Abstract
Background: Articular cartilage injuries are a common injury among young, active patients, and the most appropriate treatment for these injuries remains controversial. A promising new technology in the treatment of high-grade cartilage injuries is particulated juvenile articular cartilage (PJAC) allograft (DeNovo NT, Zimmer, Warsaw, Indiana). This has been shown to be successful in multiple joints including the knee, talus, and elbow. No studies or case reports exist in supporting or discouraging its use in injuries of the wrist, in specific, the scaphoid. Methods: The use of PJAC allograft is described for the treatment of an active 21-year-old male with an Outerbridge Grade IV chondral lesion on the proximal pole of his right scaphoid and right distal radius scaphoid facet who had failed conservative management. The patient was followed clinically and radiographically for 21 months. Results: The patient had return to full sport (jujutsu) and full range-of-motion, both of which represented an improvement from his preoperative exam. Radiographically, the chondral lucency seen had decreased in size and was almost completely absent on radiographs after 21 months. Conclusions: The results of this case suggest that PJAC can be used safely and effectively in the wrist thereby potentially broadening the indications for its use.
Keywords: allograft, cartilage, osteochondritis, trauma, wrist
Introduction
There are a multitude of surgical treatment options for cartilage restoration after a chondral injury. The choice of technique depends on numerous factors, including the type of lesion, the chronicity, the location of the lesion, its accessibility by arthroscopic or open approaches, concomitant injury, and previous procedures performed.2,7 Among the most studied and utilized are microfracture, osteochondral fragment repair, osteochondral autograft and allograft and autologous chondrocyte implantation (ACI).2,7,11,12,17 There is no consensus as to the most effective form of treatment. Particulated juvenile articular cartilage (PJAC) allograft (DeNovo NT, Zimmer, Warsaw, Indiana) is a promising new option in the surgical treatment of high-grade chondral lesions. The vast majority of the early research into this treatment option has focused on its use around the knee, in patellar chondral lesions and distal femoral chondral lesions, with encouraging results in regard to function and satisfaction scores, as well as radiographic and histological outcomes.3,6,9,19 Successful PJAC allograft use has also been reported in lesions in the talus.1 This technique has been shown, at least in the short-term, to form grossly normal cartilage tissue on subsequent arthroscopic exams, while other studies have shown the formation of hyaline-like repair tissue at the site of the graft as opposed to the less structurally sound fibrocartilage that forms from microfracture procedures.5,8,10,15
Specifically for high-grade cartilage defects of the wrist, osteochondral autograft has been used more frequently than allograft, typically with a costochondral donor site, and long-term data demonstrate it to be a viable option.18 Donor site pain continues to be a common complication after this procedure.13 To our knowledge, there are no publications describing the use of PJAC for high-grade chondral lesions in the scaphoid.
Scaphoid impaction injuries classically occur in athletes who participate in sports necessitating forced and repetitive hyperextension of the wrist. This causes impaction of the dorsal lip of the radius to come into contact with the proximal/dorsal articular surfaces of the scaphoid. This injury is commonly seen in weight lifters, gymnasts, and push-up enthusiasts.14 Treatment generally consists of rest, bracing, and activity modification. If conservative treatment fails, a dorsal scaphoid ridge or dorsal radial lip cheilectomy has traditionally been offered.16 These treatment approaches, however, do not address any existing cartilage defect, which can be a source of great pain and functionally limiting, especially in a high-level athlete.
This case report describes a novel approach to high-grade cartilage defects in the wrist. We describe the use of PJAC allograft in an active 21-year-old male with an Outerbridge Grade IV chondral lesion in the proximal pole of his scaphoid and distal radius scaphoid facet with encouraging clinical and radiographic results 21 months postoperatively.4
Case Report
Patient Description
The patient is a left-hand-dominant 21-year-old male who presented with right wrist pain sustained while practicing jujutsu. Four months prior to presentation in our Hand Center, he noticed pain while attempting to push himself up from a seated position on the ground with his right hand while at jujutsu class. On presentation, the majority of his pain was felt during flexion and extension of the wrist. He was tender over the scapholunate interval and at the proximal pole of the scaphoid, and Watson’s test elicited pain but no “clunk.” He failed a trial of 6 weeks of immobilization in a short arm cast prior to presentation but still remained painful. He was referred to occupational therapy for range of motion exercises but was unable to achieve his desired motion. His range of motion in clinic was 30° of flexion, 90° of extension, and full pronation and supination. Functionally, he was unable to return to compete in jujutsu or carry trays at his work as a waiter because of pain and restricted motion in his wrist. Plain films of the hand (Figure 1) demonstrated a cystic lucency in the proximal pole. A magnetic resonance imaging of the wrist (Figure 2) was obtained, which revealed a focal 4 × 5-mm cartilage defect along the proximal pole of the scaphoid and corresponding articular surface of the radial scaphoid facet, consistent with Outerbridge grade IV chondromalacia. Extensive edema and a cystic lucency were also noted within the proximal pole of the scaphoid.
