Abstract
Background:
Pain is the most common problem experienced by hemodialysis patients, especially musculoskeletal pain in lower extremities, which is usually not completely treated and adversely affects their quality of life. The present study was conducted with the aim to determine and compare the effects of topical application of menthol and rosemary for musculoskeletal pain in hemodialysis patients.
Materials and Methods:
The present single-blind clinical trial recruited 105 eligible patients undergoing hemodialysis in selected hospitals affiliated to Isfahan University of Medical Sciences; patients were selected by convenient sampling. Participants’ severity of pain was determined prior to intervention. They were then randomly divided into rosemary, menthol, and placebo groups. All three groups applied medication on the site of pain on their legs three times a day for three days and recorded the severity of pain four hours after morning and afternoon applications. The statistical analysis of data was performed using SPSS 18.
Results:
The mean score of severity of pain before the intervention was not significantly different among the three groups (p = 0.83), but it became significantly different after intervention (p = 0.001). Significant differences were observed in mean severity of pain before and after intervention in rosemary and menthol groups (p < 0.001), but not in the placebo group (p = 0.21).
Conclusions:
Topical application of menthol and rosemary can alleviate severity and frequency of recurrence of musculoskeletal pain in hemodialysis patients; however, according to the results of the study, none had precedence over the other.
Keywords: Hemodialysis, Iran, menthol, pain, rosemary
Introduction
Pain is one of the most prevalent problems among patients undergoing hemodialysis.[1] It has been reported that 54% of these patients suffer from pain.[2] This pain may be due to polycystic kidney disease, chronic kidney failure (renal osteodystrophy and vascular calcification), high urea, or its accompanying diseases such as diabetes, arthritis, and cardiovascular disease (CVD).[3] Moreover, the source of 64% of pain these patients experience is due to musculoskeletal issues and it is experienced in the legs.[4] The intensity of this pain ranges from medium to high.[5]
The experience of chronic pain has negative effects on patients; the resulting immobility causes high prevalence of depression, irritability, inability to cope with stress, increased fatigue, and reduced life satisfaction.[6] Chronic pain affects different body systems such as the endocrine system and causes an increase in the antidiuretic hormone (ADH), adrenocorticotropic hormone (ACTH), cortisol, epinephrine, norepinephrine (NE), catecholamines (CA), renin, angiotensin II, aldosterone, and glucagon, and reduces insulin.[7] Furthermore, by affecting the cardiovascular system, it increases the heart rate, cardiac workload, peripheral and systemic vascular resistance, myocardial oxygen consumption, and coronary vascular resistance.[7] On the other hand, lack of pain management results in an increase in the number of referrals to health centers and duration of hospitalization.[6] In addition, pain negatively affects different aspects of quality of life (QOL) including physical activity, social performance, emotional functioning, daily activities, and energy level.[4]
Usually, pain in these patients, despite its chronicity, is not completely treated. A cohort study on Canadian patients undergoing hemodialysis showed that pain had not been effectively controlled in 75% of cases.[5] Pain management is one of the most important responsibilities of the nursing profession. Pain relief is achieved through pharmaceutical and non-pharmaceutical methods. Since the use of chemical medication in patients with impaired kidney function causes many complications, more reliable drugs with fewer side effects are required.[8] Herbal medicines have been used for pain relief since thousands of years,[9] and researchers have emphasized their accessibility, diversity, public acceptance, simple technology, fewer side effects, and economic efficiency.[10]
Menthol is a topical analgesic that constitutes 30–70% of peppermint essential oil[11] and is effective in the treatment of mild pain and musculoskeletal pain. Its topical application activates transient receptor potential melastatin 8 (TRPM8) and induces a sensation of coolness at the site of application, and thus, it inhibits afferent neurons and spinal dorsal horn, which guides pain impulses from the site to the thalamus.[12] Moreover, menthol increases local blood flow through the dilation of blood vessels.[13] Another herbal medication used in traditional medicine as an analgesic is rosemary.[14] Rosemary oil has pharmacological analgesic[15] and antagonistic effects on inflammatory factors such as prostaglandins (PG).[16] Rosemary also improves blood flow through the dilation of blood vessels.[17]
Some studies on the effects of rosemary essence on pain relief have reported a significant reduction in pain intensity.[18,19,20] Many studies have also been conducted on the effects of menthol on pain due to different diseases and the results of some have suggested its positive effects on the reduction of pain intensity.[12,21,22] However, some studies found that menthol had no effect on the reduction of pain.[23]
The cause of pain varies among patients with chronic kidney failure undergoing hemodialysis. Therefore, there is uncertainty as to whether these two herbal medicines can control musculoskeletal pain among these patients. Hence, the present study was conducted to determine and compare the effect of topical use of menthol and rosemary for musculoskeletal pain in patients undergoing hemodialysis.
