Abstract
Background
The aim of the study was to assess the efficacy of balloon angioplasty-assisted mechanical thrombectomy without urgent stenting in the carotid artery as another approach for endovascular treatment of tandem occlusions.
Methods
Fifteen consecutive cases of tandem occlusions treated with the endovascular approach between January 2014 and May 2016 were reviewed. The study cohort included patients with an etiology of large vessel atherosclerosis. Extracranial carotid stenting was performed in another session if post-thrombectomy mRS modified Rankin Score (mRS) was 0–2. Good clinical outcome was determined by follow-up at 7–10, 30 and 90 days according to the mRS.
Results
Most patients (80%) were male. Eight (53.4%) patients received intravenous thrombolysis before angiography. Proximal revascularization was successful in 100% of cases with balloon angioplasty internal carotid artery (ICA) origin. Successful recanalization (modified thrombolysis in cerebral infarction (mTICI) 2b-3) (mTICI 2 b–3) occurred in 12 cases (80%) and good clinical outcomes were achieved in 10 patients (66.7%). Cervical ICA stent placement was performed in 10 patients with good clinical outcomes. No symptomatic intracranial hemorrhage occurred after delayed ICA stenting
Conclusions
This is the first reported case series to evaluate this approach for endovascular treatment of tandem occlusions. Carotid angioplasty-assisted mechanical thrombectomy without urgent stenting seems to be a safer approach.
Keywords: Acute stroke, angioplasty-assisted mechanical thrombectomy, carotid angioplasty, interventional neurology, tandem occlusion
Introduction
Tandem occlusion refers to simultaneous proximal extracranial occlusion in conjunction with a downstream intracranial occlusion (terminal internal carotid artery (ICA) or/and middle cerebral artery (MCA)).1 In a study, the frequency of anterior circulation tandem occlusion was reported as 10.5%.2 Tandem occlusions complicate the thrombectomy procedure and prolong the duration of intervention. The rate of successful recanalization in tandem occlusion with intravenous tissue plasminogen activator is reported as 5.9%.2,3 Good clinical outcomes (mRS 0–2) and high recanalization rates can be achieved by adding mechanical thrombectomy to intravenous tissue plasminogen activator in these cases.3 The endovascular approach applied to tandem occlusion cases varies from center to center. In some centers, the anterograde approach (balloon angioplasty, stenting and mechanical thrombectomy) is used,4–18 and in others, a retrograde approach (balloon angioplasty, mechanical thrombectomy and stenting) is used.16–22 Unlike other reports, in our study, balloon angioplasty alone was performed to maintain access in occluded extracranial ICA, followed by mechanical thrombectomy of the distal occlusions (terminal ICA, MCA or anterior cerebral artery (ACA)). The decision for extracranial ICA stenting was based on the findings of post-thrombectomy unenhanced control brain computed tomography scans and clinical outcomes. The aim of this study was to discuss the efficacy of this approach for endovascular treatment of tandem occlusions.
Methods
Study design
This was a retrospective study involving the prospectively and consecutively collected data of 15 patients. We analyzed consecutive patients with acute ischemic stroke due to extracranial ICA occlusion and a concomitant occlusion in either terminal ICA occlusion, MCA or ACA at Ankara Numune Training and Research Hospital from January 2014 to May 2016. Tandem occlusion was demonstrated on admission by cranial computed tomography angiography and confirmed by catheter angiography. In this study, all proximal occlusions were treated by lone balloon angioplasty, and all distal embolic occlusions were treated with mechanical thrombectomy.
This study was approved by the institutional research ethics board.
Patient selection criteria
The inclusion criteria were tandem occlusion within the anterior circulation and age 18–82. Endovascular treatment was performed within 6 h of symptom onset in patients with a National Institutes of Health Stroke Scale score of ≥6 upon presentation to the emergency department.
Patients were excluded from endovascular stroke treatment if they had minor focal, neurologic deficit with a National Institutes of Health Stroke Scale score of < 6 or if early signs of an advanced infarction (more than one-third of the MCA territory) were present on non-enhanced computed tomography imaging. Patients with intracranial hemorrhage or subdural hematoma were excluded. Also, patients known to have a pre-stroke score > 2 on the mRS, which could affect the outcome, or tandem occlusions due to dissection or floating thrombus in the ICA were excluded from the analysis.
