Abstract
Regulations usually distinguish between prescription‐only (POM) and over‐the‐counter (OTC) medicines. The former requires medical prescription; the latter are available for SM of common minor or easily treated ailments. However, in the Eastern Mediterranean countries, theoretical prescription medicines can easily be purchased without a prescription, as self‐medication (SM) resulting in potential misuse and unnecessary risk for patients. The magnitude of this activity is uncertain. The aim of this article, therefore, is to undertake a comprehensive review to identify the different types of medicines that can easily be purchased as SM in Middle East and recognized as misused. An extensive review of the published literature (1990–2015) was conducted using Pubmed, web of science, Cochrane, and Google Scholar databases, for OTC medicine misuse in the Middle East. A total of 72 papers were identified. Medicines involved in misuse included: codeine containing products, topical anesthetics, topical corticosteroids, antimalarial, and antibiotics. Self‐medication misuse of medicines seemed widespread. Individual treatment patterns were not clearly identified. Studies were not standardized, limiting the comparability between studies and the estimation of the scale of misuse. Pharmacists, friends, or parents were found to be the main sources of SMs. Knowledge and attitudes are an important contributing factor in the misuse of these medications. Strategies and interventions to limit misuse were rarely identified in literature. In conclusion, a massive problem involving a range of medicines was found in Middle East. Standardization of studies is a prerequisite to the understanding and prevention of misuse of self‐medication.
Keywords: Eastern Mediterranean countries, Middle East, misuse, over‐the‐counter, Prescription medicines, Self‐medication
Abbreviations
- EMRO
Eastern Mediterranean Region
- OTC
over‐the‐counter
- POM
prescription‐only
- SM
self‐medication
Introduction
Regulations usually distinguish between prescription‐only (POM) and over‐the‐counter (OTC) medicines. The former requires medical prescription; the latter are available for SM of common minor or easily treated ailments. Many patients may treat themselves and self‐medicate, using either OTC medication or prescription medicines without prescription.
OTC medicines are medicines that are approved for self‐medication (SM) because their indication is easily recognized by patients and usually self‐limiting, and the medicine is thought to be safe and effective. Paracetamol and low‐dose NSAIDs for pain relief are typical of these OTC medicines. However, SM is not limited to OTC medicines, and patients self‐medicate with prescription medicines. These are medicines that may have been prescribed and left over from a previous treatment episode, or bought directly from the community pharmacies without a prescription. The latter is in principle not authorized. However, in practice in many countries the dispensing of prescription medicines by pharmacists, without a prescription is not unusual, especially for the short‐term treatment of common diseases.
SM has become quite common in developed (Blenkinsopp and Bradley 1996) and more common in developing countries (Kamat and Nichter 1998). In developing countries people are not only using OTC products as SM but also prescription medicines, as SM products, without supervision. SM has been studied in many different populations, showing that about 25–75% of the population consumes SM medicines (Wazaify et al. 2005). SM is highly prevalent in the community in Eastern Mediterranean countries. In Middle East, prescription medicines can easily be purchased without prescription, resulting in potential misuse and unnecessary risk. Patients may use medicines without a prescription from pharmacies, use old prescriptions, share medicines with friends/relatives, and use leftover medicines from previous prescription‐based dispensing.
However, there is a relative lack of literature relating to SM misuse in the Middle East. There has been relatively little systematic research on this topic, partly due to the perception that SM misuse is not as problematic as other types of drug abuse. A single review article (Cooper 2013) has described the current knowledge of OTC medicine misuse and identifies the different types of OTC medicines implicated. A number of specific medicines have been implicated in literature including: opiate‐based OTC analgesics, cough syrup containing dextromethorphan or pseudoephedrine, diphenhydramine, and other antihistamines (Lessenger and Feinberg 2008). Moreover, as antibiotics are available without prescription in the Middle East they were also included in the review.
Misuse has been defined as the incorrect use of an OTC product for a medical purpose, usually in terms of dosage or duration of use (Hughes et al. 1999).
The aim of this article, therefore, is to undertake a comprehensive review to identify the different types of medicines that can easily be purchased as SM in Middle East and recognized as misused. Other objectives were to describe current knowledge and understanding about the range of SM misuses and to identify the source of SM practice.
Materials and Methods
Search strategy
Databases, namely, Medline/Pubmed, Web of Science, Cochrane Library, and other sources, were used to identify peer‐reviewed papers dealing with the review theme in WHO Eastern Mediterranean countries. Search terms were identified through a pilot review of the literature and were used to identify articles through a systematic, standardized process.
The words/strings used for search and inclusion criteria were as follows: using combinations of the following terms: “over the counter”, “OTC”, “non‐prescription”, “self prescription medicines”, “prescription medicines”, “misuse”, “abuse”, “addiction”, “dependency,” and “nonmedical use”, “irrational use”, “inappropriate use”, Arab and name of countries belonging to the WHO Eastern Mediterranean Region (EMRO). The search strategy is outlined in figure 1. The search was limited to publications between 1990 and July 2015. Reviews (Lessenger and Feinberg 2008; Al‐Tawfiq et al. 2010; Cooper 2013; Shehnaz et al. 2014a,b) were used for reference mining but they were not included.
Figure 1.
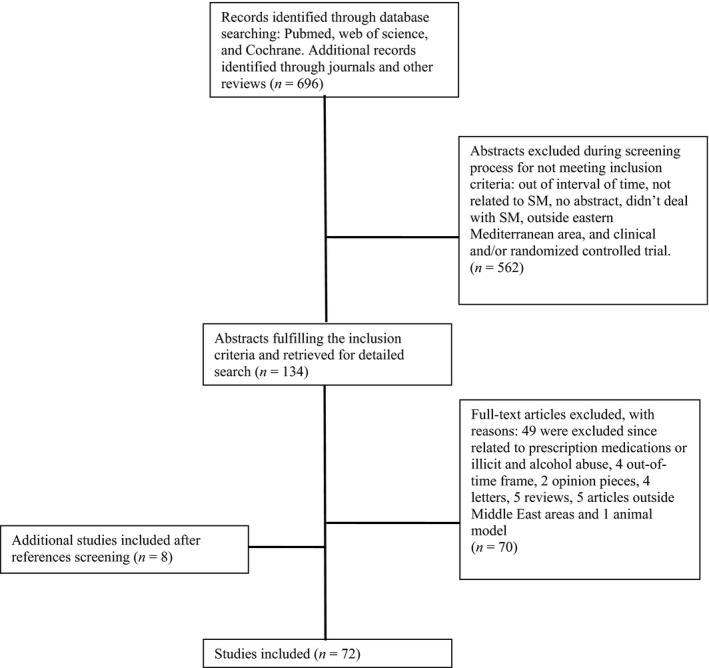
Selection of articles.
Article selection
For a paper to be included in the review, four criteria were jointly required: (1) SM or over‐the‐counter (OTC) or prescription medications as some are available without prescription in the community pharmacy in Middle East, (2) WHO Eastern Mediterranean country, (3) Publication from 1990 to July 2015, and (4) Availability of abstract in English, French or Arabic.
Exclusion criteria included non‐English, French, or Arabic language publications and reference exclusively to prescribed or illicitly obtained medicines. Articles related to alcohol or substance abuse were also excluded; although they represent an important category, they cover different objectives of the review theme related to SM misuse. Studies were also excluded via search limits if they were as follows: review articles, on animal models; hospital‐based studies; clinical and/or randomized controlled trials; editorials, letters, opinions, or comment publication type.
