Abstract
Background: Triceps tendon ruptures (TTR) are an uncommon injury. The aim of this systematic review was to classify diagnostic signs, report outcomes and rerupture rates, and identify potential predisposing risk factors in all reported cases of surgical treated TTR. Methods: A literature search collecting surgical treated cases of TTR was performed, identifying 175 articles, 40 of which met inclusion criteria, accounting for 262 patients. Data were pooled and analyzed focusing on medical comorbidities, presence of a fleck fracture on the preoperative lateral elbow x-ray film (Dunn-Kusnezov Sign [DKS]), outcomes, and rerupture rates. Results: The average age of injury was 45.6 years. The average time from injury to day of surgery was 24 days while 10 patients had a delay in diagnosis of more than 1 month. Renal disease (10%) and anabolic steroid use (7%) were the 2 most common medical comorbidities. The DKS was present in 61% to 88% of cases on the lateral x-ray film. Postoperatively, 89% of patients returned to preinjury level of activity, and there was a 6% rerupture rate at an average follow-up of 34.6 months. The vast majority (81%) of the patients in this review underwent repair via suture fixation. Conclusions: TTR is an uncommon injury. Risks factors for rupture include renal disease and anabolic steroid use. Lateral elbow radiographs should be scrutinized for the DKS in patients with extension weakness. Outcomes are excellent following repair, and rates of rerupture are low.
Keywords: triceps tendon, rupture, avulsion, steroid, renal disease
Introduction
Spontaneous triceps tendon ruptures (TTR) are uncommon, accounting for less than 2% of all tendon injuries.1,40 Published reports of TTR are primarily contained within a few small case series. In addition to the infrequent description of this injury pattern, the diagnosis is difficult, misdiagnosis is common, often delayed.3,14-16,35,39,40 A number of medical comorbidities have been described as potential predisposing risk factors for TTR, including anabolic steroid use, local steroid injection for bursitis, oral steroid, renal disease, diabetes, and familial tendinopathy.3,5,9,10,13,19,20,22,25,26,32,34,36,37,42 However, the degree to which these factors contribute to TTR is unknown. The purpose of this systematic review is to (1) identify medical conditions which can be associated with TTR, (2) determine the prevalence of the Dunn-Kusnezov Sign (DKS) associated with TTR, and (3) highlight outcomes of surgical repair and rerupture rates following surgical intervention of TTR.
Materials and Methods
The present study is reported following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) guidelines.38 There was no source of funding for this analysis.
Eligibility
The inclusion criteria for the present analysis incorporated articles that: (1) reviewed results of treatment of patients with TTR; (2) adult patients; and (3) patients who were treated with surgical intervention. Finally, (4) only studies written in the English language were considered.
Studies were excluded if they: (1) were a technique description, therapy article, biomechanical analysis, or a review; (2) analyzed only nonoperative treatment; (3) were a letter to the editor; (4) were not written in the English language; (5) reviewed only partial tears; (6) involved a total elbow replacement; (7) involved patella cubiti; (8) were published in a non-American or non-European journal; (9) were published more than 30 years ago; and (10) reviewed pediatric patients only. In addition, (11) we excluded pediatric patients in series.41 Finally, (12) those reports lacking adequate orthopedic follow-up were excluded. Cases in the latter typically were in medical, as opposed to surgical journals, and only mentioned a triceps injury in passing and did not report any outcome measures.
Variables of Interest
The primary data points obtained were the rates of (1) presence of fleck fracture, DKS, on the lateral x-ray film; (2) return to full preoperative function; (3) time to surgery; (4) delayed diagnosis, subjectively defined to be greater than a month in the majority of the articles; (5) medical comorbidity; and (6) repair technique. The prevalence of the DKS was reported both with and without the 2 largest series.21,35
Search Strategy and Selection of Studies
A systematic review was performed for all articles published on the treatment of TTR through PubMed, MEDLINE, and EMBASE between the years 1985 and 2015. Search terms included triceps* tendon* rupture*.
The abstracts generated by the search were individually assessed for relevance by 2 primary authors. Full articles were reviewed independently according to the inclusion and exclusion criteria. All analysis was verified by J.C.D.
