancer, colorectal cancer, prostate cancer, lung cancer, endometrial cancer) with considerable overlap with hospice terminal diagnoses, which we also excluded from our regression analyses.
Statistical Analysis
We randomly divided our final cohort in half to create a development set and a validation set for our predictive analysis. The development set was used to construct the predictive model while the validation set was used to evaluate its performance. The two sets were compared using Chi-square tests for categorical variables and Wilcoxon sign-rank tests for continuous variables to assess whether there were significant differences between the two groups. We then performed bivariate analyses to identify candidate predictor variables. Those variables associated with the outcome of hospitalization (P-value <0.2) were subsequently entered into a multivariable logistic regression model. Using a backward stepwise elimination approach, logistic regression was performed to identify variables independently associated with the outcome of interest.24 A final set of risk factors were selected based on statistical significance (P-value <0.05) and ease of implementation. The model was subsequently applied to the validation set and an area under the receiver-operating curve (ROC) was calculated for both sets and compared.
To make estimates from the logistic model more interpretable, we developed a risk scoring tool. The scoring tool was modeled after a regression coefficient-based scoring method.25,26 Scores were assigned by dividing the smallest risk-factor coefficient (i.e., 0.212) in our multivariable model into the coefficient of each individual risk factor then rounding it to the nearest integer.27 The overall risk score for each enrollment was subsequently determined by adding up the scores for each risk factor in the model. The predictive accuracy of the model was determined by calculating sensitivity, specificity, positive predictive value, and negative predictive value at multiple cutoff points. Statistical analysis was conducted using STATA MP 14.1 (College Station, Tx).
Results
Description of study cohort and hospitalization
There were 384,484 hospice enrollments between April 1, 2012 and June 30, 2012 in our study cohort. We excluded cases in which: (1) there was no flag that care was delivered at home (N=126,555), (2) there were incongruent reasons for discharge (N=59,510), (3) there was more than one or no documented hospice diagnosis (N=66,044), or (4) there were observations that had missing predictor variables (N=8,581). The final cohort used for our analysis consisted of 123,894 enrollments, of which a total of 6,797 (5.5%) enrollments were hospitalized +/− 2 days after hospice discharge.