Figure 1.

Preoperative posteroanterior view of the right wrist showing a cystic lucency in the proximal pole of the scaphoid.
Figure 2.
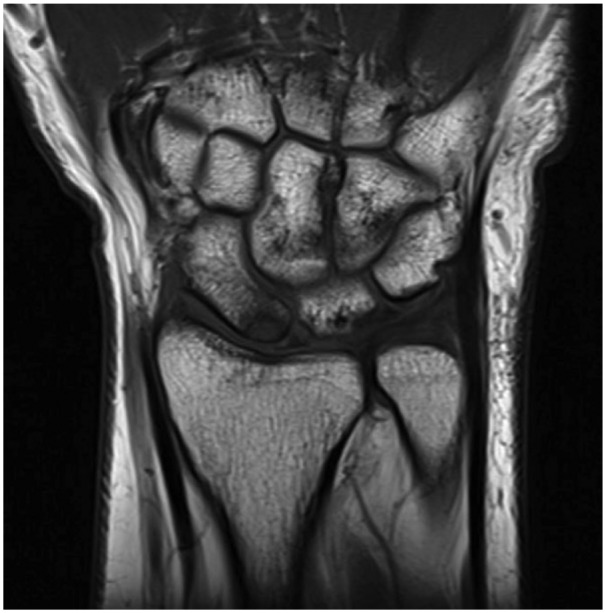
Preoperative magnetic resonance imaging (T1-weighted) coronal view of the wrist illustrating the 4 × 5-mm cartilage defect along the proximal pole of the scaphoid with cartilage loss also present along the corresponding articular surface of the radius.
Intervention
Once the patient had failed nonoperative treatment including a period of extended immobilization, and because of his high-functioning preinjury status, surgical intervention was recommended. An initial diagnostic wrist arthroscopy was performed to evaluate the articular cartilage, the volar radiocarpal ligaments, triangular fibrocartilage complex (TFCC), and proximal intrinsic ligaments. All extrinsic and intrinsic ligaments that were visualized were intact. The radiocarpal joint was then exposed using a dorsal approach, and osteochondral defects were immediately identifiable on the proximal pole of the scaphoid and the corresponding radial scaphoid facet (Figure 3). A burr was used to debride the defects leaving a stable cartilage rim on all sides. The PJAC allograft was then placed with fibrin glue to hold the grafts in place at both defects (Figure 4). After the fibrin glue was dry, the incisions were closed and the patient was placed in a volar splint. His wrist was immobilized in a short arm cast for 6 weeks postoperatively. He was seen postoperatively at 2 weeks, 6 weeks, and 12 weeks. Interval healing of the scaphoid and radial lesions were seen by 6 weeks and increased ossification of the osteochondral defects were seen at 12 weeks postoperatively (Figure 5). Occupational therapy was utilized for finger and wrist range-of-motion exercises.
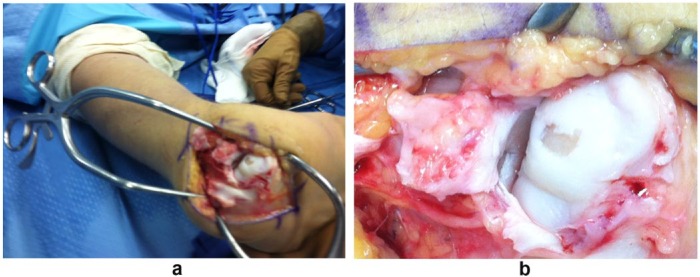
Figure 3.
a and b, Intraoperative views of the full-thickness osteochondral lesion on the proximal articulating surface of the scaphoid.
