Abstract
Eagle syndrome is defined by an elongated styloid process or a calcified stylohyoid ligament that impinges on surrounding structures and causes a variety of symptoms. Classically, Eagle syndrome presents as neck, throat, or ear pain. The vascular variant, stylocarotid syndrome, can present as headache, transient ischemic attack, or stroke. Carotid artery dissection is a rare complication of stylocarotid syndrome. We report a case of stylocarotid syndrome in a 60-year-old man who presented with a right internal carotid artery (ICA) dissection and focal neurological deficits. Computed tomography with three-dimensional reformatting was used in the evaluation of his pathology. His dissecting right ICA was stented with subsequent symptom resolution. Improved recognition of the relationship between an elongated styloid or calcified stylohyoid ligament and symptomatology may lead to optimal etiology recognition and directed treatment.
Keywords: Eagle syndrome, stylocarotid syndrome, elongated styloid process, internal carotid artery (ICA) dissection, stroke, computed tomography (CT) with three-dimensional (3D) reformatting, stenting of right internal carotid artery (ICA)
Introduction
The styloid process is a bony prominence located on the inferior aspect of the temporal bone that extends anteromedially. There is variance in the anatomy based on length, angulation, and its proximity to the carotid artery.1 Investigators have defined an elongated styloid process as greater than 3 cm in length.2–4 The incidence of an elongated styloid process was initially thought to be 4%, but evaluation with radiographs have suggested an incidence as high as 18%.2,5 Only a minority of these patients are symptomatic.1
Eagle syndrome was first described in 1937 by the otolaryngologist, Watt W. Eagle, as an elongated styloid process or calcified stylohyoid ligament associated with symptoms related to compression of local structures.2 The classic presentation of Eagle syndrome is throat or neck pain, otalgia, dysphagia, and sensation of a foreign body in the throat.6,7 Stylocarotid syndrome, the less common vascular variant of Eagle syndrome, can present as headache, transient ischemic attack (TIA), or stroke.8 Stylocarotid syndrome results from the styloid process compressing the internal (ICA) or external carotid artery. An elongated styloid process is not necessary for stylocarotid syndrome, as it can also be due to medial or lateral deviation.1 Although a rare complication of stylocarotid syndrome, carotid artery dissection has been described.9–11 Some authors suggest that mechanical injury from the elongated styloid process may contribute to the pathogenesis of cervical carotid artery dissection.12
Case report
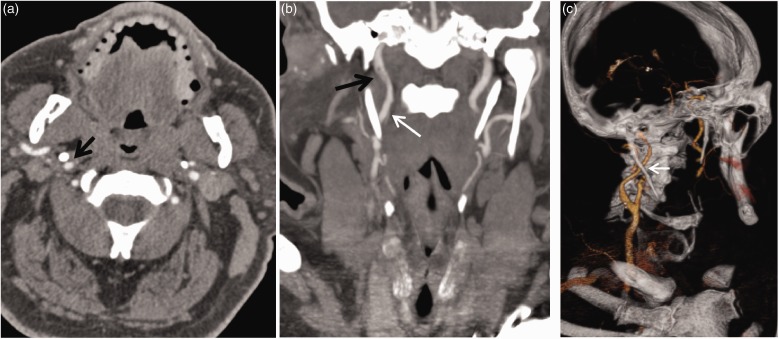
A 60-year-old right-handed obese man with a past medical history of childhood seizures, poorly controlled insulin-dependent diabetes mellitus, controlled hypertension, and an approximately 45-year pack history of smoking cigarettes presented to the emergency department because of sudden onset of right retro-auricular pain, severe bifrontal headache, left arm and leg paresthesia and weakness, and transient slurred speech for approximately one hour. He reported a boxing career history as well. Neurological examinations in the emergency department revealed an initial National Institute of Health Stroke Scale (NIHSS) score of 2. A computed tomography angiogram (CTA) of the head revealed a dissection flap and an approximately 2 cm long mural thrombus of the distal cervical segment of the right ICA (Figure 1). An elongated styloid process with partially calcified stylohyoid ligament was measured at 6.9 cm on the right and 4.4 cm on the left. The right ICA was visualized traveling as close to as 1 mm away from the styloid process.