Eight patients, presenting within 4.5 h from symptom onset and without contraindication to systemic thrombolysis, were immediately treated with intravenous tissue plasminogen activator (iv-tPA) (0.9 mg/kg) before being immediately transferred to the angiography unit. Five patients who presented between 4.5 and 6 h after symptom onset and two patients who had contraindication to systemic thrombolysis did not receive iv-tPA.
Imaging
Cranial Computed tomography was performed on admission to rule out intracerebral hemorrhage (ICH), and cranial computed tomography angiography was performed to determine the site of occlusion and assess the collateral scoring. Control cranial computed tomography scans were acquired 24 h after treatment, and also, if ICH was detected, cranial computed tomography scanning was repeated 7–10 days before stenting.
Symptomatic ICH was defined as clinical deterioration of > 4 points on the National Institutes of Health Stroke Scale score.
Collateral supply was evaluated as absent, poor, moderate or good based on the ratio of the area of parenchyma supplied by collateral circulation to the target territory.23
Follow-up clinical assessment
Successful revascularization was defined as post-treatment mTICI score 2b–3. An mRS of 0 to 2 was defined as a good functional outcome. Neurologic evaluation was performed on admission with the National Institutes of Health Stroke Scale. The mRS was assessed by stroke neurologists at 7–10, 30 and 90 days after treatment.
Endovascular procedure
The femoral artery was punctured under local anesthesia and a femoral sheath was placed. The 5 F femoral sheath was changed to a 6 Fr 90 cm guiding sheath (Destination™, Terumo, Tokyo, Japan) and placed distal to the common carotid artery (CCA). After sheath placement, 40 U/kg heparin was administered. In all cases, a triaxial system was used. The extracranial ICA total occlusion was initially passed with a 0.014 inch micro-guide wire (Hi-torque whisper MS Guide Wire™, Abbott Vascular, Abbott Park, IL, USA) and pre-dilatation was performed using a 3.0 or 3.5 mm balloon catheter. Control angiography was performed through the guiding sheath to assess ICA patency. If there was a residual re-stenosis, balloon angioplasty was repeated. Once adequate patency was maintained, a distal access catheter (Navien™ Intra Cranial Support Catheter with 0.058 inch distal inner diameter, ev3-Medtronic, Neurovascular, Irvine, California, USA) was advanced to the distal segments of the ICA over a microcatheter (Rebar™ Reinforced Micro Catheter with 0.027 inch distal inner diameter, ev3-Medtronic, Neurovascular, Irvine, California, USA) and hydrophilic guidewire. After placement of the microcatheter distal to the thrombus, the stent retriever (Preset™, Phenox GmbH, Bochum, Germany or Solitaire FR™, ev3-Medtronic, Neurovascular, Irvine, California, USA) was advanced through the microcatheter. The microcatheter was then pulled back until the stent retriever was completely unfolded. Afterward, the device was pulled back under negative suction into the distal access catheter, which was placed in the distal ICA.
Extracranial ICA stenting
Carotid stenting was performed in 10 patients within 7–10 days and was performed in two patients within 30 days. A 6 Fr guiding catheter was advanced to the CCA. A distal protection device (Spider device, ev3, Plymouth, MN, USA) was placed in the distal cervical or petrous segment of the ICA. Then, a self-expandable stent was advanced and deployed along the stenosis. Post-dilatation with a balloon catheter was performed in all cases.
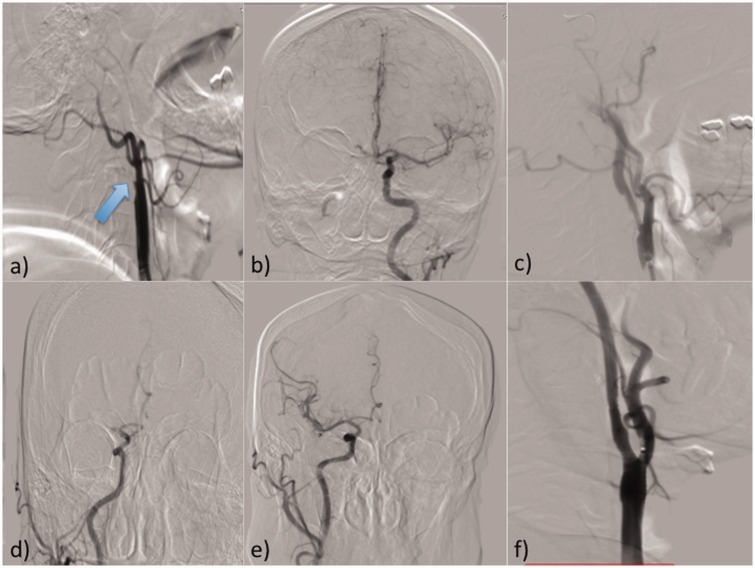
Angiographic images of a case example are presented in Figure 1.