Content reviews were performed to select articles that met these criteria. From the title review, articles were excluded if they were not relevant to the subject matter. Any articles with an ambiguous title or title suggestive of the topic were evaluated in the abstract review. Abstracts were reviewed for details that indicated the article may meet inclusion criteria. Finally, full‐text articles were reviewed and assessed to determine whether inclusion criteria were met. Full‐text reviews were also conducted on review articles to identify additional articles from their bibliographies.
Data abstraction
The following details were extracted from each study using an abstraction form: year of publication, country of origin, population sampled, recall period, and data pertaining to the study objectives.
Results
Literature search results
The database search yielded 696 publications for review. Fifty other records were added through other sources like health journals edited in Iran, Pakistan, and Saudi Arabia and previous reviews for reference mining but they were not included. 562 articles were excluded for reasons of duplicated records, review articles, irrelevant topic, time of publication, availability of abstract, outside eastern Mediterranean area, and clinical and/or randomized controlled trial.
A secondary search was performed to elaborate the primary concept. A total of 134 full‐text articles were assessed of which 49 were excluded as they were related to prescription medications or illicit and alcohol abuse or medication storage and wastage, which did not meet our study objective. Another 21 articles (four out of time frame, two opinion pieces, four letters, five reviews, five articles outside Middle East area, and one animal model) were excluded. An additional eight articles were added after reference screening. This resulted in 72 articles, which fulfilled the inclusion criteria. (Fig. 1).
Study characteristics
The studies in the 72 publications differed substantially in sample size, recall period, and location. These studies reviewing overall prevalence, frequencies, and pattern of OTC misuse originated from different countries: Iran (n = 16), Pakistan (n = 12), Jordan (n = 11), Saudi Arabia (n = 8), Lebanon (n = 3), United Arab Emirates (n = 4), Kuwait (n = 2), Egypt (n = 2), Syria (n = 2), Yemen (n = 2), Iraq (n = 2), Palestine (n = 2), Bahrain (n = 2), Libya (n = 1), Sudan (n = 1), and Oman (n = 1). An additional paper included Lebanon, Egypt, Jordan, Tunisia, and Libya (Scicluna et al. 2009). All the studies were cross sectional in nature barring 1 case report (Risco and Millar 1992) and 1 prospective study (Nazarzadeh et al. 2014). Most studies used self‐administered questionnaires or face‐to‐face interviews for data collection. Mixed data collection techniques were also adopted.
Prevalence of SM
SM was highly prevalent in the community in Eastern Mediterranean countries, ranging from 35.4% to 83% in Iran (Jalilian et al. 2013; Jafari et al. 2015), 42.5% in Jordan (Yousef et al. 2008), 35.4% in Saudi Arabia (Alghanim 2011), and 68.1% in Pakistan (Syed et al. 2015). It is also well prevalent among adolescents in many Middle East countries including Jordan (87%) (ALBashtawy et al. 2015), Palestine (98%) (Sawalha 2008), Kuwait (92%) (Abahussain et al. 2005), Emirates (89.2%) (Shehnaz et al. 2013), Bahrain (44.8%) (James et al. 2006), and Pakistan (80.4%) (Mumtaz et al. 2011).
SM was also common for children and among pregnant women. Medication without prescription was given to 51.3% children in Pakistan (Haider and Thaver 1995), mostly consisting of unidentified medicines or analgesics/antipyretics. Good past experience (61.3%) with the medicine was the main reason for SM (Haider and Thaver 1995). In addition, more than 35% of the women self‐medicated during pregnancy (Baghianimoghadam et al. 2013).
Scale of SM misuse
Methods used to describe the extent of OTC misuse varied. This variety is due to different methods and data sources, which make comparisons between countries difficult. Several studies relied on the perceptions or behavior of pharmacists (in Jordan, Palestine, Lebanon, Saudi Arabia, Egypt, and Syria), whereas others relied on sampling the public, pharmacy customers, or among university or school students.
Studies varied as to whether they focused on a particular product or on a range of products. Studies based on pharmacists’ approaches appeared to generate more detailed and varied descriptions of medicines that may be misused. In Jordan, for example, antibiotics were commonly cited by pharmacists as being misused, as regulations restricting their supply were not always enforced (Albsoul‐Younes et al. 2010). Similar studies were conducted in Palestine and Egypt by Sweileh et al. (2004) and Elhoseeny et al. (2013) based on perception of community pharmacists. In Palestine, 66% of community pharmacists believe that there is an increase in misuse of OTC medicines (Sweileh et al. 2004). Antitussives, analgesics, antihistamines, laxatives, decongestants, and sedatives hypnotics and tranquilizers were also identified by pharmacists as misused OTC medicines (Sweileh et al. 2004).
The use of nonprescription medicine among patients/consumers was reported by 66.9% of pharmacists to have increased in the past 4 years (Elhoseeny et al. 2013). Iran pharmacies sold 57% of prescription items without prescription (Zargarzadeh et al. 2008). Shehnaz study in the United Arab Emirates showed high prevalence of SM with antibiotics (53%) and sedative/hypnotics (27%) (Shehnaz et al. 2013).
Moreover, some studies showed that the practice of SM is influenced by pharmacists. In Syria, from 200 pharmacies visited, 87% agreed without insistence from the investigator to sell antibiotics without prescription. This figure increased to 97% when the investigators who were at first denied antibiotics insisted on having the antibiotics (Al‐Faham et al. 2011). In Saudi Arabia, only one attendant pharmacist refused to dispense medications without prescription. Seventeen percent dispensed urinary antiseptic only and 82% gave antibacterial agents (Al‐Ghamdi 2001).
Medicines involved in SM misuse
Medicines implicated in SM misuse belong to different pharmacologic groups: Codeine‐based products, tramadol, topical ocular anesthetic, topical corticosteroids. antibiotics, and antimalarials were also described as misused medicines in many articles as seen in Table 1.
Table 1.
