Abstract
Background:
Providing intubated patients admitted to the intensive care units with oral healthcare is one of the main tasks of nurses in order to prevent Ventilator-Associated Pneumonia (VAP). This study aimed at comparing the effects of two mouthwash solutions (echinacea and chlorhexidine) on the oral microbial flora of patients hospitalized in the intensive care units.
Materials and Methods:
In this clinical trial, 70 patients aged between18 and 65 years undergoing tracheal intubation through the mouth in three hospitals in Arak, were selected using simple random sampling and were randomly divided into two groups: the intervention group and the control group. The oral health checklist was used to collect the data (before and after the intervention). The samples were obtained from the orally intubated patients and were then cultured in selective media. Afterwards, the aerobic microbial growth was investigated in all culture media. The data were analyzed using SPSS software.
Results:
The microbial flora in the echinacea group significantly decreased after the intervention (p < 0.0001) and it was also the case withmicrobial flora of the patients in the chlorhexidine group (p < 0.001). After 4 days, the oral microbial flora of the patients in the intervention group was lower than that of the patients in the control group (p < 0.001).
Conclusions:
The results showed that the echinacea solution was more effective in decreasing the oral microbial flora of patients in the intensive care unit. Given the benefits of the components of the herb Echinacea, it can be suggested as a viable alternative to chlorhexidine.
Keywords: Chlorhexidine, Echinacea, intensive care units, Iran, oral hygiene
Introduction
Ventilator-Associated Pneumonia (VAP) is a common bacterial nosocomial infection, which is most prevalent among the patients in Medical Surgical Intensive Care Units (MSICUs).[1] Comatose patients undergoing artificial ventilation are at high risk for pneumonia due to oral plaque formation and the fact that the mouth is open for a long time period.[2,3,4,5] In acutely ill patients, especially those hospitalized in the ICUs, normal oral flora significantly tends to contain gram-negative bacilli and Staphylococcus aureus.[6] Studies have shown that during the first 24 hours after the admission to the ICU, pathogenic bacteria colonize in the mouth.[3,4,5,6,7] When critically ill patients are intubated, normal flora of the mouth is quickly converted into pathogens that are responsible for VAP.[8] It has been found that the number of organisms in the mouth increases from the first to fourth day and remains high up to the seventh day.[9] The risk of nosocomial pneumonia and mortality rate in ventilated patients is higher than that in other patients.[4,10,11] These infections also impose economic costs and increase length of stay in the hospital. To avoid this infection, using anti-bacterial mouthwash solutions has been recommended as the most important strategy for preventing VAP.
One of the compounds that has been recently proposed as a mouthwash is Echinacea extract. In the US, echinacea is commonly marketed alone or in combination with other herbs to strengthen the immune system and in turn to prevent or treat colds.[12] Although the mechanism by which this plant exerts its effects is not exactly clear, a significant increase in phagocytic activity was observed when using echinacea.[13,14] Chemical components of echinacea species include lipophilic ones (i.e., alkamides and polyacetylenes), water-soluble polysaccharides, caffeic acid derivatives (i.e., echinacoside, chicoric acid, and coffeic acid), and flavonoids.[14] Echinacea's polysaccharides have the property of stimulating the immune system and its polyacetylenes have anti-inflammatory effects.[15] Echinacea components increase the number of white blood cells in circulation, activate T lymphocytes, enhancephagocytosis, stimulate production of cytokines (interferon, tumor necrosis factor, interleukin-1, and interleukin-6), inhibit hyaluronidase, and stimulate the adrenal cortex and the alternative pathway of the complement system.[7,12,13,16] The German Commission E (translated by the American Botanical Society) has approved the oral use of Echinacea purpurea (i.e., the above-ground parts) for colds, respiratory tract infections, and urinary tract infections, and its topical use for poorly healing wounds.[17] Among available mouthwashes, chlorhexidine has been shown to be highly effective in reducing dental plaques and pathogenic microorganisms including streptococcus mutans. Nowadays, in most studies on mouthwashes, chlorhexidine is used as a positive control to the aim of comparing the efficacy of other products, as it is believed that chlorhexidine is a gold standard.[18,19,20] However, the incidence of side effects such as undesirable tooth discoloration, unpleasant taste, dryness, and burning sensation in the mouth discourages patients to use this mouthwash.[21,22,23] Given the advantages of herbal compounds and their fewer side effects compared to their chemical counterparts and at the same time considering the fact that the effect of this drug has not been evaluated on the patients undergoing tracheal intubation, the present study was conducted to compare the efficacy of echinacea and that of chlorhexidine on the oral microbial flora of the patients undergoing tracheal intubation.