Assessment of Methodological Quality and Data Collection
The GRADE (Grading of Recommendations Assessment, Development and Evaluation Working Group) criteria is an assessment template used to evaluate the quality of methods used in published studies.2 Using this template, the quality of the selected studies was independently assessed by the 2 primary authors. Disagreement concerning study quality was moderated by the senior author.
Data Pooling Across Studies and Data Analysis
Demographic data and outcome measures were collected and pooled. No clear sources of bias were identified among the articles included. Outcome measures were compiled and compared.
Results
The search resulted in 175 potentially eligible studies, while 40 met inclusion and exclusion criteria (Figure 1). There were 29 case reports and 11 case series included, accounting for 262 patients. Analysis of the included case series (Tables 1 and 2) and the included case reports (Table 3) is depicted.
Figure 1.
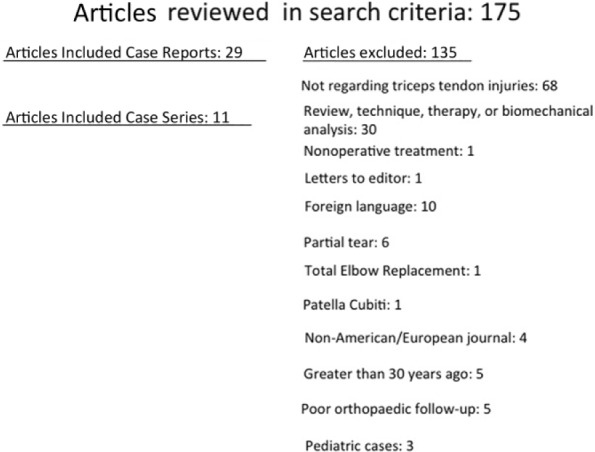
Systematic review process of identification, inclusion, and exclusion of studies, as well as reasons for exclusion.
Table 1.
Case Series: Surgical Volume, Follow-up, Time to Surgery, Findings, and Complications.
| Author | Repairs | Mean follow-up (range), mo | Average age, y | Study findings | Complications |
|---|---|---|---|---|---|
| van Riet et al35 | 23 | 93 (7-264) | 47 | Peak strength of 82% as compared with contralateral side (range, 75%-106%) ROM, 10°-136° All patients had 4-5/5 strength testing |
3 (13%) reruptures 1 patient had olecranon avulsion, ulnar neuropathy, and required HWR Average 10° loss ROM |
| Mirzayan et al21 | 150 | NR | 49 | Neither outcome scores, strength, nor ROM | BT fixation: anchor fixation Reoperation rate (2.1% vs 9.4%)* Infection rate (0% vs. 5.2%)* |
| Mair et al19 | 11 | 36 (NR) | 29 | All regained full ROM without weakness 10/11 returned to professional football |
1 (9%) rerupture |
| Bava et al4 | 5 | 32 (18-49) | 47 | Postoperative: DASH: 1.4 ASES: 99.2 Mayo Elbow: 95.8 Oxford Elbow (pain), 96; (function), 100; (social), 96 |
NR |
| Kokkalis et al17 | 11 | 21 (12-40) | 53 | Preoperative → postoperative VAS: 8.5 → 2.4 Preoperative → postoperative strength:1.6 → 4.8 Postoperative arc of motion: 136° 9/11 patients “very satisfied” and returned to full work |
Loss of 7° arc of motion 1/11 (9%) had postoperative pain over suture knot |
| Farrar and Lippert (1981)12 | 3 | 10 (9-12) | 48 | 3/4 (75%) had 4/5 strength 1/4 (25%) had 5/5 strength |
NR |
| Sierra et al29 | 11 | 17 (7-168) | 50 | 10/11 (91%) in follow-up returned to preinjury activity 2/11 (18%) had 4/5 strength 9/11 (82%) had 5/5 strength |
1 (6%) rerupture 1 (6%) radial nerve palsy 1 (6%) ulnar neuropathy |
| Sollender et al31 | 4 | NR | 42 | 1 patient suture repair 3 patients—NR 4/4 patients were weight lifters using anabolic steroids 2/4 patients had local steroid injection |
1 (25%) rerupture—early return to aggressive weight lifting 1 (25%) contralateral triceps rupture |
| Kose et al18 | 8 | 19 (12-26) | 25 | All patients satisfied; all returned to previous level of function 6/8 (75%) excellent Mayo, 2/8 (25%) good Mayo 5/5 strength in all |
1 (13%) ulnar nerve entrapment, required release 1 (13%) PIN palsy |
| Yoon et al41 | 2 | 19 (5-60) | 21 | 3/4 (75%) had ROM 0°-140° with full strength | 1 (25%) 10° loss of extension |
| Neumann et al24 | 7 | 12 (NR) | 49 | Mean DASH, 10.3 6/7 (83%) had full ROM |
1 (14%) had loss of flexion (110°) |
Note. ROM = range of motion; HWR = hardware removal; NR = not reported; BT = bone tunnel; DASH = Disabilities of the Arm, Shoulder and Hand; ASES = American Shoulder and Elbow Surgeons; Mayo = Mayo Elbow Score; VAS = Visual Analog Scale; PIN = posterior interosseous nerve.