Types of drugs misused in the retrieved publications
| Types of Drugs misused | Number of papers (n) | Countries | Prevalence of SM % | Study participants | Reference |
|---|---|---|---|---|---|
| Analgesics (including codeine‐containing medicines) | 4 | Iran | 28.7% | 564 University students | Sarahroodi et al. (2012) |
| 60% | 210 University and school students | Sedighi et al. (2006) | |||
| Saudi Arabia | 504 University students | Ibrahim et al. (2015) | |||
| Pakistan | 55.4% | 1380 Community participants | Qazi et al. (2013) | ||
| Jordan | 32% | 393 Pharmacists | Albsoul‐Younes et al. (2010) | ||
| Tramadol | 2 | Iran | 56%4.8% | 162 Pharmacy customers 1894 School students | Zabihi et al. (2011), Nazarzadeh et al. (2014) |
| Antibiotics | 38 | Iran | 35.8% | 320 University staff | Askarian and Maharlouie (2012) |
| 42.2% | 195 University members | Sarahroodi et al. (2010) | |||
| 43% | 272 Patients at clinics | Jafari et al. (2015) | |||
| 53% | 153 University females | Sarahroodi and Arzi (2009) | |||
| 57.6% | 572 Community participants | Heidarifar et al. (2013) | |||
| Jordan | 40.7% | 477 Patients at clinics | Sawair et al. (2009) | ||
| 46.3 | 480 pharmacy customers | Al‐Bakri et al. (2005) | |||
| 62% | 37 Community participants | Darwish et al. (2014) | |||
| 32% | 174 Patients at clinics | Scicluna et al. (2009) | |||
| 59.1% | 1141 Community participants | Shehadeh et al. (2012) | |||
| N/A | 1091 Pharmacy customers | Alzoubi et al. (2013) | |||
| 68.8% | 679 University students | Suaifan et al. (2012) | |||
| N/A | 393 Pharmacists | Albsoul‐Younes et al. (2010) | |||
| Lebanon | 32% | 110 Pharmacists | Farah et al. (2015) | ||
| 42% | 340 Pharmacy customers | Cheaito et al. (2014) | |||
| 37% | 119 Patients at clinics | Scicluna et al. (2009) | |||
| Pakistan | 71.4% | 780 University and school students | Aslam et al. (2013) | ||
| N/A | 1342 Households | Sturm et al. (1997) | |||
| 30% Pharyngitis 23% Gastroenteritis | 851 Community participants | Qazi et al. (2013) | |||
| 25% storage | 158 Households | Nasir et al. (2012) | |||
| 35.2% | 572 University students | Zafar et al. (2008) | |||
| 10.8% storage | 158 Households | Haider and Thaver (1995) | |||
| Saudi Arabia | 48% | 353 School teachers | Belkina et al. (2014) | ||
| 11.6% for children | 610 Community Parents | Abobotain et al. (2013) | |||
| 5% | 1596 University and school students 88 Pharmacists | Almalak et al. (2014), Al‐Ghamdi (2001) | |||
| Syria | 85% | 365 Community participants | Barah and Goncalves (2010) | ||
| N/A | 200 pharmacists | Al‐Faham et al. (2011) | |||
| UAE | 40.2 | 300 University students | Suleiman and Rubian (2013) | ||
| 46% | 860 Community parents | Abasaeed et al. (2009) | |||
| 11.4% | 324 School students | Shehnaz et al. (2013) | |||
| Iraq | 26% | 300 Households | Jassim (2010) | ||
| Egypt | 23.3% | 884 Pharmacy customers | Sabry et al. (2014) | ||
| 30% | 300 Patients at clinics | Scicluna et al. (2009) | |||
| Kuwait | 27.50% | 680 Community participants | Awad and Aboud (2015) | ||
| Libya | 43% | 363 University students | Ghaieth et al. (2015) | ||
| 48% | 286 Patients at clinics | Scicluna et al. (2009) | |||
| Oman | 67% | 718 Community participants | Jose et al. (2013) | ||
| Yemen | 78.2% | 367 School teachers | Belkina et al. (2014) | ||
| 60% | 2000 Patients at clinics | Mohanna (2010) | |||
| Sudan | 48.10% | 1750 Households | Awad et al. (2005) | ||
| Tunisia | 20.00% | 264 Patients at clinics | Scicluna et al. (2009) | ||
| Antimalarial | 2 | Sudan | 43.4% | 1750 Households | Awad et al. (2005) |
| Yemen | Abdo‐Rabbo (2003) | ||||
| Topical Anesthetics | 2 | Iran | 80.5% | 390 Welders | Sharifi et al. (2013) |
| Saudi Arabia | Risco and Millar (1992) | ||||
| Topical Corticosteroids | 1 | Iraq | 7.90% | 1780 Patients at clinics | Al‐Dhalimi and Aljawahiry (2006) |
| Cough/cold products | 3 | Pakistan | N/A | 864 University students | Bano et al. (2012) |
| Jordan | N/A | 393 Pharmacists | Albsoul‐Younes et al. (2010) | ||
| Palestine | N/A | 864 University students | Sweileh et al. (2004) | ||
| Decongestants | 1 | Jordan | N/A | 393 Pharmacists | Albsoul‐Younes et al. (2010) |
| Laxatives | 1 | Palestine | N/A | 97 Pharmacists | Sweileh et al. (2004) |
| Sedatives/Hypnotics and Benzodiazepines | 3 | Jordan | N/A | 393 Pharmacists | Albsoul‐Younes et al. (2010) |
| United Arab Emirates | N/A | 324 School students | Shehnaz et al. (2013) | ||
| Jordan | N/A | 393 Pharmacists | Albsoul‐Younes et al. (2010) |
Analgesics
Codeine is usually supplied and consumed as codeine‐containing pain‐killer tablets that mostly also contain acetaminophen. Both acetaminophen–codeine tablets and tramadol tablets are prescription medicines, but many pharmacies sell them without a prescription (Zabihi et al. 2011). In Iran, Codeine‐containing tablets, especially acetaminophen–codeine tablets are among the most requested medicines as OTC (Zargarzadeh et al. 2008). Headache was the most common problem (Sarahroodi et al. 2012), and Sedighi showed that 91% of Iranian migraine sufferers used SM, mostly Acetaminophen and Codeine (Sedighi et al. 2006).
The prevalence of lifetime tramadol misuse among Iranian students was 4.7% (Nazarzadeh et al. 2014). This is due to easy accessibility from pharmacies without prescription. For instance, 56% of patients requesting for tramadol did not have a prescription (Zabihi et al. 2011).
Topical Anesthetics
Topical ocular anesthetics are commonly misused among Iranian welders: 80.5% declared that they had used topical anesthetics at least once during their working lives (Sharifi et al. 2013). All were Men. Mostly patients prefer self‐treatment over seeking help from a physician, for cultural and financial reasons. The most commonly used topical anesthetic was tetracaine (Sharifi et al. 2013). Topical ocular anesthetic misuse is associated with many harmful adverse effects. A case report stated a 40‐year‐old patient in Saudi Arabia frequently self‐administering topical oxybuprocaine drops had developed ocular ultrastructural alterations (Risco and Millar 1992).
Topical corticosteroids
Al‐Dhalimi showed that topical corticosteroids were commonly misused by 7.9% of Iraqi patients presenting at the dermatological center for lightening the skin or mild acne. The most commonly used topical steroids were potent and highly potent corticosteroids, including Clobetasole propionate and Betamethasone valerate. About half were aged 10–19 years. In 34.3% of cases, medical staff was responsible for recommending the medicines, including pharmacists (Al‐Dhalimi and Aljawahiry 2006).
Cough/cold products and laxatives
Sweileh et al. (2004) and Albsoul‐Younes et al. (2010) reported that antitussives, analgesics, antihistamines, decongestants, and laxatives were identified by pharmacists as misused medicines (Sweileh 2004). The antitussive products most misused were those containing the following combinations: (codeine phosphate/pseudoephedrine/triprolidine) (53.6%) or (ephedrine/ammonium chloride/ codeine phosphate/pheniramine maleate) (5.2%).
Antibiotics and antimalarials
Inappropriateness of antibiotic use is defined as suboptimal use of antibiotics to treat antibiotic‐responsive conditions, including use of overly broad agents, incorrect drug dosing or duration, and poor drug adherence (Sabry et al. 2014). Misuse of antibiotics is common in Eastern Mediterranean countries, with self‐medication rates ranging from 32% to 42% as reported in Lebanon (Cheaito et al. 2014) (Farah et al. 2015), and from 32% to 62%% in Jordanian studies (Darwish et al. 2014) (Scicluna et al. 2009); rates as high as 57.6% were reported in Iran (Heidarifar et al. 2013), in Emirates (56%) (Abasaeed et al. 2009), Syria (85%) (Barah and Goncalves 2010), Tunisia (20%) (Scicluna et al. 2009), and Yemen (60%) (Mohanna 2010). A percentage of 73.9 of Sudan population had used antibiotics or antimalarials without a prescription (Awad et al. 2005).