Materials and Methods
The study was undertaken in Khorshid Hospital and Amin Hospital of Isfahan and Emam Khomeini Hospital of Falavarjan, Iran. The present study was a single-blind (subjects) clinical trial (IRCT2016101430296N1) with three groups. Sampling was performed in March and April 2016. Sample volume, in the confidence interval of 95% and power of 80%, was calculated as 32 individuals in each group. With the consideration of 10% sample loss, 35 subjects were placed in each group [Diagram 1]. Thus, the study comprised 105 patients with chronic kidney failure undergoing three sessions of hemodialysis per week. Age range was 18–65 years and a permanent and active health record in the hemodialysis ward, and were conscious.[24] Other inclusion criteria included lack of a history of diagnosed musculoskeletal disorders (MSDs), candidacy for transplantation during the study, drug use,[25] skin damage, such as skin rash or wound, at the site of drug administration,[26] capability of verbal communication, lack of any physical, auditory, and visual defects, the passage of at least 3 months since the beginning of hemodialysis, being literate, and a pain intensity score in the lower extremities of at least 4. The subjects were selected through convenience sampling. The participants could leave the study at any stage due to unwillingness to continue or hospitalization; however, all subjects remained in the study until the end. The data collection tools consisted of a demographic characteristics questionnaire and the 10-point Pain Intensity Numerical Rating Scale (PI-NRS). The reliability of the PI-NRS was evaluated by Farrar et al. through test-retest method (r = 0.83) between two stages, and its validity was obtained through content validity.[27] In Iran, the reliability of this scale was evaluated by Yaghouby et al. using the Pearson correlation coefficient between two stages (r = 0.96).[28]
Diagram 1.
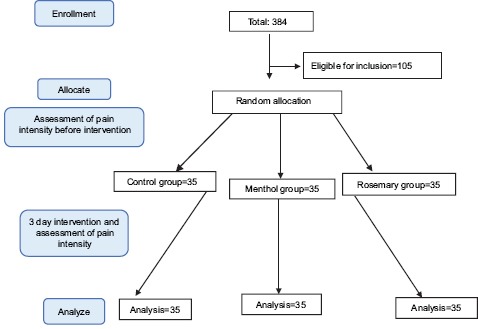
Consort chart
Demographic characteristics including age, sex, duration of hemodialysis treatment, and the cause of kidney failure were obtained from the patients’ health records and written in the questionnaire. Pre-intervention pain intensity was determined using the PI-NRS. The subjects were selected based on the inclusion criteria and consent forms were obtained from all participants. Then, using the table of random numbers, 35 individuals were randomly allocated to each group [5% menthol drop, rosemary spray, and placebo groups (hygienic Vaseline ointment)]. Before the intervention, the existence of any allergies was determined in all participants. The medication used in each group was placed on the inside of the upper arm without vascular access, and after 24 hours, its status in terms of allergic symptoms, such as itchiness, irritation, redness, rash, and a burning sensation, was determined. In case of lack of any allergic reactions, the medication, based on the group of the participant, and the PI-NRS form, to determine pain intensity, frequency of analgesics use, incidence of allergies, and recurrence of pain, were distributed among the subjects. The dosage, method of use on the site of pain, and the frequency of use of the medication were verbally explained to subjects. An instruction booklet and the researcher's phone number, in case of emergencies such as observation of allergic symptoms, were also provided for each participant.
Since the present study was a single-blind trial, the patients received no information regarding the name of the medication (the patient was only told that this medication was for pain relief in the legs), and sprays, drops, and ointments were distributed in containers without names or information. The rosemary, menthol, and placebo groups used 2 puffs of rosemary spray, 10 drops of menthol, and Vaseline ointment, respectively, three times a day (morning, noon, and night) for three consecutive days at the site of pain on the legs. The participants evaluated their pain intensity using the PI-NRS and recorded the result in the questionnaire 4 hours after medication use in the morning and noon. They completed the other sections of the questionnaire (analgesics use, and pain or allergy incidence) once a day. During the study, the researcher followed up on the use of medication by the participants through phone calls and visiting the dialysis wards. After the intervention, the completed questionnaires were collected and the collected data were analyzed using Chi-squared test, one-way ANOVA, and paired t-test in SPSS software (version 18, SPSS Inc., Chicago, IL, USA).