Not statistically significant.
Table 2.
Case Series: Mean Time to Surgery, Radiographic Evidence of Fracture, Medical Comorbidity, and Surgical Technique.
| Author | Mean time to surgery (range), d | Radiographic evidence? | Medical comorbidity contributing to injury? | Technique |
|---|---|---|---|---|
| van Riet et al35 | 63 | Yes: 5/23 | 1—local infection 3—poliomyelitis |
14 suture repair 9 reconstruction with augmentation |
| Mirzayan et al21 | 19 | Yes: 58.4%a | 2.7%—anabolic steroida | Both suture anchor and suture with bone tunnel |
| Mair et al19 | NR | NR | 1—anabolic steroid 6—steroid injection for bursitis |
Suture without augmentation |
| Bava et al4 | NR | NR | NR | Suture anchor (×2) |
| Kokkalis et al17 | NR (8-21) | Yes: 8/11 | None | Suture repair |
| Farrar and Lippert (1981)12 | NR | Yes: 3/3 | 1—renal disease | Suture repair |
| Sierra et al29 | 12 (1-45) | NR | 1—steroid use | Suture repair |
| Sollender et al31 | NR | 1/1 3—NR |
4—anabolic steroid 2—local steroid injection |
Suture repair |
| Kose et al18 | 12 (1-75) | Yes: 8/8 | 1—anabolic steroid use | Suture repair |
| Yoon et al41 | NR | Yes: 4/4 | 4—associated radial head, MCL | 1 suture repair with tension band wire 1 suture repair with anchor (×1) 2 suture repair |
| Neumann et al24 | NR | NR | NR | 6 suture repair 1 suture anchor repair |
Table 3.
Case Reports by Medical Comorbidity.
| Author | Age, y | Mechanism | Radiographic evidence? | Repair and outcomes | Notes |
|---|---|---|---|---|---|
| Anabolic steroid use | |||||
| Nikolaidou et al25 | 28 | Weight lifting | NR | Suture anchor repair At 18 mo: full ROM and strength |
Long-term anabolic steroid use |
| Duchow et al10 | 31 | Fight | Yes: 1/1 | Suture repair Hematoma evacuation and suture repair At 12 wk: full ROM, no ulnar nerve symptoms |
Ulnar nerve compression attributed to forming hematoma History of local steroid injections Long-term use of anabolic steroids and competitive power lifting |
| Bach et al3 | 33 | Weight lifting (snatch 325 lbs) | NR | Suture repair At 9 mo: full ROM, benched 375 lbs, cleaned 407 lbs |
Anabolic steroid use Olympic weight lifter Delayed presentation (28 mo) |
| Bunshah et al5 | 40 | Weight lifting | Yes: 1/1 | Suture repair At 1 y: Mayo Elbow Score, 85; strength 5/5 |
Anabolic steroid use Powerlifter |
| Local steroid injection | |||||
| Weistroffer et al (2003)37 | 49 | Prior bilateral BKA; injured while landing ATV | No: 0/1 | Suture repair with augmentation At 2 y: ROM, 5°-140°, 5/5 strength 6% side-side difference on isokinetic testing Return to competitive motorcycle racing |
Had prior triceps suture repair Described repair with hamstring autograft augmentation |
| Stannard and Bucknell32 | 35 | Bench pressing 315 lbs | NR | Suture repair At 9 mo: ROM, 0°-140° and able to bench greater than 300 lbs |
Six injections for olecranon bursitis (last injection 3 wk prior to rupture) History of anabolic steroid use (12-wk cycles for 4 y—last cycle 6 mo prior) |
| Oral steroid medication | |||||
| Pina et al26 | 43 | Fall, 1 m | Yes: 1/1 | 3 suture anchors At 1 y: full painless ROM Complete strength |
History of oral steroid for asthma |
| Renal disease | |||||
| de Waal Malefijt et al9 | 66 | Avulsion | Yes: 1/1 | Suture repair At 6 mo: ROM, 5°-140° |
