Abstract
Vascular events in patients with coarctation of the aorta have been extensively reported and account for the majority of morbidity and mortality in untreated patients. The exact mechanism for this association is not completely understood and may include acquired anomalies or congenital abnormalities of intracranial vessel. Here we report a case of intracranial internal carotid artery dissection with subsequent formation of acquired large carotid aneurysm in a child with severe systemic hypertension and coarctation of the aorta. Endovascular aneurysm exclusion was pursued and it was able to control this potentially lethal complication. This case supports the notion of acquired nature of intracranial vessel abnormalities and underscores the clinical role of interventional neuroradiology in a subset of patients with congenital heart disease.
Keywords: Coarctation of the aorta, intracranial vessel dissection, vascular dissection
Introduction
Vascular events in patients with coarctation of the aorta have been extensively reported and account for the majority of morbidity and mortality in untreated patients.1,2 A complex relationship has been identified between coarctation of the aorta and intracranial aneurysms.3 The incidence of intracranial aneurysms in coarctation of the aorta has been claimed to range between 0 and 10% and such variability is likely due to heterogeneity of studied cohorts regarding age at repair, underlying cardiovascular risk profile, associated lesions, screening modality and age at screening.3–5 The classical hypothesis of a common developmental defect linking coarctation of the aorta to intracranial aneurysms via common origin from neural-crest precursor has been recently challenged by the observation of low rate of intracranial aneurysms in early repaired coarctation of the aorta patients.6 In addition, there is a growing awareness that coarctation of the aorta may carry an overly abnormal cardiovascular risk profile due to the high incidence of systemic high blood pressure, often associated with other classical cardiovascular risk factors.1 From this perspective intracranial aneurysms may well be related to acquired disease of an intracranial blood vessel. This intriguing and complex interplay between innate and acquired vascular derangement in coarctation of the aorta has relevant clinical implications because it may affect screening strategies and dictate modern therapeutic approaches of early correction.6
Here we report a case of intracranial internal carotid artery dissection with subsequent formation of acquired large carotid aneurysm in a child with severe systemic hypertension and coarctation of the aorta.
Case
A nine-year-old female was admitted for acute onset of right-sided hemiplegia a few hours before. At admission her right arm blood pressure was 150/100 mmHg, heart rate was 85 beats per minute, and electrocardiogram showed sinus rhythm with left ventricular hypertrophy; her oxygen saturation was 98%. Her physical examination was notable for right-sided hemiplegia and right facial drop with aphasia, and there were blunted femoral pulses with radio-femoral delay. She had a history of coarctation of the aorta with a (normally functioning) bicuspid aortic valve, diagnosed one month before after a diagnostic work-up prompted by chronic headache and elevated systemic blood pressure. At that time she was started on a multiple drug regimen including beta- and alpha-adrenergic receptor blocker, dihydropyridine calcium antagonist and diuretics, and a brain magnetic resonance imaging was within normal limits.
Upon evaluation, neuroimaging studies demonstrated an ischemic lesion of the left-sided anterior corona radiata, body of caudate nucleus and ipsilateral lentiform nucleus (Figure 1). Focused magnetic resonance angiography confirmed the presence of severe flow limitation of the supraclinoid segment of the left internal carotid artery associated with limited intracranial (subarachnoid) hemorrhage located at the level of the perichiasmal cistern with ipsilateral high-grade hypoperfusion of A1 segment of the anterior cerebral artery and M1 segment of the middle cerebral artery with diminished flow of M2 and M3 segment of the middle cerebral artery (Figure 2(a)). The unifying working hypothesis was dissection of intracranial portion of the left internal carotid artery with distal hypoperfusion and ischemic stroke. This hypothesis was confirmed by appropriate magnetic resonance imaging (Figure 2(b) and (c)). Longitudinal neuroimaging surveillance showed progression of the ischemic lesions extending toward the cortical segment of the middle cerebral artery vascular bed with patient clinical stability, and consensus was to pursue a conservative approach with blood pressure control and antiplatelet therapy. The patient was started on an aphasia rehabilitation program with a prolonged in-hospital stay. A month after hospital admission, she presented with a new episode of severe headache. A new contrast computed tomography ruled out a new intracranial bleeding and showed a large, newly formed aneurysm of the supraclinoid segment of the left internal carotid artery (Figure 3).