Ethical considerations
Consent forms were obtained from the participants after explaining the study goals to them, and explaining that the study involved no additional costs and that they could leave the study at any stage. They were also assured of the confidentiality of their information. The results of the study were provided for any subjects who wished to have them.
Results
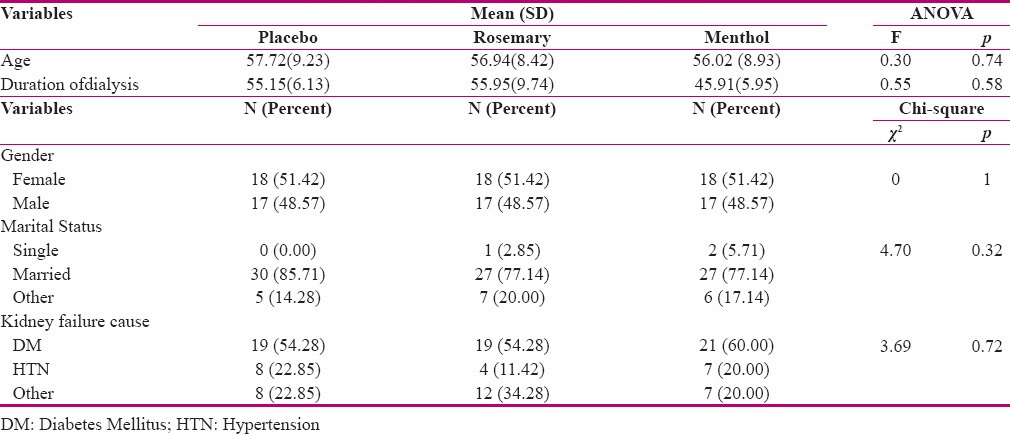
In the present study, 105 patients undergoing hemodialysis qualifying the inclusion criteria participated. Since none of the participants had allergic reactions to the medications used and they were all willing to take part in the study, all subjects completed the study. Mean age of the participants was 56.89 (8.86) years and mean duration of their hemodialysis treatment was 52.33 (7.27) months. Among the participants, 51.42% were women and 48.57% were men; 2.85% were single, 83.16% were married, and 13.86% were divorcees or widowers. The highest prevalence of cause of kidney failure was related to diabetes (56.19%) and hypertension (18.09%) [Table 1].
Table 1.
Demographic and disease characteristics
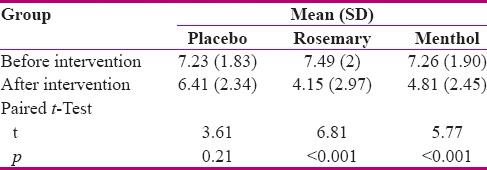
One-way ANOVA results showed no statistically significant difference between the groups in terms of pain intensity before the intervention (p = 0.83), but showed a significant difference between the groups after the intervention (p = 0.001) [Table 2]. Paired t-test showed that the mean pain intensity score of the rosemary and menthol groups were significantly lower after the intervention compared to before the intervention (p < 0.001). However, in the placebo group, this difference was not significant (p = 0.21) [Table 3].
Table 2.
Mean score of severity of pain in participants before and after intervention
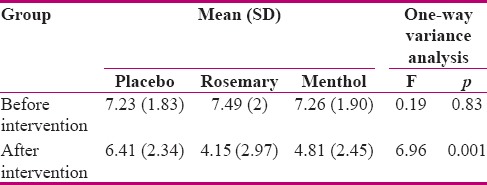
Table 3.
Mean score of severity of pain in three groups of patient before and after intervention
The results of one-way ANOVA also showed a significant difference in mean variation in pain intensity after the intervention compared to before the intervention in the three groups (p < 0.001). Mean variation in pain intensity in the placebo group was significantly lower than the rosemary (p < 0.001) and menthol groups (p = 0.005). However, no significant difference was observed between the menthol and rosemary groups in this regard (p = 0.115). One-way ANOVA showed no significant difference in mean analgesic use between the groups during the 3 days of intervention (p > 0.05). Nevertheless, Chi-squared test showed that pain incidence was significantly higher in the placebo group compared to the other groups on each day of the intervention (p < 0.001).