Figure 1.
(a) Axial computed tomography angiography (CTA) of the neck demonstrates close proximity of the elongated styloid process to the internal carotid artery (ICA) on the right (arrow). (b) Coronal reformat demonstrates a dissection flap (white arrow) and mural filling defect (black arrow). (c) Three-dimensional volume rendering CTA demonstrates the elongated styloid process crossing the cervical ICA (arrow).
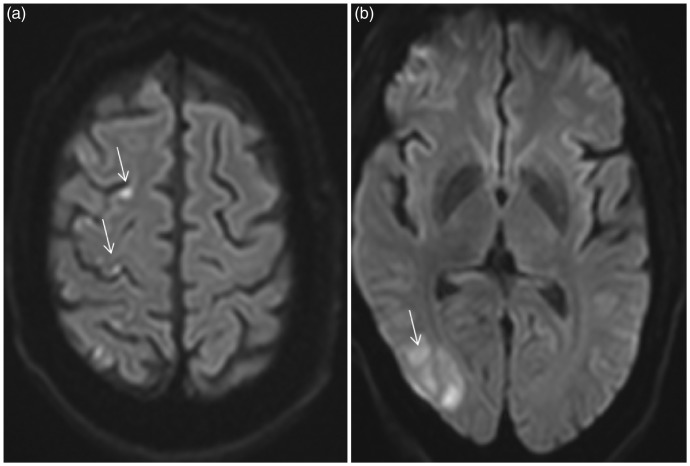
The patient was medically anticoagulated using Heparin. Magnetic resonance imaging of the brain demonstrated numerous microinfarcts in the right parietal cortex, periventricular area and frontal cortex (Figure 2). Magnetic resonance angiography of the neck confirmed the filling defect within the distal right cervical ICA.
Figure 2.
(a) and (b) Axial diffusion-weighted imaging demonstrate multiple acute infarcts involving the right frontal and parietal cortices (arrows).
The following day, the patient experienced recurrent transient stroke symptoms. Repeat CT of the head revealed new right parietal lobe infarct. Heparin was discontinued after daily aspirin 81 mg and clopidogrel 75 mg were initiated.
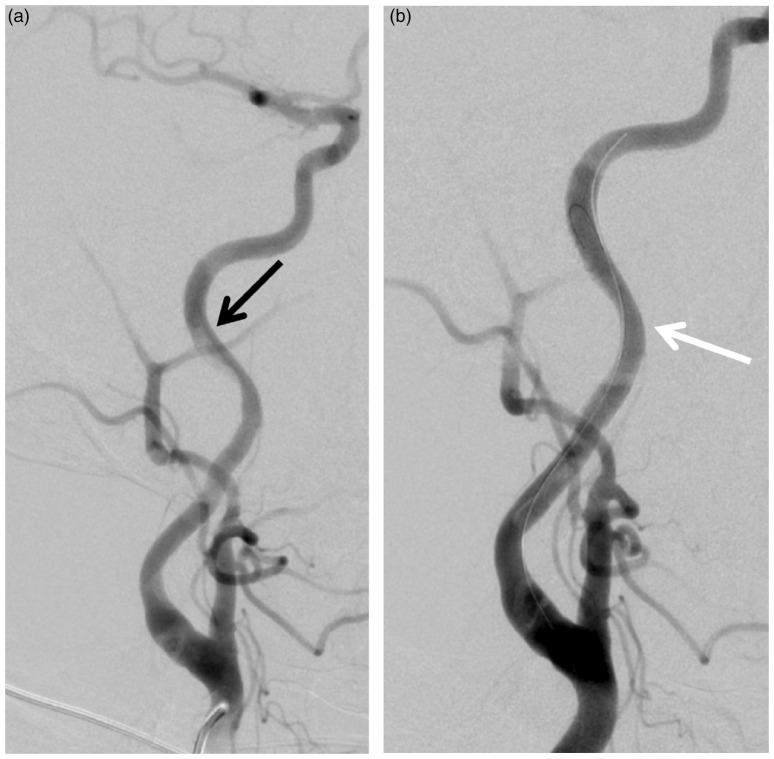
Four days after initial presentation, a conventional diagnostic angiogram of the right common carotid was performed (Figure 3). A 21 mm long dissection flap within the lateral portion of the cervical right ICA was identified. The stenosis measured 71% by North American Symptomatic Carotid Endarterectomy Trial criteria (NASCET).