Tuberculosis-induced renal insufficiency Parathyroid glands removed 3 wk prior for secondary hyperparathyroidism |
| Zaidenberg et al (2015)42 | 36 (B) | Fall | Yes: 2/2 | Suture repair At 12 mo: full ROM, 5/5 strength DASH: 6 |
Renal transplant secondary to acute glomerulonephritis Required hemodialysis |
| Gupta and Murthi13 | 48 | Fall | Yes: 1/1 | Suture repair with ORIF of distal humerus At 36 mo: ROM 10°-120° |
Renal transplant requiring hemodialysis and oral steroids |
| Tsourvakas et al34 | 27 (B) | Fall | Yes: 2/2 | Suture repair At 3 mo: full ROM |
CKD from acute glomerulonephritis requiring hemodialysis |
| Mont et al22 | 22 (B) | Seizure | No: 0/2 | Suture repair At 1 y: ROM, 0°-120° |
Glomerulonephritis with end-stage renal disease Hypocalcemic-induced tetany causing bilateral triceps/quadriceps tendon ruptures |
| Diabetes mellitus | |||||
| Wagner and Cooney36 | 61 | Roller skating fall | Yes: 1/1 | Suture repair Follow-up: NR 5/5 strength ROM, 20°-130° Return to work as mechanism |
Poorly controlled, insulin-dependent DM Associated nephrolithiasis and essential HTN 5 mo |
| Isolated trauma | |||||
| Tarallo et al (2015)33 | 40 | Car accident | Yes: 1/1 | Suture repair At 30 d: full ROM |
No medical problems |
| Naito et al23 | 17 | Football | Yes: 1/1 | Suture repair At 9 mo: full ROM and strength |
No medical problems Associated radial head/trochlear fractures |
| Daglar et al (2009)7 | 39 | Fall | Yes: 1/1 | Suture repair At 10 mo: 10°-140° |
No medical problems |
| Singh and Pooley30 | 31 | Ice hockey | NR | Suture repair At 6 mo: return to professional hockey |
MRI was negative but surgical exploration demonstrated complete intramuscular rupture of all 3 heads |
| Rajasekhar et al. (2002)28 | 42 | Fell 3 ft | Yes: 1/1 | Suture repair with tension band At 1 y: full ROM and strength |
K-wires removed at 3 mo |
| Dev et al (1999)8 | 53 | Fell | Yes: 1/1 | Steel wire repair At 6 wk: 0°-110° |
Injury included avulsion of triceps origin as well which was treated conservatively |
| Yazdi et al39 | 27 24 |
Fall Fall |
Yes: 1/1 NR |
Suture repair with VY-plasty technique At 2 y: Both patients had full elbow strength and ROM and had returned to work |
Comorbidities not recorded Both were delayed presentation (4 mo) |
| Naito et al23 | 18 | Football | Yes: 1/1 | Suture repair At 2 mo: full ROM and return to football |
Comorbidities not recorded |
| Herrick and Herrick14 | 32 | Unknown | Yes: 1/1 | Unknown repair technique At 1 y: able to bench press 215 kg |
Significant delay to presentation Cubital tunnel syndrome Powerlifter |
| Inhofe and Moneim15 | 19 | Fall | Yes: 1/1 | Suture repair At 3 mo: 10°-135°, resumed recreational activities |
Delay in presentation (9 mo) No medical comorbidities |
| Familial | |||||
| McCulloch et al20 | 19 | Football | Yes: 1/1 | Suture repair At 6 mo: full ROM and strength |
No medical problems Father: bilateral triceps rupture |
Note. NR = not reported; ROM = range of motion; BKA = below knee amputation; ATV = all-terrain vehicle; DASH = Disabilities of the Arm, Shoulder and Hand; ORIF = open reduction internal fixation; CKD = chronic kidney disease; DM = diabetes mellitus; HTN = hypertension; (B) = bilateral; MRI = magnetic resonance imaging.