Materials and Methods
This study was a double-blind, randomized, clinical trial comparing the efficacy of two mouthwash solutions (echinacea and chlorhexidine) on the oral microbial flora of the intubated patients admitted to the ICUs. It was registered in the Iranian Registry of Clinical Trial (IRCT2012092610942N1). In this study, 70 intubated patients admitted to the intensive care units from April to October 2014 in three hospitals in Arak, Iran (Vali-e-Asr, Amir-al-Momenin, and Ghods) were selected through purposive sampling and then were randomly divided into two groups: the intervention group (n = 35) and the control group (n = 35). According to the data from previous studies, considering P1 = 5%, P0 = 25%, 1-α = 95%, and Power = 80%, the sample size for the present study was calculated as 35 patients in each group.[3,9]
Care in the form of using mouthwash was provided using echinacea mouthwash 0.01%[24] in the intervention group and chlorhexidine 0.2% in the control group as 15 ml twice a day for each group. Method, timing, and frequency of using mouthwash were the same for both groups. Also, rinsing with normal saline and suctioning secretions was performed every 2–3 hours for both groups of patients. This was the routine care provided to the patients in the ICU. Due to the existence of different wards and large number of nurses who provided their patients with care, the researchers taught mouthwash use and oral care methods to all co-researchers in a training program and they were asked to perform oral care on the basis of the written protocol given to them.
As the first step, demographic data, history and the cause of hospitalization, and drugs and medications required for the patients were recorded. Next, 50 μl of the aspirated secretions (before and after the intervention) was collected from the posterior part of the mouth (oropharyngeal region) of each patient by a lab technician using a pipette and this sample's volume was adjusted to 1 ml with normal saline. Immediately, 10 μl of this solution was transferred to a Blood agar plate and incubated overnight at 37°C. Then, the number of aerobic bacteria was counted based on cfu/ml (colony-forming units per ml). Nurses and lab technicians were not aware of the groups to which the patients belonged. The first samples for oral cultures (pre-test) were obtained within 12 hours after the admission (for each patient in both groups) and the next samples were collected every 12 hours during the intervention. Finally, the samples for the last culture (post-test) were collected exactly 4 days after the last intervention.
Before performing oral care, in order to ensure suitable limb occlusion pressure, thecuff pressure was regulated using a proper manometer (20–25 mm Hg). All areas of the mouth, both internal and external surfaces of the teeth, gums, and tongue were brushed (the movement from back to front) twice a day using kids’toothbrushes. Before and after brushing each section of the mouth, mouthwash solution was poured on the same area by a special syringe and was suctioned in less than 30 seconds.[25] In patients with an airway, it was removed, cleaned, and placed in the mouth again. Mouthwash solution used for the patients in the intervention group was echinacea solution and chlorhexidine solution was used in the control group as 15 cc twice a day employing kids’ soft toothbrushes. In addition, rinsing with normal saline and oral suction in all patients were done every 2–3 hours according to standard protocols. Before each toothbrushing, all areas of the patient's mouth were checked using the flashlight for any clots, sores, redness, and bleeding tissues, and the items were recorded. In case of any injury, the doctor was informed and if any other treatments were needed, suitable proceedings were conducted following the physician order.[26] To prepare echinacea solution 1%, the dried herb was soaked in water for 60 hours, filtered, and maintained at 40–44°C for its solvent to be evaporated. Finally, a solution containing 95 g dried herb per ml was obtained and used.[27] The data were analyzed using SPSS version 20 (version 20, SPSS Inc., Chicago, IL). For all statistical analyses, significance levels were set as P value <0.05. To analyze the quantitative variables, Chi-square test, Fisher exact test, independent t-test, and Friedman test were used.
Ethical considerations
The Vice Chancellor for Research and Technology of Arak University of Medical Sciences approved the study (91-126-5), and the informed consents were obtained from all patients’ companions at the beginning of the study.
