Abstract
Study Design:
Systematic review (update).
Objective:
Degenerative cervical myelopathy (DCM) is a progressive degenerative spine disease that is increasingly managed surgically. The objective of this study is to determine the role of nonoperative treatment in the management of DCM by updating a systematic review published by Rhee and colleagues in 2013. The specific aims of this review were (1) to determine the comparative efficacy, effectiveness, and safety of nonoperative and surgical treatment; (2) to assess whether myelopathy severity differentially affects outcomes of nonoperative treatment; and (3) to evaluate whether activities or minor injuries are associated with neurological deterioration.
Methods:
Methods from the original review were used to search for new literature published between July 20, 2012, and February 12, 2015.
Results:
The updated search yielded 2 additional citations that met inclusion criteria and compared the efficacy of conservative management and surgical treatment. Based on a single retrospective cohort, there were no significant differences in posttreatment Japanese Orthopaedic Association (JOA) or Neck Disability Index scores or JOA recovery ratios between patients treated nonoperatively versus operatively. A second retrospective study indicated that the incidence rate of hospitalization for spinal cord injury was 13.9 per 1000 person-years in a nonoperative group compared with 9.4 per 1000 person-years in a surgical group (adjusted hazard ratio = 1.57; 95% confidence interval = 1.11-2.22; P = .011).
Conclusion:
Nonoperative management results in similar outcomes as surgical treatment in patients with a modified JOA ≥ 13, single-level myelopathy and intramedullary signal change on T2-weighted magnetic resonance imaging. Furthermore, patients managed nonoperatively for DCM have higher rates of hospitalization for spinal cord injury than those treated surgically. The overall level of evidence for these findings was rated as low.
Keywords: cervical spondylotic myelopathy, degenerative cervical myelopathy, nonoperative management, systematic review
Introduction
Degenerative cervical myelopathy (DCM) refers to cord compression arising from nontraumatic, noninfectious, and nononcologic causes such as cervical spondylotic myelopathy, ossification of the posterior longitudinal ligament, hypertrophy of the ligamentum flavum, degenerative disc disease, and progressive cervical kyphosis.1 Surgery is increasingly recommended for patients with moderate and severe myelopathy as it effectively halts neurological progression and helps improve functional status, disability, and quality of life.2 Unfortunately, little is known about the role of nonoperative treatment in the management of DCM.
The objective of this study is to update a systematic review published in 2013 by Rhee et al3 that investigated (1) the comparative efficacy, effectiveness, and safety of nonoperative and surgical treatment for DCM; (2) whether the severity of myelopathy differentially affects outcomes of nonoperative treatment; and (3) whether specific activities or minor injuries are associated with neurological deterioration in patients treated nonoperatively for DCM.
Materials and Methods