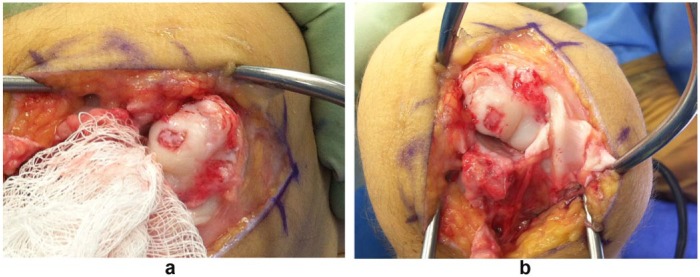
Figure 4.
a and b, Intraoperative views after the allograft was placed.
Figure 5.
Posteroanterior views of the wrist at (a) 6 weeks, (b) 12 weeks, and (c) 21 months, respectively, postoperatively.
Note. The previously seen lucency in the proximal pole of the scaphoid has decreased in size and is almost completely gone by 21 months. These radiographic findings correlated with a complete resolution of symptoms and return to activity.
Follow-up was arranged for this patient 21 months postoperatively. Functionally, he had returned to work as a waiter and to his previous level of jujutsu training without any pain. Postoperatively, his range of motion was 90° of flexion and extension and full pronation and supination. The patient was able to bear weight and perform push-ups on his right wrist without any hindrance in strength or function (Figures 6-8). Radiographs demonstrated almost complete resolution of the osteochondral lesion (Figure 5).
Figure 6.
(a) Pronation and (b) supination approximately equal to the contralateral, uninjured side, at 21 months postoperatively.
Figure 7.
(a) Flexion and (b) extension approximately equal to the contralateral, uninjured side, at 21 months postoperatively.
Figure 8.

Patient able to return to full activities, including push-ups.
Discussion
Repair of full-thickness articular cartilage defects presents a challenging clinical scenario due to the lack of biologic regenerative capacity of hyaline cartilage. Current treatment modalities for high-grade chondral lesions of the wrist vary and include microfracture, primary osteochondral fragment repair, osteochondral auto and allograft and ACI. While the durability of hyaline cartilage is a disadvantage of microfracture, detractors also emphasize the frequency of donor site morbidity with autograft procedures, and 2-stage procedures, like ACI, also have inherent drawbacks, costs, and risks. Particulated juvenile articular cartilage has been used with success around the knee and in the hindfoot and theoretically offers an attractive 1-stage alternative to the donor site morbidity associated with autograft in scaphoid proximal pole osteochondral defects, though, to our knowledge, no literature describes its use in the scaphoid. We have described the use of PJAC in an Outerbridge grade IV lesion of the scaphoid in a high-functioning individual with evidence of pain-free return to preinjury levels of activity. The results of this case suggest that there is great potential for the use of PJAC for focal full-thickness chondral lesions of the scaphoid.
While the biologic and structural advantages of using young, healthy cartilage are clear, there are important disadvantages with use of PJAC as well. These include risk of disease transmission and cost. While disease transmission with the use PJAC is theoretically possible, like any allogenic transplantation, the risk is certainly low. Cost, however, remains high. Currently, 1 unit of DeNovo NT graft is approximately $4500. This underscores the need for appropriate patient selection, adequate preoperative work-up, and discussions with the patient about alternative options. Young patients, without history of preexisting carpal arthritis, are the best candidates for this procedure. Patient compliance is a must, given the strict postoperative restrictions and rehabilitation instructions. Given the success highlighted in this case report in a high-functioning young individual, there is potentially a role for PJAC use in the wrist, although future larger-scale studies are necessary.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all patients for being included in the study.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Bleazey S, Brigido SA. Reconstruction of complex osteochondral lesions of the talus with cylindrical sponge allograft and particulate juvenile cartilage graft: provisional results with a short-term follow-up. Foot Ankle Spec. 2012;5:300-305. [DOI] [PubMed] [Google Scholar]