Discussion
The present study was conducted in order to determine and compare the effects of the topical use of menthol and rosemary for musculoskeletal pain in the legs among patients undergoing hemodialysis. The results showed no significant difference in mean pain intensity score before the intervention in the three groups. In other words, it approved the random allocation of the participants to the groups. Nonetheless, there was a significant difference in mean pain intensity in the three groups after the intervention; mean pain intensity was lower in the menthol and rosemary groups after the intervention compared to before the intervention. Ghannadi et al. studied the effects of the topical application of the combination of rosemary and lavender on pain in patients with knee osteoarthritis (OA).[18] They found that mean pain intensity of patients significantly decreased in weeks 4, 8, and 12 of the study compared to the beginning of the study.[18] In addition, Jung-Hee et al. studied the effects of aromatherapy with lavender, rosemary, and rose oil on headache, anxiety, and cortisol level among middle-aged women and found a higher reduction in mean pain intensity in the experimental group compared to the control group.[19] Gedney et al. studied the impact of aromatherapy with two essential oils (lavender and rosemary) on emotional and sensory responses of induced pain and reported a reduction in pain intensity as a result of this treatment.[20] The results of all of these studies were in agreement with that of the present study.
Therefore, the use of rosemary essence is effective on the reduction of pain intensity. 1,8-cineol, as the main natural component in rosemary essence, can inhibit the formation of the inflammatory mediators of prostaglandins, leukotrienes, and cytokines in laboratory environment. Thus, it seems that it has presented significant analgesic and anti-inflammatory effects in the present study.
Atashzadeh et al. compared the effects of massage with menthol with that of sweet almond oil on pain intensity among patients with multiple sclerosis (MS).[21] The results of their study suggested that mean pain intensity after the intervention in the two groups had significantly decreased compared to before the intervention; however, this reduction was higher in the menthol group.[21] Topp et al. compared the effect of topical application of menthol and placebo on function and pain in the knee among patients with OA.[22] They reported that menthol decreased pain intensity in these patients during the studied activities compared to placebo.[22] Sundstrup et al. evaluated the impact of the topical application of menthol on pain in slaughterhouse workers with carpal tunnel syndrome (CTS). They reported a 31% reduction in pain due to CTS.[12]
Yosipovitch et al. studied the effects of the topical application of menthol on itchiness, pain, warmth, and the biophysical characteristics of skin. However, the results of their study showed that although menthol is a strong stimulant of the skin compared to alcohol, it was not more effective than alcohol in the reduction of pain and itchiness.[29] This difference with the results of the present study seems to be due to the difference in the concentration of menthol used in the two studies. Vase et al. assessed the effect of menthol on phantom pain among patients who had undergone upper limb amputation with varying pain intensities.[23] They reported an increase in pain intensity among these patients (p = 0.011).[23] The difference between the results of this study and that of the present study may be due to the difference in the type of pain studied (phantom pain vs. musculoskeletal pain).
Menthol reduces pain through the stimulation of the TRPM8, blocking of calcium channels of nerves, inhibition of voltage-gated sodium channels in the dorsal horn, dilation of blood vessels, and increasing of local blood flow. Lack of transmission of pain signals is a factor which causes the reduction in pain after the application of menthol and is approved by the results of the present study.
The limitations of the present study were the lack of direct supervision of the researcher on all stages of data collection and the short duration of the intervention due the limited time allocated to the thesis. Therefore, it is recommended that in future studies the intervention be performed for a longer period of time.
Conclusion
The prevalence and intensity of pain, especially musculoskeletal pain, is high among patients undergoing hemodialysis, and they also have a high rate of medication intake as a substitute for the loss of functioning of the kidney. Thus, relieving pain with the use of medication and methods with fewer side effects and complications is essential among these patients. Hence, the present study was conducted in this regard and showed that the topical use of menthol and rosemary reduces musculoskeletal pain intensity in the legs among patients undergoing hemodialysis.
Financial support and sponsorship
Isfahan University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
This article was derived from the master thesis with project number 394968, Isfahan University of Medical Sciences, Isfahan, Iran. The authors thank the managers and patients participating in the study. We appreciate the Clinical Research Development Center of Khorshid, Amin, and Emam Khomeini Falavarjan hospitals.