The final cohort was randomly split into a development (N=61,947) and a validation (N=61,947) set. Hospitalization occurred in 3347 (5.4%) enrollments in the development set and 3450 (5.6%) enrollments in the validation set. In the development set, a majority of home hospice patients (59%) were not hospitalized in the 3 months prior to enrollment into hospice. There were no significant differences between the development and validation sets with regards to age, gender, race, region, hospice terminal diagnosis, number of hospitalizations 3 months prior to the date of enrollment, number of previous hospice enrollments, number of chronic conditions, and hospice profit status (Table 1).
Table 1.
Characteristics of Home Hospice Enrollments in Development and Validation Set
| Characteristics | Development (N=61947) |
Validation (N=61947) |
P-value | |
|---|---|---|---|---|
| Age (years) | 0.37 | |||
| 18–55 | 1291 (2.1) | 1317 (2) | ||
| 56–65 | 3780 (6.1) | 3739 (6) | ||
| 66–75 | 12776 (20.6) | 13055 (21.2) | ||
| 76–85 | 20906 (33.8) | 20794 (33.6) | ||
| 86+ | 23194 (37.4) | 23042 (37.2) | ||
| Median (IQRa) | 82 (74–89) | 82 (74–89) | 0.29 | |
| Gender | 0.5 | |||
| Women | 35903 (58) | 36019 (58) | ||
| Men | 26044 (42) | 25928 (42) | ||
| Race/Ethnicity | 0.99 | |||
| White | 52696 (85.1) | 52690 (85.1) | ||
| Black | 5984 (9.6) | 5977 (9.6) | ||
| Other | 3267 (5.3) | 3280 (5.3) | ||
| Region | 0.17 | |||
| Midwest | 12174 (19.7) | 11864 (19.2) | ||
| West | 15532 (25.1) | 15597 (25.2) | ||
| East | 9367 (15.1) | 9446 (15.2) | ||
| South | 24874 (40.1) | 25040 (40.4) | ||
| Hospice Diagnosis | 0.22 | |||
| Cancer | 21023 (34) | 20818 (34) | ||
| Non-cancer | 40924 (66) | 41129 (66) | ||
| Number of Chronic Conditionsb | 0.61 | |||
| 0–1 | 23654 (38.2) | 23523 (38) | ||
| 2 | 12187 (19.7) | 12202 (19.7) | ||
| 3 | 12190 (19.7) | 12120 (19.6) | ||
| 4+ | 13916 (22.4) | 14102 (22.7) | ||
| Median (IQR) | 2 (1–3) | 2 (1–3) | 0.7 | |
| Health Services Utilization | ||||
| Number of hospitalizations 3 months prior to date of enrollment | 0.1 | |||
| 0 | 36645 (59) | 36929 (60) | ||
| 1 or more | 25302 (41) | 25018 (40) | ||
| Number of previous hospice enrollments | 0.48 | |||
| 0 | 57375 (92.6) | 57473 (92.8) | ||
| 1 | 4067 (6.6) | 3997 (6.5) | ||
| 2 or more | 505 (0.8) | 477 (0.7) | ||
| Hospice profit status | 0.23 | |||
| For profit | 31258 (50.5) | 31015 (50.1) | ||
| Not-for-profit | 25711 (41.5) | 26008 (42) | ||
| Government | 4978 (8) | 4924 (7.9) | ||
= Interquartile range
= heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, depression, history of hip fracture
Bivariate Predictors of Hospitalization
Patients with 4 or more chronic conditions (OR=8.69, CI 7.72–9.77) had a significantly greater odds of being hospitalized compared to patients with 0 or 1 chronic condition. Patients who received care in a not-for-profit (OR=2.21, CI 2.05–2.38) or government (OR=1.88, CI 1.66–2.14) operated hospices also had an increased odds of hospitalization when compared to for-profit hospices. Furthermore, younger age (OR=2.56, CI 2.12–3.09), non-Black minorities (OR=1.40, CI 1.21–1.62), and Blacks (OR=2.68, CI 2.45–2.92) were associated with greater odds of hospitalization compared to Whites (Table 2).