Electronic Literature Search
An updated search based on a previous protocol3 was conducted in PubMed and the Cochrane Collaboration library for literature published between July 20, 2012, and February 12, 2015. Detailed methodology was previously described, including search strategy, inclusion and exclusion criteria, data extraction, data analysis, and evaluation of study quality and overall strength of evidence.3
Results
Study Selection
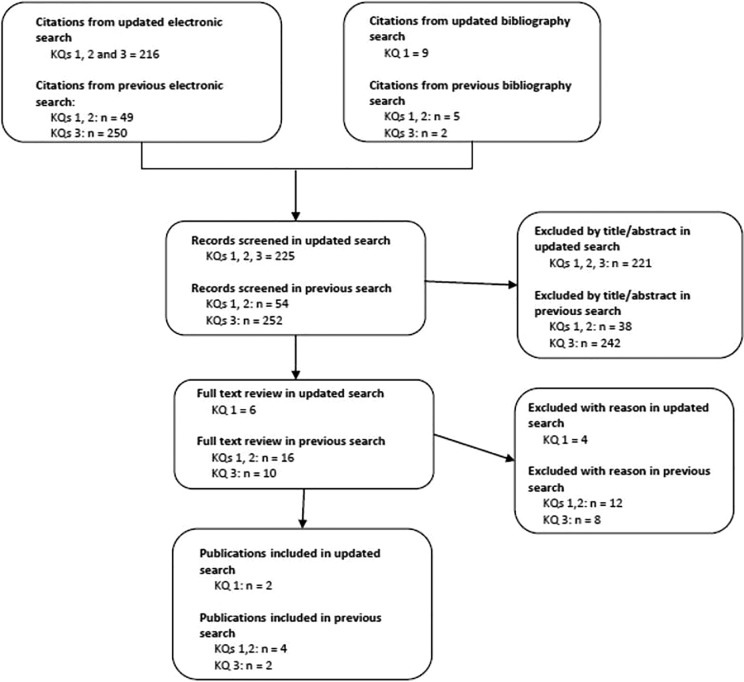
The updated electronic search yielded 216 new citations. An additional 9 citations were identified through directed manual search (Figure 1). After reviewing the titles and abstracts, we retrieved the full text of 6 studies. Four of these did not meet one or more inclusion criteria and were excluded at full-text review4–7 (Table 1). The remaining 2 studies compared the efficacy of conservative treatment and surgical management and were included in this update (Table 2). Both had a moderately high risk of bias (Table 3).
Figure 1.
Results of literature search. KQ = key question.
Table 1.
Excluded Studies and Reasons for Exclusion.
| Author (Year) | Reasons for Exclusion |
|---|---|
| Gu et al (2014)4 | Acute spinal cord injury following minor trauma in patients with OPLL |
| Kong et al (2013)7 | No comparative effectiveness between surgical and nonsurgical treatments |
| Wu et al (2012)6 | No comparative effectiveness between surgical and nonsurgical treatments; only results of nonoperative treatment |
| Wu et al (2011)5 | No comparative effectiveness between surgical and nonsurgical treatments; disease prevalence and incidence were reported |
Abbreviation: OPLL, ossification of the posterior longitudinal ligament.
Table 2.
Characteristics of New Studies Assessing Efficacy, Effectiveness, and/or Safety.
| Author (Year) and Study Design | Patient Characteristics | Mean Follow-up/% Follow-up | Initial Severity | Nonoperative Treatment Type | Surgery Treatment Type | Outcome Measures | |
|---|---|---|---|---|---|---|---|
| Nonoperative | Surgery | ||||||
| Wu et al (2013)8 | N = 14 140 | ≥1 year/% NR | NR | NR | NR |
|
|
| Retrospective cohort, | Mean age = NR |
|
|||||
| administrative database | Male = NR |
|
|||||
|
|||||||
|
|||||||
| Li et al (2014)9 | N = 91 | 31.76 months/100% | JOA ≥ 13 (n = 38) | JOA ≥ 13 (n = 53) |
|
|
|
| Retrospective cohort | Mean age = 50.9 years | ||||||
| Male = 51.6% | |||||||
Abbreviations: NR, not reported; SCI, spinal cord injury; JOA, Japanese Orthopaedic Association.
a(Post-treatment JOA score − Prior-treatment JOA score)/(17 − Prior-treatment JOA score) × 100%.
Table 3.
Class of Evidence for Therapeutic Studies.
| Methodological Principle | Wu et al (2013)8 | Li et al (2014)9 |
|---|---|---|
| Study design | ||
| Prospective cohort study | ||
| Retrospective cohort study | ✓ | ✓ |
| Case-control study | ||
| Case-series | ||
| Independent or blind assessment | ||
| Co-interventions applied equally | ||
| Complete follow-up of ≥80% | ✓ | ✓ |
| Adequate sample size | ✓ | |
| Controlling for possible confoundinga | ✓ | |
| Moderately high risk | Moderately high risk |
aGroups must have comparable baseline characteristics or analysis must control for confounding.