Antibiotic SM was common among university and school students in Palestine (98%) (Sawalha 2008), Libya (46%) (Ghaieth et al. 2015), United Arab Emirates (40%) (Sharifi et al. 2013), Saudi Arabia (48%) (Belkina et al. 2014), Pakistan (from 71.4% to 80.4%) (Aslam et al. 2013), and Iran (53%) (Sarahroodi and Arzi 2009). This practice was also observed among parents for their children. This practice was clear in Saudi Arabia (Darwish et al. 2014) and in the Scicluna study (Scicluna et al. 2009).
Respiratory tract symptoms were the main indication for which respondents indicated they would self‐medicate. Antibiotics were mainly used for treatment of sore throat, cough, and flu. These results were found in Iran (Heidarifar et al. 2013), Iraq (Jassim 2010), Jordan (Sawair et al. 2009), Kuwait (Awad and Aboud 2015), Libya (Ghaieth et al. 2015), Lebanon (Cheaito et al. 2014), Pakistan (Qazi et al. 2013), Egypt (Sabry et al. 2014), Tunisia (Scicluna et al. 2009), and Saudi Arabia (Belkina et al. 2014). Other reasons for self‐medication were for urinary tract infections (Scicluna et al. 2009) or gastrointestinal symptoms (Mohanna 2010).
Poor compliance with antibiotic therapy has a great impact on antibiotic misuse. Most patients did not complete the full course of antibiotic and took them for less than 3 days. This was observed in many Middle East countries and ranged from 39% to 86% as seen in Table 2. Reasons most frequently mentioned by patients for noncompliance were as follows: rapid improvement of symptoms, forgetfulness, and frequent dosing (Al‐Shammeri et al. 1995) .
Table 2.
Percentage of antibiotic compliance in the retrieved publications
| Countries | % Antibiotic Compliance | Study Setting | Reference |
|---|---|---|---|
| Jordan | 39% | 800 University students | Suaifan et al. (2012) |
| 40% | 508 Community participants | Darwish et al. (2014) | |
| Kuwait | 64% | 680 Community participants | Awad and Aboud (2015) |
| Iran | 37.10% | 542 Community participants | Heidarifar et al. (2013) |
| 26.80% | 564 University students | Sarahroodi and Arzi (2009) | |
| Libya | 86% | 363 University students | Ghaieth et al. (2015) |
| Oman | 29% | 718 Community participants | Jose et al. (2013) |
| 56% | 400 School teachers | Belkina et al. (2014) | |
| Pakistan | 42% | 780 University and school students | Aslam et al. (2013) |
| Saudi Arabia | 71.30% | 300 Households | Abobotain et al. (2013) |
| 61% | 1200 School teachers | Belkina et al. (2014) | |
| United Arab Emirates | 75% | 385 Women in clinics | Suleiman and Rubian (2013) |
The most common antibiotics used were amoxicillin or ampicillin among different Middle East countries including Libya, Tunisia, Egypt (Scicluna et al. 2009), United Arab Emirates (Abasaeed et al. 2009), Pakistan (Qazi et al. 2013), Iran (68.6%) (Heidarifar et al. 2013), and Jordan (Sawair et al. 2009). In Saudi Arabia, fluoroquinolones were the most commonly dispensed antibiotic for urinary tract infections (82%) (Al‐Ghamdi 2001). Amoxicillin–clavulanic acid was mostly used among Lebanese (48.9%) (Cheaito et al. 2014), among university students in United Arab Emirates, (48.9%) (Suleiman and Rubian 2013), and in Pakistan (62.8%) (Aslam et al. 2013). Metronidazole and TMP/SMX were also commonly used in Pakistan (29.2%) (Qazi et al. 2013) and in Yemen (35%) (Mohanna 2010) respectively.
Sources and reasons for self‐medication
People tended to select medication based mainly on advice received from community pharmacist (see Table 3). Ease in access to antibiotics and availability of pharmacist consultation were the main factors resulting in an increase in the use of antibiotics. Cheaito et al. (2014) reported that pharmacists were the main helpers for antibiotic self‐medication. Similar findings were in Sharif's study which showed that pharmacy was the main source of antibiotic self‐medication (slightly more than 90%) (Sharifi et al. 2013) and among Libyan students (75%) (Ghaieth et al. 2015).
Table 3.
Sources for Self‐Medication
| Sources of SM | Number of articles (n) | Country, % | References |
|---|---|---|---|
| Pharmacists | 23 | Egypt, 13.1%, 30% | Scicluna et al. (2009); Sabry et al. (2014) |
| Iran 18.6%, 30%, 44.8%, 61.2% | Sarahroodi and Arzi (2009), Heidarifar et al. (2013), Sharifi et al. (2013), Askarian and Maharlouie (2012) | ||
| Jordan 14.2%, 23.1%, 30%, 53.6%, 30% | Al‐Bakri et al. (2005), Yousef et al. (2008), Sawair et al. (2009)), Scicluna et al. (2009) | ||
| Lebanon 29.8%, 35% | Cheaito et al. (2014), Scicluna et al. (2009) | ||
| Libya 74%, 12% | Scicluna et al. (2009), Ghaieth et al. (2015) | ||
| Pakistan 33.49% | Qazi et al. (2013) | ||
| Yemen 55.1% | Belkina et al. (2014) | ||
| Saudi Arabia 21.6%, 74% | Alghanim (2011), Belkina et al. (2014) | ||
| Emirates 21.4%, 16.3%, 74% | Shehnaz et al. (2013, 2014a,b), Abasaeed et al. (2009), Mohanna (2010) | ||
| Iraq 18.6% | Al‐Dhalimi and Aljawahiry (2006) | ||
| Yemen N/A | Abdo‐Rabbo (2003) | ||
| Tunisia 12% | Scicluna et al. (2009) | ||
| Parents/Friends | 19 | Iran 0.6%, 6%, 54.7%, 40.1% | Sharifirad et al. (2011), Sarahroodi and Arzi (2009), Heidarifar et al. (2013), Sharifi et al. (2013), Nazarzadeh et al. (2014) |
| Jordan 51.8%, 10.3%, 12% | Sawair et al. (2009), Scicluna et al. (2009), Shehadeh et al. (2012) | ||
| Libya 26%, 11% | Scicluna et al. (2009), Ghaieth et al. (2015) | ||
| Pakistan 20.09% | Qazi et al. (2013) | ||
| Yemen 7.3% | Belkina et al. (2014) | ||
| Saudi Arabia 19.3%, 20.3% | Belkina et al. (2014), Alghanim (2011) | ||
| Emirates 20.2% | Shehnaz et al. (2013), Suleiman and Rubian (2013) | ||
| Iraq 20.7% | Al‐Dhalimi and Aljawahiry (2006) | ||
| Yemen N/A | Abdo‐Rabbo (2003) | ||
| Kuwait N/A | Abahussain et al. (2005) | ||
| Egypt 11% | Scicluna et al. (2009) | ||
| Lebanon 10% | Scicluna et al. (2009) | ||
| Tunisia 13% | Scicluna et al. (2009) | ||
| Physician advice or health professionals | 5 | Lebanon 50.8% | Cheaito et al. (2014) |
| Emirates 25.8% | Suleiman and Rubian (2013) | ||
| Jordan 21.9% | Yousef et al. (2008)) | ||
| Iran 27.2% | Sharifi et al. (2013) | ||
| Iraq 11.4% | Al‐Dhalimi and Aljawahiry (2006) | ||
| Dr. over phone | 1 | Jordan 37.5% | Suaifan et al. (2012) |
| Leftover | 10 | Iran 38.2%, 47.8%, 52% | Sarahroodi and Arzi (2009), Askarian and Maharlouie (2012), Heidarifar et al. (2013) |