Figure 1.
Treatment steps of the right tandem occlusion.
(a) Right CCA injection; arrow indicates the origin of proximally occluded right ICA; (b) left CCA injection showing blockage of contrast passage to right MCA due to occlusion; (c) right CCA injection after balloon angioplasty; (d) right CCA injection demonstrating right MCA M1 proximal occlusion; (e) right CCA injection demonstrating recanalization of right MCA after successful thrombectomy; (f) stent placement to right ICA 1 week after thrombectomy procedure.
Antiplatelet regimen
Dual antiplatelet therapy was initiated with a dose of 75 mg clopidogrel and 100 mg aspirin at least 5 days before stenting in patients with no ICH. In patients with asymptomatic ICH, resorption was confirmed by repeated non-contrast brain computed tomography, and after resorption of ICH, a loading dose of 600 mg clopidogrel plus 300 mg aspirin was administered prior to ICA stenting. Following stent placement, dual antiplatelet therapy was continued as 75 mg of clopidogrel and 100 mg of aspirin daily for 3 months.
Results
Fifteen patients, including 3 women and 12 men, with concomitant extracranial carotid lesions and intracranial embolism (terminal ICA, MCA, anterior cerebral artery), with a mean age of 62.2 ± 11 years (range from 44 to 77 years, median 61 years) were included. The mean National Institutes of Health Stroke Scale score upon admission was 13 ± 4 (range 7–20, median 12).
All patients were treated with balloon angioplasty-assisted thrombectomy. All carotid occlusions were due to atherosclerotic plaque formation. Proximal revascularization was successful in 100% of cases with balloon angioplasty of ICA origin without urgent stenting. Successful recanalization occurred in 12 cases (80%) and good clinical outcomes were achieved in 10 patients (66.7%).
Following thrombectomy, asymptomatic ICH was seen in six patients, and symptomatic ICH was seen in one patient.
Extracranial ICA stenting was performed in 10 (66.4%) of the 15 patients. Stenting was performed according to good clinical outcome (mRS 0–2) in 10 patients within 7–10 days and in 2 patients within 30 days. Five patients were not appropriate for extracranial carotid stenting due to high mRS, and in this group one patient died due to symptomatic intracranial hemorrhage 2 days after thrombectomy. No intracranial hemorrhage or cerebral hyperperfusion syndrome occurred after stenting. Table 1 summarizes baseline demographic, clinical and procedural data.
Table 1.
Clinical, demographic and procedural data of all patients.
| Number of patients (n) | 15 |
| Age, mean ± SD (min.–max.) | 62.2 ± 11 (44–77) |
| Sex (F/M) n (%) | 3/12 (20/80) |
| iv-tPA n (%) | 8 (53.4) |
| Basal NIHSS at admission (mean ± SD) (min.–max.) | 13 ± 4 (7–20) |
| Time between symptom onset and groin puncture (minutes), mean ± SD (min.–max., median) | 168 ± 46 (90–330, 170) |
| Recanalization time (minutes), mean ± SD (min.–max., median) | 69 ± 39 (40–150, 75) |
| Tandem occlusion (n (%)) | 15 (100) |
| Right extracranial ICA–MCA (n (%)) | 8 (53.3) |
| Right extracranial ICA–terminal ICA (n (%)) | 2 (13.3) |
| Left extracranial ICA–MCA (n (%)) | 3 (20) |
| Left extracranial ICA–terminal ICA (n (%)) | 1 (6.7) |
| Left extracranial ICA–Terminal ICA–MCA–ACA (n (%)) | 1 (6.7) |
| Proximal recanalization rate with only balloon angioplasty (n (%)) | 15 (100) |
| Distal recanalization rate (mTICI 2b–3) (n (%)) | 11 (73.3) |
| Extracranial ICA stenting within 7–10 days (n (%)) | 8 (53.3) |
| Extracranial ICA stenting within 30 days (n (%)) | 2 (13.3) |
| 7–10-day clinical outcome mRS 0–2 (n (%)) | 8 (53.3) |
| 30-day clinical outcome mRS 0–2 (n (%)) | 10 (66.7) |
| 90-day clinical outcome mRS 0–2 (n (%)) | 10 (66.7) |
| 90-day clinical outcome mRS 6 (n (%)) | 1 (6.7) |
| Micro guide wire-related complication (n (%)) | 1 (6.7) |
| Hemorrhage (post-procedure) (n (%)) | 5 (33.3) |
| Asymptomatic ICH (n (%)) | 4 (26.6) |
| Symptomatic ICH (n (%)) | 1 (6.6) |
| Post-stenting hemorrhage | 0 |
NIHSS: National Institutes of Health Stroke Scale.