The first study was an administrative database study on 14 140 patients from Taiwan who were hospitalized for DCM between 1998 and 2009 and had at least 1-year follow-up.8 Patients were divided into 2 groups based on whether they were treated conservatively (the type of nonoperative treatment was not specified) or surgically. Patients who were rehospitalized for a spinal cord injury were also identified. The incidence rate of hospitalization for spinal cord injury was 13.9 per 1000 person-years in the nonoperative group and 9.4 per 1000 person-years in the surgical group (adjusted hazard ratio = 1.57; 95% confidence interval = 1.11-2.22; P = .011; Table 4). A limitation of this study was that specific clinical information could not be obtained as data was derived from an administrative ICD-9 database.
Table 4.
Incidence Rates and Hazard Ratios of Spinal Cord Injury in Patients Treated Nonoperatively Versus Surgically for Cervical Spondylotic Myelopathy: Results Derived From Wu et al.8
| Nonoperative | Surgery | Crude HR | P | Adjusted HRa | P | |
|---|---|---|---|---|---|---|
| Number of hospitalizations for SCI | 122 | 44 | ||||
| Observed person-years | 8777 | 4685 | ||||
| Incidence rateb (95% CI) | 13.9 (11.6-16.6) | 9.39 (7.0-12.6) | 1.48 (1.04-2.14) | .025 | 1.57 (1.11-2.22) | .011 |
Abbreviations: HR, hazard ratio; SCI, spinal cord injury; CI, confidence interval.
aAdjusted for age and sex, diabetes, hypertension, osteoporosis, rheumatoid arthritis, and osteoarthritis.
bPer 1000 person-years.
The second included study was a retrospective cohort study of 91 Chinese DCM patients9 with modified Japanese Orthopedic Association (mJOA) scores ≥13 and increased intramedullary signal change on T2-weighted magnetic resonance imaging (MRI). Patients were excluded if they had ossification of the posterior longitudinal ligament or multilevel myelopathy. Outcomes were compared between a surgical (n = 53) and nonsurgical (n = 38) group using several assessment tools, including postoperative Neck Disability Index (NDI) and Japanese Orthopaedic Association (JOA) scores and JOA recovery ratios. There were no significant differences between the 2 treatment groups with respect to baseline functional status (JOA) or disability (NDI). Patients managed surgically underwent a 1-level anterior cervical discectomy and fusion, whereas those treated nonoperatively received medication, traction, acupuncture, and/or physical therapy. There were no significant differences in posttreatment JOA or NDI scores or in JOA recovery ratios between the 2 groups at a mean follow-up of 34 months for the nonoperative group and 31 months for the surgery group (Table 5). Limitations of this study include its relatively short-term follow-up and retrospective design, which could be associated with selection bias when determining type of treatment.
Table 5.
Summary of Japanese Orthopaedic Association and Neck Disability Index Scores in Patients Treated Nonoperatively Versus Surgically: Results Derived From Li et al.9
| Nonoperativea | Surgerya | P | |
|---|---|---|---|
| Pretreatment JOA score | 14.37 ± 0.97 | 14.23 ± 1.07 | .365 |
| Posttreatment JOA score | 15.45 ± 0.92 | 15.60 ± 0.91 | .891 |
| JOA recovery ratio (%)b | 43.86 ± 29.55 | 52.83 ± 27.44 | .646 |
| Pretreatment NDI (%) | 20.82 ± 4.24 | 21.15 ± 4.98 | .303 |
| Posttreatment NDI (%) | 18.73 ± 4.54 | 18.03 ± 4.76 | .991 |
Abbreviations: JOA, Japanese Orthopaedic Association; NDI, Neck Disability Index.
aValues shown are mean ± standard deviation.
b(Posttreatment JOA score − pretreatment JOA score)/(17 − pretreatment JOA score) × 100%.