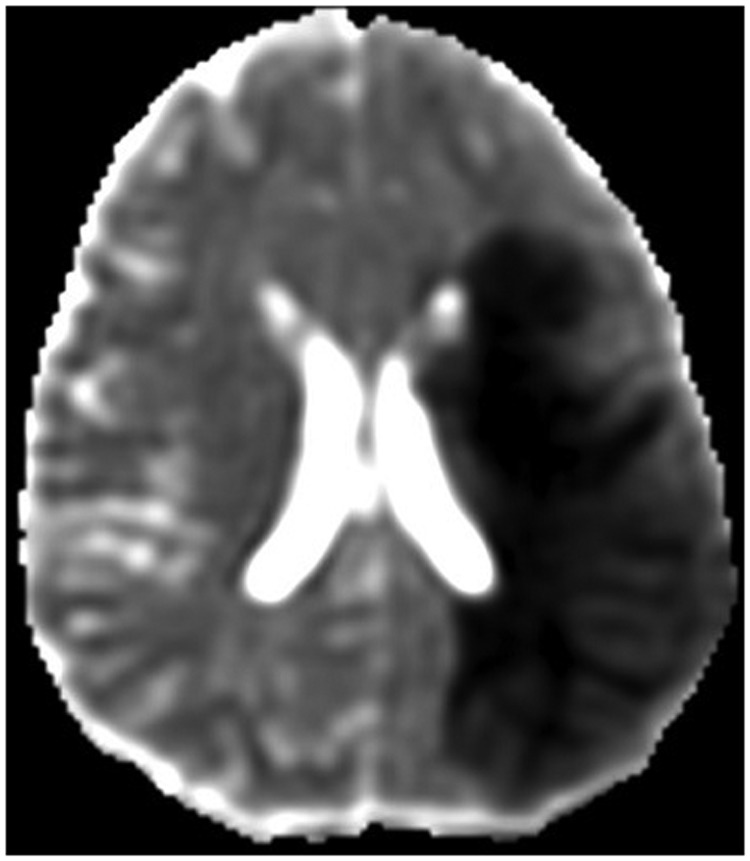
Figure 1.
Magnetic resonance imaging, diffusion weighted imaging (apparent diffusion coefficient) showing a large subacute infarct on the left middle cerebral artery vascular territory.
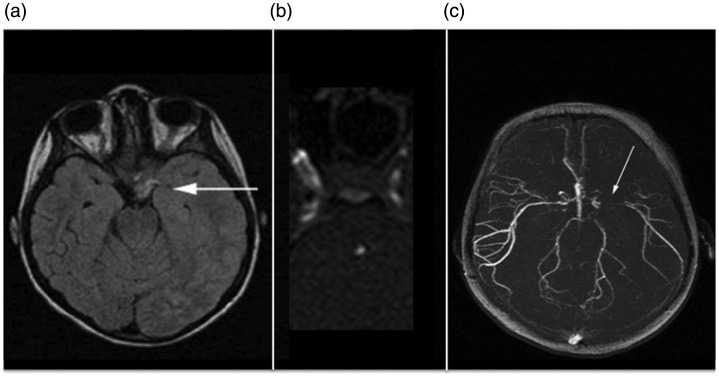
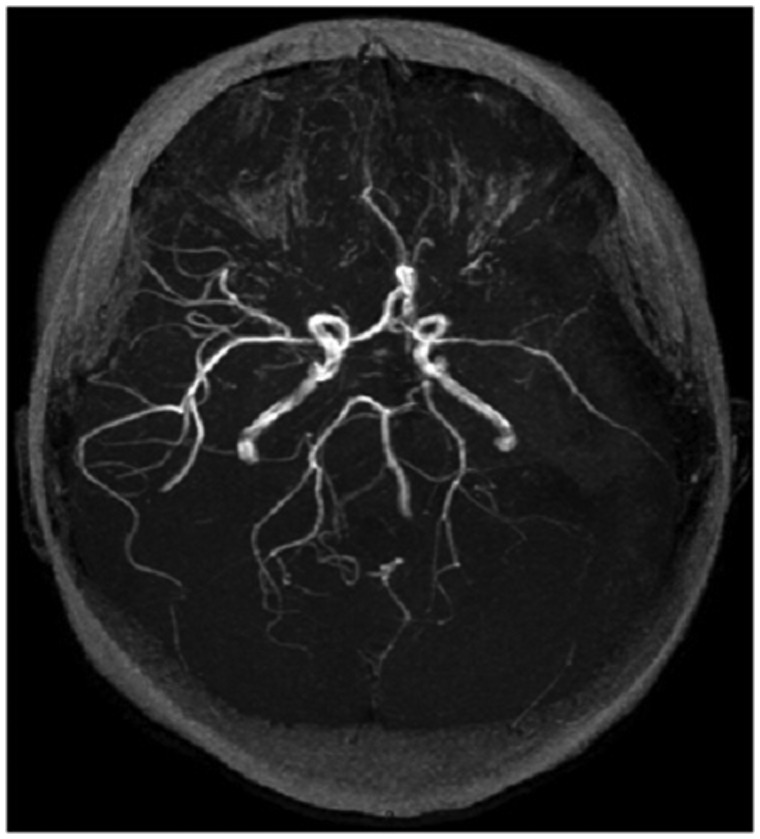
Figure 2.
(a) Magnetic resonance imaging axial flair image showing subarachnoid hemorrhage