Abstract
Bronchopulmonary sequestration is a rare anomaly of the lung which is characterized by the presence of a mass of lung tissue which has no connection with the normal bronchopulmonary tree. Sequestration is of two types - intralobar and extralobar, of which intralobar is the more common one. Patients typically present with recurrent hemoptysis, which at times can be massive or with recurrent respiratory tract infections. This case is being presented to highlight the radiological as well as the intraoperative appearance of this rare anomaly.
KEY WORDS: Intralobar, lung, sequestration
THE CASE
A 37-year-old male, who was a nonsmoker, presented to us with a history of recurrent episodes of massive hemoptysis. He was on symptomatic management with antibiotics, hemostatics, and cough suppressants. Clinical examination revealed the presence of Grade 4 clubbing and on auscultation there were coarse, leathery, mid-inspiratory crackles in the left infrascapular and infraaxillary areas. Chest X-ray posteroanterior view showed cystic spaces in the left lower zone. He was evaluated with contrast-enhanced computed tomography (CECT) scan of the thorax which showed the presence of cystic bronchiectasis in the left lower lobe [Figure 1]. Multiple lobulated cystic areas were seen in the basal segments of the left lower lobe [Figures 2 and 3]. The arterial supply to this region was found to be derived from the lower thoracic aorta [Figure 4]. The venous drainage was to the inferior pulmonary vein [Figure 5]. These findings were suggestive of intralobar sequestration. He underwent thoracotomy and left lower lobectomy. Intraoperatively, the arterial supply was confirmed to be arising from the lower thoracic aorta, which was carefully isolated, ligated, and divided [Figure 6]. The patient had an uneventful postoperative recovery and thereafter had complete relief of symptoms.
Figure 1.
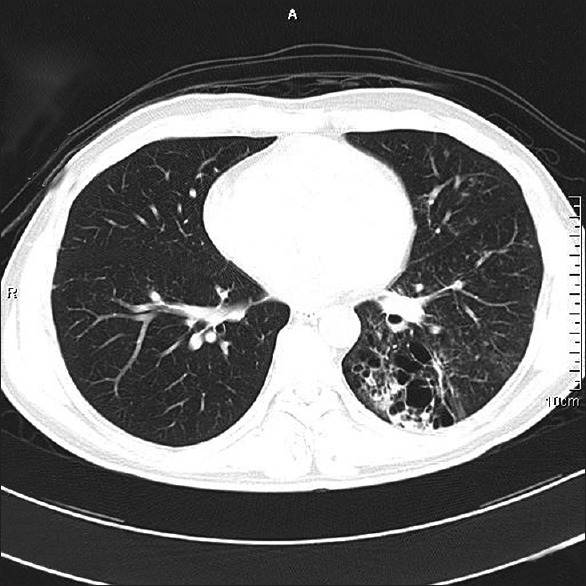
Axial 64-slice high-resolution computed tomography thorax showing cystic spaces in the left lower lobe
Figure 2.
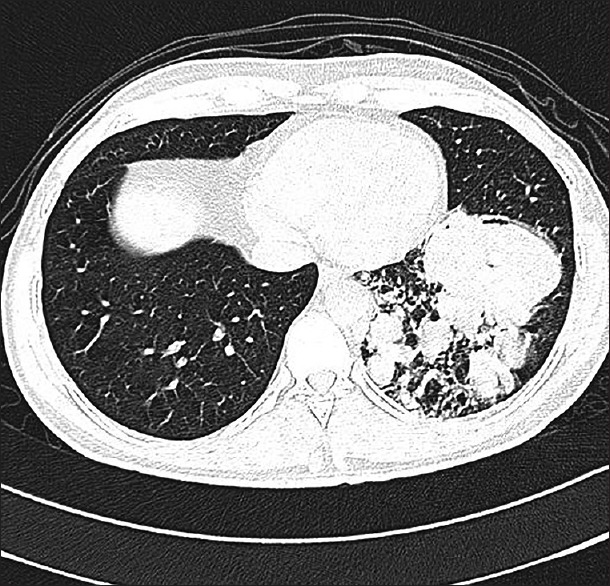
Axial 64-slice high-resolution computed tomography thorax showing the presence of multiple lobulated cystic areas in the left lower lobe
Figure 3.