Evidence Summary
An updated summary of the evidence is presented in Table 6. Based on low-level evidence, nonoperative treatment for patients with “milder” (JOA ≥ 13), single-level DCM and intramedullary MRI signal change results in similar outcomes as surgery based on postoperative JOA and NDI scores and JOA recovery ratios.
Table 6.
Evidence Summary.
| Studies; N | Strength of Evidence | Conclusions/Comments | Baseline | Upgrade (Levels) | Downgrade (Levels) | |
|---|---|---|---|---|---|---|
| Question 1: What is the evidence of efficacy, effectiveness and safety of nonoperative treatment for patients with degenerative cervical myelopathy? | ||||||
| Nonoperative versus Operative Treatment | ||||||
| JOA scores | 1 RCT (N = 68)10,11 1 retrospective cohort (N = 91)9 | Low | There is low evidence that there is no difference in mJOA scores between patients with “milder” CSM (mJOA ≥ 12) that receive operative versus nonoperative care: (1) scores were similar at 1, 2, 3, and 10 year follow-up (RCT); (2) there were no differences in JOA scores after 2 to 3 years (retrospective cohort). | High | None | Risk of bias (1) Imprecise (1) |
| NDI | 1 retrospective cohort (N = 91)9 | Very Low | There is very low evidence from one retrospective cohort study that there is no difference in NDI between patients treated operatively versus nonoperatively after 2 to 3 years. | Low | None | Risk of bias (1) Imprecise (1) |
| JOA improvement | 1 retrospective cohort (N = 101)12 | Very Low | There is very low evidence from one small retrospective observational study (N = 101) to compare the proportion of patients with JOA improvement following operative versus nonoperative care. Patients that received nonoperative care had “milder” CSM (mJOA ≥ 13), while those receiving surgery had moderate to severe CSM (mJOA < 13) at baseline. | Low | None | Imprecise (1) Indirect (1) |
| Neurological symptoms | 1 prospective cohort (N = 62)13 | Very Low | There is very low evidence from one small prospective observational study (N = 62) that neurological symptoms of upper extremity pain, arm or leg numbness, arm weakness, headache, or difficulty walking are superior in surgically treated patients. | Low | None | Imprecise (1) Indirect (1) |
| Timed 10-meter walk | 1 RCT (N = 68)10,11 | Low | There is low evidence from one small RCT (N = 68) that, in patients with “milder” CSM (mJOA ≥ 12), surgery results in a slower 10-meter walk test than nonoperative care. Test times from baseline remained similar in the nonoperative group but increased in the surgical group during 3 years of follow-up. At 10 years following treatment, no difference was identified between groups. | High | None | Risk of bias (1) Imprecise (1) |
| Activities of daily living | 1 RCT (N = 68)10,11 | Low | There is low evidence from one small RCT (N = 68) that there is no difference between operative and nonoperative groups in the proportion of “milder” patients (mJOA ≥ 12) that had worse or improved clinician-based or patient-reported daily activity scores. There were no differences between groups at 1, 2, 3, and 10 years following treatment. | High | None | Risk of bias (1) Imprecise (1) |
| Incidence of hospitalization for SCI | 1 retrospective cohort (N = 14 140)8 | Low | There is low evidence to demonstrate that the incidence of hospitalization for SCI is greater in CSM patients undergoing conservative care compared to those treated surgically. In one retrospective cohort study, the hazard is approximately one and a half times greater in the conservative group than the surgical group, even after adjustment for confounders such as age, sex, diabetes, and hypertension. | Low | None | None |
| Rigorous versus nonrigorous nonoperative treatment | ||||||
| JOA scores | 1 retrospective cohortd (N = 101)12 | Very Low | There is very low evidence to demonstrate that the proportion of patients with JOA improvement or worsening was different between patients receiving rigorous versus nonrigorous nonoperative care. In the one small retrospective observational study (N = 69), 38% of patients treated rigorously improved versus 6% of those not treated rigorously. However, this study has a small sample size, did not adjust for potential confounding, and has imprecise results. | Low | Large effect (1) | Risk of bias (1) Imprecise (1) |