mostly distributed around the perichiasmal cystern. (b) and (c) Time of flight magnetic resonance angiography revealing stenosis of the left internal carotid artery due to dissection and showing poor visualization of M1 segment of the left middle cerebral artery.
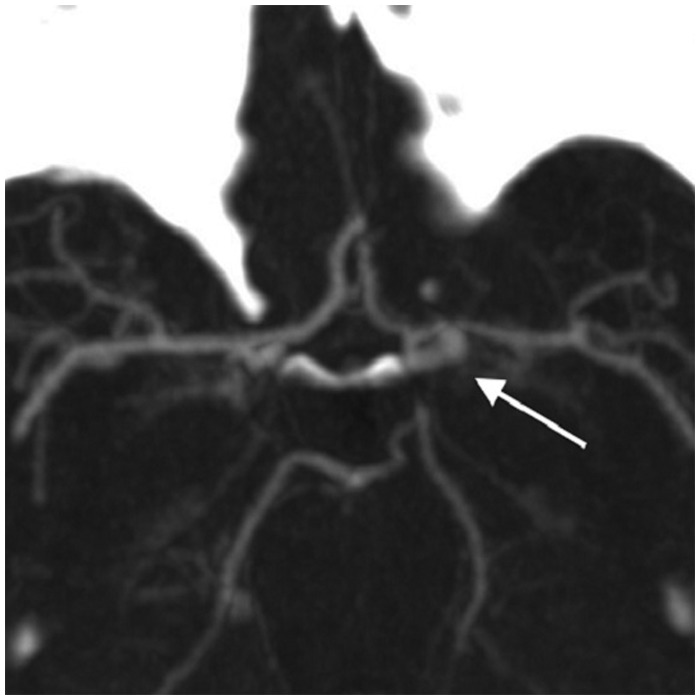
Figure 3.
Computed tomography angiography showing supraclinoid left internal carotid artery aneurysm.