The average age was 45.6 years (range, 17-61 years), and average follow-up was 34.6 months (range, 1.5-264 months). Upon presentation, 61% of patients had a fleck fracture present on the lateral x-ray film—the DKS. Nearly 90% of patients returned to preinjury level of activity while only 7% experienced a rerupture. The average time to surgery was 24 days while 10 patients in our series had a significant delay in diagnosis (Table 4).
Table 4.
Weighted Averages and Prevalence of Study Characteristics.
| Characteristic | n | Value |
|---|---|---|
| Total TTR | 262 | 262 |
| Average age, y | 262 | 45.6 y (range, 17-61 y) |
| Average follow-up, mo | 107 | 34.6 mo (range, 1.5-264 mo) |
| % of DKS % of DKS (without Mirzayan et al21 and van Riet et al35) |
223 50 |
137 (61.4%) 44 (88%) |
| % return to preoperative function | 79 | 71 (89.0%) |
| % rerupture | 101 | 6 (5.9%) |
| Average time to surgery | 192 | 23.6 d |
| % delay diagnosis >1 mo | 10 | a |
| Medical comorbidity | ||
| Anabolic steroid | 219 | 16 (7.3%) |
| Steroid injection | 219 | 11 (5%) |
| Oral steroid medication | 219 | 1 (<1%) |
| Renal disease | 95 | 12 (10%) |
| Diabetes | 95 | 1 (<1%) |
| Infection | 95 | 1 (<1%) |
| Neuromuscular disease | 95 | 3 (3.2%) |
| Repair technique | ||
| Suture repair | 108 | 88 (81%) |
| Suture anchor | 108 | 17 (17%) |
| Other | 108 | 3 (3%) |
Note. TTR = triceps tendon rupture; DKS = Dunn-Kusnezov Sign.
Time to diagnosis was inconsistently reported, and a percentage was not calculated.
The most common medical comorbidity contributing to TTR was renal disease (10%) followed by anabolic steroid use (7%) and neuromuscular disease (3.2%). The vast majority of repairs were conducted with suture repair only (81%) while a minority used suture anchors (17%). Mechanism of injury can be seen in Table 3 but was not analyzed in Table 4, as mechanism of injury was inconsistently reported in the case series.
Discussion
TTR are an uncommon injury, and descriptions of the injury are contained within small case series and a collection of case reports. The aim of the present systematic review was to combine all known data to better understand TTR. The 3 main findings of the current review were as follows: (1) renal disease (10%) and anabolic steroid use (7%) were the most common medical comorbidities; (2) at presentation, the DKS was present in 61% of cases on the lateral x-ray film; and (3) after surgical intervention, 89% of patients returned to preinjury level of activity while there was only a 6% rerupture rate.
Renal disease (10%) was the most common medical comorbidity in this TTR cohort. Renal disease is known to cause tendinopathy.16,40 The increase in parathyroid hormone frequently seen in renal disease depolymerizes bone, weakening tendon insertions, and may lead to tendon ruptures.11,27 The largest case series included was a multicenter, multisurgeon report published as an abstract only, including 150 TTR. Although 66% had medical comorbidities, the specifics of these comorbidities were not well delineated and were left out of present prevalence.
Anabolic steroid use (7%), local steroid injection (5.3%), and oral corticosteroid were also found to be associated with TTR. Sollender et al31 reported on 4 middle-aged weight lifters who used anabolic steroid and sustained a TTR. In addition, 2 patients had received local steroid injection and tendinopathy. The authors hypothesized that age- and activity-related tendinopathy, in concert with anabolic steroids, lead to the TTR. In addition, patients involved in heavy lifting who present with triceps tendinopathy may be at risk for future rupture.
The DKS, present on the lateral x-ray film, has previously been described as pathognomonic for TTR.6 Although many other reports have described its presence, no large report has determined its prevalence among TTR. Our analysis has determined that the DKS is present in 61% of TTR. If the largest series, a published abstract, and the second largest series are removed from the analysis, the prevalence of the DKS increases to 88%.21,35 Combined, these 2 retrospective reviews accumulated data from 14 different centers. These large multicenter retrospective reviews are subject to a degree of reporting error, so the prevalence may be higher in TTR. Regardless, providers should be aware of this radiographic finding, present in roughly 61% to 88% of patients, which may help reduce misdiagnoses and eliminate the diagnostic odyssey.