| Question 2: Do outcomes of nonoperative treatment vary according to severity of myelopathy? | ||||||
| No Evidence | No studies were identified that evaluated the effect of myelopathy severity on treatment outcomes in patients receiving nonoperative management. | None | None | |||
| Question 3: What is the evidence that different activities or minor injuries alter the risk of neurological deterioration or myelopathy development in patients treated nonoperatively for degenerative cervical myelopathy or asymptomatic cervical cord compression? | ||||||
| Development or deterioration of myelopathy | 2 retrospective cohorts (N = 317)14,15 | Very Low | There is very low evidence to determine whether different activities or minor injuries alter the risk of neurological deterioration or myelopathy development. In one retrospective cohort study, 7% of patients with asymptomatic stenosis developed myelopathy following a traumatic event to the head, spine, trunk, or shoulders versus 24% who developed myelopathy without a traumatic event. In a second retrospective cohort of 27 patients with OPLL: (1) 87% of patients who had myelopathy experienced neurological deterioration and (2) 68% of nonmyelopathic patients developed myelopathy following a minor trauma. | Low | None | Imprecise (1) |
Abbreviations: JOA, Japanese Orthopaedic Association; RCT, randomized controlled trial; mJOA, modified JOA; CSM, cervical spondylotic myelopathy; NDI, Neck Disability Index; SCI, spinal cord injury; OPLL, ossification of the posterior longitudinal ligament.
aBaseline quality: High = majority of articles low/moderately low risk of bias; Low = majority of articles moderately high/high risk of bias.
bUpgrade: Large magnitude of effect (1 or 2 levels); dose response gradient (1 level); plausible confounding decreases magnitude of effect (1 level).
cDowngrade: Inconsistency of results (1 or 2 levels); indirectness of evidence (1 or 2 levels); imprecision of effect estimates (1 or 2 levels); risk of bias (1 or 2 levels); failure to specify subgroup analysis a priori (1 level); reporting bias (1 level).
dPatient characteristics given for nonoperative group only.
Rates of hospitalization for subsequent spinal cord injury were significantly higher in patients undergoing initial conservative treatment compared to those managed operatively: 9.4 (95% CI = 7.0-12.6) per 1000 person-years for those treated surgically, and 13.9 (95% CI = 11.6-16.6) per 1000 person-years for those treated without surgery.
However, the overall evidence for these findings is graded as “low” due to the retrospective nature of these studies. This means that our confidence in the estimates of effect for these outcomes is limited and that the true effect may be substantially different from these estimates.
Conclusions
The results of this update indicate that nonoperative management results in similar outcomes as surgical treatment in patients with a mJOA ≥ 13, single-level myelopathy, and intramedullary signal change on T2-weighted MRI. However, we believe that these patients, if managed nonoperatively, should be followed closely and monitored for neurological deterioration. It is important that clinicians inform their patients of the possibility of disease progression and educate them on future relevant symptoms.
Furthermore, patients managed nonoperatively for DCM have higher rates of subsequent hospitalization for spinal cord injury than those treated surgically. This increased risk should be factored into clinical decision making and included in discussions with patients when weighing the risks and benefits of operative versus nonoperative care.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by AOSpine and the Cervical Spine Research Society (CSRS). Dr Fehlings wishes to acknowledge support from the Gerald and Tootsie Halbert Chair in Neural Repair and Regeneration and the DeZwirek Family Foundation. Dr Tetreault acknowledges support from a Krembil Postdoctoral Fellowship Award.