No dissection in the angioplasty performed ICA segment, no ipsilateral recurrent stroke and no ipsilateral cervical carotid reocclusion was seen in the time period between mechanical thrombectomy and extracranial ICA stenting.
Discussion
The mechanical thrombectomy procedure was performed after sufficient patency was obtained by intervention via extracranial ICA occlusion with balloon angioplasty. Following mechanical thrombectomy, stenting of the extracranial internal carotid lesions was performed in cases with mRS 0–2. The rationale for delayed stenting in our study is that stenting was postponed until the patient’s good functional outcome and absence of parenchymal hemorrhage were confirmed.
In this way, futile stenting together with development of cerebral hemorrhage or expansion of an existing hemorrhage due to unnecessary antiaggregant use would be prevented. To the best of our knowledge, this report is the first to evaluate this treatment approach.
The number of articles regarding endovascular approaches for the treatment of tandem occlusion has continued to increase over the past few years. Stent-assisted mechanical thrombectomy was performed in these reports in two different ways: (i) balloon angioplasty and extracranial ICA stenting followed by mechanical thrombectomy (anterograde approach)4–18 or (ii) extracranial ICA stenting (retrograde approach)16–22 after balloon angioplasty and mechanical thrombectomy of the distal artery. There is only a limited number of reports in which carotid balloon angioplasty was performed without stenting followed by mechanical thrombectomy in acute phase (there is no data in these reports whether carotid stenting was performed or not),8,22,24 and there is no study in which balloon angioplasty-assisted mechanical thrombectomy was performed initially followed by extracranial carotid stenting in another session.
The rate of successful recanalization of intravenous tissue plasminogen activator is reported as 7%–9% for tandem occlusions.4,25,26
A meta-analysis of mechanical thrombectomy performed using a stent retriever combined with intravenous tissue plasminogen activator reported a successful recanalization rate of 73%–89%27 (Table 2). However, in two studies only, this rate increased to 100%.11,14 In the present study, the successful recanalization rate was 73.3% with the combined use of intravenous tissue plasminogen activator in 53.4% of the cases.
Table 2.
Studies of endovascular treatment assisted by balloon angioplasty in acute stroke with tandem occlusion.
| Patients (n) | Urgent extracranial ICA stenting (n) | iv-tPA (%) | mTICI 2b–3 (%) | mRS 0–2 (%) | asymptomatic ICH aICH (%) | symptomatic ICH sICH (%) | Mortality (%) | |
|---|---|---|---|---|---|---|---|---|
| Malik6 | 77 | 76 | NA | 75.3 | 41.6 | 5.1 | 5.1 | 24.7 |
| Steglich-Arnholm21 | 47 | 47 | 85 | 87 | 68 | 39 | 4 | 9 |
| Maurer13 | 43 | 38 | 74.4 | 76.7 | 32.6 | 11.6 | 2.3 | 20.9 |
| Mpotsaris8 (stenting group) | 17 | 17 | 82.3 | 94.2 | 41.2 | NA | 5.8 | 23.5 |
| Mpotsaris8 (without stenting group) | 24 | 0 | 83.3 | 79.2 | 33.4 | NA | 8.3 | 20.8 |
| Lescher22 (stenting group) | 9 | 9 | 78 | 56 | 33 | NA | 0 | 33.3 |
| Lescher22 (without stenting group) | 30 | 0 | 73 | 67 | 37 | NA | 10 | 3.1 |
| Lockau17 | 37 | 37 | 54.1 | 72.9 | 45.9 | 5.4 | 10.8 | 18.9 |
| Kwak7 | 35 | 35 | 22.9 | 74.3 | 62.9 | NA | 2.9 | 11.4 |
| Puri16 | 28 | 28 | 39.2 | 71.4 | 56.5 | 36.4 | 7.1 | 14 |
| Cohen12 | 24 | 24 | 30.4 | 79.2 | 76 | 25 | 0 | 8.3 |
| Stampfl9 | 24 | 24 | 41.6 | 62.5 | 33.3 | NA | 16.6 | 16.6 |