Table 2.
Bi-variate Analysis of Predictor Variables of Hospitalization in Development Set (N=61947)
| Predictor Variables | Hospitalized (%) | Not Hospitalized (%) | OR (95% CI) | |
|---|---|---|---|---|
| Age (years) | ||||
|
| ||||
| 18–55 | 137 (10.6) | 1154 (89.4) | 2.56 (2.12–3.09) | |
| 56–65 | 291 (7.7) | 3489 (92.3) | 1.80 (1.57–2.06) | |
| 66–75 | 789 (6.2) | 11987 (93.8) | 1.42 (1.29–1.56) | |
| 76–85 | 1103 (5.3) | 19803 (94.7) | 1.20 (1.10–1.31) | |
| 86+ | 1027 (4.4) | 22167 (95.6) | 1 | |
| Gender | ||||
|
| ||||
| Women | 1964 (5.5) | 33939 (94.5) | ||
| Men | 1383 (5.3) | 24661 (94.7) | 0.97 (0.90–1.04) | |
| Race/Ethnicity | ||||
|
| ||||
| White | 2448 (4.7) | 50248 (95.3) | 1 | |
| Black | 690 (11.5) | 5294 (88.5) | 2.68 (2.45–2.92) | |
| Other | 209 (6.4) | 3058 (93.6) | 1.40 (1.21–1.62) | |
| Region | ||||
|
| ||||
| Midwest | 454 (3.7) | 11720 (96.3) | 1 | |
| West | 748 (4.8) | 14784 (95.2) | 1.31 (1.16–1.47) | |
| East | 587 (6.3) | 8780 (93.7) | 1.73 (1.52–1.96) | |
| South | 1558 (6.3) | 23316 (93.7) | 1.72 (1.55–1.92) | |
| Hospice Diagnosis | ||||
|
| ||||
| Cancer | 808 (3.8) | 20215 (96.2) | 1 | |
| Non-cancer | 2539 (6.2) | 38385 (93.8) | 1.65 (1.53–1.79) | |
| Number of Chronic Conditionsa | ||||
|
| ||||
| 0–1 | 351 (1.5) | 23303 (98.5) | 1 | |
| 2 | 535 (4.4) | 11652 (95.6) | 3.05 (2.66–3.49) | |
| 3 | 851 (7) | 11339 (93) | 4.98 (4.39–5.65) | |
| 4+ | 1610 (11.6) | 12306 (88.4) | 8.69 (7.72–9.77) | |
| Health Services Utilization | ||||
|
| ||||
| Number of hospitalizations 3 months prior to date of enrollment | ||||
|
|
||||
| 0 | 1663 (4.5) | 34982 (95.5) | ||
| 1 or more | 1684 (6.7) | 23618 (93.3) | 1.50 (1.40–1.61) | |
| Number of previous hospice enrollments | ||||
|
|
||||
| 0 | 2901 (5.1) | 54474 (94.9) | 1 | |
| 1 | 368 (9.1) | 3699 (90.9) | 1.87 (1.67–2.09) | |
| 2 or more | 78 (15.5) | 427 (84.5) | 3.43 (2.69–4.38) | |
| Hospice profit status | ||||
|
| ||||
| For profit | 1104 (3.5) | 30154 (96.5) | 1 | |
| Not-for-profit | 1922 (7.5) | 23789 (92.5) | 2.21 (2.05–2.38) | |
| Government | 321 (6.5) | 4657 (93.5) | 1.88 (1.66–2.14) | |
= heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, depression, history of hip fracture
Multivariable Analysis
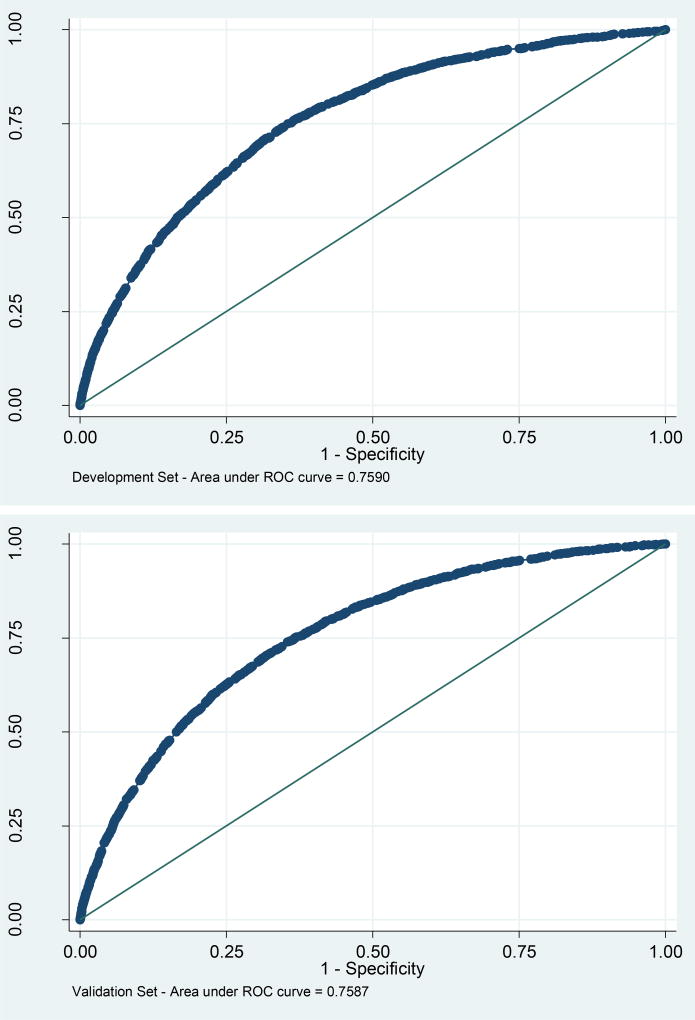
In the multivariable analysis, age, race, region, hospice diagnosis, number of chronic conditions, number of previous hospice enrollments, and hospice profit status were each significantly associated with hospitalization (Table 3). The number of hospitalizations 3 months prior to enrollment was not statistically significant (p = 0.57) in the multivariable analysis and dropped. Our final model included 7 predictor variables. This model had an area under the ROC curve of 0.76 in the development set and 0.76 in the validation set.
Table 3.