- 2. Buckwalter JA. Evaluating methods of restoring cartilaginous articular surfaces. Clin Orthop Relat Res. 1999;367(suppl):S224-S238. [DOI] [PubMed] [Google Scholar]
- 3. Buckwalter JA, Bowman GN, Albright JP, Wolf BR, Bollier M. Clinical outcomes of patellar chondral lesions treated with juvenile particulated cartilage allografts. Iowa Orthop J. 2014;34:44-49. [PMC free article] [PubMed] [Google Scholar]
- 4. Cole BJ, Malek MM. Articular Cartilage Lesions. New York, NY: Springer; 2004. [Google Scholar]
- 5. Davidson PA, Rivenburgh DW, Dawson PE, Rozin R. Clinical, histologic, and radiographic outcomes of distal femoral resurfacing with hypothermically stored osteoarticular allografts. Am J Sports Med. 2007;35:1082-1090. [DOI] [PubMed] [Google Scholar]
- 6. Farr J, Tabet SK, Margerrison E, Cole BJ. Clinical, radiographic, and histological outcomes after cartilage repair with particulated juvenile articular cartilage: a 2-year prospective study. Am J Sports Med. 2014;42(6):1417-1425. [DOI] [PubMed] [Google Scholar]
- 7. Friel NA, Bajaj S, Cole BJ. Chapter 21 articular cartilage injury and adult OCD treatment options and decision making. In Scott W. Norman, ed. Insall & Scott Surgery of the Knee. 5th ed. Philadelphia, PA: Elsevier; 2012:153-162. [Google Scholar]
- 8. Frisbie DD, Lu Y, Kawcak CE, DiCarlo EF, Binette F, McIlwraith CW. In vivo evaluation of autologous cartilage fragment-loaded scaffolds implanted into equine articular defects and compared with autologous chondrocyte implantation. Am J Sports Med. 2009;37(suppl 1):71S-80S. [DOI] [PubMed] [Google Scholar]
- 9. Ghazavi MT, Pritzker KP, Davis AM, Gross AE. Fresh osteochondral allografts for post-traumatic osteochondral defects of the knee. J Bone Joint Surg Br. 1997;79(6):1008-1013. [DOI] [PubMed] [Google Scholar]
- 10. Griffin JW, Gilmore CJ, Miller MD. Treatment of a patellar chondral defect using juvenile articular cartilage allograft implantation. Arthrosc Tech. 2013;2(4):e351-e354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hangody L, Füles P. Autologous osteochondral mosaicplasty for the treatment of full-thickness defects of weight-bearing joints: ten years of experimental and clinical experience. J Bone Joint Surg Am. 2003;85:25-32. [DOI] [PubMed] [Google Scholar]
- 12. Horas U, Pelinkovic D, Herr G, Aigner T, Schnettler R. Autologous chondrocyte implantation and osteochondral cylinder transplantation in cartilage repair of the knee joint. A prospective, comparative trial. J Bone Joint Surg Am. 2003;85:185-192. [DOI] [PubMed] [Google Scholar]
- 13. LaPrade RF, Botker JC. Donor-site morbidity after osteochondral autograft transfer procedures. Arthroscopy. 2004;20(7):e69-e73. [DOI] [PubMed] [Google Scholar]
- 14. Linscheid RL, Dobyns JH. Athletic Injuries of the wrist. Clin Orthop Relat Res. 1985;198:141-151. [PubMed] [Google Scholar]
- 15. Lu Y, Dhanaraj S, Wang Z, et al. Minced cartilage without cell culture serves as an effective intraoperative cell source for cartilage repair. J Orthop Res. 2006;24:1261-1270. [DOI] [PubMed] [Google Scholar]
- 16. Mitchell JA, Adams BD. Hand and wrist injuries: wrist pain in gymnasts. In: Renstrom PAFH, ed. Clinical Practice of Sports Injury Prevention and Care, Volume V of The Encyclopedia of Sports Medicine. Boston, MA: Blackwell Scientific Publications; 1993:78-83. [Google Scholar]
- 17. Mithoefer K, McAdams T, Williams RJ, Kreuz PC, Mandelbaum BR. Clinical efficacy of the microfracture technique for articular cartilage repair in the knee: an evidence-based systematic analysis. Am J Sports Med. 2009;37:2053-2063. [DOI] [PubMed] [Google Scholar]
- 18. Obert L, Lepage D, Ferrier M, Tropet Y. Rib cartilage graft for posttraumatic or degenerative arthritis at wrist level: 10-year results. J Wrist Surg. 2013;2(3):234-238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Tompkins M, Hamann JC, Diduch DR, et al. Preliminary results of a novel single-stage cartilage restoration technique: particulated juvenile articular cartilage allograft for chondral defects of the patella. Arthroscopy. 2013;29(10):1661-1670. [DOI] [PubMed] [Google Scholar]