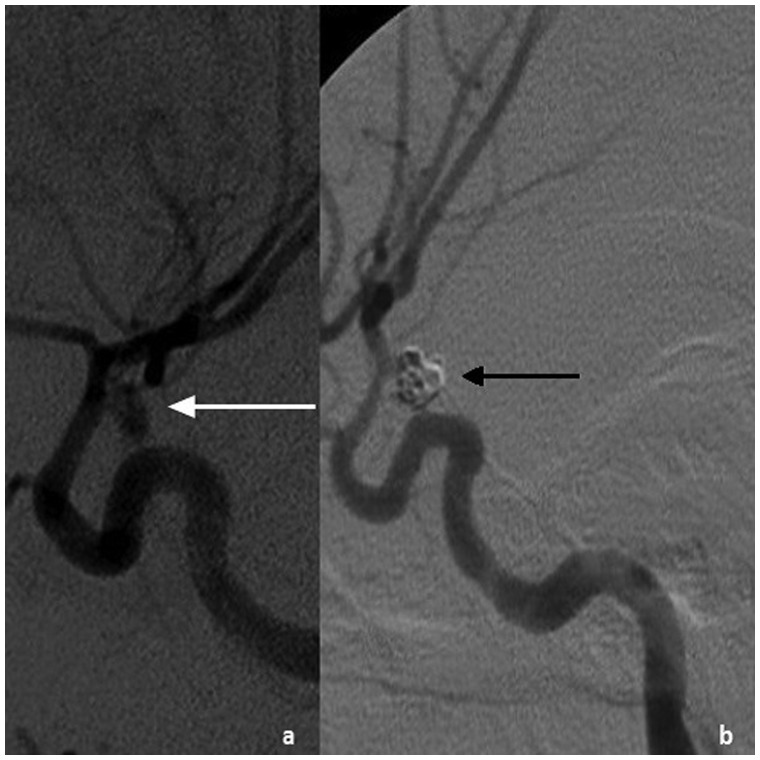
At that point a 6Fr catheter was placed into the patient’s right brachial artery and selective left common and left internal carotid artery angiography was performed. The left carotid artery aneurysm was confirmed and through an axial microcatheter, soft platinum coils (Boston Scientific, MA, US) were released, achieving complete exclusion of the aneurysm from luminal perfusion (Figure 4).
Figure 4.
(a) Selective intracranial angiography confirming the presence of internal carotid artery aneurysm. (b) Exit angiography confirming complete exclusion of the aneurysm after selective coiling.
After the procedure the patient was discharged with improved neurological condition. Longitudinal follow-up included an elective interventional treatment of her coarctation of the aorta with transcatheter (femoral artery) implantation of a covered stent (CP stent©, NuMed Inc, USA) with good angiographic result and progressive reduction of her antihypertensive medications. She was then discharged on aspirin and beta-blocker for blood pressure control. At her last follow-up evaluation she presented with an improved neurological status with significant regression of her aphasia and almost normal right-sided body motor function. She was free of recurrent headache with excellent blood pressure control, and a magnetic resonance imaging of the brain showed stable results (Figure 5).
Figure 5.
Longitudinal follow-up magnetic resonance imaging confirming stable results with no evidence of aneurysmal recurrence and distal flow in the middle and anterior left-sided cerebral artery.
Discussion
Vascular health in patients with coarctation of the aorta remains a challenging task for clinicians. A large body of evidence suggests that coarctation of the aorta is not just a focal pathology of the thoracic aorta but is strongly associated with diffuse abnormalities of arterial blood vessels, in particular in the “high pressure” portion of the vascular system, as suggested by abnormal flow-mediated dilation studies performed and reported by independent investigators.7,8 A major source of confusion still remains on the origin of this “vasculopathy.” Whether this is an innate abnormality related to the common neural crest embryology of the aorta with cardiac muscular arteries, aortic arch, and cervicocephalic blood vessels or just secondary to the detrimental long-standing effect of high blood pressure and other cardiovascular risk factors, this is a debated and clinically important issue.