| Heck and Brown10 | 23 | 23 | 30.4 | 73.9 | 52.1 | NA | 21.7 | 39.1 |
| Dorado20 | 20 | 13 | 50 | 95.8 | 30.4 | 45.8 | 20.8 | 16.7 |
| Spiotta11 | 16 | 16 | 50 | 100 | 56.3 | 50 | 12.5 | 18.7 |
| Mishra14 | 7 | 7 | 28.5 | 100 | 85.7 | 29 | 0 | 0 |
| Cohen18 | 7 | 7 | 0 | 85.7 | 71.4 | NA | 14.2 | 14.2 |
| Shao15 | 6 | 6 | 16.6 | 83.3 | 16.6 | 33.3 | 0 | 16.6 |
In the same meta-analysis, good clinical outcomes were achieved in 33%–55% of cases,27 and this rate has increased to 85% in more recent publications12,14,18 (Table 2). In our study, good clinical outcome was achieved in 66.7% of the cases. One of the most important factors in achieving a good clinical outcome is the presence of collateral circulation. When cases with mild, moderate and good collateral circulation were included in our cases, we reached good clinical outcomes in 10 patients among 11 TICI 2b or 3 recanalized patients on the 90th day. As we decided to perform stenting based on the results of post-thrombectomy cranial brain computed tomography and functional outcome status, we aimed to prevent futile stenting. Since the leptomeningeal anastomoses are important for viability of the penumbratic target territory, in our opinion, all these patients had well-developed leptomeningeal anastomosis as a result of slowly developing atherosclerotic stenosis of the extracranial ICA. Thus, good clinical outcome was achieved in 66.7% of patients.
In a meta-analysis evaluated by Sivan-Hoffmann et al.,27 acute ICA stenting was performed in 193 of 237 patients and the symptomatic bleeding rate was reported to vary from 8% to 20% (Table 2). In a study conducted with a limited number of cases, hemorrhagic complications were not reported,4 while the symptomatic bleeding rate was reported as 22% in another study.10
Mpotsaris et al.8 reported that there was no increase in symptomatic bleeding among patients with and without stenting. Interestingly, in a study reported by Lescher et al.,22 no bleeding was observed in the stenting group, while bleeding was reported in 13% of cases in the non-stenting group. Dorado et al.20 reported significantly lower rates of parenchymal hemorrhage, symptomatic intracranial hemorrhage and mortality in the non-stenting group as compared with the stenting group (33.6%, 2.5% and 5% vs. 45.8%, 20.8% and 16.7%, respectively).
The risk of intracranial hemorrhage was known to be increased in cases that received intravenous thrombolytic treatment before mechanical thrombectomy, which is augmented by the addition of dual antiplatelet treatment. This is one of the most important problems caused by stent-assisted mechanical thrombectomy in tandem occlusion cases. Another problem is that stent thrombosis can develop if dual antiaggregant treatment cannot be continued in cases of symptomatic or asymptomatic intracranial hemorrhage. Dual antiaggregant treatment could safely be started in our cases after control brain computed tomography scans revealed no intracranial hemorrhage on days 7–10. Therefore, we did not experience hemorrhagic problems in our cases. Also, unnecessary stenting could be prevented by considering the patient’s status in terms of radiological and clinical outcomes.
Another important problem is the risk of recurrent stroke due to downstream emboli in the period between mechanical thrombectomy and stenting. In our series, we did not observe such embolic problems in this period. In the literature, we found no clinical follow-up information in cases where only balloon angioplasty-assisted mechanical thrombectomy was performed without stenting.