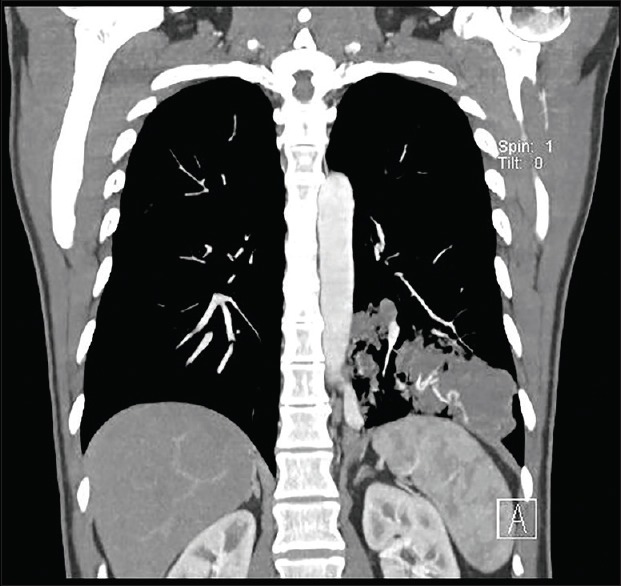
Coronal reconstruction of computed tomography thorax showing the presence of the sequestrated lung tissue in the left lower lobe
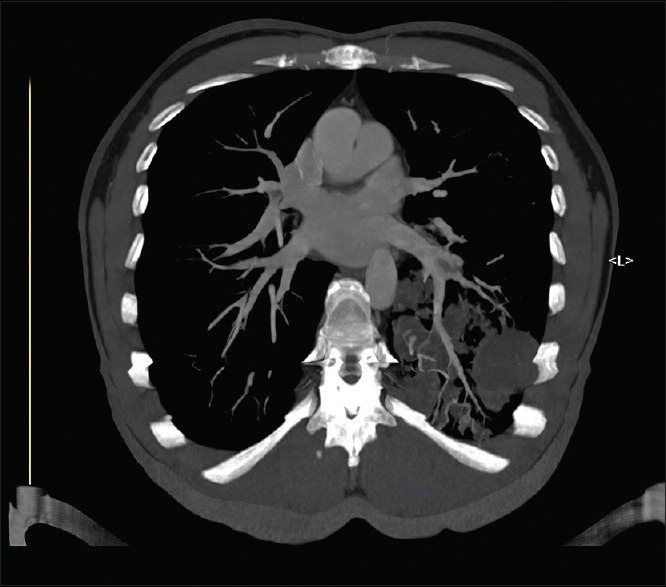
Figure 4.

Sagittal computed tomography image showing the aberrant arterial blood supply arising from the descending thoracic aorta
Figure 5.
Axial computed tomography image showing the venous drainage going to the inferior pulmonary vein
Figure 6.
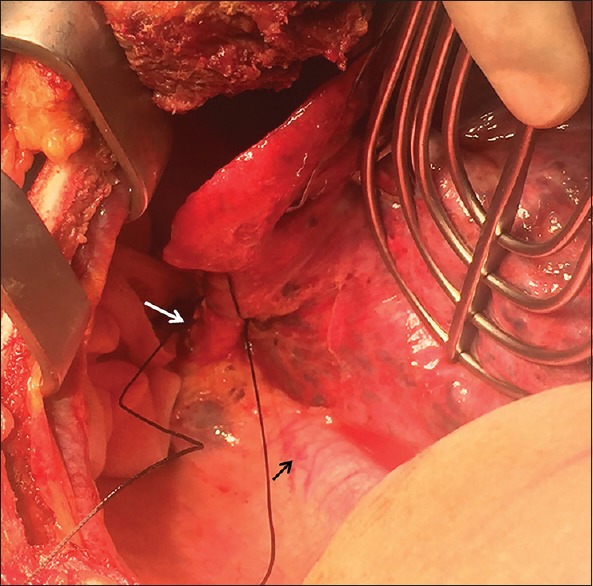
Intraoperative image of the abnormal arterial branch (white arrow) arising from the descending thoracic aorta (black arrow) and supplying the sequestrated lung tissue in the left lower lobe (arrowhead)
DISCUSSION
First described in 1861 by Rektorzik, pulmonary sequestration represents a malformation characterized by the presence of dysplastic lung tissue, having no communication with the tracheobronchial tree and having its own systemic arterial supply.[1] Intralobar sequestration, which is more common than extralobar, is most often located in the lower lobes (98%), with a predilection for the medial and posterior basal segments of the left lower lobe.[2] It is surrounded by normal lung tissue all around. The systemic arterial supply is most commonly seen to arise from the lower thoracic aorta (72%). The other sources are abdominal aorta, celiac axis, splenic artery, intercostal artery, and rarely even from subclavian or internal thoracic arteries.[3] The venous drainage is always to the pulmonary veins.