References
- 1.Ozdemir G, Ovayolu N, Ovayolu O. The effect of reflexology applied on haemodialysis patients with fatigue, pain and cramps. Int J Nurs Pract. 2013;19:265–73. doi: 10.1111/ijn.12066. [DOI] [PubMed] [Google Scholar]
- 2.Masajtis Zagajewska A, Pietrasik P, Krawczyk J, Krakowska M, Jarzebski T, Pietrasiewicz B, et al. Similar prevalence but different characteristics of pain in kidney transplant recipients and chronic hemodialysis patients. Clinical transpl ntation. 2011;25:144–51. doi: 10.1111/j.1399-0012.2010.01359.x. [DOI] [PubMed] [Google Scholar]
- 3.Glick N, Davison SN. Managing chronic pain in advanced chronic kidney disease. US. Nephrology. 2011;6:21–8. [Google Scholar]
- 4.Gamondi C, Galli N, Schonholzer C, Marone C, Zwahlen H, Gabutti L, et al. Frequency and severity of pain and symptom distress among patients with chronic kidney disease receiving dialysis. Swiss Med Wkly. 2013;143:w13750. doi: 10.4414/smw.2013.13750. [DOI] [PubMed] [Google Scholar]
- 5.Upadhyay C, Cameron K, Murphy L, Battistella M. Measuring pain in patients undergoing hemodialysis: A review of pain assessment tools. Clin Kidney J. 2014;7:367–72. doi: 10.1093/ckj/sfu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Davison SN, Jhangri GS. Impact of pain and symptom burden on the health-related quality of life of hemodialysis patients. J Pain Symptom Manage. 2010;39:477–85. doi: 10.1016/j.jpainsymman.2009.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Pasero C, McCaffery M. Pain assessment and pharmacologic managment. St. Louis: Moseby-Elisevier; 2011. p. 13. [Google Scholar]
- 8.Ghods A, Abfroosh N, Ghorbani R, Asgari M. Effect of lavender inhallation on pain intensity during insertion of vascular needles in hemodialysis patients. Journal of Babol University of Medical Sciences. 2014;16:7–14. [Google Scholar]
- 9.Martinez AL, Gonzalaz Trujano ME, Chavez M, Pellice F. Antinociceptive effectiveness of triterpenes from rosemary in visceral nociception. J Ethnopharmacol. 2012;142:28–34. doi: 10.1016/j.jep.2012.03.052. [DOI] [PubMed] [Google Scholar]
- 10.Payyappallimana U. Role of traditional medicine in primary health care: An overview of perspectives and challenges. Yokohama Journal Social Sciences. 2009;14:57–77. [Google Scholar]
- 11.Nouraldini M, Noureddin M, Salami M, Mesdaghinia AR, Verdi J, Salimian M. A study of analgesic effects of aqueous extract of menthe spicata in Rats. Feyz Journal. 2007;10:19–23. [Google Scholar]
- 12.Sundstrup E, Jakobsen MD, Brandt M, Jay K, Colado JC, Wang Y, et al. Acute effect of topical menthol on chronic Pain in slaughterhouse workers with carpal tunnel syndrome: Triple-blind, randomized placebo-controlled trial. Rehabil Res Pract. 2014;2014:310913. doi: 10.1155/2014/310913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Higashi Y, Kiuchi T, Furuta K. Efficacy and safety profile of a topical methyl salicylate and menthol patch in adult patients with mild to moderate muscle strain: A randomized, double-blind parallel-group, placebo-controlled multicenter study. Clin Ther. 2010;32:34–43. doi: 10.1016/j.clinthera.2010.01.016. [DOI] [PubMed] [Google Scholar]
- 14.Zhang A, Sun H, Wang X. Recent advances in natural products from plants for treatment of liver diseases. Eur J Med Chem. 2013;63:570–7. doi: 10.1016/j.ejmech.2012.12.062. [DOI] [PubMed] [Google Scholar]
- 15.Takaki I, Bersani Amado LE, Vendruscolo A, Sartoretto SM, Diniz SP, Bersani Amado CA, et al. Anti-inflammatory and antinociceptive effects of rosmarinus officinalis L. essential oil in experimental animal models. J Med Food. 2008;11:741–6. doi: 10.1089/jmf.2007.0524. [DOI] [PubMed] [Google Scholar]