Figure 3.
Digital subtraction angiography of the right common carotid artery before (a) and after (b) deployment of stent across the dissection (black arrow) and mural thrombus with resolution of the abnormalities (white arrow).
The patient remained neurologically stable until the sixth day of hospital admission when he experienced a sudden onset of right retro-auricular pain, headache, and recurrent increase in left arm weakness and numbness. Because of recurrent infarcts in spite of medical treatment, the decision was made to proceed on the same day with stenting of the right ICA dissection. The decision to stent the dissection was made for the following reasons:
The stenosis is greater than 70%.13
Optimal medical therapy with dual antiplatelet medications failed to prevent embolization.
The risk of propagation of dissection (suggested by recurrent neck pain).
The patient has no other significant arterial lesions aside from the right ICA lesion, an indication that the dissection is caused by the styloid process. A 40 × 6 mm PRECISE PRO RX® Carotid Stent (Cordis, Milpitas, CA) was deployed across the dissection. After the procedure, he no longer had a headache, neck pain, or new neurologic deficits.
Approximately three weeks after discharge, an otolaryngologist evaluated the patient in clinic. The patient reported complete minimal residual symptoms.
Discussion
Stylocarotid syndrome is a rare vascular variant of Eagle syndrome. Patients can present with symptoms ranging from headache to TIA or stroke as a result of the elongated styloid process impinging on the ICA or external carotid artery.8 Carotid artery dissection, a rare complication of stylocarotid syndrome, may result from direct mechanical insult by an elongated styloid process.9–12 When patients meet the definition of having an elongated styloid process, they are four times as likely to develop a carotid artery dissection.12 Other etiologies predisposing to spontaneous carotid artery dissections include smoking, trauma, underlying connective tissue or vascular disorder, and possibly history of migraines and hypertension.14–16
There are no treatment guidelines for Eagle syndrome with carotid dissection. An indication for endovascular treatment can be extrapolated from the NASCET trial—Dissection causing greater than 70% stenosis. Medical judgment also plays a role (e.g. preventing propagation of dissection intracranially or noncompliant patients).
CT imaging is paramount in the diagnosis of stylocarotid syndrome.8,17 When three-dimensional reformatting is used with CT imaging, the relationship between an elongated styloid process and adjacent blood vessels can be better established.18 Understanding the spatial relationship between the styloid process and carotid arteries is beneficial when evaluating the etiology of an ICA dissection in order to guide potential intervention.
Some authors have proposed that the only definitive treatment for any symptomatic variant of Eagle syndrome is styloidectomy.19,20
Conclusion
There are no treatment guidelines for Eagle syndrome with carotid dissection, and medical judgment plays an important role in evaluating treatment options.
This report illustrates successful percutaneous endovascular treatment of a carotid dissection induced by an elongated styloid process.