Multivariable Predictors of Hospitalization
| Development Cohort (N=61947) | |||
|---|---|---|---|
|
| |||
| Regression coefficient | Odds ratio (95% CI) | ||
| Age (years) | 85+ | 0 | 1 |
| 76–85 | 0.2118459 | 1.24 (1.13–1.35) | |
| 66–75 | 0.4755137 | 1.61 (1.45–1.78) | |
| 56–65 | 0.7395941 | 2.09 (1.82–2.42) | |
| 18–55 | 1.077977 | 2.94 (2.41–3.59) | |
| Race | White | 0 | 1 |
| Black | 0.7540618 | 2.13 (1.93–2.34) | |
| Other | 0.3471183 | 1.41 (1.22–1.65) | |
| Region | Midwest | 0 | 1 |
| West | 0.3286696 | 1.39 (1.23–1.57) | |
| East | 0.6760134 | 1.97 (1.73–2.24) | |
| South | 0.2676567 | 1.31 (1.17–1.46) | |
| Hospice Diagnosis | Cancer | 0 | 1 |
| Non-cancer | 0.2812292 | 1.32 (1.21–1.45) | |
| Number of Chronic Conditionsa | 0–1 | 0 | 1 |
| 2 | 1.1255 | 3.08 (2.69–3.54) | |
| 3 | 1.596627 | 4.94 (4.34–5.61) | |
| 4+ | 2.092593 | 8.11 (7.19–9.14) | |
| Number of previous hospice enrollments | 0 | 0 | 1 |
| 1 | 0.2674227 | 1.31 (1.16–1.47) | |
| 2 or more | 0.5589534 | 1.75 (1.35–2.26) | |
| Hospice profit status | For profit | 0 | 1 |
| Not for profit | 0.6995597 | 2.01 (1.86–2.18) | |
| Government | 0.5274475 | 1.69 (1.48–1.94) | |
= heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, depression, history of hip fracture
Risk scoring tool
The risk scoring tool (Table 4) was derived using the regression coefficients in the multivariate logistic regression analysis from Table 3. Utilizing this scoring system, patients could receive a total score from 0 to 29 based on the risk factors in the model (Table 4). The median score in the development cohort was 10 (Interquartile range [standard deviation]; 6–14 [4.9]). Table 4 lists four cutoff points that were tested along with their corresponding sensitivities, specificities, positive predictive values, and negative predictive values. A cutoff score of 18 or more, which captured 5 percent of enrollments in our development set, predicts hospitalization with a positive predictive value of 22% and a sensitivity of 21%.
Table 4.
Hospitalization Risk Scoring Tool
| Points (Range 0–29) | ||
|---|---|---|
| Age (years) | 85+ | 0 |
| 76–85 | 1 | |
| 66–75 | 2 | |
| 56–65 | 3 | |
| 18–55 | 5 | |
|
| ||
| Race | White | 0 |
| Other | 2 | |
| Black | 4 | |
|
| ||
| Region | Midwest | 0 |
| South | 1 | |
| West | 2 | |
| East | 3 | |
|
| ||
| Hospice Diagnosis | Cancer | 0 |
| Non-cancer | 1 | |
|
| ||
| Number of Chronic Conditionsa | 0–1 | 0 |
| 2 | 5 | |
| 3 | 8 | |
| 4+ | 10 | |
|
| ||
| Number of previous hospice enrollments | 0 | 0 |
| 1 | 1 | |
| 2 or more | 3 | |
|
| ||
| Hospice profit status | For profit | 0 |
| Government | 2 | |
| Not for profit | 3 | |
= heart disease, lung disease, renal disease, dementia disorders, stroke/TIA, diabetes, depression, history of hip fracture
Discussion
Our analysis identified pre-hospice factors associated with hospitalization in the home hospice population. Patients who were younger, belonged to a racial/ethnic minority group, and reported more chronic conditions were more likely to be hospitalized. After developing and applying our risk scoring tool, we found that over 20% of enrollments with scores of 18 or greater were hospitalized. To our knowledge, this is the first predictive risk tool that has been developed and validated in this patient population. Our model serves as a benchmark for future predictive models in the field of care transitions in hospice. Furthermore, this tool can be used by hospices as a preliminary screen to identify at-risk patients where implementation of services (e.g., care management, increased number of nursing visits, continuous home care, inpatient hospice care) may help reduce hospitalization.
Reasons for hospitalizations in this cohort are varied and complex, which makes it challenging to accurately predict our outcome of interest. By using Medicare claims data, we were able to capture a subset of risk factors; however, other predisposing factors (e.g., care preferences, psycho-social influences, caregiver variables) and precipitating factors (e.g., acute symptoms) may be more salient in predicting hospitalization and are not captured in this dataset. Nonetheless, our results provide important associations that can provide insight into how hospices can better identify patients at risk for hospitalization.