The surgical outcomes following TTR are generally excellent with 89% returning to preinjury activity level. Because the body of the systematic review is comprised of discontinuous case reports and short series, outcome measures are varied. After 32 months, Bava et al4 reported that 5 patients after surgical repair of TTR had an average Disabilities of the Arm, Shoulder and Hand (DASH) of 1.4, American Shoulder and Elbow Surgeons (ASES) of 99.2, and Mayo Elbow Score of 95.8. Furthermore, the vast majority of patients had full strength and range of motion following surgical repair.17,18,24,41 Other patients were able to return to heavy weight lifting. After repairing TTR, Bach et al3 reported their patient was able to bench 375 lbs and power clean 407 lbs, whereas Naito et al23 reported that their patient was able to bench 215 kg at 2 months postoperatively. Furthermore, other patients returned to competitive motorcycle racing, professional football, and professional hockey after TTR repair.19,30,37
There were 6 reruptures (5.9%). Three reruptures occurred in the second largest series of 23 TTR.35 One was a routine primary rerupture, whereas a second may have been precipitated by an infection. The third patient actually had 2 reruptures after traumatic episodes. Mair et al19 reported having a rerupture sustained during rehabilitation exercises in a professional football player 6 weeks after the initial repair. In the analysis of middle-aged bodybuilders using anabolic steroids by Sollender et al31, one patient sustained a rerupture during early aggressive weight lifting and another patient had a contralateral rupture in the postoperative period. The 2 other reruptures were due to direct trauma.29
The vast majority (81%) of the patients in this review underwent repair via suture fixation. Mirzayan et al21 compared suture repair with suture anchor fixation following TTR and found no difference in terms of infection rate, reoperation rate, or rerupture rate. However, the authors did note that those repaired with suture anchors were released from medical care sooner. Given the limited data on comparison of surgical technique, the authors do not believe one technique is superior to the other.
There are 3 primary limitations to this study. First, the findings of this review are subject to the bias and error inherent to retrospective data collection. Second, the interpretation of outcomes is limited by their heterogeneity from report to report. Third, 2 case series account for 173 TTR, or 66% of the cases in this systematic review.21,35 The reporting of outcomes, presence of DKS, and complications may be skewed toward these authors reporting.
Despite these limitations, this study represents one of the first systematic reviews of the literature. The 3 key findings were as follows: (1) Renal disease (10%) and anabolic steroid use (7%) were the 2 most prevalent medical comorbidities; (2) the DKS was present in 61% to 88% of TTR on the lateral x-ray film; and (3) 89% of patients returned to preinjury level of activity postoperatively. TTR is a rare and frequently misdiagnosed injury because the vague signs and symptoms associated with it include ecchymosis, pain, and lack of active extension. However, with careful evaluation of potential medical risk factors, scrutiny of the lateral x-ray film for the DKS, early referral to an orthopedist, and better physical exam techniques, patients may expect a positive outcome following surgical repair of TTR. Future research should be directed toward creating a large series with uniform, validated outcome measures.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: This article does not contain any studies with human or animal subjects.