Results
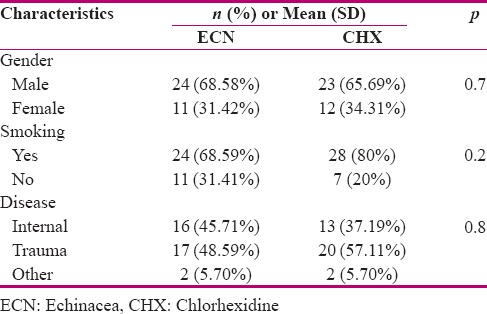
The majority of the patients were male (67.1%), with no history of smoking (74.2%), and with an average age of 44.9 years. Trauma was the most common reported cause of hospitalization (52.8%). Chi-square test was used to investigate the difference between the two groups in terms of sex and smoking. The results [Table 1] showed that before the intervention, there was nosignificant difference between the two groups in terms of age, sex, smoking history, illness, hospital, systolic and diastolic blood pressure, respiratory rate, heart rate, and the number of teeth, (p > 0. 05). To investigate the differences between the two groups in terms of age, systolic and diastolic blood pressure, heart rate, respiratory rate, and the number of teeth, Mann–Whitney U test was used [Table 1] for Kolmogorov–Smirnov test did not find a normal distribution.
Table 1.
Demographic characteristics of the control and intervention groups
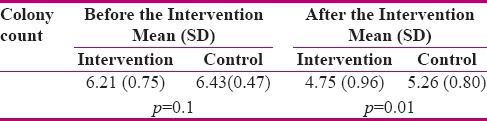
To compare the total microbial flora counts of the patients in the intervention and control groups, independent t-test was used. Although the microbial count is lower in the intervention group 6.2 (0.75) than that in the control group 6.43 (0.47), according to p = 0.1, there is no significant difference between them. (Descriptive statistics of the base-10 log data conversion has been obtained). In other words, bacterial counts were not significantly different among the patients before the intervention. The mean and standard deviation of the patients’ oral microbial flora in the intervention and control groups 4 days after admission were 4.75 (96) and 5.26 (0.8), respectively (Descriptive statistics of the base-10log data conversion have been obtained) [Table 2]. Comparing the mean and standard deviation of the patients’oral microbial flora in the intervention and control groups 4 days after admission using independent t-test showed that the difference was significant (p = 0.01) [Table 2]. In other words, the microbial flora of the patients in the echinacea group (after the intervention) is lower than that of the chlorhexidine group.
Table 2.
Comparing the intervention and control groups before and after the intervention
Discussion
Oropharyngeal region is the main site of colonization of bacteria in the upper respiratory tract.[28] Patients in the intensive care units are experiencing growth and proliferation of bacteria in the pharyngeal mucosa for various reasons, such as epithelial damage and mucosal lesions, reduced immunoglobulin A in saliva, reduced production of saliva, as well as mechanical damage caused by endotracheal intubation and nasogastric tubes.[28] Bacteriological studies have shownthat some patients during hospitalization acquirehospital pathogens such as methicillin-resistant Staphylococcus aureus, Enterobacter Aerogenes, and Acinetobacter Baumannii. The results showed that the standard oral care in the ICU is insufficient for controlling plaques and oral infections caused by nosocomial pathogens.[28]
Fourrier believes that the use of antibacterial materials can reduce the number of pathogenic bacteria in the oral cavity and the irentrance into the trachea. Thus, use of disinfectants reduces the rate of hospital-acquired pneumonia three times. Therefore, employing different approaches to reduction of bacterial pollution in oral cavity of the patients was associated with a reduction of nosocomial infection.[27] Maozhen believes that the lungs and lower airways are sterile and microbes may enter the lower airways through inhalation, but respiratory tract infection occurs most importantly through aspiration of oropharyngeal secretions.[29] Actually, the placement of an endotracheal tube can facilitate micro-aspiration of the pharynx secretions into the lungs and lower airways. Hence, it is recommended that oral care and use of mouthwash solutions, especially Chlorhexidine, be started immediately after intubation.[30] Scannapieco et al. suggest that microorganisms in the digestive system and oropharyngeal region are two main sources for pneumonia in intubated patients and play a key role in the pathogenesis of pneumonia.[30]