Some of our findings echo the results of previous studies in hospice and EoL care.7,18 For example, we found that younger patients had an increased odds of hospitalization which is in agreement with a study demonstrating that younger cancer patients on hospice were more likely to be hospitalized.18 In addition, the impact of the number of chronic conditions on hospitalization is similar to previous work demonstrating that co-morbidities were associated with a care transition at the EoL.7 Patients enrolling in hospice with multiple medical issues typically require more care and caring for patients at home can be challenging, especially when family caregivers are largely responsible for delivering increasingly complex care.28,29
Our analysis showed that racial and ethnic minorities (i.e., Blacks, non-Black minorities) had higher odds of hospitalization when compared to Whites, which builds upon EoL studies in the cancer and heart failure populations.18,30 One study found that Black Medicare beneficiaries with lung or colorectal cancer were more likely to be hospitalized whereas another study reported Black patients diagnosed with heart failure had more emergency department visits and hospitalizations compared to their White counterparts. A prior study suggests that minorities prefer more intensive medical care when compared to Whites at the EoL, which may partially explain this association.2 However, it is important to keep in mind that a majority of minorities still prefer to die at home.2 Further research is needed to better understand the perceptions, barriers and challenges around home hospice care in this group so that interventions can be tailored to reduce care transitions and improve quality of care in the home hospice setting.
We also found that for-profit hospices were associated with lower odds of hospitalization when compared to not-for-profit and government run hospices. This finding adds to the literature examining differences and similarities between for-profit and not-for-profit hospices.7,31 One study comparing the two showed that for-profit hospices were associated with more burdensome care transitions compared to not-for profit hospices.31 Another study found that for-profit hospices enrolled patients with longer lengths of stay and diagnoses associated with lower skilled needs, which may translate to a selection of patients who have fewer care needs and therefore, less risk of hospital utilization.32 We were unable to examine other hospice organizational variables (e.g., size, chain or non-chain, types of services offered), which might help to better understand these results. Further research on this particular topic is merited.
Our findings highlight the critical need for solutions to reduce care transitions in home hospice, particularly transitions to the hospital. Ongoing work in this area includes one study in which utilization of continuous home care in hospice (i.e., providing 24-hour nursing care at a patient’s residence) reduces the risk of an inpatient hospital death.33 This suggests that proactive use of this service may reduce hospice to hospital transitions, and that it may be useful to focus limited resources on the subgroup of patients at greatest risk for hospitalization. Similarly, general inpatient hospice units can provide more intensive palliative services for patients on hospice outside of the patient’s home. Future studies as to whether its use is associated with a reduction in hospitalization is warranted. Finally, nurses play a significant role in the delivery of medical care in the home hospice setting and a recent review found an association between frequency of nursing visits and increased likelihood of a home death.34 Understanding how the role of nursing influences hospitalization and finding ways to effectively deliver nursing care, particularly to the most vulnerable patients should be the focus of future studies. Overall, we believe a multi-pronged approach is needed to address this issue. Targeting patients and caregivers, improving hospice organization and practice, and promoting hospices’ reach through policy change will be key components to reducing transitions from hospice to hospital.
Our study has several limitations. We were unable to identify and include two types of care transitions, observational stays and emergency room visits, which are transitions similar to an acute care hospitalization. In addition, given the limitations (e.g. missing data, incongruent outcomes) of the dataset, we dropped a significant portion of enrollments. However, we felt that our exclusion criteria were appropriate to maintain the objectives of the analysis while still providing us with a large nationally representative analytical cohort of patients receiving care under the Medicare hospice benefit. We did not have details regarding hospice size or practice patterns, which may also influence the odds of hospitalization. Finally, EoL decisions regarding care can be complex and our reliance on claims data did not allow us to capture nuances such as care preferences, psycho-social influences, caregiver burden, and other support-related variables which may be influential in our outcome variable of interest.
Conclusion
In conclusion, we found that patients who were younger, a racial/ethnic minority, and those who had a greater number of chronic conditions were at higher risk of hospitalization. We developed a predictive tool for hospices which aims to identify patients at risk for hospitalization. This tool should serve as a benchmark to assess future predictive models. Identifying these patients and developing interventions to proactively reduce care transitions is important in improving the quality of care we deliver to patients and caregivers at the EoL.