References
- 1. Nouri A, Tetreault L, Singh A, Karadimas SK, Fehlings MG. Degenerative cervical myelopathy: epidemiology, genetics, and pathogenesis. Spine (Phila Pa 1976). 2015;40:E675–E693. [DOI] [PubMed] [Google Scholar]
- 2. Tetreault L, Goldstein CL, Arnold P, et al. Degenerative cervical myelopathy: a spectrum of related disorders affecting the aging spine. Neurosurgery. 2015;77(suppl 4):S51–S67. [DOI] [PubMed] [Google Scholar]
- 3. Rhee JM, Shamji MF, Erwin WM, et al. Nonoperative management of cervical myelopathy: a systematic review. Spine (Phila Pa 1976). 2013;38(22 suppl 1):S55–S67. [DOI] [PubMed] [Google Scholar]
- 4. Gu Y, Chen L, Dong RB, Feng Y, Yang HL, Tang TS. Laminoplasty versus conservative treatment for acute cervical spinal cord injury caused by ossification of the posterior longitudinal ligament after minor trauma. Spine J. 2014;14:344–352. [DOI] [PubMed] [Google Scholar]
- 5. Wu JC, Liu L, Chen YC, Huang WC, Chen TJ, Cheng H. Ossification of the posterior longitudinal ligament in the cervical spine: an 11-year comprehensive national epidemiology study. Neurosurg Focus. 2011;30:E5. [DOI] [PubMed] [Google Scholar]
- 6. Wu JC, Chen YC, Liu L, et al. Conservatively treated ossification of the posterior longitudinal ligament increases the risk of spinal cord injury: a nationwide cohort study. J Neurotrauma. 2012;29:462–468. [DOI] [PubMed] [Google Scholar]
- 7. Kong LD, Meng LC, Wang LF, Shen Y, Wang P, Shang ZK. Evaluation of conservative treatment and timing of surgical intervention for mild forms of cervical spondylotic myelopathy. Exp Ther Med. 2013;6:852–856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wu JC, Ko CC, Yen YS, et al. Epidemiology of cervical spondylotic myelopathy and its risk of causing spinal cord injury: a national cohort study. Neurosurg Focus. 2013;35:E10 doi:10.3171/2013.4.FOCUS13122. [DOI] [PubMed] [Google Scholar]
- 9. Li FN, Li ZH, Huang X, et al. The treatment of mild cervical spondylotic myelopathy with increased signal intensity on T2-weighted magnetic resonance imaging. Spinal Cord. 2014;52:348–353. doi:10.1038/sc.2014.11. [DOI] [PubMed] [Google Scholar]
- 10. Kadanka Z, Bednarik J, Novotny O, Urbanek I, Dusek L. Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years. Eur Spine J. 2011;20:1533–1538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kadanka Z, Mares M, Bednanik J, et al. Approaches to spondylotic cervical myelopathy: conservative versus surgical results in a 3-year follow-up study. Spine (Phila Pa 1976). 2002;27:2205–2210. [DOI] [PubMed] [Google Scholar]
- 12. Yoshimatsu H, Nagata K, Goto H, et al. Conservative treatment for cervical spondylotic myelopathy. Prediction of treatment effects by multivariate analysis. Spine J. 2001;1:269–273. [DOI] [PubMed] [Google Scholar]
- 13. Sampath P, Bendebba M, Davis JD, Ducker TB. Outcome of patients treated for cervical myelopathy. A prospective, multicenter study with independent clinical review. Spine (Phila Pa 1976). 2000;25:670–676. [DOI] [PubMed] [Google Scholar]
- 14. Bednarik J, Sladkova D, Kadanka Z, et al. Are subjects with spondylotic cervical cord encroachment at increased risk of cervical spinal cord injury after minor trauma? J Neurol Neurosurg Psychiatry. 2011;82:779–781. [DOI] [PubMed] [Google Scholar]
- 15. Katoh S, Ikata T, Hirai N, Okada Y, Nakauchi K. Influence of minor trauma to the neck on the neurologicals outcome in patients with ossification of the posterior longitudinal ligament (OPLL) of the cervical spine. Paraplegia. 1995;33:330–333. [DOI] [PubMed] [Google Scholar]