Most of the studies recommend chlorhexidine solution to disinfect the oral cavity. Efficiency and benefits of chlorhexidine mouthwash compared to other solutions have been approved, especially in critically ill patients admitted to the ICU. However, there are documents that have raised doubts about the effectiveness of this mouthwash solution. Several studies have investigated the effect of chlorhexidine on the microbial flora or prevention of ventilator-associated pneumonia in patients admitted to the intensive care units, providing different results. In 2006, a study by Ranjbar et al. was conducted on 80 ICU patients. In this study, the effect of chlorhexidine 0.2% on prevention of late VAP was compared with that of normal saline. The results showed that although there was no difference between the two groups in the case of early pneumonia, late VAP in the Chlorhexidine group was lower than that of normal saline (p < 0.05).[31] According to Fourrier (2000), although colonization was lower in the group using chlorhexidine than that in the other group using bicarbonate, the difference was not significant.[27] Similar results were found in another study by Fourrierin (2005).[32]
In addition, the result of Grap (2004) revealed that there was a decrease in colonization of pathogens in the oropharyngeal area after using chlorhexidine in the intervention group compared to the control group; however, the difference was not significant.[29] In a study conducted in 2011 by Barry, the effects of three mouthwashes (sterile water, sodium bicarbonate, and chlorhexidine 0.2%) were assessed on the risk of VAP in patients on ventilators. Kids’ toothbrushes were also used in this study three times a day. The culture results showed no difference between the groups. In other words, the type of mouthwash solution had no effect on the oral microbial contamination.[31] Bírošová also reported antimicrobial and antimutagenic activities for echinacea extract.[33] The echinacea extract obtained from Echinacea purpurea L. has been extensively used as a medicine.[34] The antimicrobial property of this compound has been also proved. For instance, Stanisavlijevic et al. showed that echinacea extract can prevent the growth of Candida albicans and Saccharomyces cerevisiae, but has no effect on the growth of Aspergillus niger.[35]
As the oral flora of the patients in the intervention and control groups were same at baseline, the significant difference between the microbial loads of these two groups after the intervention can show that echinacea was more effective in disinfecting and reducing microorganisms of oropharyngeal region. Although echinacea decreased the number of microorganisms, more studies are needed to determine its effect on the microorganisms responsible for VAP, in particular its role in preventing VAP. It is worth mentioning that no impact study has been done so far on the use of echinacea as a mouthwash solution in patients undergoing tracheal intubation; but it seems that this solution can improve the oral health of patients. This study had some limitations. There was no relationship between the duration of intubation and severity and type of microbial contamination in this study, which may be due to the small sample size. On the other hand, one of the contributing factors in bacterial biofilm formation was the type and number of intravenous antibiotics which could affect the study results.
Conclusion
Based on the findings of this study, echinacea can be used as a suitable mouthwash with minor complications. Further studies on the subject are recommended.
Financial support and sponsorship
Arak University of Medical Sciences.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
This article was derived from MSc thesis. The authors wish to thank the Research Deputy of Arak University of Medical Sciences, which approved and financially supported this project (No. 750).
References