Figure 1.
ROC Curve for Development and Validation Set
Table 5.
| Cutoff score | >=20 | >=18 | >=16 | >=14 |
|---|---|---|---|---|
| Sensitivity | 9.5% | 20.9% | 40.9% | 60.6% |
| Specificity | 98.6% | 95.7% | 88.3% | 75.9% |
| Positive predictive value | 27.9% | 21.6% | 16.6% | 12.5% |
| Negative predictive value | 95.0% | 95.5% | 96.3% | 97.1% |
= Positive predictive value
= Negative predictive value
References
- 1.Townsend J, Frank AO, Fermont D, et al. Terminal cancer care and patients’ preference for place of death: a prospective study. BMJ. 1990;301(6749):415–417. doi: 10.1136/bmj.301.6749.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Barnato AE, Anthony DL, Skinner J, Gallagher PM, Fisher ES. Racial and Ethnic Differences in Preferences for End-of-Life Treatment. J Gen Intern Med. 2009;24(6):695–701. doi: 10.1007/s11606-009-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.http://www.nhpco.org/sites/default/files/public/Statistics_Research/2014_Facts_Figures.pdf
- 4.National Hospice and Palliative Care Organization. 2012 Hospice Care in America. 2012 www.nhpco.org.
- 5.Department of Health and Human Services. Federal Register. 2015 doi: 10.3109/15360288.2015.1037530. [DOI] [PubMed] [Google Scholar]
- 6.Department of Health and Human Services. Federal Register. 2014 [Google Scholar]
- 7.Wang S-Y, Aldridge MD, Gross CP, et al. Transitions Between Healthcare Settings of Hospice Enrollees at the End of Life. J Am Geriatr Soc. 2016;64(2):314–322. doi: 10.1111/jgs.13939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institute of Medicine. Dying in America Improving Quality and Honoring Individual Preferences Near the End of Life The Pressing Need to Improve End-of-Life Care. 2014 [Google Scholar]
- 9.Brennan TA, Leape LL, Laird NM, et al. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. 1991. Qual Saf Health Care. 2004;13(2):145–151. 151–152. doi: 10.1136/qshc.2002.003822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smith AK, Fisher J, Schonberg MA, et al. Am I Doing the Right Thing? Provider Perspectives on Improving Palliative Care in the Emergency Department. Ann Emerg Med. 2009;54(1):86–93. 93. doi: 10.1016/j.annemergmed.2008.08.022. [DOI] [PubMed] [Google Scholar]
- 11.Phongtankuel V, Scherban BA, Reid MC, et al. Why Do Home Hospice Patients Return to the Hospital? A Study of Hospice Provider Perspectives. J Palliat Med. 2016;19(1):51–56. doi: 10.1089/jpm.2015.0178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Evans WG, Cutson TM, Steinhauser KE, Tulsky JA. Is There No Place Like Home? Caregivers Recall Reasons for and Experience upon Transfer from Home Hospice to Inpatient Facilities. J Palliat Med. 2006;9(1):100–110. doi: 10.1089/jpm.2006.9.100. [DOI] [PubMed] [Google Scholar]
- 13.Plotzke M, Christian T, Poznaik E. Medicare Hospice Payment Reform : Analyses to Support Payment Reform. 2014:1–129. [Google Scholar]
- 14.Goldenheim A, Oates D, Parker V, Russell M, Winter M, Silliman RA. Rehospitalization of Older Adults Discharged to Home Hospice Care. J Palliat Med. 2014;17(7):841–844. doi: 10.1089/jpm.2013.0224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Salam-White L, Hirdes JP, Poss JW, Blums J. Predictors of emergency room visits or acute hospital admissions prior to death among hospice palliative care clients in Ontario: a retrospective cohort study. BMC Palliat Care. 2014;13(1):35. doi: 10.1186/1472-684X-13-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inouye SK, Zhang Y, Jones RN, et al. Risk factors for hospitalization among community-dwelling primary care older patients: development and validation of a predictive model. Med Care. 2008;46(7):726–731. doi: 10.1097/MLR.0b013e3181649426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Teno JM, Bowman J, Plotzke M, et al. Characteristics of Hospice Programs with Problematic Live Discharges. J Pain Symptom Manage. 2015 doi: 10.1016/j.jpainsymman.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 18.Cintron A, Hamel MB, Davis RB, Burns RB, Phillips RS, McCarthy EP. Hospitalization of hospice patients with cancer. J Palliat Med. 2003;6(5):757–768. doi: 10.1089/109662103322515266. [DOI] [PubMed] [Google Scholar]