In a recent pooled analysis by Johansson et al., they found high risk (11.5% at 14 days) of recurrent ipsilateral ischemic events in symptomatic carotid stenosis patients within the 14-day time period currently recommended for carotid endarterectomy. The reason why we did not experience recurrent ipsilateral ischemic events may be due to either stabilization of the carotid plaque by balloon angioplasty or the small number of cases included in the study.28
Dorado et al.20 suggested avoiding urgent stent placement in the extracranial ICA for endovascular treatment of acute tandem occlusion because of the high rate of intracranial hemorrhage due to delayed reperfusion and the use of intra-arterial antithrombotic treatment, whereas Heck and Brown10 recommended balloon angioplasty to reach the intracranial vessel in cases of tandem occlusion and suggested stenting only for cases where sufficient patency cannot be obtained in the acute setting.
Other disadvantages of stent-assisted mechanical thrombectomy are increased complexity of the endovascular procedure, prolonged recanalization time, and the risk of jailing of instruments among stent struts, especially with the anterograde approach, which can be easily halted with the use of a distal access catheter.
Some studies have reported that the recanalization duration was longer in the stenting group,8,9,20 while some studies reported no time delay for cases with stenting.22
The limitations of this study are; it was performed in a single center, it was non-randomized and retrospective, and included a relatively small number of cases. Another defect of this study is the lack of randomized groups comparing delayed stenting with urgent stenting.
Conclusion
The results of this study demonstrated that balloon angioplasty-assisted mechanical thrombectomy and extracranial stenting in different sessions can be a safer approach for the endovascular treatment of tandem occlusions. With this approach, futile stenting and occurrence of hemorrhagic complications can be avoided.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Rubiera M, Ribo M, Delgado-Mederos R, et al. Tandem internal carotid artery/middle cerebral artery occlusion: An independent predictor of poor outcome after systemic thrombolysis. Stroke 2006; 37: 2301–2305. [DOI] [PubMed] [Google Scholar]
- 2.Grigoryan M, Haussen DC, Hassan AE, et al. Endovascular treatment of acute ischemic stroke due to tandem occlusions: Large multicenter series and systematic review. Cerebrovasc Dis 2016; 41: 306–312. [DOI] [PubMed] [Google Scholar]
- 3.Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. [DOI] [PubMed] [Google Scholar]
- 4.Miyamoto N, Naito I, Takatama S, et al. Urgent stenting for patients with acute stroke due to atherosclerotic occlusive lesions of the cervical internal carotid artery. Neurol Med Chir 2008; 48: 49–55. [DOI] [PubMed] [Google Scholar]
- 5.Roth C, Papanagiotou P, Behnke S, et al. Stent-assisted mechanical recanalization for treatment of acute intracerebral artery occlusions. Stroke 2010; 41: 2559–2567. [DOI] [PubMed] [Google Scholar]
- 6.Malik AM, Vora NA, Lin R, et al. Endovascular treatment of tandem extracranial/intracranial anterior circulation occlusions: Preliminary single-center experience. Stroke 2011; 42: 1653–1657. [DOI] [PubMed] [Google Scholar]
- 7.Kwak HS, Hwang SB, Jin GY, et al. Predictors of functional outcome after emergency carotid artery stenting and intra-arterial thrombolysis for treatment of acute stroke associated with obstruction of the proximal internal carotid artery and tandem downstream occlusion. AJNR Am J Neuroradiol 2013; 34: 841–846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mpotsaris A, Bussmeyer M, Buchner H, et al. Clinical outcome of neurointerventional emergency treatment of extra- or intracranial tandem occlusions in acute major stroke: Antegrade approach with wallstent and solitaire stent retriever. Clin Neuroradiol 2013; 23: 207–215. [DOI] [PubMed] [Google Scholar]
- 9.Stampfl S, Ringleb PA, Mohlenbruch M, et al. Emergency cervical internal carotid artery stenting in combination with intracranial thrombectomy in acute stroke. AJNR Am J Neuroradiol 2014; 35: 741–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heck DV, Brown MD. Carotid stenting and intracranial thrombectomy for treatment of acute stroke due to tandem occlusions with aggressive antiplatelet therapy may be associated with a high incidence of intracranial hemorrhage. J NeuroIntervent Surg 2015; 7: 170–175. [DOI] [PubMed] [Google Scholar]