| Iraq 45% | Jassim (2010) | ||
| Jordan 46%, 49%, 60% | Shehadeh et al. (2012), Suaifan et al. (2012), Darwish et al. (2014) | ||
| Lebanon 19.4% | Cheaito et al. (2014) | ||
| Emirates 1.1%, 28% | Suleiman and Rubian (2013), Abasaeed et al. (2009) | ||
| Stores at home for future use | 2 | Jordan 50% | Scicluna et al. (2009) |
| Tunisia 40% | Scicluna et al. (2009) | ||
| Libya 59% | Scicluna et al. (2009) | ||
| Lebanon 60% | Scicluna et al. (2009) | ||
| Egypt 40% Iraq 23% | Scicluna et al. (2009), Jassim (2010) | ||
| Self present based on: previous experience of symptoms or disease or knowledge | 6 | Emirates 27% | Suleiman and Rubian (2013) |
| Iran 30.1% 48.5%, 75% | Sarahroodi et al. (2012) | ||
| Jordan 27%, 53.1% | Yousef et al. (2008), Sawair et al. (2009) | ||
| Yemen 17.1% | (Belkina et al. 2014) | ||
| Saudi Arabia 31.6% | Belkina et al. (2014) | ||
| Previous treatment | 3 | Jordan 36.1%, 40% | Scicluna et al. (2009), Sawair et al. (2009) |
| Tunisia 45% | Scicluna et al. (2009) | ||
| Libya 48% | Scicluna et al. (2009) | ||
| Lebanon 88% | Scicluna et al. (2009) | ||
| Egypt 40% | Scicluna et al. (2009) | ||
| Iran N/A | Jalilian et al. (2013) | ||
| Previous suggestion by physician or Dr. always prescribe the same antibiotic | 2 | Iran 32.6% | Sarahroodi et al. (2010) |
| Lebanon 43% | Scicluna et al. (2009) | ||
| Egypt 11% | Scicluna et al. (2009) | ||
| Tunisia 21% | Scicluna et al. (2009) | ||
| Jordan 10% | Scicluna et al. (2009) | ||
| Libya 30% | Scicluna et al. (2009) | ||
| Old prescription | 3 | Yemen 20.6% | Belkina et al. (2014) |
| Saudi Arabia 27.5%, 50.8% | Alghanim (2011), Belkina et al. (2014) | ||
| Emirates 26% | Mohanna (2010) | ||
| Doctor prescription to friend | 1 | Emirates 3.4% | Suleiman and Rubian (2013) |
Another study reported that the most common sources of information on medicines were parents or friends. In Jordan, 51.8% of adult patients use antibiotic based on a relative's advice (Shehadeh et al. 2012). Similar results were reported in many other Middle East countries. Prescription of antibiotics by physicians over phone is also an important contributing factor.
Use of leftover antibiotics is a major source for antibiotic use. Many patients tended also to keep antibiotics at home either for future use or for prophylaxis against infections (Ullah et al. 2013). In this case, antibiotics could be used without physician consultation. In Scicluna et al. (2009) almost half of those interviewed admitted to having stored some type of antibiotic at home, which was not for current use.
The most common reasons for self‐medication were prior experience of the disease or similar symptoms (Al‐Azzam et al. 2007; James et al. 2008; Yousef et al. 2008; Zafar et al. 2008; Scicluna et al. 2009; Mumtaz et al. 2011; Jalilian et al. 2013), certainty of its safety, (Jalilian et al. 2013), prior consumption of the drug (Jalilian et al. 2013), busy offices of physicians (Jalilian et al. 2013; Shoaib et al. 2013), and nonseriousness of the illness (James et al. 2008; Yousef et al. 2008; Mumtaz et al. 2011; Jalilian et al. 2013; Shoaib et al. 2013) or low severity of disease (Ullah et al. 2013). Long waiting time to be seen by doctors (James et al. 2008; Yousef et al. 2008) and avoiding the cost of doctors’ visits were also reported as common reasons for self‐medication (Yousef et al. 2008).
Self‐medication was significantly associated with age, male gender, education level, and socioeconomic status. Young age, male, and having poor health status were more likely to practice self‐medication (Alghanim 2011; Syed et al. 2015).
Knowledge and attitudes of self‐medication
Knowledge of self‐medication is an important factor for drug misuse. In Egypt, 82.4% of the pharmacists considered the most common contributing factor for inappropriate self‐ medication use was lack of knowledge of patients/customers about the active ingredients in a branded product Elhoseeny et al. (2013). Tawfiq's study showed that more than 60% of the respondents did not try to read the leaflets of their medications (Al‐Tawfiq et al. 2010).
The knowledge and attitude toward antibiotics are important contributing factors in the misuse of these medications. There is a limited understanding of which infections might require antibiotics and the safety and risks of such misusage. For instance, one Jordan study showed that 67.1% of the public believed that antibiotics treat common cold and cough. A percentage of 28.1 misused antibiotics as analgesics (Shehadeh et al. 2012). Many patients thought they were used for viral infections (Alzoubi et al. 2013; Darwish et al. 2014). Better knowledge was found to be a predictor for positive attitudes (Awad and Aboud 2015).
Discussion
The current review summarizes a number of themes and data to inform understanding of self‐medication misuse in Eastern Mediterranean area. In addition, it highlights the different medicines involved in self‐medication misuse, their prevalence, and their practice in different settings. Apparently, the uncontrolled consumption and monitoring of consumption of medicines in the Middle East is one reason for SM. This all is probably because of the easy availability of such medicines without prescription. So, people could misuse analgesics containing codeine, despite the availability of alternative active OTC medications such s paracetamol or NSAIDs. However, they are available as prescription medicines in some developed countries. Similar findings are observed to that reported in many developed countries. For example, in England (Paxton and Chapple 1996) and Scotland (Matheson et al. 2002) 69% and 68.5% of pharmacists considered there to be some form of OTC medicine misuse in their pharmacies.
This review showed that regardless of the type of studied samples (driven from general population or selected subgroups of population) the reported prevalence of self‐medication misuse in Eastern Mediterranean countries is very high. Therefore, high prevalence of misuse seems to be a health challenge in the Middle East. However, much still remains undone in this area in Eastern Mediterranean area. Many important researches remained unexplored in different countries of Middle East.