- 19.Dongjie F, Charles EM. CHAS. GMC. Chronic Kidney Disease and the Risks of Death, Cardiovascular Events, and Hospitalization. Nejm. 2004:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 20.Jencks S. Rehospitalizations among Patients in the Medicare Fee-for-Service Program. N Engl J Med. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 21.Kind AJH, Smith MA, Frytak JR, Finch MD. Bouncing back: Patterns and predictors of complicated transitions 30 days after hospitalization for acute ischemic stroke. J Am Geriatr Soc. 2007;55(3):365–373. doi: 10.1111/j.1532-5415.2007.01091.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Callahan CM, Arling G, Tu W, et al. Transitions in care for older adults with and without dementia. J Am Geriatr Soc. 2012;60(5):813–820. doi: 10.1111/j.1532-5415.2012.03905.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Natarajan S, Nietert PJ. Hypertension, diabetes, hypercholesterolemia, and their combinations increased health care utilization and decreased health status. J Clin Epidemiol. 2004;57(9):954–961. doi: 10.1016/j.jclinepi.2004.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Hosmer DW, Jr, Lemeshow S. Applied Logistic Regression. 2000 [Google Scholar]
- 25.Harrell F. Regression coefficients and scoring rules. J Clin Epidemiol. 1996;49(7):819. doi: 10.1016/0895-4356(95)00068-2. [DOI] [PubMed] [Google Scholar]
- 26.Moons KG, Harrell FE, Steyerberg EW. Should scoring rules be based on odds ratios or regression coefficients? J Clin Epidemiol. 2002;55(10):1054–1055. doi: 10.1016/s0895-4356(02)00453-5. [DOI] [PubMed] [Google Scholar]
- 27.Wasson JH, Sox HC, Neff RK, Goldman L. Clinical Prediction Rules. N Engl J Med. 1985;313(13):793–799. doi: 10.1056/NEJM198509263131306. [DOI] [PubMed] [Google Scholar]
- 28.Care E, Wolff JL, Dy SM, Frick KD, Kasper JD. End-of-Life Care: Findings From a National Survey of Informal Caregivers. Arch Intern Med. 2007;167(1):40–46. doi: 10.1001/archinte.167.1.40. [DOI] [PubMed] [Google Scholar]
- 29.Rhee Y, Degenholtz HB, Lo Sasso AT, Emanuel LL. Estimating the Quantity and Economic Value of Family Caregiving for Community-Dwelling Older Persons in the Last Year of Life. J Am Geriatr Soc. 2009;57(9):1654–1659. doi: 10.1111/j.1532-5415.2009.02390.x. [DOI] [PubMed] [Google Scholar]
- 30.Unroe KT, Greiner MA, Johnson KS, Curtis LH, Setoguchi S. Racial differences in hospice use and patterns of care after enrollment in hospice among Medicare beneficiaries with heart failure. Am Heart J. 2012;163(6):987–993. doi: 10.1016/j.ahj.2012.03.006. [DOI] [PubMed] [Google Scholar]
- 31.Teno JM, Bowman J, Plotzke M, et al. Characteristics of Hospice Programs With Problematic Live Discharges. J Pain Symptom Manage. 2015;50(4):548–552. doi: 10.1016/j.jpainsymman.2015.05.001. [DOI] [PubMed] [Google Scholar]
- 32.Wachterman MW, Marcantonio ER, Davis RB, Mccarthy EP. Association of Hospice Agency Profit Status With Patient Diagnosis, Location of Care, and Length of Stay. JAMA. 2014;305(5):472–479. doi: 10.1001/jama.2011.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Casarett D, Harrold J, Harris PS, et al. Does Continuous Hospice Care Help Patients Remain at Home? J Pain Symptom Manage. 2015 doi: 10.1016/j.jpainsymman.2015.04.007. [DOI] [PubMed] [Google Scholar]
- 34.Costa V, Earle CC, Esplen MJ, et al. The determinants of home and nursing home death: a systematic review and meta-analysis. BMC Palliat Care. 2016;15(1):8. doi: 10.1186/s12904-016-0077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]