- 16.Faria LR, Lima CS, Perazzo FF, Carvalho JC. Anti inflammatory and antinociceptive activities of essential oil from Rosmarinus officinalis L (Lamiaceae) International Journal of Pharmaceutical Sciences Review and Research. 2011;7:1–8. [Google Scholar]
- 17.Solhi H, Salehi B, Alimoradian A, Pazouki S, Kazemifar AM, Taghizadeh M, et al. Beneficial effects of rosmarinus officinalis for treatment of opium withdrawal syndrome during addiction treatment programs: A clinical trial. Addict Health. 2013;5:90–4. [PMC free article] [PubMed] [Google Scholar]
- 18.Ghannadi A, Karimzadeh H, Tavakoli N, Darafsh M, Ramezanloo P. Efficacy of a combined Rosemary and Lavender Topical ointment in the Treatment of patient with osteoarthritis of the knee. Zahedan Journal of Research in Medical Sciences. 2013;15:23–9. [Google Scholar]
- 19.Jung- Hee C, Myung Ja K, Hee Seung K, Yeong In K. Effects of aromatherapy in blending oil of basil, lavender, rosemary, and rose on headache, anxiety and serum cortisol level in the middle-aged women. Journal Browse. 2010;12:133–9. [Google Scholar]
- 20.Gedney JJ, Glover TL, Fillingim RB. Sensory and affective Pain discrimination after Inhalation of Essential Oils. Psychosom Med. 2004;66:599–606. doi: 10.1097/01.psy.0000132875.01986.47. [DOI] [PubMed] [Google Scholar]
- 21.Atashzadeh Shorideh F, Mohammadi SH, Abed Saeedi ZH, Alavi Majd H. Effect of aromatherapy and massage on pain of patient with multiple sclerosis. Journal of Shahid Beheshti School of Nursing & Midwifery. 2007;17:28–32. [Google Scholar]
- 22.Topp R, Brosky JA, Pieschel D. The Effect of either topical menthol or a placebo on functioning and knee Pain among patients with knee OA. Journal of Geriatric Physical Therapy. 2012;36:92–9. doi: 10.1519/JPT.0b013e318268dde1. [DOI] [PubMed] [Google Scholar]
- 23.Vase L, Svensson P, Nikolajsen L, Arendt-Nielsen L, Jensen TS. The effects of menthol on cold allodynia and wind-up-like pain in upper limb amputees with different levels of phantom limb pain. Neurosci Lett. 2013;553:42–57. doi: 10.1016/j.neulet.2012.11.005. [DOI] [PubMed] [Google Scholar]
- 24.Baloochi Beydokhti T, Kianmehr M, Tavakolizadeh J, Basiri Moghadam M, Biabani F. Effect of muscle relaxation on hemodialysis patients’ pain. Quarterly of the Horizon of Medical Sciences. 2015;21:75–80. [Google Scholar]
- 25.Bagheri Nesami M, Espahbodi F, Nikkhah A, Shorofi SA, Yazdani Charati J. The effects of lavender aromatherapy on pain following needle insertion into a fistula in hemodialysis patients. Complement Ther Clin Pract. 2014;20:1–4. doi: 10.1016/j.ctcp.2013.11.005. [DOI] [PubMed] [Google Scholar]
- 26.Begum A, Sandhya S, Ali SS, Vinod KR, Reddy S, Banji D. An in-depth review on the medicinal flora Rosmarinus officinalis (Lamiaceae) Acta Sci Pol Technol Aliment. 2013;12:61–73. [PubMed] [Google Scholar]
- 27.Farrar JT, Troxel AB, Stott C, Duncombe P, Jensen MP. Validity, reliability and Clinical importance of change in a 0-10 numeric rating measure of spasticity: A Post hoc analysis of a randomize double -blind placebo controlled trial. Clin Ther. 2008;30:974–85. doi: 10.1016/j.clinthera.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 28.Yaghobi M, Amini k, Fathi M, Ahmadi F, Mohamadi I, Salehnejad GH. Effects of massage on pain due to cramp muscle during hemodialysis. Scientific Journal of Ilam University of Medical Sciences. 2008;17:1–8. [Google Scholar]
- 29.Yosipovitch G, Szolar C, Hui XY, Maibach H. Effect of topically applied menthol on thermal, pain and itch sensations and biophysical properties of the skin. Arch Dermatol Res. 1996;288:245–8. doi: 10.1007/BF02530092. [DOI] [PubMed] [Google Scholar]