The inappropriate use of antibiotic is risky. This may include the use of antibiotics beyond the scope of their indications to treat ailments unrelated to bacterial infections or using antibiotic with incorrect dosages for inappropriate period of time. As a result, most antibiotics are used in unnecessary cases that would mostly recover without any antibiotic. For instance, people may self‐medicate with antibiotic for treatment of mild ailments as throat or teeth symptoms, nasal congestion, cough, flu, and urinary discomfort. Although patients can use many alternative OTC medications as cough, decongestants, or antihistamine products for upper respiratory tract infections, many still prefer to use of antibiotics. Inappropriate use of antibiotics may eventually lead to antibiotic resistance.
The main sources for self‐medication were previously prescribed pharmaceuticals stored in the household and those purchased in pharmacies (Al‐Bakri et al. 2005). Prescribing of medicine based on Essential Medicine List formularies, information campaigns, and regulatory reinforcement might control or reduce SM misuse. In Chile, the prohibition of OTC sales of antibiotic and a simultaneous public education campaign had an immediate and significant impact on the acquisition of antibiotic from pharmacies (Abasaeed et al. 2009). Similarly, sales of antibiotic without prescription in Zimbabwe decreased when the law against over‐the‐counter sales was strictly enforced (Avorn and Solomon 2000).
The use of leftover medications is a unique consequence of poor compliance with medications including antibiotics because it affords the patient opportunities to self‐ medicate with a partial supply of antibiotics. Overprescription of antibiotics by physicians is also an important factor that increases patient self‐medication. Awareness and educational programs for physicians and consumers appear promising to control the overuse of antibiotics, noncompliance, and the use of leftovers.
Methodologically, studies are not standardized, which limits the quality of studies as well as comparability. Most of the studies were cross‐sectional descriptive studies often using self‐administered questionnaires, face‐to‐face interviews, or pharmacists’ perception. Many studies report data based on pharmacists’ perceptions of the problem of misuse and the profile of those they considered to be affected, such as reported by Albsoul‐Younes et al. (2010), Elhoseeny et al. (2013), or Sweileh et al. (2004). These study designs are similar to those conducted in Scotland (Paxton and Chapple 1996; Matheson et al. 2002). Although these studies may have high response rate, they are still subjective.
Like all literature reviews, and despite our best effort to use standard methodology for such reviews, the possibility of a selection bias cannot be excluded, even though we did search for local language papers that might have escaped other researchers. Lack of access to some of the databases in the field and to unpublished research reports was the main limitations in our attempt to shed light on OTC misuse behavior. Uninformative titles and abstracts are also a limitation. However, the main limitation in our analysis is the heterogeneous methodological nature and reporting of the studies. Even finding more studies hidden in obscure repositories would probably not have changed that conclusion. In addition, most studies were consistent and showed similar results on the widespread use of self‐medication, so that again missing studies would not change these results.
Conclusion
This review relating to self‐medication misuse has found a massive problem involving a range of medicines. Considerable attention should be paid to the risks of future expansion of inappropriate self‐medication. Better physician education of appropriate medication use is one approach that may encourage the prudent use of antimicrobial and other medicines. In addition, policy making should be implemented in Middle East area in order to restrict sales of prescription medications without prescription.
Authors Contribution
Malak Khalifeh had the original idea, did the literature search, and wrote the original manuscript. Nicholas Moore had the original idea, and edited/amended the manuscript. Pascale Salameh had the original idea, and edited/amended the manuscript. All authors read and approved the final manuscript as submitted.
Disclosures
The authors declare no conflicts of interest.
Acknowledgements
The authors thank the Lebanese university for funding this project.
Khalifeh M. M., Moore N. D., Salameh P. R.. Self‐medication misuse in the Middle East: a systematic literature review, Pharma Res Per, 5(4), 2017, e00323, https://doi.org/10.1002/prp2.323
References
- Abahussain E, Matowe LK, Nicholls PJ (2005). Self‐reported medication use among adolescents in Kuwait. Med Princ Pract 14: 161–164. [DOI] [PubMed] [Google Scholar]
- Abasaeed A, Vlcek J, Abuelkhair M, Kubena A (2009). Self‐medication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries 3: 491–497. [DOI] [PubMed] [Google Scholar]
- Abdo‐Rabbo A (2003). Household survey of treatment of malaria in Hajjah, Yemen. East Mediterr Health J 9: 600–606. [PubMed] [Google Scholar]
- Abobotain AH, Sheerah HA, Alotaibi FN, Joury AU, Mishiddi RM, Siddiqui AR, et al. (2013). Socio‐demographic determinants of antibiotic misuse in children. A survey from the central region of Saudi Arabia. Saudi Med J 34: 832–840. [PubMed] [Google Scholar]
- Al‐Azzam SI, Al‐Husein BA, Alzoubi F, Masadeh MM, Al‐Horani MA (2007). Self‐medication with antibiotics in Jordanian population. Int J Occup Med Environ Health 20: 373–380. [DOI] [PubMed] [Google Scholar]
- Al‐Bakri AG, Bustanji Y, Yousef AM (2005). Community consumption of antibacterial drugs within the Jordanian population: sources, patterns and appropriateness. Int J Antimicrob Agents 26: 389–395. [DOI] [PubMed] [Google Scholar]
- ALBashtawy M, Batiha AM, Tawalbeh L, Tubaishat A, AlAzzam M (2015). Self‐medication among school students. J Sch Nurs 31: 110–116. [DOI] [PubMed] [Google Scholar]
- Albsoul‐Younes A, Wazaify M, Yousef AM, Tahaineh L (2010). Abuse and misuse of prescription and nonprescription drugs sold in community pharmacies in Jordan. Subst Use Misuse 45: 1319–1329. [DOI] [PubMed] [Google Scholar]
- Al‐Dhalimi MA, Aljawahiry N (2006). Misuse of topical corticosteroids: a clinical study in an Iraqi hospital. East Mediterr Health J 12: 847–852. [PubMed] [Google Scholar]
- Al‐Faham Z, Habboub G, Takriti F (2011). The sale of antibiotics without prescription in pharmacies in Damascus, Syria. J Infect Dev Ctries 5: 396–399. [DOI] [PubMed] [Google Scholar]
- Al‐Ghamdi MS (2001). Empirical treatment of uncomplicated urinary tract infection by community pharmacist in the Eastern province of Saudi Arabia. Saudi Med J 22: 1105–1108. [PubMed] [Google Scholar]
- Alghanim SA (2011). Self‐medication practice among patients in a public health care system. East Mediterr Health J 17: 409–416. [PubMed] [Google Scholar]