Statement of Informed Consent: Informed consent was obtained when necessary.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Anzel SH, Covey KW, Weiner AD, Lipscomb PR. Disruption of muscles and tendons: an analysis of 1,014 cases. Surgery. 1959;45:406-414. [PubMed] [Google Scholar]
- 2. Atkins D, Best D, Briss PA, et al. ; GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bach BR, Jr, Warren RF, Wickiewicz TL. Triceps rupture. A case report and literature review. Am J Sports Med. 1987;15(3):285-289. [DOI] [PubMed] [Google Scholar]
- 4. Bava ED, Barber FA, Lund ER. Clinical outcome after suture anchor repair for complete traumatic rupture of the distal triceps tendon. Arthroscopy. 2012;28(8):1058-1063. [DOI] [PubMed] [Google Scholar]
- 5. Bunshah JJ, Raghuwanshi S, Sharma D, Pandita A. Triceps tendon rupture: an uncommon orthopaedic condition [published online ahead of print March 12, 2015]. BMJ Case Rep. doi: 10.1136/bcr-2014-206446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carpentier E, Tourne Y. Avulsion traumatique du tendon tricipital brachial. A propos d’un cas. Ann Chir Main Memb Super. 1992;11:163-165. [DOI] [PubMed] [Google Scholar]
- 7. Daglar B, Delialioglu OM, Ceyhan E, Altas O, Bayrakci K, Gunel U. Combined surgical treatment for missed rupture of triceps tendon associated with avulsion of the ulnar collateral ligament and flexor-pronator muscle mass. Strategies Trauma Limb Reconstr. 2009;4(1):35-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dev S, Jimulia T, Pusey RJ. Rupture of the triceps muscle at its attachments. Injury. 1999;30(1):70-71. [DOI] [PubMed] [Google Scholar]
- 9. de Waal Malefijt MC, Beeker TW. Avulsion of the triceps tendon in secondary hyperparathyroidism. A case report. Acta Orthop Scand. 1987;58:434-435. [DOI] [PubMed] [Google Scholar]
- 10. Duchow J, Kelm J, Kohn D. Acute ulnar nerve compression syndrome in a powerlifter with triceps tendon rupture—a case report. Int J Sports Med. 2000;21(4):308-310. [DOI] [PubMed] [Google Scholar]
- 11. Engel MB. Mobilization of muco-protein by parathyroid extract. Ann Pathol. 1952;53:339-351. [PubMed] [Google Scholar]
- 12. Farrar EL, III, Lippert FG., III Avulsion of the triceps tendon. Clin Orthop Relat Res. 1981;161:242-246. [PubMed] [Google Scholar]
- 13. Gupta RR, Murthi AM. Distal humeral fracture with associated triceps tendon avulsion in a renal transplant recipient. Orthopedics. 2010;10:204–207 doi: 10.3928/01477447-20100129-26. [DOI] [PubMed] [Google Scholar]
- 14. Herrick RT, Herrick S. Ruptured triceps in a powerlifter presenting as cubital tunnel syndrome. A case report. Am J Sports Med. 1987;15(5):514-516. [DOI] [PubMed] [Google Scholar]
- 15. Inhofe PD, Moneim MS. Late presentation of triceps rupture. A case report and review of the literature. Am J Orthop (Belle Mead NJ). 1996;25(11):790-792. [PubMed] [Google Scholar]
- 16. Keener JD, Sethi PM. Distal triceps tendon injuries. Hand Clin. 2015;31(4):641-650. [DOI] [PubMed] [Google Scholar]
- 17. Kokkalis ZT, Mavrogenis AF, Spyridonos S, Papagelopoulos PJ, Weiser RW, Sotereanos DG. Triceps brachii distal tendon reattachment with a double-row technique. Orthopedics. 2013;36(2):110-116. [DOI] [PubMed] [Google Scholar]
- 18. Kose O, Kilicaslan OF, Guler F, Acar B, Yuksel HY. Functional outcomes and complications after surgical repair of triceps tendon rupture. Eur J Orthop Surg Traumatol. 2015;7:1131-1139. [DOI] [PubMed] [Google Scholar]
- 19. Mair SD, Isbell WM, Gill TJ. Triceps tendon ruptures in professional football players. Am J Sports Med. 2004;32(2):431-434. [DOI] [PubMed] [Google Scholar]
- 20. McCulloch PC, Spellman J, Bach BR. Familial triceps tendon ruptures. Orthopedics. 2008;31(6):600-602. [DOI] [PubMed] [Google Scholar]
- 21. Mirzayan R, Singh A, Acevedo DC, Sodl JF, Yian E, Navarro RA. Surgical treatment of 150 acute distal triceps tendon ruptures. J Shoulder Elbow Surg. 2015;24:e120. [Google Scholar]
- 22. Mont MA, Torres J, Tsao AK. Hypocalcemic-induced tetany that causes triceps and bilateral quadriceps tendon ruptures. Orthop Rev. 1994;23(1):57-60. [PubMed] [Google Scholar]