- 1.Kalanuria AA, Zai W, Mirski M. Ventilator-associated pneumonia in the ICU. Crit Care. 2014;18:208. doi: 10.1186/cc13775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abidia RF. Oral care in the intensive care unit: A review. J Contemp Dent Pract. 2007;8:76–82. [PubMed] [Google Scholar]
- 3.Garcia R, Jendresky LC. Reduction of microbial colonization in the oropharynx and dental plaque reduces ventilator-associated pneumonia. American Journal of Infection. 2004:32. [Google Scholar]
- 4.Hutchins K, Karras G, Erwin J, Sullivan KL. Ventilator-associated pneumonia and oral care: A successful quality improvement project. Am J Infect Control. 2009;37:590–7. doi: 10.1016/j.ajic.2008.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Sharma S, Nanda A, Koli D, Daksh S, Verma M. Role of a Dentist in Comprehensive Management of a Comatose Patient with Post Traumatic Head Injury and Neuropathological Chewing. Indian J Palliat Care. 2014;20:146–52. doi: 10.4103/0973-1075.132639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Scannapieco FA, Stewart EM, Mylotte JM. Colonization of dental plaque by respiratory pathogens in medical intensive care patients. Crit Care Med. 1992;20:740–5. doi: 10.1097/00003246-199206000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Pedreira ML, Kusahara DM, de Carvalho WB, Nunez SC, Peterlini MA. Oral care interventions and oropharyngeal colonization in children receiving mechanical ventilation. Am J Crit Care. 2009;18:319–28. doi: 10.4037/ajcc2009121. [DOI] [PubMed] [Google Scholar]
- 8.Munro CL, Grap MJ, Jones DJ, McClish DK, Sessler CN. Chlorhexidine, toothbrushing, and preventing ventilator-associated pneumonia in critically ill adults. Am J Crit Care. 2009;18:428–37. doi: 10.4037/ajcc2009792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Munro CL, Grap MJ, Hummel RS, Elswick RK, Sessler CN, Mckinney J. Oral health status effect on VAP. Am J Crit Care. 2006;15:453–60. [PubMed] [Google Scholar]
- 10.Bagg J, MacFarlane TW, Poxton IR, Miller CH. Essentials of Microbiology for Dental Students. New York, NY: Oxford University Press; 1999. pp. 227–310. [Google Scholar]
- 11.Berry AM, Davidson PM, Masters J, Rolls K. Systematic literature review of oral hygiene practices for intensive care patients receiving mechanical ventilation. Am J Crit Care. 2007;16:552–62. [PubMed] [Google Scholar]
- 12.O’Hara M, Kiefer D, Farrell K, Kemper K. A review of 12 commonly used medicinal herbs. Arch Fam Med. 1998;7:523–36. doi: 10.1001/archfami.7.6.523. [DOI] [PubMed] [Google Scholar]
- 13.Wagner H, editor. immunomodulatory agents from plants Ch BirkhauserVenag. Basel, Switzerland: 1999. B. R. chemistry, analysis and immunological investigations of Echinacea phytopharmaceuticals; pp. 41–8. [Google Scholar]
- 14.Bauer R, Khan IA, Wagner H. TLC and HPLC analysis of Echinacea pallida and Echinacea angustifulia roots. Planta Med. 2008;54:426–30. doi: 10.1055/s-2006-962489. [DOI] [PubMed] [Google Scholar]
- 15.Pharmacists ASoH-S. Herbal Therapy, Medicinal Plants, and Natural Products: An IPA Compilation. American Society of Health-System Pharmacists. 1999 [Google Scholar]
- 16.Panchabhai TS, Dangayach NS, Krishnan A, Kothari VM, Karnad DR. Oropharyngeal cleansing with 0.2% Chlorhexidine for prevention of nosocomial pneumonia in critically ill patients: An open-label randomized trial with 0.01% potassium permanganate as control. Chest. 2009;135:1150–6. doi: 10.1378/chest.08-1321. [DOI] [PubMed] [Google Scholar]
- 17.Percival SS. Use of Echinacea in medicine. Biochem Pharmacol. 2000;60:155–8. doi: 10.1016/s0006-2952(99)00413-x. [DOI] [PubMed] [Google Scholar]
- 18.Anderson GB, Bowden J, Morrison EC, Caffesse RG. Clinical effects of Chlorhexidine mouthwashes on patients undergoing orthodontic treatment. Am J Orthod Dentofacial Orthop. 1997;111:606–12. doi: 10.1016/s0889-5406(97)70312-3. [DOI] [PubMed] [Google Scholar]
- 19.Renton-Harper P, Addy M, Mora NJ, Doherty FM, RG N. A Comparison of Chlorhexidine, Cetylpyridinium Chloride, Triclosan and C31G Mouthrinse Products for Plaque Inhabitation. J Periodontol. 1996;67:486–89. doi: 10.1902/jop.1996.67.5.486. [DOI] [PubMed] [Google Scholar]