Our group recently reported that incidence of intracranial aneurysms in a young cohort of patients with early repair of coarctation of the aorta is virtually non-existent.6 Although this is a preliminary observation rising from a single-center study with limited longitudinal follow-up, if confirmed in other studies, such data may put into question the developmental theory linking intracranial aneurysms to coarctation of the aorta.
The case here reported seems to add some evidence to our working hypothesis that intracranial aneurysms in coarctation of the aorta may be secondary to long-standing hypertension and may be prevented by early repair and strict blood pressure control. Indirect evidence of such a hypothesis is given by the observation that vascular morbidity and mortality including stroke is significantly reduced in a more contemporary longitudinal cohort of patients (who now routinely undergo early repair with surgical or transcatheter approaches).6,9,10
This report of acquired large intracranial aneurysms in a coarctation of the aorta patient following acute carotid dissection with stroke exemplifies the complexity of such disease; it recommends a high level of suspicion for such complication in children with intracranial vascular anomalies (for whom coarctation of the aorta screening should be recommended) and reinforces the acquired and progressive origin of blood vessel pathology in this disease.
Acknowledgment
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national guidelines on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008, and has been approved by the institutional committees (Azienda Ospedaliera-Universitaria Policlinico Sant’Orsola-Malpighi, Bologna, Italy).
Declaration of conflicting interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Krieger EV, Stout K. The adult with repaired coarctation of the aorta. Heart 2010; 96: 1676–1681. [DOI] [PubMed] [Google Scholar]
- 2.Cohen M, Fuster V, Steele PM, et al. Coarctation of the aorta. Long-term follow-up and prediction of outcome after surgical correction. Circulation 1989; 80: 840–845. [DOI] [PubMed] [Google Scholar]
- 3.Connolly HM, Huston J, 3rd, Brown RD, Jr, et al. Intracranial aneurysms in patients with coarctation of the aorta: A prospective magnetic resonance angiographic study of 100 patients. Mayo Clin Proc 2003; 78: 1491–1499. [DOI] [PubMed] [Google Scholar]
- 4.Curtis SL, Bradley M, Wilde P, et al. Results of screening for intracranial aneurysms in patients with coarctation of the aorta. AJNR Am J Neuroradiol 2012; 33: 1182–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cook SC, Hickey J, Maul TM, et al. Assessment of the cerebral circulation in adults with coarctation of the aorta. Congenit Heart Dis 2013; 8: 289–295. [DOI] [PubMed] [Google Scholar]
- 6.Donti A, Spinardi L, Brighenti M, et al. Frequency of intracranial aneurysms determined by magnetic resonance angiography in children (mean age 16) having operative or endovascular treatment of coarctation of the aorta (mean age 3). Am J Cardiol 2015; 116: 630–633. [DOI] [PubMed] [Google Scholar]
- 7.Vogt M, Kühn A, Baumgartner D, et al. Impaired elastic properties of the ascending aorta in newborns before and early after successful coarctation repair: Proof of a systemic vascular disease of the prestenotic arteries? Circulation 2005; 111: 3269–3273. [DOI] [PubMed] [Google Scholar]
- 8.de Divitiis M, Pilla C, Kattenhorn M, et al. Vascular dysfunction after repair of coarctation of the aorta: Impact of early surgery. Circulation 2001; 104(12 Suppl 1): I165–I170. [DOI] [PubMed] [Google Scholar]
- 9.Brown ML, Burkhart HM, Connolly HM, et al. Coarctation of the aorta: Lifelong surveillance is mandatory following surgical repair. J Am Coll Cardiol 2013; 62: 1020–1025. [DOI] [PubMed] [Google Scholar]
- 10.Choudhary P, Canniffe C, Jackson DJ, et al. Late outcomes in adults with coarctation of the aorta. Heart 2015; 101: 1190–1195. [DOI] [PubMed] [Google Scholar]