- 23. Naito K, Homma Y, Morita M, Mogami A, Obayashi O. Triceps tendon avulsion: a case report and discussion about the olecranon ossification nucleus. Eur J Orthop Surg Traumatol. 2013;2:S193-S196. [DOI] [PubMed] [Google Scholar]
- 24. Neumann H, Schulz AP, Breer S, Faschingbauer M, Kienast B. Traumatic rupture of the distal triceps tendon (a series of 7 cases). Open Orthop J. 2015;9:536-541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nikolaidou ME, Banke IJ, Laios T, Petsogiannis K, Mourikis A. Synthetic augmented suture anchor reconstruction for a complete traumatic distal triceps tendon rupture in a male professional bodybuilder with postoperative biomechanical assessment. Case Rep Orthop. 2014;2014:962930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pina A, Garcia I, Sabater M. Traumatic avulsion of the triceps brachii. J Orthop Trauma. 2002;16(4):273-276. [DOI] [PubMed] [Google Scholar]
- 27. Preston ET. Avulsion of both quadriceps tendons in hyperparathyroidism. JAMA. 1972;221:406-407. [PubMed] [Google Scholar]
- 28. Rajasekhar C, Kakarkapudi TK, Bhrama MS. Avulsion of the triceps tendon. Emerg Med J. 2002;19:271-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sierra RJ, Weiss NG, Shrader MW, Steinmann SP. Acute triceps ruptures: case report and retrospective chart review. J Shoulder Elbow Surg. 2006;15(1):130-134. [DOI] [PubMed] [Google Scholar]
- 30. Singh RK, Pooley J. Complete rupture of the triceps brachii muscle. Br J Sports Med. 2002;36(6):467-469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Sollender JL, Rayan GM, Barden GA. Triceps tendon rupture in weight lifters. J Shoulder Elbow Surg. 1998;7:151-153. [DOI] [PubMed] [Google Scholar]
- 32. Stannard JP, Bucknell AL. Rupture of the triceps tendon associated with steroid injections. Am J Sports Med. 1993;21:482-485. [DOI] [PubMed] [Google Scholar]
- 33. Tarallo L, Zambianchi F, Mugnai R, Costanzini CA, Catani F. Distal triceps tendon repair using Krakow whipstitches, K wires, tension band and double drilling technique: a case report. J Med Case Rep. 2015;9(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Tsourvakas S, Gouvalas K, Gimtsas C, Tsianas N, Founta P, Ameridis N. Bilateral and simultaneous rupture of the triceps tendons in chronic renal failure and secondary hyperparathyroidism. Arch Orthop Trauma Surg. 2004;124(4):278-280. [DOI] [PubMed] [Google Scholar]
- 35. van Riet RP, Morrey BF, Ho E, O’Driscoll SW. Surgical treatment of distal triceps ruptures. J Bone Joint Surg Am. 2003;85(10):1961-1967. [DOI] [PubMed] [Google Scholar]
- 36. Wagner JR, Cooney WP. Rupture of the triceps muscle at the musculotendinous junction: a case report. J Hand Surg Am. 1997;22:341-343. [DOI] [PubMed] [Google Scholar]
- 37. Weistroffer JK, Mills WJ, Shin AY. Recurrent rupture of the triceps tendon repaired with hamstring tendon autograft augmentation: a case report and repair technique. J Shoulder Elbow Surg. 2003;12:193-196. [DOI] [PubMed] [Google Scholar]
- 38. Welch V, Petticrew M, Tugwell P, et al. ; PRISMA-Equity Bellagio Group. PRISMA-Equity 2012 extension: reporting guidelines for systematic reviews with a focus on health equity. PLoS Med. 2012;9(10):e1001333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Yazdi HR, Zomashi I, Ghorban HM. Neglected triceps tendon avulsion: case report, literature review, and a new repair method. Am J Orthop (Belle Mead NJ). 2012;41(7):E98-E99. [PubMed] [Google Scholar]
- 40. Yeh PC, Dodds SD, Smart LR, Mazzocca AD, Sethi P. Distal triceps ruptures. J Am Acad Orthop Surg. 2010;18(1):31-40. [DOI] [PubMed] [Google Scholar]
- 41. Yoon MY, Koris MJ, Ortiz JA, Papandrea RF. Triceps avulsion, radial head fracture, and medial collateral ligament rupture about the elbow: a report of 4 cases. J Shoulder Elbow Surg. 2012;21(2):e12-e17. [DOI] [PubMed] [Google Scholar]
- 42. Zaidenberg EE, Gallucci GL, Boretto JG, De Carli P. Simultaneous bilateral rupture of the triceps tendon in a renal transplant patient. Case Rep Orthop. 2015;2015:903690. [DOI] [PMC free article] [PubMed] [Google Scholar]