- Almalak H, Albluwi AI, Alkhelb DA, Alsaleh HM, Khan TM, Hassali MA, et al. (2014). Students’ attitude toward use of over the counter medicines during exams in Saudi Arabia. Saudi Pharm J 22: 107–112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al‐Shammeri SA, Khoja T, Al‐Yamani MJ (1995). Compliance with Short‐term antibiotic therapy among patients attending primary health centres in Riyadh, Saudi Arabia. J Roy Soc Health 1995: 231–234. [DOI] [PubMed] [Google Scholar]
- Al‐Tawfiq JA, Stephens G, Memish ZA (2010). Inappropriate antimicrobial use and potential solutions: a Middle Eastern perspective. Expert Rev Anti Infect Ther 8: 765–774. [DOI] [PubMed] [Google Scholar]
- Alzoubi K, Al‐Azzam S, Alhusban A, Mukattash T, Al‐Zubaidy S, Alomari N, et al. (2013). An audit on the knowledge, beliefs and attitudes about the uses and side‐effects of antibiotics among outpatients attending 2 teaching hospitals in Jordan. East Mediterr Health J 19: 478–484. [PubMed] [Google Scholar]
- Askarian M, Maharlouie N (2012). Irrational antibiotic use among secondary school teachers and university faculty members in Shiraz, Iran. Int J Prev Med 3: 839–845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aslam M, Mirza TB, Muhammad AFS, Sarwat J (2013). Self‐Medication with Antibiotics among Secondary and Tertiary Level Students in Karachi, Pakistan: A Cross Sectional Study. Inventi Rapid: Pharmacy Practice 2013: 1–5. [Google Scholar]
- Avorn J, Solomon DH (2000). Cultural and economic factors that (mis)shape antibiotic use: the nonpharmacologic basis of therapeutics. Ann Intern Med 133: 128–135. [DOI] [PubMed] [Google Scholar]
- Awad AI, Aboud EA (2015). Knowledge, attitude and practice towards antibiotic use among the public in Kuwait. PLoS ONE 10: e0117910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awad A, Eltayeb I, Matowe L, Thalib L (2005). Self‐medication with antibiotics and antimalarials in the community of Khartoum State, Sudan. J Pharm Pharm Sci 8: 326–331. [PubMed] [Google Scholar]
- Baghianimoghadam MH, Mojahed S, Baghianimoghadam M, Yousefi N, Zolghadr R (2013). Attitude and practice of pregnant women regarding self‐medication in Yazd, Iran. Arch Iran Med 16: 580–583. [PubMed] [Google Scholar]
- Bano N, Najam R, Qazi F (2012). Irrational Drug Use based on self‐medication for some common clinical conditions in an educated population of Karachi. Pak J Med Sci 28: 359–362. [Google Scholar]
- Barah F, Goncalves V (2010). Antibiotic use and knowledge in the community in Kalamoon, Syrian Arab Republic: a cross‐sectional study. East Mediterr Health J 16: 516–521. [PubMed] [Google Scholar]
- Belkina T, Al Warafi A, Hussein Eltom E, Tadjieva N, Kubena A, Vlcek J (2014). Antibiotic use and knowledge in the community of Yemen, Saudi Arabia, and Uzbekistan. J Infect Dev Ctries 8: 424–429. [DOI] [PubMed] [Google Scholar]
- Blenkinsopp A, Bradley C (1996). Patients, society, and the increase in self medication. BMJ 312: 629–632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheaito L, Azizi S, Saleh N, Salameh P (2014). Assessment of self‐medication in population buying antibiotics in pharmacies: a pilot study from Beirut and its suburbs. Int J Public Health 59: 319–327. [DOI] [PubMed] [Google Scholar]
- Cooper RJ (2013). Over‐the‐counter medicine abuse ‐ a review of the literature. J Subst Use 18: 82–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darwish DA, Abdelmalek S, Abu Dayyih W, Hamadi S (2014). Awareness of antibiotic use and antimicrobial resistance in the Iraqi community in Jordan. J Infect Dev Ctries 8: 616–623. [DOI] [PubMed] [Google Scholar]
- Elhoseeny TA, Ibrahem SZ, Abo el Ela AM (2013). Opinion of community pharmacists on use of nonprescription medications in Alexandria, Egypt. J Egypt Public Health Assoc 88: 79–84. [DOI] [PubMed] [Google Scholar]
- Farah R, Lahoud N, Salameh P, Saleh N (2015). Antibiotic dispensation by Lebanese pharmacists: a comparison of higher and lower socio‐economic levels. J Infect Public Health 8: 37–46. [DOI] [PubMed] [Google Scholar]
- Ghaieth MF, Elhag SR, Hussien ME, Konozy EH (2015). Antibiotics self‐medication among medical and nonmedical students at two prominent Universities in Benghazi City, Libya. J Pharm Bioallied Sci 7: 109–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haider S, Thaver IH (1995). Self medication or self care: implication for primary health care strategies. J Pak Med Assoc 45: 297–298. [PubMed] [Google Scholar]
- Heidarifar R, Koohbor M, Kazemian MM, Mikaili P, Sarahroodi S (2013). Sef‐medication with Antibiotics among Iranian population in qom state. J Sci Innov Res 2: 785–789. [Google Scholar]
- Hughes GF, McElnay JC, Hughes CM, McKenna P (1999). Abuse/misuse of non‐prescription drugs. Pharm World Sci 21: 251–255. [DOI] [PubMed] [Google Scholar]
- Ibrahim NK, Alamoudi BM, Baamer WO, Al‐Raddadi RM (2015). Self‐medication with analgesics among medical students and interns in King Abdulaziz University, Jeddah, Saudi Arabia. Pak J Med Sci 31: 14–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jafari F, Khatony A, Rahmani E (2015). Prevalence of self‐medication among the elderly in Kermanshah‐Iran. Glob J Health Sci 7: 360–365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jalilian F, Hazavehei SM, Vahidinia AA, Jalilian M, Moghimbeigi A (2013). Prevalence and related factors for choosing self‐medication among pharmacies visitors based on health belief model in Hamadan Province, west of Iran. J Res Health Sci 13: 81–85. [PubMed] [Google Scholar]
- James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP (2006). Evaluation of the knowledge, attitude and practice of self‐medication among first‐year medical students. Med Princ Pract 15: 270–275. [DOI] [PubMed] [Google Scholar]
- James H, Handu SS, Khaja KA, Sequeira RP (2008). Influence of medical training on self‐medication by students. Int J Clin Pharmacol Ther 46: 23–29. [DOI] [PubMed] [Google Scholar]
- Jassim AM (2010). In‐home Drug Storage and Self‐medication with Antimicrobial Drugs in Basrah, Iraq. Oman Med J 25: 79–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jose J, Jimmy B, Alsabahi AG, Al Sabei GA (2013). A study assessing public knowledge, belief and behavior of antibiotic use in an omani population. Oman Med J 28: 324–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamat VR, Nichter M (1998). Pharmacies, self‐medication and pharmaceutical marketing in Bombay, India. Soc Sci Med 47: 779–794. [DOI] [PubMed] [Google Scholar]
- Lessenger JE, Feinberg SD (2008). Abuse of prescription and over‐the‐counter medications. J Am Board Fam Med 21: 45–54. [DOI] [PubMed] [Google Scholar]
- Matheson M, Bond CM, Pitcarin J (2002). Misuse of over‐the‐counter medicines from community pharmacies: a population survey of Scottish pharmacies. Pharm J 269: 66–68. [Google Scholar]