- 11.Spiotta A, Lena J, Vargas J, et al. Proximal to distal approach in the treatment of tandem occlusions causing an acute stroke. J NeuroInterv Surg 2015; 7: 164–169. [DOI] [PubMed] [Google Scholar]
- 12.Cohen JE, Gomori JM, Rajz G, et al. Extracranial carotid artery stenting followed by intracranial stent-based thrombectomy for acute tandem occlusive disease. J NeuroIntervent Surg 2015; 7: 412–417. [DOI] [PubMed] [Google Scholar]
- 13.Maurer CJ, Joachimski F, Berlis A. Two in one: Endovascular treatment of acute tandem occlusions in the anterior circulation. Clin Neuroradiol 2015; 25: 397–402. [DOI] [PubMed] [Google Scholar]
- 14.Mishra A, Stockley H, Goddard T, et al. Emergent extracranial internal carotid artery stenting and mechanical thrombectomy in acute ischaemic stroke. Interv Neuroradiol 2015; 21: 205–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shao Q, Zhu L, Li T, et al. Management of tandem internal carotid and middle cerebral arterial occlusions with endovascular multimodal reperfusion therapy. Int J Neurosci 2016; 126: 1077–1083. [DOI] [PubMed] [Google Scholar]
- 16.Puri AS, Kühn AL, Kwon HJ, et al. Endovascular treatment of tandem vascular occlusions in acute ischemic stroke. J NeuroIntervent Surg 2015; 7: 158–163. [DOI] [PubMed] [Google Scholar]
- 17.Lockau H, Liebig T, Henning T, et al. Mechanical thrombectomy in tandem occlusion: Procedural considerations and clinical results. Neuroradiology 2015; 57: 589–598. [DOI] [PubMed] [Google Scholar]
- 18.Cohen JE, Gomori M, Rajz G, et al. Emergent stent-assisted angioplasty of extracranial internal carotid artery and intracranial stent-based thrombectomy in acute tandem occlusive disease: Technical considerations. J NeuroIntervent Surg 2013; 5: 440–446. [DOI] [PubMed] [Google Scholar]
- 19.Nedeltchev K, Brekenfeld C, Remonda L, et al. Internal carotid artery stent placement in 25 patients with acute stroke: Preliminary results. Radiology 2005; 237: 1029–1037. [DOI] [PubMed] [Google Scholar]
- 20.Dorado L, Castano C, Millan M, et al. Hemorrhagic risk of emergent endovascular treatment plus stenting in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis 2013; 22: 1326–1331. [DOI] [PubMed] [Google Scholar]
- 21.Steglich-Arnholm H, Holtmannspötter M, Kondziella D, et al. Thrombectomy assisted by carotid stenting in acute ischemic stroke management: Benefits and harms. J Neurol 2015; 262: 2668–2675. [DOI] [PubMed] [Google Scholar]
- 22.Lescher S, Czeppan K, Porto L, et al. Acute stroke and obstruction of the extracranial carotid artery combined with intracranial tandem occlusion: Results of interventional revascularization. Cardiovasc Intervent Radiol 2015; 38: 304–313. [DOI] [PubMed] [Google Scholar]
- 23.Nambiar V, Sohn SI, Almekhlafı MA, et al. CTA collateral status and response to recanalization in patients with acute ischemic stroke. AJNR Am J Neuroradiol 2014; 35: 884–890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Dababneh H, Bashir A, Hussain M, et al. Endovascular treatment of tandem internal carotid and middle cerebral artery occlusions. J Vasc Interv Neurol 2014; 7: 26–31. [PMC free article] [PubMed] [Google Scholar]
- 25.Jovin TG, Gupta R, Uchino K, et al. Emergent stenting of extracranial internal carotid artery occlusion in acute stroke has a high revascularization rate. Stroke 2005; 36: 2426–2430. [DOI] [PubMed] [Google Scholar]
- 26.Castaño C, Dorado L, Guerrero C, et al. Mechanical thrombectomy with the Solitaire AB device in large artery occlusions of the anterior circulation. A pilot study. Stroke 2010; 41: 1836–1840. [DOI] [PubMed] [Google Scholar]
- 27.Sivan-Hoffmann R, Gory B, Armoiry X, et al. Stent-retriever thrombectomy for acute anterior ischemic stroke with tandem occlusion: A systematic review and meta-analysis. Eur Radiol 2017; 27: 247–254. [DOI] [PubMed] [Google Scholar]
- 28.Johansson E, Cuadrado-Godia E, Hayden D, et al. Recurrent stroke in symptomatic carotid stenosis awaiting revascularization. A pooled analysis. Neurology 2016; 86: 1–7. [DOI] [PubMed] [Google Scholar]