Initially, intrathoracic sequestration was thought to be a congenital anomaly and the “accessory lung bud theory” was considered to be the basis for its development.[4,5,6] Current concepts, however, suggest that it could be an acquired disease and attribute it to obliterative bronchitis and obstruction of lower lobe bronchus secondary to repeated necrotizing infections of the lung.[3] Contrast-enhanced CT scan of thorax done in angiogram protocol helps to delineate the abnormal arterial supply and venous drainage and confirms the diagnosis of sequestration.[7] Magnetic resonance angiogram is yet another useful investigation.[8] Surgical resection is the treatment of choice. Open surgery through posterolateral thoracotomy is often preferred over video-assisted thoracic surgery since it helps in easier identification, isolation, and division of abnormal feeding arteries.
This case is presented to highlight the importance of considering the clinical possibility of sequestration whenever evaluating patients with lower lobe bronchiectasis. Knowledge about this condition and its abnormal blood supply is of paramount importance for the surgeon while operating on such cases. Recent advances in imaging modalities are most useful in providing reconstructed images which help locate the diseased area as well as identify the source of abnormal blood supply as is very evidently demonstrated in our case.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Felker RE, Tonkin IL. Imaging of pulmonary sequestration. AJR Am J Roentgenol. 1990;154:241–9. doi: 10.2214/ajr.154.2.2105007. [DOI] [PubMed] [Google Scholar]
- 2.Savic B, Birtel FJ, Tholen W, Funke HD, Knoche R. Lung sequestration: Report of seven cases and review of 540 published cases. Thorax. 1979;34:96–101. doi: 10.1136/thx.34.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prasad R, Garg R, Verma SK. Intralobar sequestration of lung. Lung India. 2009;26:159–61. doi: 10.4103/0970-2113.56357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Bassam A, Al-Rabeeah A, Al-Nassar S, Al-Mobaireek K, Al-Rawaf A, Banjer H, et al. Congenital cystic disease of the lung in infants and children (experience with 57 cases) Eur J Pediatr Surg. 1999;9:364–8. doi: 10.1055/s-2008-1072284. [DOI] [PubMed] [Google Scholar]
- 5.Langston C. New concepts in the pathology of congenital lung malformations. Semin Pediatr Surg. 2003;12:17–37. doi: 10.1053/spsu.2003.00001. [DOI] [PubMed] [Google Scholar]
- 6.Carter R. Pulmonary sequestration. Ann Thorac Surg. 1969;7:68–88. doi: 10.1016/s0003-4975(10)66147-4. [DOI] [PubMed] [Google Scholar]
- 7.Ikezoe J, Murayama S, Godwin JD, Done SL, Verschakelen JA. Bronchopulmonary sequestration: CT assessment. Radiology. 1990;176:375–9. doi: 10.1148/radiology.176.2.2367650. [DOI] [PubMed] [Google Scholar]
- 8.Au VW, Chan JK, Chan FL. Pulmonary sequestration diagnosed by contrast enhanced three-dimensional MR angiography. Br J Radiol. 1999;72:709–11. doi: 10.1259/bjr.72.859.10624331. [DOI] [PubMed] [Google Scholar]