- Mohanna M (2010). Self‐medication with Antibiotic in Children in Sana'a City, Yemen. Oman Med J 25: 41–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mumtaz Y, Jahangeer A, Mujtaba T, Zafar SN (2011). Self Medication among University Students of Karachi. JLUMHS 10: 102–105. [Google Scholar]
- Nasir MA, Hashmi RI, Ahmad NS (2012). Drug utilization patterns in Rawalpindi and Islamabad, Pakistan. J Pak Med Assoc 62: 426–429. [PubMed] [Google Scholar]
- Nazarzadeh M, Bidel Z, Carson KV (2014). The association between tramadol hydrochloride misuse and other substances use in an adolescent population: phase I of a prospective survey. Addict Behav 39: 333–337. [DOI] [PubMed] [Google Scholar]
- Paxton R, Chapple P (1996). Misuse of over‐the‐counter medicines: a survey in one English county. Pharm J 256: 313–315. [Google Scholar]
- Qazi F, Bano N, Zafar SN, Shoaib M, Yousuf R (2013). Self‐medication of Antibiotics in Pharyngitis and Gastroenteritis‐ A Community Based Study in Karachi, Pakistan. Int J Pharm Sci Rev Res 21: 207–211. [Google Scholar]
- Risco JM, Millar LC (1992). Ultrastructural alterations in the endothelium in a patient with topical anesthetic abuse keratopathy. Ophthalmology 99: 628–633. [DOI] [PubMed] [Google Scholar]
- Sabry NA, Farid SF, Dawoud DM (2014). Antibiotic dispensing in Egyptian community pharmacies: an observational study. Res Social Adm Pharm 10: 168–184. [DOI] [PubMed] [Google Scholar]
- Sarahroodi S, Arzi A (2009). Self‐Medication practice with antibiotics, Is it a problem among Iranian Colledge Students in Tehran? J Biol Sci 9: 829–832. [Google Scholar]
- Sarahroodi S, Arzi A, Sawalha AF, Asthtarinezhad A (2010). Antibiotics Self‐Medication among Southern Iranian University Students. Int J Pharmacol 6: 48–52. [Google Scholar]
- Sarahroodi S, Maleki‐Jamshid A, Sawalha AF, Mikaili P, Safaeian L (2012). Pattern of self‐medication with analgesics among Iranian University students in central Iran. J Family Community Med 19: 125–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawair FA, Baqain ZH, Abu Karaky A, Abu Eid R (2009). Assessment of self‐medication of antibiotics in a Jordanian population. Med Princ Pract 18: 21–25. [DOI] [PubMed] [Google Scholar]
- Sawalha AF (2008). A descriptive study of self‐medication practices among Palestinian medical and nonmedical university students. Res Social Adm Pharm 4: 164–172. [DOI] [PubMed] [Google Scholar]
- Scicluna EA, Borg MA, Gur D, Rasslan O, Taher I, Redjeb SB, et al. (2009). Self‐medication with antibiotics in the ambulatory care setting within the Euro‐Mediterranean region; results from the ARMed project. J Infect Public Health 2: 189–197. [DOI] [PubMed] [Google Scholar]
- Sedighi B, Ghaderi‐Sohi S, Emami S (2006). Evaluation of self‐medication prevalence, diagnosis and prescription in migraine in Kerman, Iran. Neurosciences (Riyadh) 11: 84–87. [PubMed] [Google Scholar]
- Sharifi A, Sharifi H, Karamouzian M, Mokhtari M, Esmaeili HH, Nejad AS, et al. (2013). Topical ocular anesthetic abuse among Iranian welders: time for action. Middle East Afr J Ophthalmol 20: 336–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharifirad G, Pirzadeh A, Azadbakht L (2011). Knowledge and practice in association with self‐medication of nutrient supplements, herbal and chemical pills among women based on Health Belief Model. J Res Med Sci 16: 852–853. [PMC free article] [PubMed] [Google Scholar]
- Shehadeh M, Suaifan G, Darwish RM, Wazaify M, Zaru L, Alja'fari S (2012). Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J 20: 125–133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehnaz SI, Khan N, Sreedharan J, Issa KJ, Arifulla M (2013). Self‐medication and related health complaints among expatriate high school students in the United Arab Emirates. Pharm Pract (Granada) 11: 211–218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shehnaz SI, Agarwal AK, Khan N (2014a). A systematic review of self‐medication practices among adolescents. J Adolesc Health 55: 467–483. [DOI] [PubMed] [Google Scholar]
- Shehnaz SI, Khan N, Sreedharan J, Arifulla M (2014b). Drug knowledge of expatriate adolescents in the United Arab Emirates and their attitudes towards self‐medication. Int J Adolesc Med Health 26: 423–431. [DOI] [PubMed] [Google Scholar]
- Shoaib M, Yousuf R, Anjum F, Saeed L, Ghayas S, Ali T, Seddiqui S, Alam S, Rizvi M, Ahmed M, Zaib‐un‐Nisa (2013). Survey based study on the use of nonprescription drugs among pharamcists and non‐pharmacists. Afr J Pharm Pharmacol 38: 554–559. [Google Scholar]
- Sturm AW, van der Pol R, Smits AJ, van Hellemondt FM, Mouton SW, Jamil B, et al. (1997). Over‐the‐counter availability of antimicrobial agents, self‐medication and patterns of resistance in Karachi, Pakistan. J Antimicrob Chemother 39: 543–547. [DOI] [PubMed] [Google Scholar]
- Suaifan G, Shehadeh M, Darwish DA, Al‐ljel H, Al‐Motassem Y, Rula D (2012). A cross sectional study on knowledge, attitude, and Behaviour related to antibiotic use and resistanc among medical and non‐medical university students in Jordan. Afr J Pharm Pharmacol 10: 763–770. [Google Scholar]
- Suleiman I, Rubian S (2013). Antibiotics use with and without a prescription in healthcare students. Am J Pharmacol Sci 5: 96–99. [Google Scholar]
- Sweileh W (2004). Self‐Medication and Over‐The‐Counter Practices: a Study in Palestine. J Al‐Aqsa Unv 8: 1–9. [Google Scholar]
- Sweileh WM, Arafat RT, Al‐Khyat LS, Al‐Masri DM, Jaradat NA (2004). A pilot study to investigate over‐the‐counter drug abuse and misuse in Palestine. Saudi Med J 25: 2029–2032. [PubMed] [Google Scholar]
- Syed M, Mehreen F, Lubna A (2015). Self‐medication among downtown urban population of karachi, pakistan. Indian J Med Res Pharm Sci 4: 2349–5340. [Google Scholar]
- Ullah H, Khan SA, Ali S, Karim S, Baseer A, Chohan O, et al. (2013). Evaluation of self‐medication amongst university students in Abbottabad, Pakistan; prevalence, attitude and causes. Acta Pol Pharm 70: 919–922. [PubMed] [Google Scholar]
- Wazaify M, Shields E, Hughes CM, McElnay JC (2005). Societal perspectives on over‐the‐counter (OTC) medicines. Fam Pract 22: 170–176. [DOI] [PubMed] [Google Scholar]
- Yousef AM, Al‐Bakri AG, Bustanji Y, Wazaify M (2008). Self‐medication patterns in Amman, Jordan. Pharm World Sci 30: 24–30. [DOI] [PubMed] [Google Scholar]
- Zabihi E, Hoseinzaadeh A, Emami M, Mardani M, Mahmoud B, Akbar MA (2011). Potential for tramadol abuse by patients visiting pharmacies in northern iran. Subst Abuse 5: 11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zafar SN, Syed R, Waqar S, Zubairi AJ, Vaqar T, Shaikh M, et al. (2008). Self‐medication amongst university students of Karachi: prevalence, knowledge and attitudes. J Pak Med Assoc 58: 214–217. [PubMed] [Google Scholar]
- Zargarzadeh AH, Minaeiyan M, Torabi A (2008). Prescription and nonprescription drug use in isfahan, Iran: an observational, cross‐sectional study. Curr Ther Res Clin Exp 69: 76–87. [DOI] [PMC free article] [PubMed] [Google Scholar]