- 20.Rosin M, Welk A, Bernhardt O, Ruhnau M, Pitten FA, Kocher T, et al. Effect of a polyhexamethylene biguanide mouthrinse on bacterial counts and plaque. J Clin Periodontol. 2001;28:1121–6. doi: 10.1034/j.1600-051x.2001.281206.x. [DOI] [PubMed] [Google Scholar]
- 21.Bishara SE, Damon PL, Olsen ME, Jakobsen JR. Effect of applying Chlorhexidine antibacterial agent on the shear bond strength of orthodontic brackets. Angle Orthod. 1996;66:313–6. doi: 10.1043/0003-3219(1996)066<0313:EOACAA>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 22.Leyes Borrajo JL, Garcia VL, Lopez CG, Rodriguez-Nunez I, Garcia FM, Gallas TM. Efficacy of Chlorhexidine mouthrinses with and without alcohol: A clinical study. J Periodontol. 2002;73:317–21. doi: 10.1902/jop.2002.73.3.317. [DOI] [PubMed] [Google Scholar]
- 23.Salehi P, Sh MD. Comparison of the antibacterial effects of persica mouthwash with Chlorhexidine on streptococcus mutans in orthodontic patients. DARU J Pharma Scien. 2006;14:172–82. [Google Scholar]
- 24.Jurkstiene V, Kondrotas AJ, Kevelaitis E. Compensatory reactions of immune system and action of Purple Coneflower (Echinacea purpurea (L.) Moench) preparations. Medicina (Kaunas, Lithuania) 2004;40:657–62. [PubMed] [Google Scholar]
- 25.Keith J, Patricia D. M. A. Mosby's Medical, Nursing, and Allied Health Dictionary. ed. editor. 2005 [Google Scholar]
- 26.Pearson LS. A comparison of the ability of foam swabs and toothbrushes to remove dental plaque: Implications for nursing practice. J Adv Nurs. 1996;23:62–9. doi: 10.1111/j.1365-2648.1996.tb03136.x. [DOI] [PubMed] [Google Scholar]
- 27.Fourrier F, Cau-Pottier E, Boutigny H, Roussel-Delvallez M, Jourdain M, Chopin C. Effects of dental plaque anti-septic decontamination on bacterial colonization and nosocomial infections in critically ill patients. Intensive Care Med. 2000;26:1239–47. doi: 10.1007/s001340000585. [DOI] [PubMed] [Google Scholar]
- 28.Mojon P. Oral health and respiratory infection. J Can Dent Assoc. 2002;68:340–5. [PubMed] [Google Scholar]
- 29.Grap MJ, Munro CL, Elswick RK, Jr, Sessler CN, Ward KR. Duration of action of a single, early oral application of Chlorhexidine on oral microbial flora in mechanically ventilated patients: A pilot study. Heart Lung. 2004;33:83–91. doi: 10.1016/j.hrtlng.2003.12.004. [DOI] [PubMed] [Google Scholar]
- 30.Scannapieco FA, Bush RB, Paju S. Associations between periodontal disease and risk for nosocomial bacterial pneumonia and chronic obstructive pulmonary disease. A systematic review. Ann Periodontol. 2003;8:54–69. doi: 10.1902/annals.2003.8.1.54. [DOI] [PubMed] [Google Scholar]
- 31.Ranjbar H, Arab M, Abbaszadeh A, Ranjbar A. Affective Factors on Oral Care and its Documentation in Intensive Care Units. Iranian Journal of Critical Care Nursing. 2011;4:45–52. [Google Scholar]
- 32.Fourrier F, Dubois D, Pronnier P, Herbecq P, Leroy O, Desmettre T, et al. Effect of gingival and dental plaque antiseptic decontamination on nosocomial infections acquired in the intensive care unit: A double-blind placebo-controlled multicenter study. Crit Care Med. 2005;33:1728–35. doi: 10.1097/01.ccm.0000171537.03493.b0. [DOI] [PubMed] [Google Scholar]
- 33.Birosova L, Olejnikova P. Antimicrobial and antimutagenic activities of extracts from different organs of Echinacea angustifolia DC (Asteracea) Journal of Food & Nutrition Research. 2012:51. [Google Scholar]
- 34.Dalby-Brown L, Barsett H, Landbo AK, Meyer AS, Molgaard P. Synergistic antioxidative effects of alkamides, caffeic acid derivatives, and polysaccharide fractions from Echinacea purpurea on in vitro oxidation of human low-density lipoproteins. J Agric Food Chemi. 2005;53:9413–23. doi: 10.1021/jf0502395. [DOI] [PubMed] [Google Scholar]
- 35.Stanisavlijevic I, Stojicevic S, Velickovic D, Velickovic D, M L. Antioxidant and antimicrobial activities of Echinacea (Echinacea purpurea L.) extracts obtained by classical and ultrasound extraction. Biotechnol Bioengin. 2009;17:478–83. [Google Scholar]