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Piagkou M, Anagnostopoulou S, Kouladouros K, et al. Eagle’s syndrome: A review of the literature. Clin Anat 2009; 22: 545–558. [DOI] [PubMed] [Google Scholar]
- 2.Eagle WW. Elongated styloid processes: Report of two cases. Arch Otolaryngol 1937; 47: 584–587. [Google Scholar]
- 3.Kaufman SM, Elzay RP, Irish EF. Styloid process variation. Radiologic and clinical study. Arch Otolaryngol 1970; 91: 460–463. [DOI] [PubMed] [Google Scholar]
- 4.Keur JJ, Campbell JP, McCarthy JF, et al. The clinical significance of the elongated styloid process. Oral Surg Oral Med Oral Pathol 1986; 61: 399–404. [DOI] [PubMed] [Google Scholar]
- 5.Correll RW, Jensen JL, Taylor JB, et al. Mineralization of the stylohyoid-stylomandibular ligament complex: A radiographic incidence study. Oral Surg Oral Med Oral Pathol 1979; 48: 286–291. [DOI] [PubMed] [Google Scholar]
- 6.Eagle WW. Elongated styloid process: Further observations and a new syndrome. Arch Otolaryngol 1948; 47: 630–640. [DOI] [PubMed] [Google Scholar]
- 7.Eagle WW. Symptomatic elongated styloid process: Report of two cases of styloid process-carotid artery syndrome with operation. Arch Otolaryngol 1949; 49: 490–503. [DOI] [PubMed] [Google Scholar]
- 8.Chuang WC, Short JH, McKinney AM, et al. Reversible left hemispheric ischemia secondary to carotid compression in Eagle syndrome: Surgical and CT angiographic correlation. AJNR Am J Neuroradiol 2007; 28: 143–145. [PMC free article] [PubMed] [Google Scholar]
- 9.Zuber M, Meder JF, Mas JL. Carotid artery dissection due to elongated styloid process. Neurology 1999; 53: 1886–1887. [DOI] [PubMed] [Google Scholar]
- 10.Todo T, Alexander M, Stokol C, et al. Eagle syndrome revisited: Cerebrovascular complications. Ann Vasc Surg 2012; 26: 729.e1–729.e5. [DOI] [PubMed] [Google Scholar]
- 11.David J, Lieb M, Rahimi S. Stylocarotid artery syndrome. J Vasc Surg 2014; 60: 1661–1663. [DOI] [PubMed] [Google Scholar]
- 12.Raser JM, Mullen MT, Kasner SE, et al. Cervical carotid artery dissection is associated with styloid process length. Neurology 2011; 77: 2061–2066. [DOI] [PubMed] [Google Scholar]
- 13.Paciaroni M, Eliasziw M, Kappelle LJ, et al. Medical complications associated with carotid endarterectomy. North American Symptomatic Carotid Endarterectomy Trial (NASCET). Stroke 1999; 30: 1759–1763. [DOI] [PubMed] [Google Scholar]
- 14.Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med 2001; 344: 898–906. [DOI] [PubMed] [Google Scholar]
- 15.Volker W, Besselmann M, Dittrich R, et al. Generalized arteriopathy in patients with cervical artery dissection. Neurology 2005; 64: 1508–1513. [DOI] [PubMed] [Google Scholar]
- 16.Micheli S, Paciaroni M, Corea F, et al. Cervical artery dissection: Emerging risk factors. Open Neurol J 2010; 4: 50–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sveinsson O, Kostulas N, Herrman L. Internal carotid dissection caused by an elongated styloid process (Eagle syndrome). BMJ Case Rep 2013. DOI :10.1136/bcr-2013-009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Karam C, Koussa S. Eagle syndrome: The role of CT scan with 3D reconstructions [article in French]. J Neuroradiol 2007; 34: 344–345. [DOI] [PubMed] [Google Scholar]
- 19.Strauss M, Zohar Y, Laurian N. Elongated styloid process syndrome: Intraoral versus external approach for styloid surgery. Laryngoscope 1985; 95: 976–979. [PubMed] [Google Scholar]
- 20.Ghosh LM, Dubey SP. The syndrome of elongated styloid process. Auris Nasus Larynx 1999; 26: 169–175. [DOI] [PubMed] [Google Scholar]